ABSTRACT
Purpose: To find immunomediator combinations which could sensitively indicate keratoconus progression.
Methods: Tear samples of 42 patients with keratoconus were collected at baseline and at the end of a one-year follow-up. The concentrations of 13 mediators were measured by CBA. Based on Pentacam HR examination, eyes were divided into a non-progressive and a progressive group.
Results: At the end of the follow-up, significant differences were observed in the release of IFNγ, IL-13, IL-17A, CCL5, MMP-13 and PAI-1 between the two groups. Changes in five Pentacam parameters correlated positively with changes in IFNγ, IL-13, IL-17A, CXCL8, CCL5, TIMP-1 and t-PA. We found that tear level of IL-13 in combination with NGF can predict the progression of keratoconus with 100% specificity and 80% sensitivity.
Conclusion: The findings of our longitudinal study may underscore the importance of NGF and IL-13 tear levels in the prediction of keratoconus progression.
Keratoconus (KC) is a progressive ectatic corneal disorder with heterogeneous clinical severity and varying progression.Citation1 Citation2 Its prevalence is around 1:375 in the general population highlighting its public health importance.Citation3 The etiology of this visually debilitating disease is not yet known in detail, but recent studies suggest that the pathogenesis is related to a combination of genetic, biomechanical, biochemical and environmental risk factors including inflammation, oxidative stress, and allergy.Citation4–16
Altered levels of various cytokines, enzymes, regulatory and growth factors, and diagnostic markers of inflammation and tissue injury have been found in the tears or in the cornea of patients with keratoconus, pointing to the crucial role of the immune system in the pathogenesis of keratoconus.Citation6,Citation11–14 These include proinflammatory cytokines (tumor necrosis factor (TNF), interleukin (IL)-1β, IL-6), inflammatory chemokines (CXCL8, CCL5), inflammatory mediators (IL-12, interferon (IFN)-γ, IL-17), the anti-inflammatory cytokine IL-10, cytokines associated with allergy development (IL-4, IL-13), enzymes and their co-factors associated with tissue remodeling (matrix metalloproteinases (MMPs), tissue inhibitor of metalloproteinase-1 (TIMP-1), cathepsin B). Various growth factors, other enzymes, enzyme inhibitors, cellular proteins which can serve as diagnostic markers in the context of cellular and tissue injury or inflammation were also described, including epidermal growth factor (EGF), vascular endothelial growth factor (VEGF); insulin-growth factors (IGFs), nerve growth factor (NGF), lipocalins, lipophilins, phospholipase A2, cystatins, albumin, type I and type II keratins, lactoferrin, Prolactin-Induced Protein, α-fibrinogen, α1-antitrypsin; apolipoprotein A1 (ApoA1), lysozyme C, zinc-α2-glycoprotein (ZAG), metabolic enzymes (e.g. GAPDH), different immunoglobulins (IgA, IgG1, and the κ-isotype of the Ig light chains) and the polymeric immunoglobulin transport receptor (pIgR/PIGR).Citation4–8,10−12,Citation15–35 Disease specific changes in these molecular markers can be of diagnostic value in keratoconus.Citation32
To the best of our knowledge, there are no studies examining these mediators in the tear fluid to predict the progression of the disease. However, early detection of progression in keratoconus is of high importance because early identification of the progressive nature of the disease allows early treatment to reduce the risk of visual impairment. If tear biomarker profiling could predict the progression of keratoconus earlier than the parameters used nowadays, it would be ideal for clinical application. Corneal collagen crosslinking (CXL) proved to be effective in halting the progression of keratoconus by several studies.Citation36–39 It has been reported that the best results of CXL are obtained in progressive KC patients treated in early stage.Citation40 This possible treatment underscores the challenge of identifying the appropriate patients as early as possible.
