Abstract
Background
In March 2022, a COVID-19 outbreak disrupted the global supply of iodine contrast media (ICM). Healthcare systems implemented contrast-saving strategies to maintain their remaining ICM supplies. This study sought to determine the impact of contrast shortage on the incidence of contrast-associated acute kidney injury (CA-AKI).
Methods
This was a retrospective study of 265 patients undergoing 278 percutaneous coronary interventions (PCI) during 4-month periods prior to (9/1/2021 to 12/31/2021) and during (5/1/2022 to 8/31/2022) contrast shortage at a single center. The primary endpoint was the incidence of CA-AKI between study periods.
Results
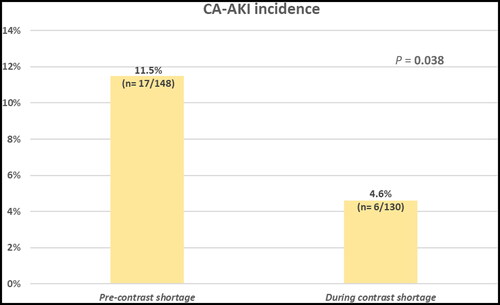
A total of 148 and 130 PCIs were performed before and during contrast shortage, respectively. The incidence of CA-AKI significantly decreased from 11.5% to 4.6% during contrast shortage (P = 0.04). During the shortage, average contrast volume per PCI was significantly lower (123 ± 62 mL vs 88 ± 46 mL, P < 0.001), while coronary imaging was significantly higher (34.3% vs 50%, P = 0.009) compared to preshortage. All-cause mortality at discharge was comparable between study periods (2.8% vs 3.3%, respectively; P = 0.90).
Conclusion
The scarcity of ICM for PCI procedures in this single-center experience was associated with a significant increase in the utilization of intravascular imaging and a significant reduction in CA-AKI.
In March 2022, the Chinese government implemented a “Zero-COVID” strategy to contain a COVID-19 outbreak in Shanghai, China.Citation1 The lockdown of more than 26 million people resulted in a wide-ranging economic and social burden.Citation2 General Electric (GE) Healthcare, one of the world’s largest suppliers of iodinated contrast media (ICM), operating primarily in Shanghai, was forced to cease production of Omnipaque (iohexol) ICM, resulting in a disruption of international supply chains and ultimately a significant global shortage of ICM.Citation3 Other companies producing ICM could not rapidly ramp up production to meet the global healthcare demand. GE Healthcare had resumed and scaled up production in July 2022, but ICM availability was expected to remain limited as the factory continued to restore global supply.Citation4
In many hospitals across the United States, the use of contrast-enhanced imaging had declined by as much as 95%,Citation5 leaving physicians torn between the desire to provide optimal patient care and the need to maintain the minimal remaining supplies of ICM. To address this shortage, affected hospitals implemented risk-mitigating strategies, novel workflows, and system-level actions through multidisciplinary and collaborative efforts. While most elective contrast-enhanced imaging exams were deferred until further notice, no interruptions were planned for cardiac catheterization procedures. With a finite supply, interventionalists resorted to various contrast-saving strategies such as diluting iodinated contrast, repackaging larger-volume single-use vials of ICM into several smaller aliquots, and using gadolinium, carbon dioxide (CO2), and air as alternative contrast agents during noncoronary evaluations and interventions.Citation6 Moreover, interventionalists increased the application of epicardial coronary pressure measurement techniques (“coronary physiology”) including instantaneous wave-free ration and fractional flow reserve. These coronary physiology assessments measure the coronary artery pressure drop across epicardial coronary lesions with the ultimate practical clinical application of identifying significant stenoses that compromise myocardial perfusion.
Contrast-associated acute kidney injury (CA-AKI) is defined as an impairment of renal function resulting from the administration of ICM, in the absence of any other cause.Citation7 Iodinated contrast medium was first reported to cause acute kidney injury in 1954,Citation8 and the condition is now well known by physicians. In the National Cardiovascular Data Registry (NCDR) Cath-PCI, 985,737 patients undergoing elective and urgent percutaneous coronary intervention (PCI) were reviewed; the incidence of CA-AKI was 7.1%.Citation9 In a systematic review of more than 1.2 million patients undergoing PCI, the pooled incidence of CA-AKI was 12.8%Citation10; thus, the overall incidence of post-PCI CA-AKI varies widely between studies due to the different study populations and the use of different AKI definitions.Citation11 Although PCI-related complications have decreased over time, tangible risks remain.
