Abstract
Vaccination hesitancy is an important barrier for the effective control of the COVID-19 pandemic. Identifying determinants of COVID-19 vaccination hesitancy is essential in order to reduce mortality rates. Further, given the variability of the factors and the different recommendations used in each country, it is important to conduct cross-country research to profile individuals who are hesitant toward COVID-19 vaccinations. This cross-sectional study aimed to examine cross-country differences and the behavioral, attitudinal and demographic characteristics of vaccine hesitant individuals. Adults living in six European countries (Cyprus, France, Germany, Italy, Poland, and Spain) were eligible to participate. A total of 832 individuals completed the online survey, with 17.9% reporting being hesitant to COVID-19 vaccination. Vaccine accepters were significantly older (M = 38.9, SD = 14.3), more educated (master/postgraduate studies) and lived in a place with a higher number of residents (>500,000 people) compared to those hesitant to COVID-19 vaccination. Discriminant analysis confirmed that the hesitant profile includes a person of younger age, living alone in smaller communities, and without children. Additionally, hesitant participants reported COVID-19-specific characteristics such as lower institutional trust, less adherence to COVID-19 protective behaviors and higher pandemic fatigue. When tackling COVID-19 vaccination hesitancy both socio-demographic and behavioral/attitudinal aspects should be taken into account. Stakeholders are advised to implement targeted vaccination programs while at the same time building trust with population illness cognitions addressed in order to reduce hesitancy rates. Further, stakeholders and public health authorities in each country are suggested to target interventions according to different population characteristics as behavioral and attitudinal determinants of COVID-19 vaccination hesitancy differed between countries.
Introduction
The COVID-19 pandemic has affected over 424 million people worldwide as of February 2022, with increased mortality rates especially in vulnerable individuals such as those living with diabetes, hypertension, or heart failure.Citation1,Citation2 Even though some treatments have been introduced against COVID-19,Citation3 it is widely acknowledged that vaccines are essential in combating the pandemic. In February 2022, five vaccines were under rolling review in Europe and were administered by governmental agents following the authorization by national regulators in terms of their safety and efficiency as reported by the European Medicines Agency (EMA).Citation4 By the end of February 2022, more than four billion people worldwide were vaccinated (55.4% of the world’s population).Citation5 According to the World Health Organization (WHO),Citation6 the primary target groups for receiving the COVID-19 vaccine were healthcare workers, elderly populations, and individuals with underlying health conditions. Therefore, being vaccinated for COVID-19 was a major public health priority which however has been compromised by hesitancy toward vaccines.
Vaccination hesitancy is defined as the delay in acceptance or refusal of vaccines despite their availabilityCitation7 and constitutes one of the top ten threats to global health that has historically contributed to outbreaks of diseases (e.g., measles outbreak), increased mortality rates and increased healthcare costs.Citation8 During the COVID-19 pandemic it was recognized as an important barrier for achieving herd immunity against COVID-19.Citation6 By February 2022, most of the COVID-19 deaths and hospitalizations worldwide were related to refusal to take the vaccine.Citation5 For example, in Cyprus, 80% and 66% of deaths and hospitalizations respectively were unvaccinated individuals, whereas only 5.2% of deaths were fully vaccinated individuals and 34% of hospitalizations were individuals receiving at least one dose.Citation9 Also, in Italy, 84.4% and 90.5% of deaths and hospitalizations in intensive care units accordingly were unvaccinated, whereas 11.5% of deaths were fully vaccinated and 9.5% of hospitalized individuals received at least one dose.Citation10 In US, in January 2022, unvaccinated people aged 12 years and older had 21 times higher risk of dying from COVID-19.Citation11 Efficacy of vaccines (particularly mRNA) was further demonstrated by randomized clinical trials showing 95% efficacy against COVID-19 and minimization of mortality rates.Citation12,Citation13 In addition, a systematic reviewCitation14 found that the global acceptance rates of COVID-19 vaccine were largely variable until December 2020 ranging from 24% in Kuwait to 97% in Ecuador, with the lowest rates observed in the Middle East, Eastern Europe and Russia and the highest in East and South East Asian countries.