In the present study, our goals were to determine the concentrations of 13 different immune mediators in tear samples of patients with keratoconus and to correlate the changes of these mediators to the changes of Pentacam parameters which are used to detect progression. The tested multifunctional mediators were chosen as representative molecules that are associated with corneal degradation in KC. The MMP-9, MMP-13 are collagenases produced by various cell types during tissue remodeling, involving injuries and tissue repair. Their functions are regulated directly or indirectly by inhibitors (e.g. TIMP-1) or activator proteases and their respective activators and inhibitors (e.g. t-PA, plasminogen activator inhibitor (PAI-1)). The other investigated mediators are associated with different type of inflammatory processes involving the Th1 or type 1 innate lymphoid cell (ILC1) produced mediator: IFN-γ which take part in the classical inflammatory macrophage activation. Pro-inflammatory cytokines and chemokines produced by various innate inflammatory cell types: IL-6, CXCL8/IL-8, CCL5/RANTES. Cytokines mediating the resolution of the inflammation: IL-13, IL-10 produced by Th2 cells or ILC2 cells. IL-17α is an inflammatory cytokine produced by Th17 cells or ILC3 cells normally mediating neutrophil granulocyte rich inflammation and other antimicrobial defense processes in the epithelial tissues. NGF takes part in regulatory and healing mechanisms. Tear immunomediator levels and Pentacam parameters were determined at baseline and at the end of the one-year follow-up period. We aimed to find combinations of mediators which can better predict the progression of the disease than single mediators. The real clinical importance and relevance of our study lies in its ability to tell from baseline mediator levels whether keratoconus is likely to progress in the future. This can lead to an earlier treatment of at-risk patients and therefore a better visual acuity preserved in these patients. To the best of our knowledge, this is the first longitudinal study evaluating mediators in order to predict the progression of keratoconus.
Patients and Methods
Subjects and Clinical Examinations
We performed an observational cohort study involving well-characterized keratoconus patients recruited from the Department of Ophthalmology, Faculty of Medicine, University of Debrecen, Hungary. Keratoconus was diagnosed upon the presence of one or more of the following clinical signs: central or paracentral stromal thinning of the cornea, conical protrusion, Fleischer’s ring, Vogt’s striae by slit-lamp examination, and topographic changes.Citation41 Exclusion criteria included the existence of active inflammatory or infectious systemic or ocular disease (including atopic dermatitis), history of chronic, abnormal eye rubbing, and current treatment with systemic or local anti-inflammatory drugs. Patients who were pregnant or lactating during the course of the study and eyes with a history of ocular surgery (including corneal cross-linking) or trauma were also excluded. Altogether, 42 keratoconic patients (mean (SD) age 36.4 (12.3), range 15–68 years) were enrolled in the study. Both eyes of each participant underwent repeated ophthalmological evaluation, including clinical history, automated kerato-refractometry (KR-8900; Topcon Co, Tokyo, Japan), uncorrected and corrected distance visual acuity determinations, slit-lamp biomicroscopy (under low illumination to avoid reflex tearing), Rotating Scheimpflug tomography (Pentacam HR, Oculus Optikgeräte GmbH, Wetzlar, Germany). Non-stimulated tear sample collection with glass capillaries was performed at baseline and at completion of a one-year follow-up period. We involved only one eye of each patient at baseline that met all inclusion but no exclusion criteria, except for patients with one progressive and one non-progressive keratoconic eye, in which case one eye was enrolled into the non-progressive, and the other eye into the progressive group.
The study protocol was approved by the Regional and Institutional Research Ethics Committee of the University of Debrecen (DEOEC-RKEB/IKEB 3313–2011). Each patient was informed of the nature of the study and gave informed consent in writing. The tenets of the Declaration of Helsinki were followed in all procedures during the study.
Pentacam Measurements
All eyes of the involved 42 keratoconus patients were examined with a Pentacam HR (Oculus GmBH, Wetzlar, software version 1.16r26 and 1.17r139) without the application of any eye drops at baseline and at the end of follow-up to determine the progressive nature of the disease. Three sequential scans were taken of each eye by the same trained examiner. The detailed subscription of the method can be found in our previous publication.Citation31 The following parameters were exported to Microsoft Excel (Microsoft Corp, Redmond, Washington): Holladay equivalent keratometry values in the flat (K1) and steep (K2) meridian; maximal keratometry of the front surface (Kmax Front); corneal astigmatism of the front surface (Astig); corneal thickness at the thinnest point of the cornea (Pachy Min); Keratoconus Index (KI); Central Keratoconus Index (CKI); and Belin-Ambrósio deviation index (D-index). Keratoconus progression was defined as an increase in K2 and/or Kmax and/or in astigmatism of 1.00 diopter (D) or more in the prior 12 months.Citation41–44 Grade of KC was defined as mild if the steepest keratometric reading K2 was <45 diopters, moderate if K2 was between 45 and 52D, and severe if K2 was >52D.Citation23
Tear Collection and Analysis
A detailed description of non-traumatic tear collection using micro-capillary tubes from the inferior meniscus and the handling of the samples can be found in our previous publication.Citation31 Tear collections were carried out at the same time of the day, between 8.00 and 9.30 a.m. at the baseline visit and at the end of the one-year follow-up. We calculated tear volumes from the length of the tear column in the tube on a micrometer scale.