The aim of this study was to investigate the incidence, characteristics, and outcomes of CA-AKI during contrast shortage in comparison to an earlier period.
METHODS
Study population
The institutional review board for Baylor Scott & White Health approved this study. Given the retrospective nature of the study, informed consent was waived.
This was a retrospective analysis of data recorded at a single PCI center at Baylor Scott & White The Heart Hospital, Plano, Texas, USA. A total of 1200 consecutive adult patients undergoing PCI during 4-month periods in 2021 and 2022 were included. We compared a 4-month period during the contrast shortage (May 1, 2022 to August 31, 2022) with a historical 4-month period prior to the contrast shortage (September 1, 2021 to December 31, 2021). We did not include the first 4-month period of 2022 (January 1, 2022 to April 30, 2022) because our PCI center experienced varying degrees of stock depletion during the first weeks of contrast shortage. May 2022 was the first full month of significant contrast shortage at our facility, and contrast levels were restored to normal by the end of August 2022. We excluded patients with same-day discharge (n = 780), missing baseline (n = 6) or post-PCI (n = 131) serum creatinine (SCr), and patients on dialysis at the time of their PCI (n = 18). The final analytic cohort included 265 subjects, of whom 11 (4.2%) underwent 2 PCIs and 1 (0.4%) underwent 3 PCIs, with a total of 278 PCIs performed during the study periods.
Study design
Baseline SCr was defined as the preprocedural SCr value measured within 14 days prior to PCI; if multiple values were measured within 14 days, the most recent one was recorded. Postprocedural peak creatinine was defined as the highest SCr level within 72 hours following PCI. Comorbidities including hypertension, diabetes mellitus, chronic kidney disease (CKD), congestive heart failure, previous coronary artery disease (including history of acute myocardial infarction, PCI, or coronary artery bypass grafting), and previous cerebrovascular disease were recorded through patient electronic medical records (Epic electronic health record, Epic Systems). CKD was defined as a pre–contrast point estimate of glomerular filtration rate (GFR) <60 mL/min/1.73 m2 reported by stages, with an unverified assumption that the baseline creatinine represented the stable chronicity required for 3 months according to the KDIGO classification.Citation12 Indications for PCI were classified as acute coronary syndrome and non–acute coronary syndrome.
The primary endpoint was the incidence of AKI post-PCI compared between the two study periods. CA-AKI was defined as an increase in SCr of ≥0.3 mg/dL (26.5 µmol/L) above the baseline within 72 hours of contrast administration, or the initiation of new dialysis after PCI,Citation13 modified for a definition agnostic to urine output.
Secondary endpoints included the change in all-cause in-hospital mortality, mean amount of contrast volume per procedure (mL), mean fluoroscopy time per procedure (recorded in minutes), coronary imaging, physiology, and coronary atherectomy between the periods before and during contrast shortage.
Statistical analysis
Continuous data are presented as mean ± standard deviation or median (interquartile range) as appropriate, and categorical variables as proportion, unless otherwise specified. Comparisons across periods were made using t tests or Mann Whitney U tests for numerical outcomes and chi-square tests for categorical outcomes. Because of the small sample size for the subset of patients who developed CA-AKI, comparison was performed using Mann-Whitney U tests for numerical variables and Fisher exact tests for categorical variables. All analyses were performed at the 0.05 significance level using SAS Enterprise Guide 8.2 with SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
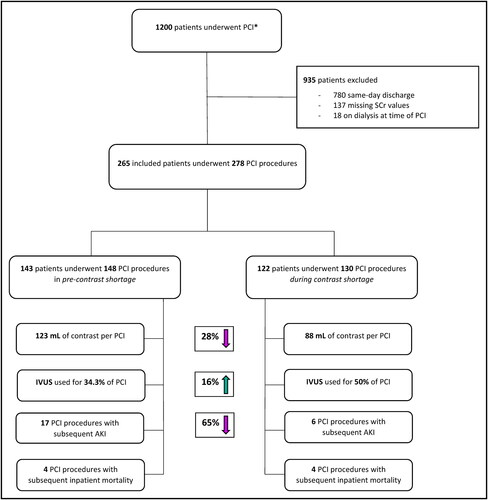
A total of 265 patients underwent 278 PCIs over two distinct 4-month periods in 2021 and 2022 at Baylor Scott & White The Heart Hospital Plano, consisting of 148 PCIs pre–contrast shortage (September 1, 2021–December 31, 2021) and 130 PCIs during contrast shortage (May 1, 2022–August 31, 2022) ().