There are several socio-demographic, cognitive and psychological factors that contribute to COVID-19 vaccination hesitancy.Citation14–16 Evidence from studies conducted primarily at the national level, suggest that female gender,Citation17,Citation18 younger age,Citation17,Citation19 lower education level,Citation15,Citation16,Citation20 lower perceived severity of COVID-19 infectionCitation15,Citation21 and lower concerns and worry regarding COVID-19Citation16,Citation22 are independently related to COVID-19 vaccination hesitancy. Further, lower institutional trust to government and healthcare authorities,Citation19,Citation20,Citation23 lower adherence to COVID-19 protective measures like physical distancing, and higher pandemic fatigue (i.e., demotivation to perform various activities or inability to sustain physical or mental operations over time due to the pandemicCitation24) were positively associated with COVID-19 vaccination hesitancy.Citation15,Citation20,Citation24 Psychological antecedents of vaccination, namely the 5 C antecedents (i.e., perceptions or processes of calculation, complacency, confidence, constraints, and collective responsibility)Citation25 have also been used to predict COVID-19 vaccination uptake.Citation26 Common reasons for COVID-19 vaccination hesitancy include beliefs in conspiracy theories,Citation17,Citation19,Citation21 concerns about vaccines’ side effects,Citation17–19 concerns regarding the speed of vaccine developmentCitation17,Citation19,Citation23 and low confidence in vaccines in general, including their importance, safety, and efficacy.Citation18,Citation19,Citation23
Overall, given the variability of the factors and the different recommendations and protective measures used in each country, it is important to conduct cross-country research examining such a variability, as well as the profiles of people who are hesitant toward COVID-19 vaccinations in order to provide relevant evidence-based recommendations. Current research is limited in examining the factors associated with COVID-19 vaccination hesitancy independently in one country. Cross-country research conducted at the European level is important in order to attain the coverage target within the European Union as traveling might resume earlier and at a higher volume compared to inter-continental flow. Further, given that there is evidence suggesting that globally about 25% of the general population are hesitant toward COVID-19 vaccines Citation27 it is important to understand and estimate the factors which differentiate vaccine hesitant individuals with vaccine accepters.
Therefore, this study aims to provide the profiles (i.e., characteristics that people are more likely to have) of individuals who are COVID-19 vaccine hesitant compared to those who are accepters. The main objectives are: a) to examine the socio-demographic characteristics of vaccine hesitant and accepters, b) to examine the behavioral and attitudinal characteristics (e.g., institutional trust, psychological antecedents of vaccination, pandemic fatigue) of vaccine hesitant and accepters, and c) to examine cross-country differences to vaccination hesitancy among six European countries (Cyprus, France, Germany, Italy, Poland, and Spain). These countries presented with similar policy-making approaches against COVID-19 but with historically different attributes that are interesting to compare. For example, France has historically a high rate of vaccination hesitancy and with the lower intent to vaccinate against COVID-19 in Europe.Citation28 The same survey conducted by the World Economic Forum identified Italy, Spain and Germany with similar levels of hesitancy whilst systematic reviews highlight high hesitancy levels in Eastern Europe and thus Poland.Citation14 Cyprus is a small European island country with high level of public health interventions and testing implemented during the COVID-19 pandemic.Citation29 Further, during the study period (December 2020-January 2021), the highest prevalence of new COVID-19 cases were identified in Spain and Cyprus followed by Italy, France, and Poland.Citation30 However, the highest prevalence of deaths due to COVID-19 were identified in Poland and Italy while the lowest prevalence of deaths were identified in Cyprus. Moreover, the strictest restrictive measures (see Supplementary Table S1 for policies implemented per country) were identified in Germany and Italy followed by Cyprus, Poland and Spain.Citation30
Table 1. Correlation matrix with Means and Standard Deviations of all included measures.
Methods
Context and research design
A cross-sectional and cross-country study was conducted between December 2020 and January 2021, through the dissemination of an online survey. During this period, in Cyprus, a second lockdown existed with protective measures taken such as the presence of curfew with only the essential shops open like pharmacies. In France, in addition to barrier gestures, curfews were imposed across the country in the period ranging from November 2020 to May 2021. In Italy, incremental control measures were implemented between September 2020 and February 2021, including partial lockdowns. In Spain, due to the increase in COVID cases, measures were taken to reduce nighttime mobility and leisure activities, perimeter closures of regions, and restrictions on family gatherings. In Poland, restrictions introduced in October 2020 (e.g., obligation to wear masks in public areas) were tightened due to the build-up of the second wave of the pandemic and the period of winter school holidays. Vaccination in the so-called “zero” group, which mainly consists of health care workers, also began at that time. More details about policy responses to COVID-19, cases, death rates, and hospitalizations in each country during the study period are available in Supplementary Table S1.
Sample size calculation, recruitment and data collection
A G*Power 3 software calculation (http://www.gpower.hhu.de/en.html) was employed to compute the required sample size of this study, even though this was a cross-sectional study. Specifically, in order to compute the required sample size, an F test for multiple regression, R2 deviation from zero was showing that a sample size of 108 individuals per country could provide a medium to large effect size (f=.20).
Convenience sampling was used. The online survey was promoted in each country using social media and through the local University email lists including students and academic staff. However, there were difficulties to approach the required sample size due to the Christmas holidays. Thus, in order to account for this problem, the countries included with a sample size less than 108 participants were removed from the cross-country comparisons. RedCap software (https://redcap.ucy.ac.cy/) was used to collect the data. Prior to completing the survey, participants provided informed consent electronically. The average duration of the survey was eight minutes. The study was approved by the Cyprus National Bioethics Committee (reference: ΕΕΒΚ ΕΠ 2019.01.131) and site approvals were obtained where necessary. Regarding inclusion criteria, individuals aged 18 years and over, living in one of the six included European countries (Cyprus, France, Germany, Italy, Poland, and Spain) were eligible to participate. There were no other exclusion criteria.
