Abstract
Surgery is a cornerstone of modern health care. Medical errors resulting from the clinical treatment of patients are a problem with global relevance. Among “never events,” wrong-site surgery accounts for preventable mistakes with a big impact on patients as well as the economy. Wrong-site surgery has many contributing factors, whose identification is challenging. Nevertheless, it remains indisputable that wrong-site surgery affects patients’ lives on many levels, ranging from physical disability to mental health. In addition, it aggravates the economic integrity of healthcare systems, healthcare workers’ professional standards, and the public’s trust in surgical services. Possible solutions for wrong-site surgery include perioperative protocols, surgical checklists, effective communication, education, continuous evaluation of existing procedures, and the implementation of new technology.
Surgery is a specialized healthcare field in which preventable medical errors and potential near misses can happen. However, the landmark publication of the Institute of Medicine, To Err Is Human, did not comment on surgery-associated deaths, injuries, or near misses. One of the major reasons for silence on this topic is related to the absence of comprehensive investigations into the processes involved in surgical care and, as a result, there was no mechanism to track them.Citation1 Among surgical errors, one major one is wrong-site surgery (WSS). By definition, WSS encompasses surgery performed on the wrong side or site of the body, a wrong surgical procedure performed, and surgery performed on the wrong patient.Citation2 The Joint Commission has expanded the definition of WSS by describing it as a sentinel event, defined as an “unexpected occurrence involving death or serious physical or psychological injuries or the risk thereof.” According to the Joint Commission, WSS is the third highest occurring event in the healthcare system.Citation3 To date, WSS constitutes a potential problem in the healthcare system that adds a massive economic, social, and professional burden and requires further attention.
WRONG-SITE SURGERY: KNOWING THE MAGNITUDE OF THE PROBLEM
WSS incidence rates range substantially from 0.09 to 4.5 per 10,000 operations in the US.Citation4 WSS has been surveyed comprehensively in the US. According to the Joint Commission’s 2022 report on sentinel events, WSS is the fourth most significant preventable problem in the healthcare field.Citation5
WSS is a source of critique of the practice of surgery worldwide, including in high-income countries with state-of-the-art healthcare systems. Unfortunately, even these systems witness such unsafe care practices. Although it can be argued that the magnitude of WSS is greater in low-resource settings but underdocumented, WSS remains a system failure with a detrimental impact on the wronged patients, the involved healthcare professionals, and the trust of the public in surgical services at large. The fact that WSS remains unaddressed further showcases the magnitude and complexity of the problem.
As these never events occur, they also add a large economic burden on healthcare systems. These surgical never events are costly and add a significant problem that can challenge the sustainability of surgical services. According to a review of medical liability settlements and judgments in the National Practitioner Data Bank, a total of $1.3 billion was recorded in payouts for surgical never events for two decades (1990–2010). Wrong-procedure events were linked to the greatest median payment. According to this data bank, in a span of 20 years, the United States had 2447 wrong procedures, 2413 WSS, and 27 wrong-patient surgeries.Citation5
Even though WSS has not been under the same scrutiny in other parts of the world as in the US, there are still several reports from other continents pointing out the relevance of WSS among never events. Dating from 2006 to 2022, five studies reported WSS in Australia, seven in Europe, and only two in Africa and Asia.Citation6
THE IMPACT OF WRONG-SITE SURGERIES
The impact of WSS is seen in many different aspects and depends on the level of harm done to the patient. An example will illustrate the impact. If a surgeon operated on the wrong leg in the case of a diabetic foot amputation, the impact would be a lifelong handicap, psychological burden, social isolation, and reduced ability to work and earn a living. Given that the amputation of the affected limb would also be needed, the patient would need a pair of prosthetic limbs. While becoming accustomed to the new normal of daily activities, the patient would be at risk of falls and further musculoskeletal or neurovascular injury. In addition, both the physical and the psychosocial constraints of the patient could affect the amount and quality of earnings. This means that although insurance or social protection tend to provide an equivalent to the salary that the person was earning at the time of the WSS, this salary will not increase at the scale of pay raises that the person would receive through experience and good performance in their working environment. If the patient is the sole earner, the situation would further impact the patient’s family.
Furthermore, WSS significantly increases indirect and third-party healthcare expenditures. This involves multiple lawsuits, litigations, and other legal approaches for the compensation for WSS. This may exhaust much of the finances of a hospital system and may lead the physician and the hospital into a cycle of loss. This will further harm not just the healthcare system but also the pay scales of the providers working in the system. The problem will continue to lead to issues that will be largely related to the economic burden that WSS can cause. Meanwhile, patients can also be trapped in a cascade of medicolegal feuds delaying their compensation and therefore their ability to regain a decent standard of living.