Figure 1. Flow chart. *A multivessel PCI in the same access session was considered a single PCI (episode). More than one PCI on the same patient, implying at least two sessions, regardless of the number of vessels treated during each, was considered as two or three different PCIs (episodes). Five patients contributed to more than two PCIs each. AKI indicates acute kidney injury; CA-AKI, contrast-associated acute kidney injury; PCI, percutaneous coronary intervention; SCr, serum creatinine.
Baseline characteristics of the overall population stratified by time periods
There were no significant differences in baseline characteristics or comorbidities between the two study groups (). Overall, the mean age was 71 ± 12 years, with the majority being men (62.3%). Hypertension (86%) was the predominant comorbidity. Common comorbidities were congestive heart failure (48.3%), diabetes mellitus (41.9%), prior acute myocardial infarction (32.1%), prior PCI (42.3%), prior coronary artery bypass grafting (17.4%), and prior cerebrovascular disease (29.1%). Overall mean baseline SCr was 1.2 ± 0.5, and 33.3% of patients presented with CKD stage ≥3 (GFR <60 mL/min/1.73 m2) at baseline, assuming the baseline SCr represented chronic stability, of whom 13.6% were stage 3a (GFR: 45–59 mL/min/1.73 m2), 13.3% stage 3b (GFR: 30–44 mL/min/1.73 m2), 6.1% stage 4 (GFR: 15–29 mL/min/1.73 m2), and 0.36% stage 5 (GFR <15 mL/min/1.73 m2). Overall, mean baseline hemoglobin was 12.8 ± 2.2 g/dL. The mean left ventricular ejection fraction was 45.6 ± 16.3%. Acute coronary syndrome (74.7%) was the most common indication for PCI. Cardiovascular instability (defined as persistent ischemic signs, acute heart failure symptoms, hemodynamic instability, ventricular arrythmia, or cardiogenic shock) was present in 63.8% of patients at admission. In the overall sample, 4.5% of the patients were thought to be in a cardiogenic shock, but when considering only patients without prolonged, nonresponsive hypotension or shock, 2.3% were categorized as having hemodynamic instability. Circulatory support was required in 12.1% of patients on admission, of whom 3.4% received pharmacological support and 8.7% received temporary mechanical circulatory support, including left-sided percutaneous left ventricular assist device (i.e., Impella, 5.6%), intra-aortic balloon pump (1.9%), and extracorporeal membrane oxygenation (1.1%).
Table 1. Baseline characteristics of patients who underwent PCI stratified according to the 2021 (pre-shortage) and 2022 (during shortage) periods
Procedural characteristics of the overall population stratified by time periods
A total of 18,174 mL of contrast was used during the pre–contrast shortage to perform 148 PCI procedures and 11,466 mL of contrast was used during contrast shortage to perform 130 PCI procedures. This corresponds to a significant reduction of 28.3% lower average contrast used per procedure performed during contrast shortage (123 ± 62 mL vs 88 ± 46 mL, P < 0.001) (). Fluoroscopic procedure time during contrast shortage was not statistically different (19.3 ± 13.3 min vs 21.7 ± 12.8 min, respectively; P = 0.07). There was a significant increase in the use of intravascular ultrasound (IVUS) following stent implantation during contrast shortage compared to the pre–contrast shortage (50% vs 34.3%, P = 0.009), whereas no differences were found in the use of IVUS prior to stent implantation (56.2% vs 52.8%, P = 0.59). There was comparable use of coronary physiology during contrast shortage (6.15% vs 11.4%, P = 0.13) to guide revascularization. Use of coronary atherectomy before and during contrast shortage was also comparable (10.8% vs 5.7%, P = 0.13) ().
Figure 2. Variation in the average amount of contrast volume (mL) per PCI across entire study months.