Measures
The included measures were already available in English and German and previously used and validated in the Cosmo survey.Citation24 All measures were translated from English to French, Greek, Italian, Polish and Spanish, and subjected to forward and backward translation procedure.Citation31 For each of the countries of Cyprus, Italy, Poland, and Spain, and for the total sample (including Germany and France), structural validity was examined with Exploratory Factor Analysis (EFA) and internal consistency with Cronbach’s alpha coefficients for the measures that included more than one item or examined as total scores according to their developers (i.e., affective risk perception, institutional trust, pandemic fatigue scale, adherence to COVID-19 protective behaviors). EFA and Cronbach’s alpha were not conducted separately for Germany and France due to the small sample sizes (i.e., Germany: n = 37; France: n = 13). The questionnaire is available in English as Supplementary A.
Outcome
Vaccination behavior
Participants responded to two questions related to their vaccination behavior developed by the authors of the present study. Specifically, they were asked whether they have been vaccinated with the COVID-19 vaccine and if not, if they plan to get vaccinated. Based on the responses on these questions, vaccination behavior status was coded as a binary variable (accepter vs. hesitant) and was the main outcome of the study. Specifically, a participant was defined as “vaccine accepter” if they responded “yes” in any of the aforementioned two questions. In contrast, a participant was defined as “vaccine hesitant” if he responded “no” to the second question (i.e., if not, do you plan to get vaccinated if a COVID-19 vaccination will be available for you).
Predictors
Socio-demographic information
Socio-demographic information included age, sex, educational level, place of residence, work as a healthcare professional, having under-aged children and living situation.
COVID-19 infection
Participants responded to two questions developed by the authors of the present study, on whether they have been infected with COVID-19 or whether they know anyone in their immediate social circle who has been infected with COVID-19.
Cognitive risk perception
Cognitive risk perception of COVID-19 was assessed using three items.Citation24 Two items referred to the probability of being infected with COVID-19 by someone from their family and by someone totally strange to them, on a Likert scale ranging from 1 (very unlikely) to 7 (very likely), and one item on severity perception if they contracted COVID-19 on a Likert scale ranging from 1 (not serious) to 7 (very serious). Higher scores in each item indicated greater probability and perceived severity to be infected with COVID-19.
Affective risk perception
Affective risk perception of COVID-19 was assessed using three items.Citation20,Citation24 The first item asked participants how often they think about COVID-19, on a Likert scale ranging from 1 (something I do not think about at all) to 7 (something I think of all the time). The second item asked participants if COVID feels terrifying, on a Likert scale ranging from 1 (not terrifying at all) to 7 (terrifying). The third item asked participants about worrying for COVID, on a Likert scale ranging from 1 (something to not worry about) to 7 (something to worry about). Higher scores in each item indicated greater thinking, terror and worrying about COVID-19. In the present study and in line with recommendations from the developers of the scale,Citation20,Citation24 one total score was calculated, with EFA indicating the presence of one factor explaining 65.4% of the total variance for the total sample (Supplementary Table S2). EFA was also conducted separately for each country indicating the presence of one factor explaining 72.4%, 60.7%, 66.3% and 60.2% of the total variance for Cyprus, Italy, Poland and Spain respectively. Further, the affective risk perception scale showed acceptable internal consistency separately for each country and for the total sample as well (α>.82).
Table 2. Sociodemographic characteristics of the participants.
Institutional trust
Institutional trust was assessed using four items measuring trust toward state authorities, international health organizations (such as WHO), pharmaceutical corporations and healthcare professionals.Citation32 For example, participants were asked “To what extent do you trust state authorities?” with all items scored on a 5-point Likert scale, ranging from 1 (very little trust) to 5 (a lot of trust). Higher scores in each item indicated greater trust in the respective institution. In line with the developers of the scale,Citation32 one total score was calculated with EFA indicating the presence of one factor explaining 45.3% of the total variance for the total sample (Supplementary Table S3). In addition, EFA indicated the presence of one factor explaining 52.3%, 42.9%, 45.5% and 46.5% of the total variance for Cyprus, Italy, Poland and Spain, respectively. Due to the low percentage of the factor explaining the total variance, results were examined both separately for each item and for the total factor as well. Acceptable internal consistency was also found separately for each country and for the total sample as well (α>.73).
Table 3. Comparisons between vaccine accepters and hesitant for socio-demographics and COVID infection measures (n = 781).
Pandemic fatigue scale (PFS)
The Pandemic Fatigue Scale (PFSCitation24) was used to measure tiredness toward COVID-19. PFS is composed of two subscales, namely behavioral (e.g., I am losing my spirit to fight against COVID-19) and information (e.g., I am sick of hearing about COVID-19) fatigue assessed by three items each. All items were scored on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). Higher scores in each subscale indicated greater behavioral and information fatigue. Additionally, EFA indicated the presence of the two subscales, explaining 53.2% of the total variance for the total sample. Separate examination of the EFA for each country showed also the presence of two factors explaining 48.8%, 49.0%, 44.9% and 40.7% of total variance for Cyprus, Italy, Poland and Spain respectively. Acceptable internal consistency was found for both subscales when examining each country separately and for the total sample, with Cronbach’s alpha>.72 for the Information Fatigue subscale and alpha>.70 for the Behavioral Fatigue subscale (Supplementary Table S4).