CONTRIBUTING FACTORS IN WRONG-SITE SURGERY
To effectively combat WSS, we must identify and address its underlying causes. In his Swiss cheese model of accident causation, British psychologist James Reason proposed that severe safety failures are almost always the result of an accumulation of mistakes that occur frequently in settings (the holes in the cheese) that have significant underlying system faults. In this model, errors made by individuals have catastrophic effects. The inescapable nature of human error and the power of a systems approach to prevent harm by identifying faults early on are also highlighted.Citation7
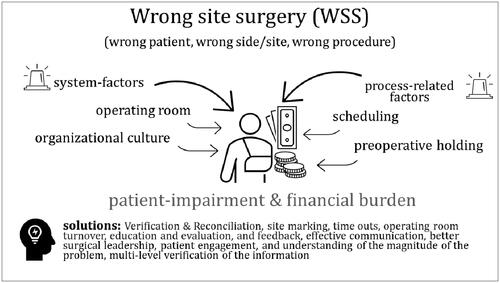
The Joint Commission highlights major factors that contribute to the occurrence of WSS. According to the Joint Commission, the contributing factors can be clustered into four major categories: (1) scheduling, (2) preoperative holding, (3) operating room, and (4) organization culture. The problems pertaining to scheduling are more related to the booking of the patient, documentation, and inappropriate history and examination information. In preoperative holding, the surgical site marking is not done by the surgeon, the information is not tallied with the patient, and inconsistent site markings and inadequate patient verification can all contribute to these errors. In the operating room, issues like distraction, lack of efficient patient hand-offs, and inaccurate information can all cause this problem to happen. For the organization culture, it is mainly an issue of surgical leadership that, if not practiced well or if there is a lack of engagement in care, can further lead to bigger problems.Citation8
Another report on patient safety and quality suggests that the reasons for WSS can be categorized as system factors or process factors. The system factors involve the healthcare system, the efficiency in care, environment safety, diligence of surgical team members, following of the protocols, and organizational structure. Errors or low-quality practices in the system can cause WSS. On the other hand, at the process level, it is said that inadequate patient assessment or care planning, miscommunication with the care team, noncompliance, and failure in effective communication can add to the problem.Citation9 Individual bias, noise, language barriers, workload, extreme emotions, work pressure, status differences, and hierarchies are considered the most important obstacles to effective surgical team communication.Citation10
FEASIBLE SOLUTIONS TO MITIGATE WRONG-SITE SURGERIES
It has been emphasized that WSS can be controlled by taking the right measures. Multiple guidelines show the feasibility of following certain steps that can control the burden. To achieve optimal surgical care, it is important to follow the protocols. The set of protocols and steps not only helps in achieving the right care but also helps in mitigating any errors, including WSS. Strict adherence to established safety protocols is nonnegotiable. Surgeons and their teams must diligently follow procedures such as marking the surgical site, confirming patient identity, and conducting time-outs before commencing surgery. Regular training and ongoing education programs should be provided to ensure that all healthcare professionals remain updated on best practices.
The Joint Commission initiated a project of a universal protocol, a set of standard steps that can reduce errors and make surgical practices safer. According to this protocol, there is a preprocedure step in which the patient is verified; the type and site of surgery are rechecked; relevant documentation is seen; any attached diagnostic, radiological, or other investigations are checked; and any required samples, blood products, or devices used in care are evaluated. This step alone can help address the problem at many levels. In the second step, there is a marking of the procedure site that involves the direct involvement of the physician who oversees the process, and in the last step, a standardized time-out is followed. Active communication is encouraged at every level.Citation11
In another recommendation by Patient Safety and Quality Healthcare, it was mentioned that there are multiple crucial processes that, if carefully addressed, can help mitigate the problem of WSS. The phases are the following: scheduling, verification and reconciliation, site marking, time-outs, operating room turnover, organizational commitment, education and evaluation, and feedback (). These steps correspond to action goals that can be achieved if these phases are correctly followed and carried out properly.Citation12
Table 1. Overview of the steps to mitigate wrong-site surgery, proposed by Patient Safety and Quality Healthcare
The potential solutions discussed by the Joint Commission and Patient Safety and Quality Healthcare have multiple overlaps. The main core idea involves effective communication, a better understanding of the possible errors, and ways to intervene so that errors can be reduced. An overview of solutions combined with the contributing factors to WSS is presented in .
Figure 1. Schematic overview of the contributing factors and the potential solutions for wrong-site surgery.