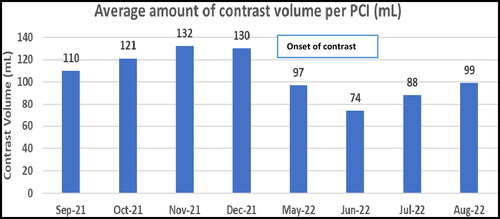
Table 2. Impact of contrast shortage on the angiographic characteristics in patients undergoing PCI
Incidence of AKI following PCI stratified by time periods
The incidence of AKI in patients undergoing PCI significantly decreased from 17 cases (11.5%) in pre–contrast shortage to 6 cases (4.6%) during contrast shortage, P = 0.04 (). None of the patients who developed AKI in either group required dialysis.
Incidence of in-hospital mortality following PCI stratified by time periods
In-hospital mortality following PCI was 3.0% and was comparable in both the pre–contrast shortage and contrast shortage cohorts (2.8% vs 3.3%, respectively; P = 0.90) ().
Table 3. Impact of contrast shortage on the clinical outcomes of all patients who underwent PCI and those who developed AKI after PCI
Baseline characteristics of the patients who developed AKI following PCI stratified by time periods
Baseline characteristics and comorbidities of patients who developed AKI (N = 23) were compared between study periods (). Baseline patient demographics were comparable in both periods, including age, gender, and body mass index. Comorbidities of patients in both cohorts were comparable except for a significantly higher number of patients with a history of diabetes mellitus in the pre–contrast shortage period (). Patients with baseline CKD (GFR <60 mL/min/1.73 m2) were comparable pre–contrast shortage and during contrast shortage (). Moreover, AKI patients in both study periods had a similar clinical presentation at admission, with no significant differences in terms of cardiovascular instability, hemodynamic instability, and cardiogenic shock. There were no significant differences in the use of pharmacological or mechanical circulatory support during PCI between the study periods ().
Table 4. Baseline characteristics of patients who developed CA-AKI following PCI, stratified according the 2021 (pre-shortage) and 2022 (during shortage) periods
Procedural characteristics among patients who developed AKI, stratified by time periods
The procedural characteristics in this subset of patients mirrored those of the overall population, with a trend toward a decrease in the average amount of contrast used per procedure during contrast shortage, whereas fluoroscopy time, IVUS use, and total atherectomy tended to increase during contrast shortage. Coronary physiology was not performed in this subset of patients. However, none of these findings was statistically significant due to the low number of patients who developed AKI in both study periods ().
Incidence of in-hospital mortality in patients who developed AKI following PCI
Among the patients who developed AKI-CA, there were insufficient events to assess for differences in mortality (4/17, 24%, vs 1/6, 17%), particularly in light of competing risks of mortality ().
DISCUSSION
The COVID-19–related lockdown in Shanghai left hospitals across the world scrambling to obtain ICM. Several studies have described the impact of contrast shortage on routine imaging and noncardiac interventions.Citation14,Citation15 However, to our knowledge, this is the first single-center experience evaluating the effects of contrast shortage on CA-AKI following PCI.
Contrast conservation strategies during a global supply shortage
To effectively address this global health challenge, hospitals across the nation followed recommendations from the American College of Radiology Committee on Drugs and Contrast Media regarding best practices for preserving ICM.Citation16 Our facility managed to conserve ICM (28.3% reduction in mean contrast volume per PCI during contrast shortage) while still performing timely and effective cardiac procedures, thus ensuring good patient care during these challenging times. At our facility, an institution-wide committee of cardiologists, cardiovascular surgeons, and radiologists was formed to establish risk-mitigating plans, implement new processes, and communicate at the institution and healthcare system level. Several adjunctive techniques including IVUS for coronary imaging and coronary physiology were being increasingly used at our institution during contrast shortage in a trial to reduce the use of ICM while still optimizing PCI results as part of implementing an ultra-low-contrast PCI protocol to further conserve contrast. As a result, the total number of PCI performed at our facility dropped by only 4.7% during contrast shortage (615 pre–contrast shortage vs 586 during contrast shortage), demonstrating that it is possible to weather a supply chain crisis by implementing multiple strategies at the institution and procedural level.