Adherence to COVID-19 protective behaviors
Adherence to COVID-19 protective behaviors was assessed using six itemsCitation32 referring to keeping distance from other people, limiting unnecessary traveling, avoiding areas where social distance cannot be kept, avoiding meeting others in closed rooms with insufficient ventilation, washing hands regularly, and wearing a face mask according to current regulations. Each item was scored on an 11-point Likert scale, ranging from 0 (never) to 10 (all of the time). Higher scores in each item indicated greater adherence to the respective protective measure. In the present study, in line with the developers of the scaleCitation32 one total score was calculated, with EFA indicating the presence of one factor explaining 56.1% of the variance for the total sample (Supplementary Table S5). When examining each country separately, EFA showed also one factor explaining 54.1%, 40.0%, 59.4% and 51.2% of total variance for Cyprus, Italy, Poland and Spain respectively. In addition, acceptable internal consistency was found both for the total sample and for each country (α>.87).
Psychological antecedents to hesitancy
The 7 C scaleCitation33 was used to assess psychological antecedents of vaccination hesitancy, namely confidence, complacency, constraints, calculation, collective responsibility, compliance, and conspiracy. It derived from the 5 C model and the 5 C validated scale,Citation25,Citation33 but with the addition of the compliance and conspiracy items. Complacency refers to perceptions that the risks of diseases are low and vaccination is unnecessary.Citation25 Confidence refers to an individual’s trust in safety and effectiveness of vaccines, and constraints refers to the availability, cost and administration of vaccines in a comfortable context. Calculation refers to the engagement of individuals in extensive information searching and collective responsibility refers to the willingness to protect others by one’s vaccination. Finally, compliance refers to the adherence of people to the recommendations of health authorities and conspiracy on the downplay of the COVID-19 severity by the health authorities.Citation33 For example, the confidence item referred to “I am absolutely certain that vaccines against the coronavirus that causes COVID-19 will be safe.” All items were scored on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). Higher scores in each item indicated lower vaccination hesitancy and higher vaccination acceptance.
Attitudes and intention to vaccinate
Attitudes and intention to vaccinate were assessed with one item each.Citation34 In particular, participants were asked whether they would get vaccinated for COVID-19 for free on the following week, on a Likert scale ranging from 1 (definitely not vaccinate) to 7 (definitely vaccinate) and whether they agreed that vaccination against COVID-19 should be mandatory for all citizens, on a Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree).
Statistical analysis
First, correlations between included measures were examined using Pearson’s coefficient with family wise error being corrected using Bonferroni correction (). In addition, Supplementary Table S6 contains internal consistency reliabilities for the measures included in this study. Normality of distribution was examined using Shapiro-Wilk test. Participants’ characteristics are presented using means and standard deviations (SD) for continuous variables with normal distributions, and medians with interquartile ranges (IQR) for continuous measures with skewed distributions. For categorical variables, the absolute (n) and relative (%) frequencies are presented. Associations between the continuous variables and sex were examined using Student’s t-test and the Shapiro-Wilk test, whereas with categorical variables with χ2 test. Effect sizes for categorical variables were examined with Cramer’s V whereas for the mean differences of two or more groups, Cohen’s d and eta squared were used accordingly.
Student’s t-test and the Shapiro-Wilk test were firstly used to examine the associations between the socio-demographic characteristics and other variables with the vaccination behavior status (, Supplementary Table S7). Then, discriminant classification analysis with the calculation of Wilk’s lambda (the closer to 1, the better discriminating ability) and Fisher’s classification function coefficients were used to explore the patterns of socio-demographic characteristics of COVID vaccine hesitant vs. accepters. Logistic regression models were used to examine the association between the socio-demographics (Model 1); COVID-19 infection variables (Model 2); cognitive risk perception (Model 3); affective risk perception (Model 4); institutional trust (Model 5); pandemic fatigue (Model 6); adherence to COVID-19 protective behaviors (Model 7); and the psychological antecedents of hesitancy (Model 8) on COVID vaccination behavior status (Supplementary Table S8). Afterwards, the significant associations of the logistic regression models were retained in a hierarchical multiple regression model adjusting for social and psychological indicators following the previous pattern (, Supplementary Table S9).
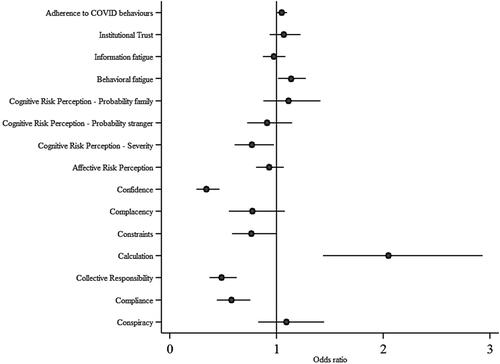
Figure 1. Odds ratios with 95% confidence intervals (CI) of psychological indicators of COVID-19 vaccine hesitancy adjusting for age, sex, educational level, place of residence, health professional status, having under-aged children, living situation, and COVID-19 infection status.
One-way analysis of variance (ANOVA) and the Kruskal-Wallis test were conducted to examine the differences between countries on the socio-demographic, behavioral and attitudinal variables (Supplementary Tables S10 and S11). All statistical tests performed were two-sided with significance level set at α=.05. Statistical analyses were conducted using STATA 14.0 (Stata Corp, College Station, TX, USA) and IBM SPSS statistical software v.25.0.
