ABSTRACT
We report a 12-year-old girl who presented with bilateral granulomatous anterior uveitis accompanied by boggy arthritis of knee and ankle joints, intermittent fever, and nodular skin rash. She was diagnosed with sporadic Blau syndrome (early-onset sarcoidosis) based on above clinical signs and presence of non-necrotising granuloma on iris biopsy. DNA sequencing revealed a previously unreported heterozygous mutation consisting of a G>A transition in exon 4 of the NOD2 gene. This resulted in a glutamic acid to lysine substitution in helical domain 2 of the nucleotide binding and oligomerization (NACHT) region, possibly reducing efficiency of auto-inhibition in NOD2 signaling. Interestingly, the ocular inflammation resolved completely following therapeutic vitrectomy in both eyes whereas the systemic symptoms of fever and arthritis continued to wax and wane while on treatment with oral methotrexate and corticosteroids.
INTRODUCTION
Blau syndrome (BS), first described by Blau and Jabs,Citation1-Citation2 is a rare, autosomal dominant, monogenic autoinflammtory syndrome caused by mutation(s) in the NOD2 gene. Familial BS and its sporadic variant early-onset sarcoidosis (EOS) consist of a triad of dermatitis, arthritis, and uveitis. Ocular manifestations include anterior uveitis, multifocal choroiditis, and panuveitis appearing around 4 years of age.Citation3 Treatment with corticosteroids and immunosuppressive is not always effective and long-term prognosis is unknown.Citation3 We report a case of sporadic BS (EOS) with a novel NOD2 mutation.
CASE DESCRIPTION
A 12-year-old girl presented with sudden, painful defective vision in the right eye since 1 month and decreased vision in the left eye since 3 years. Her best corrected visual acuity (BCVA) was counting fingers and hand movements in the right and left eye respectively. The right eye showed non-granulomatous anterior uveitis with vitreous haemorrhage () and the left eye showed chronic anterior uveitis, multiple iris granuloma, and complicated cataract (-). She suffered from intermittent febrile episodes and a nodular rash over the legs since 3 years of age and painful, boggy swelling of the knee and ankle joints for the past 6 months (). Chest imaging, tuberculin skin test, and anti-nuclear antibodies were negative, serum angiotensin converting enzyme levels were elevated, and ultrasonography of the abdomen revealed hepato-splenomegaly. There was no family history of similar disease. Based on the above history and clinical findings, we diagnosed sporadic BS (EOS).
FIGURE 1. Clinical photographs. (A) Right eye: keratic precipitates (white arrows), iris nodules (red arrow). (B) Left eye: posterior synechiae (white arrow), complicated cataract (black arrow), iris nodule (red arrow). (C) Left eye: iris nodules (red arrow), magnified image. (D) Swelling of knee joints.
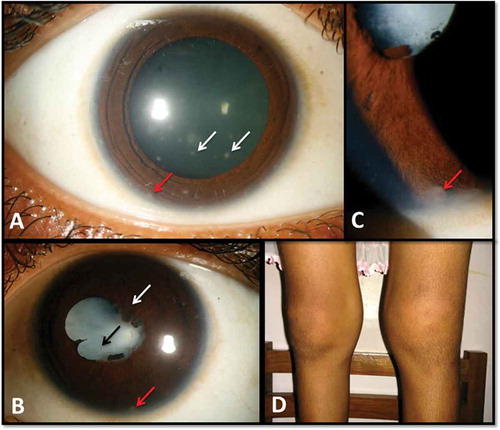
The patient was treated with oral steroids and methotrexate. She underwent pars plana vitrectomy with anterior chamber (AC) tap in the right eye and iris granuloma biopsy followed by cataract surgery and therapeutic vitrectomy in the left eye. At final follow-up after 8 months, her BCVA was 20/30 and 20/25 in the right and left eye respectively with no active ocular inflammation. Her nodular skin rash also resolved but the systemic inflammatory signs of fever and arthritis continued to wax and wane while on treatment with oral corticosteroids and methotrexate. Cyto-smears from the right eye AC tap revealed dispersed histiocytes and foam cells. Left eye showed non-necrotizing granuloma corresponding to the iris nodule (-).