Impact of ICM shortage on the incidence of CA-AKI and in-hospital mortality
The key finding of this study was the significant decrease in the incidence of CA-AKI among patients who underwent PCI during contrast shortage compared to those who underwent PCI before contrast shortage. Remarkably, CA-AKI percentage per se was relatively high in the pre–contrast shortage period compared to the national incidence of AKI post-PCI (11.5% vs 7.8% in the last published US AKI rate post-PCI by the NCDR CathPCICitation17). However, we should highlight the fact that we have excluded all patients with missing baseline (N = 6) or postprocedural (N = 131) SCr levels, and those with same-day discharge (N = 780), which may have overestimated the true incidence of CA-AKI. Indeed, in most cases, the increase in SCr during CA-AKI occurs within the first 3 days after ICM administration and peaks within 3 to 5 daysCitation18; therefore, it is important to monitor SCr levels in appropriate patients for at least 72 hours after ICM administration.Citation19
The incidence of CA-AKI is highly affected by several patient-related and contrast-related risk factors (cf. ). The most important patient-related factor is baseline SCr; several multivariable analyses have shown that CKD, defined as baseline creatinine of 1.5 mg/dL or GFR <60 mL/min/1.73 m2, is an independent risk predictor for CA-AKI.Citation20,Citation21 In the current study, the proportion of patients with CKD was similar in both study periods, and the mean SCr values at baseline were comparable. Other risk factors, including diabetes mellitus, anemia, and advanced age have been associated with CA-AKI.Citation22,Citation23 The results of the overall cohort evaluating variable demographic (age, gender, body mass index) and clinical (hypertension, diabetes mellitus, and anemia) patient characteristics showed no significant differences between study periods. However, a history of diabetes mellitus was statistically higher in patients who developed AKI pre–contrast shortage compared to those who developed AKI during contrast shortage ().
Among contrast-related factors, both contrast volume and contrast osmolarity may influence the incidence of CA-AKI. In a study by Amit et al, which evaluated more than 1.3 million patients undergoing PCI, higher ICM volumes were associated with higher rates of AKI.Citation24 In addition, Richard et al showed that the use of an ICM volume of <100 mL during PCI was associated with the lowest rates of CA-AKI.Citation25 High osmolality and viscosity increased the risk for CA-AKI, while low osmolality and viscosity were associated with less nephrotoxicity.Citation26,Citation27
Although we observed comparable patient-related risk factors in both study periods, statistically significant disparities were found between pre- and during contrast shortage for CA-AKI incidence. This finding could be explained by the concomitant significant decrease in the mean amount of contrast volume during contrast shortage.
The use of high doses of ICM is considered the most important contrast-related risk factor for in-hospital mortality after PCI. In a study by Giancarlo et al, patients who received a higher ICM dose had a more complicated clinical course and higher in-hospital mortality than patients who received a low ICM dose.Citation28 This contrasts with another study demonstrating a weak impact of high ICM dose at the time of PCI on in-hospital mortality.Citation29 In the current study, despite having a significant reduction in the amount of contrast volume during contrast shortage, in-hospital mortality was comparable between study periods, calling into question the independent association of contrast volume with in-hospital mortality after PCI.
Among postprocedural risk factors, CA-AKI has shown to be associated with poor short-term outcomes, with an overall incidence of in-hospital mortality of 20.2% in patients who develop CA-AKI post PCI.Citation30 These findings are consistent with our results, as in-hospital mortality following PCI was significantly higher in patients who developed AKI compared to those who did not develop AKI (odds ratio = 17, 95% confidence interval (3.5, 80), P = 0.001).
LIMITATIONS
One limitation of this study, resulting from the short time interval between restoration of contrast volume and the time of the analysis, was that prolonged follow-up of patients was not possible. Therefore, a systematic evaluation is needed to ensure that the conservative strategies used to address the ICM shortage did not result in long-term adverse outcomes. Another limitation is that, because of the small number of patients who developed CA-AKI, we could not perform multivariable analysis to further investigate the association between the different risk factors and the occurrence of CA-AKI.