Results
Participants characteristics
A total of 832 individuals completed the study. The sociodemographic characteristics of the participants and COVID-19 infection variables are described in . The majority of the participants were from Poland (n = 302, 36.3%), followed by Italy (n = 183, 22.0%), Spain (n = 170, 20.4%), Cyprus (n = 127, 15.3%), Germany (n = 37, 4.4%) and France (n = 13, 1.6%). Mean age of participants was 38.3 years (SD = 14.1) with males being significantly older (M = 42.3, SD = 15.8) than females (M = 37.0, SD = 13.4; p<.01). In addition, the majority of the participants had completed postgraduate studies (n = 287, 34.5%) and lived in a place of more than 500,000 people (n = 228, 27.4%). Most of the participants reported living with their own family (n = 483, 58.0%) and not having under-aged children (n = 609, 73.2%). A small number of participants (n = 120, 14.4%) were healthcare professionals. Most of the participants reported that they have not been diagnosed with COVID-19 (n = 620, 74.6%) but they know someone in their social circle that was diagnosed (n = 663, 79.7%). In regards to their vaccination behavior status, 636 participants (76.4%) were COVID-19 vaccine accepters whereas 149 participants (17.9%) were vaccine hesitant.
Correlations between included measures
Correlations between included measures with means and SDs are presented in . The largest statistically significant correlation estimates (p<.001) were found between 7 C compliance and confidence items (r=.65), and collective responsibility and complacency items (r=.57). Hence, the greater statistically significant correlation estimate (r=.65) refers to a moderate association between compliance and confidence which indicates that as the adherence to the recommendations of health authorities (compliance) increases, the individual’s trust in safety and effectiveness of vaccines (confidence) increases too.
Socio-demographic characteristics of COVID-19 vaccine hesitant vs. accepters
Vaccine accepters were significantly older (M = 38.9, SD = 14.3, p<.01), had higher education level (master/postgraduate studies; p<.01) and lived in a place with a higher number of residents (>500,000 people; p<.01) compared to vaccine hesitant participants (see ). The hierarchical regression model (see Supplementary Table S6), revealed that after adjusting for all sociodemographic predictors, only the place of residence was statistically significant. Specifically, living in a place with more than 500,000 people significantly decreased the probability of being hesitant by 81% (95% CI: .05, .77). In addition, discriminant analysis showed a significantly good classification ability of socio-demographics for vaccination behavior status (Wilk’s lambda=.96; p<.01). To be exact, discriminant analysis revealed that the profile of the COVID-19 vaccine hesitant includes a person of younger age, living alone in a place with a lower number of residents, and without under-aged children.
Behavioral and attitudinal characteristics of COVID-19 vaccine hesitant vs. accepters
The binary comparisons between vaccine hesitant and accepters (see Supplementary Table S7) revealed significant differences in all behavioral and attitudinal variables; thus they were included in logistic regression models. Vaccine accepters reported significantly greater affective risk perception (i.e., thinking, terrifying and worrying about COVID-19), greater institutional trust, adherence to COVID-19 protective behaviors, and higher median scores in the 7 C items compared to hesitant participants. Then, according to the eight logistic regression models controlling for the socio-demographic characteristics (Supplementary Table S8), having higher perceived severity of being infected with COVID-19 (Model 3), affective risk perceptions (Model 4), higher institutional trust (Model 5), and lower pandemic fatigue (Model 6) significantly increased the probability of being a vaccine accepter. Furthermore, we found that having higher adherence to COVID-19 protective behaviors (Model 7), and reporting higher scores in the 7 C items such as perceiving that vaccines are safe (Model 8) also significantly increased the probability of being a vaccine accepter.
Furthermore, based on the full model (), we found that having higher behavioral fatigue increased the probability of being vaccine hesitant by 1.14 (95% CI: 1.01, 1.27) times. Also, weighting more the benefits and risks of COVID-19 vaccination in order to make the best decision possible (7 C item), increased the probability by 2.05 (95% CI: 1.43, 2.93) times of being hesitant. In contrast, stronger beliefs that it is important for the entire society if all citizens follow the recommendations of health authorities on COVID-19 vaccination (7 C item), greater perceived severity of being infected with COVID-19 and greater adherence to COVID-19 behaviors decreased the probability of being hesitant by 42% (95% CI: .44, .75), 23% (95% CI: .61, .97) and 5% (95% CI: .84, .95), respectively.
Cross-country comparisons on COVID-19 vaccination hesitancy
Our cross-country analysis revealed that behavioral and attitudinal determinants of COVID-19 vaccination hesitancy differed between the four European countries (Cyprus, Italy, Spain and Poland). Germany and France were excluded from the cross-country comparisons due to small sample size. Results for the cross-country comparisons for socio-demographic characteristics, COVID-19 infection variables and vaccination behavior status are presented in Supplementary Table S9, whereas for behavioral and attitudinal measures in Supplementary Table S10. First, the four countries (Cyprus, Italy, Poland, and Spain) significantly differed on socio-demographic characteristics. Spanish participants (M = 52.3, SD = 12.1) were older than Polish (M = 36.6, SD = 11.3), Italian (M = 35.0, SD = 15.0) and Cypriot participants (M = 29.8, SD = 10.2). Furthermore, the majority of Polish (n = 164, 54.3%) lived in a place with more than 500,000 people while most Cypriots (n = 40, 31.5%) and Spanish (n = 62, 36.5%) lived in a place with 100,001–500,000 people and Italians (n = 87, 47.5%) in a place with 20,001–100,000 people.