The tear samples were analyzed for IL-6, IL-10, IL-13, IL-17A, CXCL8/IL-8, CCL5/RANTES, IFN-gamma, MMP-9, MMP-13, TIMP-1, NGF, t-PA, and PAI-1 concentrations using the Cytometric Bead Array method. Combined FlowCytomix Simplex Kits were used with the appropriate FlowCytomix™ Basic Kit, with minor modifications to the manufacturer’s instructions (eBioscience, Bender Med Systems GmbH, Vienna, Austria). A detailed description can be found in our previous publication.Citation45 The subsequent detection limits were as follows: IL-6: 1.2 pg/ml; IL-10: 1.9 pg/ml; IL-13: 4.5 pg/ml; IL-17A: 2.5 pg/ml; IFNγ: 1.6 pg/ml; CXCL8 (IL-8): 0.5 pg/ml; CCL5 (RANTES): 25 pg/ml; MMP-9: 95 pg/ml; MMP-13: 50 pg/ml; TIMP-1: 28 pg/ml; NGF: 126.8 pg/ml; t-PA: 4.8 pg/ml; and PAI-1: 13.5 pg/ml.Citation45
Statistical Analysis
If both eyes of the patient were in the same group, i.e. non-progressive or progressive, then we only included one randomly selected eye. Eye selection was based on generating random values using Microsoft Excel set to produce numeric indicators with equal probabilities for either eye. We included automatically the fellow, keratoconic eye of the patient if the other eye had a history of an invasive procedure (CXL, transplantation) and was therefore subject to exclusion from the study. We included both eyes if one was progressive and the other was non-progressive in nature.
Mediator concentration and Pentacam parameter variables were inspected for distribution shape and transformed to improve normality if necessary. The quantities of mediators released into tears were calculated using concentrations (pg/μl) and tear volumes (μl) collected over 2 minutes.
First we analyzed the Pentacam data at baseline and end of follow-up to determine the progression of the disease, and to be able to classify the eyes of the 42 patients into two disease groups, namely the non-progressive and the progressive groups. Then we determined statistical correlations between the changes in the levels of tear mediators and changes in Pentacam parameters during follow-up using linear regression.
As a third step, the predictive performance of tear fluid mediators was evaluated using logistic regression. All possible pairs of mediator concentration variables, and similarly of release level variables, were formed and used as continuous explanatory variables complete with an interaction term between them, in models with observed progression as the binary outcome. After each model fit, observations were sorted on predicted probability and dichotomized for model diagnostic purposes such that the number of predicted cases of progression above the cut should equal the number of observed cases. Observations with predicted probability of at least 50% were used as predicted positives in evaluating the system for sensitivity, specificity, and positive and negative predicted values (PPV and NPV, respectively). For reference, the procedure was repeated using Pentacam parameter pairs as explanatory variables. Comparison was based on a non-parametric approach evaluating the areas (AUC) under the receiver operating characteristic curves (ROC) of each Pentacam parameter model against those of each of the best two mediator release models. For these models, cutoffs were not set on the measurement scales of the predictor variables. Instead, model-predicted probabilities greater than or equal to 50% were regarded as positive predictions (progressive disease).
Results
Demographic and Pentacam Data at Baseline and End of Follow-up
A total 45 eyes of 42 patients (mean (SD) age 36.4 (12.3), range 15–68 years) were enrolled in the study. At the end of follow-up, eyes were classified into a non-progressive keratoconus group (29 eyes) and a progressive keratoconus group (16 eyes) determined by Pentacam parameters. Generally, the study only involved one eye of each patient, except in three patients where one eye was in the non-progressive, and the other in the progressive group. At baseline, KC grade in the non-progressive vs progressive group was mild in 4 vs 0, moderate in 18 vs 8, and severe in 7 vs 8 eyes. After one year, these counts were 5 vs 0, 17 vs 8, and 7 vs 8, respectively.