We should also take advantage of emerging technology to prevent never events. The StartBox Patient Safety SystemCitation13 is an example of an innovative technology evaluated for its effectiveness in preventing WSS among almost 500 orthopedic surgeries. The system consists of a mobile software application, a safety-engineered blade delivery kit, and a data reporting tool. It facilitates improved communication among surgical teams, patients, and care providers through standardized procedures and documentation. The StartBox System ensures accuracy through features such as audio recordings of planned procedures, color-coded blade delivery kits for site identification, real-time error alerts, and secure cloud-based storage of patient data. A study of the system found no occurrences of WSS, while the system did not hinder patient workflow or cause delays or technical difficulties during surgical time-outs or blade release.Citation4
It is important to understand that special steps may be needed that require an active understanding of the issue and the use of various tools and ways to achieve optimal care. There is evidence that suggests ways to lessen the burden of WSS. This involves effective communication, better surgical leadership, patient engagement, sufficient understanding of the magnitude of the problem, and multi-level verification of the information. A paper suggested that active participation of surgical teams that involves operating room briefings can reduce WSS.Citation14
It is common knowledge that the use of surgical safety checklists can reduce the burden of WSS. It is known that in many surgical services, there are multiple professionals involved in care, especially if it is a high-volume setting. In that scenario, it is quite difficult for the team leader to track and assess the distinct duties of healthcare professionals from different disciplines. The best way to mitigate errors in those settings is to follow the surgical safety checklists that can ensure a safer surgical practice and can reduce errors.Citation15
Communication breakdowns are often at the core of WSS cases. Surgeons, anesthesiologists, nurses, and support staff must foster a culture of open communication, where concerns about patient identification, procedure details, and site verification are actively discussed and resolved. Emphasizing effective interprofessional collaboration and creating clear lines of communication will promote a shared responsibility for patient safety.
Preventing WSS also requires a cultural shift within healthcare organizations. A culture of safety must be ingrained at all levels, from leadership to frontline staff. This includes creating an environment where reporting near misses and adverse events is encouraged, without fear of retribution. By fostering a blame-free culture, we can uncover vulnerabilities, learn from mistakes, and implement systemic improvements to prevent future errors.
CONCLUSION
WSS, classified as a never event, inflicts severe repercussions on patients’ lives while also imposing significant economic burdens. To mitigate the occurrence of WSS, a multifaceted approach is needed that encompasses various strategies. These include identifying and preventing potential errors, improving communication channels, reinforcing preoperative processes, strictly adhering to safety protocols, cultivating a safety-oriented culture, and harnessing the benefits of emerging technologies. By diligently pursuing these measures, we can create a future in which instances of WSS are exceedingly rare.
Disclosure statement
The authors report no funding or conflicts of interest.
- Agency for Healthcare Research and Quality. Medical Errors: The Scope of the Problem. Fact sheet. 2023.
- Carayon P, Schultz K, Hundt AS. Righting wrong site surgery. Jt Comm J Qual Saf. 2004;30(7):405–410. doi:10.1016/s1549-3741(04)30046-8.
- Joint Commission. Special report! Helpful solutions for meeting the 2006 National Patient Safety goals. Jt Com Perspect Pat Safety. 2005;5(8):1–15.
- Gloystein DM, Heiges BA, Schwartz DG, DeVine JG, Spratt D. Innovative technology system to prevent wrong site surgery and capture near misses: a multi-center review of 487 cases. Front Surg. 2020;7:563337. doi:10.3389/fsurg.2020.563337.
- Mehtsun WT, Ibrahim AM, Diener-West M, Pronovost PJ, Makary MA. Surgical never events in the United States. Surgery. 2013;153(4):465–472. doi:10.1016/j.surg.2012.10.005.
- O’Bryan E, Pollock M, Joseph S. Comparing the sterility and visibility of surgical marking pens available in Australia. ANZ J Surg. 2019;89(9):1114–1118. doi:10.1111/ans.15153.
- Agency for Healthcare Research and Quality. Systems Approach. 2019. Assessed May 9, 2023. https://psnet.ahrq.gov/primer/systems-approach.
- Joint Commission identifies 29 main causes of wrong-site surgery, offers solution. Becker’s ASC Review, June 30, 2011. https://www.beckersasc.com/asc-accreditation-and-patient-safety/joint-commission-identifies-29-main-causes-of-wrong-site-surgery-offers-solutions.html.
- Mulloy DF, Hughes RG. Wrong-site surgery: a preventable medical error. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- Oyediran OO, Olafare OH, Kolawole IO, Ayandiran EO, Ojo IO, Fajemilehin BR. The pattern of communication and teamwork among operating theatre personnel in a state of a developing country. Nurse Media J Nurs. 2022;12(2):160–171. doi:10.14710/nmjn.v12i2.45933.
- The Joint Commission. The Universal Protocol. Accessed March 8, 2020. https://www.jointcommission.org/-/media/tjc/documents/standards/universal-protocol/up_poster1pdf.pdf.
- Hospitals collaborate to prevent wrong-site surgery. Patient Safety & Quality Healthcare, September 29, 2010. https://www.psqh.com/analysis/hospitals-collaborate-to-prevent-wrong-site-surgery/.
- StartBox. Accessed June 18, 2023. https://www.startboxor.com/
- Makary MA, Mukherjee A, Sexton BJ, et al. Operating room briefings and wrong-site surgery. J Am Coll Surg. 2007;204(2):236–243. doi:10.1016/j.jamcollsurg.2006.10.018.
- Panesar SS, Noble DJ, Mirza SB, et al. Can the surgical checklist reduce the risk of wrong site surgery in orthopaedics? Can the checklist help? Supporting evidence from analysis of a national patient incident reporting system. J Orthop Surg Res. 2011;6(1):18. doi:10.1186/1749-799X-6-18.