Across countries, a higher number of vaccine accepters was found than vaccine hesitant participants (p<.01). The majority of hesitant participants were identified in Cyprus (n = 51 out of 127, 43.6%), followed by Poland (n = 54 out of 302, 18.6%), Spain (n = 13 out of 170, 8.3%) and Italy (n = 11 out of 183, 6.5%). Italians reported significantly greater affective risk perception (thinking frequency, terrifying and worrying about COVID-19), greater institutional trust and greater adherence to COVID-19 protective behaviors than participants from the other countries (Supplementary Table S11). Cypriots and Polish participants reported significantly greater perceived severity of being infected with COVID-19 as well as Cypriots reported greater information and behavioral pandemic fatigue.
Discussion
Our findings suggest that almost one fifth of the participants (18%) that reside in four European countries (Cyprus, Italy, Poland, Spain) and participated in the study during the period of December 2020-January 2021, were hesitant toward COVID-19 vaccination. A variety of behavioral, attitudinal and demographic determinants were found to be associated with COVID-19 vaccination hesitancy, reflecting the complexity of this problem.Citation7
In the present study, we found identifiable groups that are more likely to be COVID-19 vaccine hesitant across countries. These included those of younger age, living alone in smaller communities, and without under-aged children. Older people may report higher vaccination acceptance due to increased perceived risks of developing severe COVID-19 complicationsCitation16,Citation22 and people having children being more willing to be vaccinated in order to protect their children.Citation35 Also, people living in urban areas may be at higher risk of perceived COVID spread and usually have some better socio-demographic characteristics (e.g., level of education), thus associated with greater willingness to be vaccinated.Citation36
This study also confirms that hesitancy to COVID-19 vaccination carries the complexity, time-sensitivity and context-specificity of hesitancy to vaccinations in generalCitation8,Citation37 but also with additional characteristics that are COVID-19-specific namely pandemic fatigue, institutional trust and adherence to protective behaviors. Pandemic fatigue and institutional trust have been increasingly investigated as negative determinants of behavioral responses to COVID-19 pandemic.Citation38 Additionally, we found that increased worrying about the severity of being infected and about COVID-19 in general, and the psychological antecedents of reflective and automatic motivation (calculation), and greater adherence to the recommendations of health authorities (compliance) were associated with the acceptance of vaccination. Combined with findings of previous studies,Citation16,Citation24 we suggest that the strategies used for tackling hesitancy cannot be uni-dimensional such as targeting the population illness cognitions (i.e., perceived severity) and specific population groups (e.g., younger, living in rural areas and large communities) in isolation. It requires multi-dimensional approaches where increasing trust in national and international institutions can be gained while at the same time improving adherence to protective behaviors including vaccine uptake.Citation39
Our cross-country analysis revealed that behavioral and attitudinal determinants of COVID-19 vaccination hesitancy differed between the four European countries (Cyprus, Italy, Spain and Poland). Germany and France were excluded from the cross-country comparisons due to small sample size. Cyprus had the highest rates of hesitancy compared to Italy, Poland, and Spain. People living in Cyprus and Poland reported also greater pandemic fatigue and perceived severity of being infected with COVID-19. Significantly greater institutional trust (e.g., state authorities, health organizations), greater affective risk perception (e.g., worrying about COVID-19) and greater adherence to COVID-19 protective behaviors was identified in people living in Italy compared to other countries indicating a certain degree of variability despite similarly rigid control measures in place. The higher rates of vaccination hesitancy found in Cyprus might be associated with the lower institutional trust and the higher pandemic fatigue that were observed, compared to the rest of the countries. Therefore, we suggest that future studies should examine cross-country comparisons longitudinally because determinants of COVID-19 vaccination hesitancy may change over time due to the recurrence of new COVID-19 waves, and new evidence on the effectiveness of the COVID-19 vaccines.Citation40
Vaccination campaigns should prioritize younger people, those living alone in smaller communities, and those without under-aged children, and also engage these groups when designing public health campaigns.Citation41 For example, public health authorities could engage young people as health champions who can encourage their peers to vaccinate. Further, this study has confirmed evidence that trust in institutions is important for controlling of past outbreaks of infectious diseases like H1N1, SARS, MERS and Ebola.Citation42 Therefore, strategies that incorporate behavior change techniques such as credible sourcesCitation43 should also consider whether these sources are trusted by the local population and how to increase confidence.Citation44