Demographic and Pentacam data of patients in the non-progressive and in the progressive keratoconus groups at baseline and at the end of follow-up are presented in and . At baseline, there were significant differences in K2 (p = .035), Kmax (p = .014), D-index (p = .016) but not in any other Pentacam values including astigmatism (p > .05). At the end of follow-up, there were significant differences in K2 (p = .007), Kmax (p = .0008), D-index (p = .0396) and also in corneal astigmatism of the front surface (p = .027).
Table 1. Demographic and Pentacam data of participants at baseline
Table 2. Pentacam data of participants at end of follow-up
Tear Fluid Mediator Levels in the Two Groups during Follow-up
At baseline, there were no significant differences between the two groups in the release or concentration of mediators (all p values>.05).
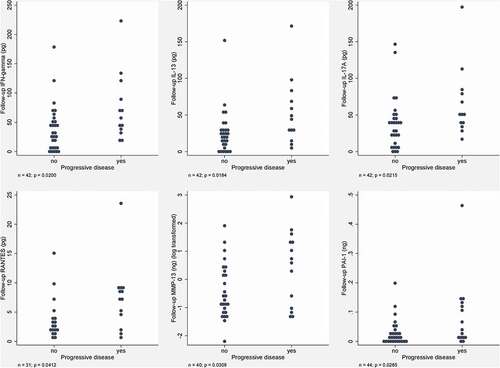
At the end of follow-up, there were significant differences in the release of IFNγ, IL-13, IL-17A, CCL5, MMP-13, and PAI-1 between the two groups (, ); however, no significant differences in mediator concentrations between the two groups were observed.
Table 3. Significant (p value is <0.05) differences in released mediator quantities (pg) between the two groups at the end of follow-up
Figure 1. Significant (p value is <0.05) differences in released mediator quantities (pg) between the two groups at the end of follow-up eye counts are presented as (n); INF?, interferon gamma; IL, interleukin; CCL5, chemokine (C–C motif) ligand 5 or RANTES (regulated on activation, normal T cell expressed and secreted); MMP-13, matrix metalloproteinase-13; PAI-1, plasminogen activator inhibitor-1.
Correlations between Changes in Tear Mediator Levels and Changes in Pentacam Parameters during Follow-up
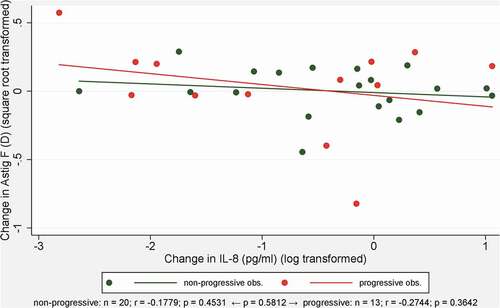
Significant differences were observed between the progressive and the non-progressive group in the way changes in the levels of the different tear mediators were correlated with changes in Pentacam parameters, as shown in and and . Changes in five out of eight analyzed Pentacam parameters correlated positively with changes in IFNγ, IL-13, IL-17A, CXCL8, CCL5, TIMP-1, and t-PA.
Table 4. Significant, groupwise heterogeneous correlations between baseline to follow-up changes in the levels of different tear mediators and changes in Pentacam parameters
Figure 2. Significant, groupwise heterogeneous correlations between baseline to follow-up changes in the levels of interleukin-17 (IL-17/A) concentration (pg/ml) and changes in corneal astigmatism of the front surface (Astig F) measured with Pentacam between the non-progressive (n=29 eyes) and the progressive (n=16 eyes) group (one representative example of Table 4 for significant correlation).
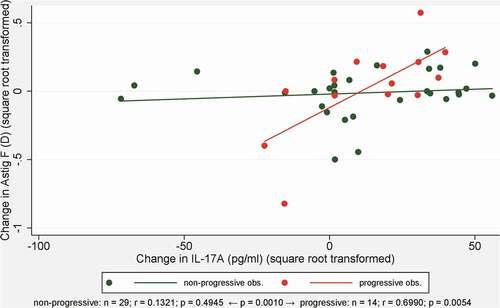
Figure 3. Non-significant correlation between baseline to follow-up changes in the levels of interleukin-8 (IL-8) concentration (pg/ml) and changes in corneal astigmatism of the front surface (Astig F) measured with Pentacam between the non-progressive (n=20 eyes) and the progressive (n=13 eyes) group (one representative example of Table 4 for non-significant correlation).