CONCLUSION
This is the first single-center experience evaluating the incidence, characteristics, and outcomes of post-PCI AKI during the global contrast shortage crisis. Contrast conservation strategies outlined by reduced contrast PCI techniques at our institution resulted in the use of lower amounts of contrast volume and increased use of coronary imaging, with a trend toward greater use of coronary physiology and a trend toward longer fluoroscopy time. This led to a significant reduction in the incidence of CA-AKI during contrast shortage compared with pre–contrast shortage, with comparable in-hospital mortality rates. Lessons learned from this experience should translate into more effective use of ICM, even beyond the period of contrast shortage.
ACKNOWLEDGMENTS
The authors would like to thank Satish and Yasmin Gupta for their unrestricted gift to Baylor Scott & White The Heart Hospital – Plano, for fostering the environment to conduct this research.
Disclosure statement/Funding
Karim Al-Azizi is a proctor and consultant for Edwards LifeSciences, a consultant and advisory board member for Medtronic, a consultant for Boston Scientific, and on a speaker’s bureau for Philips. Srinivasa Potluri is an advisory board member, proctor, and speaker for Medtronic, Boston Scientific, Abbott, and Cordis Proctor and a speaker for Edwards, Terumo, and AstraZeneca. Molly Szerlip is a proctor, speaker, and consultant for Edwards LifeSciences; an advisory board member, consultant, and proctor for Abbott Vascular; on the steering committee for Medtronic; and a speaker and consultant for Boston Scientific. Michael Mack is a trial co–principal investigator for Abbott and for Edwards Life Sciences and a trial study chair for Medtronic—all uncompensated. The other authors report no disclosures.
- Khan N, Qi L, Zhai K. Omicron puts China’s zero-Covid strategy to its toughest test. Wall Street Journal . January 12, 2022. https://www.wsj.com/articles/omicron-puts-chinas-zero-covid-strategy-to-its-toughest-test-11642003293
- Galbraith A, Stanway D. Shanghai locks down as COVID surges in China’s financial hub. Reuters, March 29, 2022. https://www.reuters.com/world/china/shanghai-reports-record-asymptomatic-covid-cases-lockdowns-begin-2022-03-28/.
- Reuters. Shanghai factories scramble to reopen as COVID lockdown lingers. Reuters, April 29, 2022. https://www.reuters.com/world/china/shanghai-factories-scramble-reopen-covid-lockdown-lingers-2022-04-29/.
- GE. GE Healthcare update on iodinated contrast media. July 15, 2022. https://www.ge.com/news/press-releases/ge-healthcare-update-on-iodinated-contrast-media.
- Eibschutz LS, Gholamrezanezhad A. How low can we go? Strategies and recommendations to combat the iodinated contrast shortage. Emerg Radiol. 2022;29(5):925–928. doi:10.1007/s10140-022-02077-7.
- Allen LM, Shechtel J, Frederick-Dyer K, et al. Rapid response to the acute iodinated contrast shortage during the Covid-19 pandemic: single-institution experience. J Am Coll Radiol. 2022;19(7):836–840. doi:10.1016/j.jacr.2022.05.005.
- Laville M, Juillard L. Contrast-induced acute kidney injury: how should at-risk patients be identified and managed? J Nephrol. 2010;23(4):387–398.
- Bartels ED, Brun GC, Gammeltoft A, Gjørup PA. Acute anuria following intravenous pyelography in a patient with myelomatosis. Acta Med Scand. 1954;150(4):297–302. doi:10.1111/j.0954-6820.1954.tb18632.x.
- Tsai TT, Patel UD, Chang TI, et al. Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the NCDR Cath-PCI registry. JACC Cardiovasc Interv. 2014;7(1):1–9. doi:10.1016/j.jcin.2013.06.016.
- Lun Z, Liu L, Chen G, et al. The global incidence and mortality of contrast-associated acute kidney injury following coronary angiography: a meta-analysis of 1.2 million patients [published correction appears in J Nephrol. 2021 Jun 17]. J Nephrol. 2021;34(5):1479–1489. doi:10.1007/s40620-021-01021-1.
- Chalikias G, Drosos I, Tziakas DN. Contrast-induced acute kidney injury: an update. Cardiovasc Drugs Ther. 2016;30(2):215–228. doi:10.1007/s10557-015-6635-0.
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–S266.
- Kellum JA, Lameire N, Aspelin P, et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2(1):1–138. doi:10.1038/kisup.2012.1.