Cross-country variations in determinants of hesitancy can be also considered. For example, in Italy, engagement of state authorities and institutions to vaccination campaigns might improve uptake whereas in the rest of the included countries, engagement to vaccinations by established authorities might provoke vaccination resistance.Citation20 Furthermore, since individuals who trust the authorities are more likely to accept the COVID-19 vaccine, then authorities should introduce vaccine programs through different channels including the healthcare systems, while building or consolidating trust to those who are more skeptical by being transparent on processes and decisions taken. Findings on the psychological antecedents of vaccinationCitation25 suggest that when promoting COVID-19 vaccinations, the emphasis should be given to the benefits of being vaccinated instead of the risks of vaccination and emphasizing the collective responsibility. Public health authorities are recommended also to use social learning approaches such as modeling to tackle vaccination hesitancy. Engaging role models in communities and people who are more likely to be trusted such as healthcare providers and developing and implementing stratified vaccination campaigns to tackle youth and people living in rural areas may increase vaccination uptake.Citation19
The findings of this study should be interpreted in light of its limitations. Data collection was done using a convenient sample approach, promoted through University email lists and social media and was conducted online, limiting our study representativeness. This resulted in mostly highly educated individuals participating and with certain groups missed (e.g., elderly). However, these evidence can be used to inform the design of future longitudinal studies with representative samples in terms of education, age and gender. Secondly, samples per country were also limited to be representative of the entire population, potentially limiting the validity of cross-country comparisons. Germany and France were removed from these analyses as their sample sizes were small. Further, the heterogeneity observed in the samples across countries may have affected the outcomes (e.g., people living in Cyprus were the youngest). Also, due to the cross-sectional design of the study only associations between the groups of interest could be examined and not causal relationships. Another limitation concerns the risk of bias due to misreporting of self-reported intentions about the COVID-19 vaccines with self-report data potentially under or over-estimating reported associations. Finally, results of this study such as attitudes against COVID-19 may change over time due to a rapidly evolving context with adverse events possibly reported in some of the COVID-19 vaccines during the roll out.Citation40
Conclusions
To conclude, various behavioral, attitudinal and demographic determinants were observed contributing to COVID-19 vaccination hesitancy in a sample comprised by people from six European countries. In consideration of the small sample size in France and Germany, it was found that the profile of the COVID-19 vaccine hesitant is a person of a younger age with no children, living alone, in a place with lower number of residents. Lower institutional trust, greater pandemic fatigue and perceived severity of being infected with COVID-19, as well as psychological antecedents of vaccination were associated with the profile of COVID-19 vaccine hesitant. To tackle under-immunized people more effectively both at a national and European level, it is advised that government, policy makers and healthcare professionals use multi-dimensional approaches where institutional trust can be gained, more hesitant groups are encouraged to receive COVID-19 vaccine and population illness cognitions are addressed while at the same time improving vaccine uptake. Only then, COVID-19 mortality rates can be reduced and possibly prevent outbreaks of pandemics in the future.
Supplemental Material
Download MS Word (66.6 KB)Disclosure statement
No potential competing interest was reported by the author(s).
Additional information
Funding
References
- Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318(5):E736–E741. doi:10.1152/ajpendo.00124.2020.
- Lippi G, Wong J, Henry BM. Hypertension in patients with coronavirus disease 2019 (COVID-19): A pooled analysis. Pol Arch Intern Med. 2020;130(4):304–309. doi:10.20452/pamw.15272.
- Rodriguez-Guerra M, Jadhav P, Vittorio TJ. Current treatment in COVID-19 disease: A rapid review. DIC. 2021;10(10):1–8. doi:10.7573/dic.2020-10-3.
- European Medicines Agency. COVID-19: latest updates. Published 2021. https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/covid-19-latest-updates.
- Our World in Data. Published 2022. https://ourworldindata.org/?fbclid=IwAR1Mi_92-CTr1RXYW097s1c_AbtXFdUH-ByPEH8heTHnaskjUT_wFkm11nQ8.
- World Health Organization. Guidance on developing a national deployment and vaccination plan for COVID-19 vaccines: interim guidance. World Health Organization. 2020. V:89. https://www.who.int/publications/i/item/WHO-2019-nCoV-Vaccine_deployment-2020.1.
- MacDonald NE, Eskola J, Liang X, et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi:10.1016/j.vaccine.2015.04.036.
- Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine. 2015;33:D66–D71. doi:10.1016/j.vaccine.2015.09.035.
- Cyprus Ministry of Health. COVID-19 deaths and hospitalizations. Published 2022. https://www.data.gov.cy.
- Sanità I d. COVID-19 Epidemiological Data. Published 2022. https://www.epicentro.iss.it/.
- Centers for Disease Control and Prevention. COVID Data Tracker. Published 2022. https://covid.cdc.gov/covid-data-tracker/#rates-by-vaccine-status.
- Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi:10.1056/nejmoa2034577.
- Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–416. doi:10.1056/NEJMoa2035389.
- Sallam M. Covid-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):115–160. doi:10.3390/vaccines9020160.
- Schwarzinger M, Watson V, Arwidson P, Luchini AF. S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Heal. 2021;2667(21):1–12. doi:10.1016/S2468-2667(21)00012-8.
- Reisdorf BC, Blank G, Cotten SR, et al. Overcoming COVID-19 vaccine hesitancy, 2021.