Significance of Mediator Pairs in Tear Fluid in the Prediction of Progressive Disease in Keratoconus
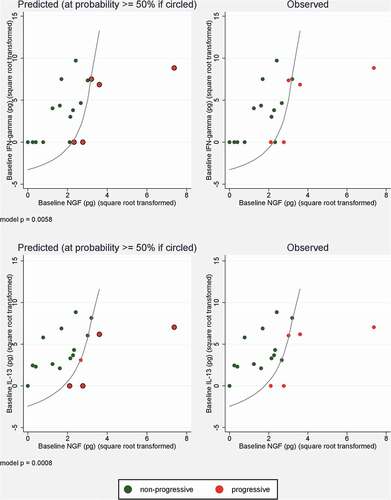
Of all possible baseline mediator pairings, those showing reasonable predictive power for keratoconus progression included IFNγ with NGF and IL-13 with NGF released quantities.
High released levels of NGF, and moderately high levels of NGF coupled with low levels of IFNγ or IL-13, were associated with increased odds of progression. The plane defined by these variable pairs was possible to separate, to a certain degree, into non-progressive and a progressive area (). The model based on released quantities of IFNγ with NGF had a reasonable specificity and NPV but a moderate sensitivity and PPV estimate (ROC AUC = 0.9385), while the one based on released IL-13 and NGF (AUC = 0.9692) had very high specificity and PPV with high NPV and reasonable sensitivity ().
Table 5. Diagnostic performance indicators of pairs of baseline tear mediator release levels in predicting keratoconus progression
Figure 4. Logistic regression-predicted and observed progression of keratoconus in relation to baseline released quantities of tear mediator pairs (INF?+NGF, IL-13+NGF). Curves indicate model-derived location of probability threshold ensuring equal number of predicted and observed progressive cases. INF?, gamma interferon; IL-13, interleukin-13; NGF, nerve growth factor.
Pentacam Parameter Pairs in the Prediction of Progressive Disease in Keratoconus
The predictive performance indicators of Pentacam parameter pairs were similar to or poorer than (especially in relation to IL-13 and NGF) those estimated for mediator release pairs (). AUC values ranged from 0.3692 to 0.7385 and were found significantly smaller in 40 out of 56 comparative relations with the two models based on mediator release.
Table 6. Diagnostic performance indicators of pairs of baseline Pentacam data to predict keratoconus progression
Discussion
Several studies have revealed that inflammatory factors play a key role in the pathomechanism of keratoconus and several associations were revealed between the levels of inflammatory mediators and the severity of the disease.Citation10,Citation28,Citation29 Tear mediator profile as a noninvasive biomarker of keratoconus can act as a prognostic biomarker and may aid in the timely treatment of this heterogeneous disease.Citation6,Citation32,Citation34,Citation46 To the best of our knowledge, there is no longitudinal study evaluating mediators in order to predict the true progression of keratoconus.
The aim of this study was to determine mediators which sensitively indicate keratoconus progression. The real clinical importance and relevance of our study lies in the ability to tell from current mediator levels whether keratoconus is likely to progress in the future. This dictates an approach where baseline levels, strictly without their follow-up counterparts, are the explanatory variables and KC progression is a binary outcome. Another interesting aspect is the possibility of interaction between various mediators: it might be that no single mediator is strongly predictive on its own, but a combination where high levels of one are accompanied by low levels of another is. Our findings suggest that certain mediators could predict the progression of KC and have outstanding roles in the pathomechanism of KC. Future directions may include targeting these inflammatory factors in the management of KC to restore the dysregulated inflammation in KC pathogenesis. This opens the potential to explore anti-inflammatory strategies to either halt or delay the progression of KC.