- Karout L, Digumarthy SR, Savage C, et al. Low contrast volume protocol in routine chest CT amid the global contrast shortage: a single institution experience. Acad Radiol. 2023;30(12):2913–2920. doi:10.1016/j.acra.2023.03.020.
- Almallouhi E, Sattur M, Lajthia O, et al. Contrast conservation measures during the global iohexol contrast shortage crisis did not affect stroke thrombectomy outcomes. J Neurointerv Surg. 2023;15(e1):e76–e78. doi:10.1136/jnis-2022-019210.
- American College of Radiology. Statement from the ACR Committee on Drugs and Contrast Media. Updated May 13, 2022; Accessed November 4, 2022. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Contrast-Media-Shortage.
- CathPCI Registry. Accessed October 31, 2022. https://cvquality.acc.org/NCDR-Home/registries/hospital-registries/cathpci-registry.
- McCullough PA. Contrast-induced acute kidney injury [published correction appears in J Am Coll Cardiol. 2008 Jun 3;51(22): 2197]. J Am Coll Cardiol. 2008;51(15):1419–1428. doi:10.1016/j.jacc.2007.12.035.
- Solomon R, Deray G, Consensus Panel for CIN. How to prevent contrast-induced nephropathy and manage risk patients: practical recommendations. Kidney Int Suppl. 2006;69(100):S51–S53. doi:10.1038/sj.ki.5000375.
- McCullough PA, Wolyn R, Rocher LL, Levin RN, O’Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103(5):368–375. doi:10.1016/s0002-9343(97)00150-2.
- Stacul F, van der Molen AJ, Reimer P, et al. Contrast induced nephropathy: updated ESUR Contrast Media Safety Committee guidelines. Eur Radiol. 2011;21(12):2527–2541. doi:10.1007/s00330-011-2225-0.
- Ohno Y, Maekawa Y, Miyata H, et al. Impact of periprocedural bleeding on incidence of contrast-induced acute kidney injury in patients treated with percutaneous coronary intervention. J Am Coll Cardiol. 2013;62(14):1260–1266. doi:10.1016/j.jacc.2013.03.086.
- Mandurino-Mirizzi A, Kajana V, Cornara S, et al. Elevated serum uric acid is a predictor of contrast associated acute kidney injury in patient with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Nutr Metab Cardiovasc Dis. 2021;31(7):2140–2143. doi:10.1016/j.numecd.2021.04.002.
- Amin AP, Bach RG, Caruso ML, Kennedy KF, Spertus JA. Association of variation in contrast volume with acute kidney injury in patients undergoing percutaneous coronary intervention. JAMA Cardiol. 2017;2(9):1007–1012. doi:10.1001/jamacardio.2017.2156.
- Owen RJ, Hiremath S, Myers A, Fraser-Hill M, Barrett BJ. Canadian Association of Radiologists consensus guidelines for the prevention of contrast-induced nephropathy: update 2012. Can Assoc Radiol J. 2014;65(2):96–105. doi:10.1016/j.carj.2012.11.002.
- Seeliger E, Sendeski M, Rihal CS, Persson PB. Contrast-induced kidney injury: mechanisms, risk factors, and prevention. Eur Heart J. 2012;33(16):2007–2015. doi:10.1093/eurheartj/ehr494.
- Barrett BJ, Carlisle EJ. Metaanalysis of the relative nephrotoxicity of high- and low-osmolality iodinated contrast media. Radiology. 1993;188(1):171–178. doi:10.1148/radiology.188.1.8511292.
- Marenzi G, Assanelli E, Campodonico J, et al. Contrast volume during primary percutaneous coronary intervention and subsequent contrast-induced nephropathy and mortality. Ann Intern Med. 2009;150(3):170–177. doi:10.7326/0003-4819-150-3-200902030-00006.
- Kooiman J, Seth M, Nallamothu BK, Heung M, Humes D, Gurm HS. Association between acute kidney injury and in-hospital mortality in patients undergoing percutaneous coronary interventions. Circ Cardiovasc Interv. 2015;8(6):e002212. doi:10.1161/CIRCINTERVENTIONS.114.002212.
- Weisbord SD, Chen H, Stone RA, et al. Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. J Am Soc Nephrol. 2006;17(10):2871–2877. doi:10.1681/ASN.2006030301.