FIGURE 2. Histopathology and DNA sequencing. (A) Left eye iris nodule biopsy: non-caseating granuloma, histiocytes (white arrow), lymphocytes (red arrow). (B) Right eye vitreous: histiocytes (white arrows). (C) G>A transition in exon 4 of NOD2. (D) Multiple sequence alignment of E667 in helical domain 2 of NACHT in NOD2.
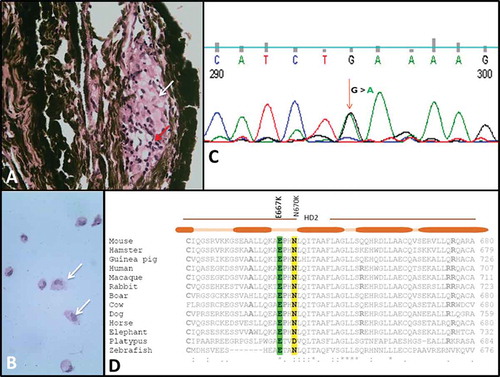
DNA sequencing of peripheral blood mononuclear cells identified a previously unreported heterozygous mutation consisting of a G>A transition in exon 4 of the NOD2 gene (). The mutation resulted in a glutamic acid to lysine substitution at position 667 of the coding sequence (E667K). The E667K mutation was located in helical domain 2 of the nucleotide binding and oligomerization (NACHT) region, which is required for NOD2 funtion. The E667K is in close proximity to another mutation in the NACHT region, an asparagine to lysine substitution at position 670 (N670K) that was shown to be associated with EOS.Citation4 E667 is conserved across species and therefore seems to be a critical residue (). It is likely that E667K inhibits, or at least reduces, the efficiency of auto-inhibition of NOD2 signaling, similar to N670K.
DISCUSSION
NOD2 plays a key role in innate immune response. It exists in an auto-inhibitory state due to an intramolecular interaction between the leucine-rich repeat region and the NACHT domains and undergoes activation following ligand binding.Citation5 NOD2 mutation in BS was thought to cause uncontrolled ligand-independent downstream signaling and subsequent transcription of inflammatory genes.Citation5 Conversely, it has recently been demonstrated that spontaneous activation does not occur and there is decreased intracellular signaling and cytokine production in muramyl dipeptide-activated pathwayin BS.Citation6
Interestingly, the first symptom in our case was intermittent febrile episodes (extra-triad manifestation) with a relatively late onset of arthritis. The presence of vitreous hemorrhage remains unexplained since no vascular abnormalities were seen. Notwithstanding, therapeutic vitrectomy helped in complete resolution of ocular inflammation even though the same could not be achieved for systemic inflammation with standard medical therapy.
DECLARATION OF INTEREST
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
ACKNOWLEDGMENT
We gratefully thank Dr Aparna Rao and Dr Vivek Warkad, LV Prasad Eye Institute, Bhubaneswar for their role in the surgical care in this patient.
FUNDING
Support was received from the Medical Research Council.
REFERENCES
- Blau EB. Familial granulomatous arthritis, iritis, and rash. J Pediatr. 1985; 107(5):689–693.
- Jabs DA, Houk JL, Bias WB, et al. Familial granulomatous synovitis, uveitis, and cranial neuropathies. Am J Med. 1985;78:801–804.
- Rose CD, Wouters CH, Meiorin S, et al. Pediatric granulomatous arthritis: an international registry. Arthritis Rheum. 2006;54:3337–3344.
- Kanazawa N, Okafuji I, Kambe N, et al. Early-onset sarcoidosis and CARD15 mutations with constitutive nuclear factor-kappaB activation: common genetic etiology with Blau syndrome. Blood. 2005;105(3):1195–1197.
- Chamaillard M, Philpott D, Girardin SE, et al. Gene-environment interaction modulated by allelic heterogeneity in inflammatory diseases. Proc Natl Acad Sci U S A. 2003;100(6):3455–3460.
- Dugan J, Griffiths E, Snow P, et al. Blau syndrome–associated nod2 mutation alters expression of full-length nod2 and limits responses to muramyl dipeptide in knock-in mice. J Immunol. 2015; 194:349–357.