In this study, first we evaluated the baseline concentrations and release of mediators in the two patient groups (stable KC eyes vs progressive KC eyes) and found no difference. Tear fluid is easily accessible and may indicate the status of the ocular surface; however, dynamic changes in the levels of various mediators could also be related to the lacrimal gland function. In our experience, even eyes suffering from the same disease may produce variable amounts of tears within a set sampling time, which is due to the large variations in individual sensitivity and variability of the disease stages resulting in various diluting effects. Differences in tear flow rate and consequently in sample volumes must be taken into consideration. Hence, we not only measured the concentrations of mediators, but also calculated the rates of their release into tears collected within 2 minutes.
Second, we analyzed the differences after one year and found that there were significant differences between the two groups in the release, but not the concentration, of IFNγ, IL-13, IL-17A, CCL5, MMP-13 and PAI-1. This means that not only the concentration itself but the amount of the tear secretion changes with time and may have an impact on the levels of mediators. It has to be later investigated whether it is the inflammation generated by disease progression that is responsible for an increase in tear production or, alternatively, keratoconus is an essentially inflammatory condition and it is the progression that generates an increase in the production or release of different mediators.
Third, we presented positive correlations between molecular profiles and KC progression built on the differences between two visits in the levels of mediators (IFNγ, IL-13, IL-17A, CXCL8, CCL5, TIMP-1 and t-PA) and five Pentacam parameters (K1, Kmax, Astig, KI, CKI). The change in astigmatism and the KI correlates the strongest with mediator changes, namely IFNγ, IL-13, IL-17A and CXCL8, CCL5, and t-PA. In addition to K2, Kmax and D-index, astigmatism was the parameter that changed significantly between the two patient groups from baseline to the end of follow-up. Interestingly, the increase in astigmatism during follow-up correlates positively with the increase of three cytokines (IFNγ, IL-13, IL-17A).
Fourth, in this study we revealed a significant role of mediator pairs in tears in the prediction of the progressive disease course in keratoconus. As far as we know, this is the first study aiming at the prediction of keratoconus with the help of tear mediators. In our study, IFNγ with NGF and IL-13 with NGF released quantities showed reasonable predictive power for keratoconus progression: high levels of NGF, and moderately high levels of NGF coupled with low IFNγ or IL-13 were associated with keratoconus progression. Based on the models, prediction based on released IL-13 and NGF seems to be more useful because it has 100% specificity and PPV with 93% NPV and reasonable (80%) sensitivity (). Martínez-Abad et alCitation47 designed a predictive model for keratoconus progression based on refractive, topographic and aberrometric changes. Our findings suggest that compared to Pentacam parameters, mediator release levels might have at least similar, but potentially greater, predictive power for keratoconus progression. This is to be fully clarified by future research specifically targeted at the question.
Karaca et alCitation48 used the serum neutrophil-to-lymphocyte ratio (NLR) to predict keratoconus progression, based on its predictive property of systemic inflammation in several diseases. Although NLR is simple and inexpensive, it was found to predict the presence of KC progression with only 79% sensitivity and 81% specificity.Citation48 We think that tear collection is a non-traumatic and noninvasive procedure and tears can truly reflect the local pathological disorders such as keratoconus.
Based on the findings of our study, IFNγ, IL-13, IL-17A, CXCL8, CCL5, MMP-13, TIMP-1 t-PA, PAI-1 and NGF seem to have a crucial function in the progression of keratoconus; as to prediction, IL-13 and NGF have the most important role. We found a significant positive association in tears of patients with KC between CCL5, MMP-13 and NGF levels and several topographic data and showed that IL-13, CXCL8, CCL5 and MMP-13 have different effects on the severity of disease depending on age.Citation28 Age influences the immune response and also the progressive nature of keratoconus. We revealed significant differences in the release of IL-13, CCL5, MMP-13 and also IFNγ, IL-17A and PAI-1 between the two groups showing their pivotal role not only in the pathomechanism of KC but in the course of progression. Produced by Th1 cells, IFNγ is associated with autoinflammatory and autoimmune diseases. Increased IL-13 and IFNγ concentrations were measured in the tears of KC patients.Citation29,Citation30 Patients with keratoconus had significantly higher levels of IFNγ (mean: 33.3 (SD 7.6) pg/ml) compared with control subjects (mean: 23.0 (SD 4.7) pg/ml) (P = .0001), without making any correction with tear flow rate, which is in line with our concentration levels (mean: 38.7 (SD 23.9) pg/ml) in