- Fadhel FH. Vaccine hesitancy and acceptance: an examination of predictive factors in COVID-19 vaccination in Saudi Arabia. Health Promot Int. 2021;1–13. doi:10.1093/heapro/daab209.
- Wang Y, Liu Y. Multilevel determinants of COVID-19 vaccination hesitancy in the United States: A rapid systematic review. Prev Med Reports. 2022;25:101673. doi:10.1016/j.pmedr.2021.101673.
- Razai MS, Osama T, McKechnie DGJ, Majeed A. Covid-19 vaccine hesitancy among ethnic minority groups. BMJ. 2021;372:n513–2. doi:10.1136/bmj.n513.
- Murphy J, Vallières F, Bentall RP, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1):1–15. doi:10.1038/s41467-020-20226-9.
- Nazlı ŞB, Yığman F, Sevindik M, Deniz Özturan D. Psychological factors affecting COVID-19 vaccine hesitancy. Ir J Med Sci. 2022;191(1):71–80. doi:10.1007/s11845-021-02640-0.
- Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–7006. doi:10.1016/j.vaccine.2020.09.041.
- Cook EJ, Elliott E, Gaitan A, et al. Vaccination against COVID-19: factors that influence vaccine hesitancy among an ethnically diverse community in the UK. Vaccines. 2022;10(1):106–113. doi:10.3390/vaccines10010106.
- Lilleholt L, Zettler I, Betsch C, Böhm R. Pandemic fatigue: measurement, correlates, and consequences. PsyArXiv Prepr. 2020;1–36. https://psyarxiv.com/2xvbr/
- Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. Plos One. 2018;13:e0208601. doi:10.1371/journal.pone.0208601.
- Kwok KO, Li KK, WEI WI, Tang A, Wong SYS, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud. 2021;114:103854. doi:10.1016/j.ijnurstu.2020.103854
- Ward JK, Alleaume C, Peretti-Watel P. The French public’s attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc Sci Med. 2020;265:112021–113414. doi:10.1016/j.socscimed.2020.113414
- IPSOS. Global attitudes on a COVID-19 vaccine: Ipsos survey for the world economic forum, 2020.
- Quattrocchi A, Mamais I, Tsioutis C, et al. Extensive testing and public health interventions for the control of COVID-19 in the Republic of Cyprus between March and May 2020. JCM. 2020;9(11):3598. doi:10.3390/jcm9113598.
- Our World in Data. COVID-19 Stringency Index. Published 2022. https://ourworldindata.org/grapher/covid-stringency-index?fbclid=IwAR0X7M6pW4TguWcKyAqTACpxbUO51LBczO2P7oKgrlNGoLj4IzFViyIvOo0.
- Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J Eval Clin Pract. 2011;17(2):268–274. doi:10.1111/j.1365-2753.2010.01434.x.
- Pummerer L, Böhm R, Lilleholt L, Winter K, Zettler I, Sassenberg K. Conspiracy theories and their societal effects during the COVID-19 pandemic. Soc Psychol Personal Sci. 2022;13(1):49–59. doi:10.1177/19485506211000217
- Geiger M, Rees F, Lilleholt L, et al. Measuring the 7Cs of vaccination readiness 2021. doi:10.1027/1015-5759/a000663.
- Pfattheicher S, Petersen MB, Böhm R. Information about herd immunity through vaccination and empathy promote COVID-19 vaccination intentions 2021. https://psyarxiv.com/wzu6k/.
- Akarsu B, Canbay Özdemir D, Ayhan Baser D, Aksoy H, Fidancı İ, Cankurtaran M. While studies on COVID-19 vaccine is ongoing, the public’s thoughts and attitudes to the future COVID-19 vaccine. Int J Clin Pract. 2021;75(4):1–10. doi:10.1111/ijcp.13891.
- Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the united states. Vaccines. 2021;9(2):118–119. doi:10.3390/vaccines9020119.
- Shen AK. Finding a way to address a wicked problem: vaccines, vaccination, and a shared understanding. Hum Vaccin Immunother. 2020;16(5):1030–1033. doi:10.1080/21645515.2019.1695458.
- Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi:10.1038/s41591-020-1124-9.
- Lawes-Wickwar S, Ghio D, Tang MY, et al. A rapid systematic review of public responses to health messages encouraging vaccination against infectious diseases in a pandemic or epidemic. Vaccines. 2021;9(2):1–26. doi:10.3390/vaccines90200:72.
- Wise J. Covid-19: European Countries suspend use of Oxford-AstraZeneca vaccine after. BMJ. 2021;372:n699. doi:10.1136/bmj.n699
- Woodall J, White J, South J. Improving health and well-being through community health champions: A thematic evaluation of a programme in Yorkshire and Humber. Perspect Public Health. 2013;133(2):96–103. doi:10.1177/1757913912453669.
- Siegrist M, Zingg A. The role of public trust during pandemics: implications for crisis communication. Eur Psychol. 2014;19(1):23–32. doi:10.1027/1016-9040/a000169.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(42):12–42. doi:10.1186/1748-5908-6-42.
- Kreps S, Prasad S, Brownstein JS, et al. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020;3(10):e2025594. doi:10.1001/jamanetworkopen.2020.25594.