the non-progressive group and 43.6 (SD 4.8) pg/ml in the progressive group at the end of the follow-up).Citation29 Jun et alCitation23 showed significantly increased tear levels of IL-17 and decreased IL-13 and CCL5 in keratoconus compared to normal controls. IL-17 is the principal proinflammatory cytokine produced by T helper 17 cells and is associated with many chronic inflammatory conditions.Citation14 Based on our study IFNγ with NGF and IL-13 with NGF are predictive indicators of keratoconus progression. IFNγ has a broad range of biological functions and IL-13 is produced by Th2 cells, as IL-10. IL-13 plays crucial roles in amplification of the Th2 response which is dampened in keratoconus. The contrary is found in allergic conjunctivitis or vernal and atopic keratoconjunctivitis.Citation23 Balasubramanian et alCitation26 detected increased expression of IL-10 and IL-6 and classified keratoconus as an inflammatory disease. Interestingly, we could not reveal any differences in the tear levels of IL-6 or IL-10 between the progressive and non-progressive groups, although Lema et alCitation4,Citation5 observed increased levels of IL-6, while Sorkhabi et alCitation29 measured decreased levels of IL-10 in keratoconic tears. IL-6 increases chemokine activation, including CXCL8 (which was higher in our study in the progressive group), and IL-10 inhibits IL-6. These results suggest that because of cytokine interaction, many of them have a role in the pathomechanism but are less significantly involved in the progression and only some mediators can be used as progression predictors. The goal of our study is to identify some of these biomarkers that contribute to KC progression in order to recognize the progression of this visually debilitating disease earlier. Higher levels of NGF existing in tears of patients with progressive keratoconus is in line with the well-known neural sensitizing role of this neuromediator.Citation49 In our previous study we revealed not only disease specific mediators in the tear fluid of patients, but we confirmed several associations between the levels of mediators and the severity of keratoconus, including NGF.Citation28 Lacrimal glands are known to produce, release, and be responsive to NGF, and NGF is a normal constituent of the tear film.Citation50 Correlation between NGF tear levels and the severity of corneal damage in the tear film of patients with dry eye disease was establishedCitation51; moreover, NGF promotes corneal healing in physiologic and pathologic conditions, and it has been shown that corneal injuries induce an increase in local NGF and NGF receptors capable of stimulating epithelial healing.Citation52 These observations suggest that NGF may be involved in local tissue damage. The inadequate balance between pro-inflammatory cytokines, proteolytic enzymes, protease inhibitors, inflammatory modulators and antioxidants may lead to increased activity of metalloproteinases.Citation10 Several studies have investigated the role of proteolytic enzymes such as MMPs in KC. MMPs are involved in the degradation of extracellular matrix or activation of cellular apoptosis. In keratoconus, the cornea expresses elevated levels of MMP‐13 and the levels of MMP‐1, ‐3, ‐7 and MMP‐13 are also increased in the tear fluid.Citation19,Citation26 The enzymatic activity of MMPs depends on TIMP, which is a potent inhibitor of MMPs. Pouliquen et alCitation53 suggested that cytokines, including CXCL8, might regulate the protease cascade including the plasmin system, involving t-PA and PAI, and also MMPs, which would lead to extracellular matrix changes in keratoconus.
Since keratoconus progression results in severe irreversible loss of visual acuity, it indicates a relevant need to find biomarkers which promptly and sensitively indicate disease progression in the future in order to select the progressive forms in time for CXL treatment.Citation47 The limitations of this study are that it cannot exclude the possibility of other mediators being involved in the progression of the keratoconic cornea, and that the identification of the source and activity of the mediators has not been investigated. Tear samples are crucial in understanding the molecular mechanism of the progression process and the multiplex platform is perfectly suited for the detection of biomarkers from tear samples. Ideally, because the progression of the disease will stop at a point, which can be accompanied by an alteration in mediator levels including a decrease of IL-13/NGF, it would have been useful to monitor the tears of eyes with progressive keratoconus without any treatment for a longer time to find out about the time of progression arrest; however, in this study the vast majority of the eyes with progressive keratoconus needed and received CXL treatment, making such long-term observations largely unavailable. Despite these limitations, it is important to indicate that our results underline the fact that many mediators are involved in the complex mechanisms of keratoconus progression. It remains to be determined in further studies which of these mediators or any others are principal in predicting keratoconus progression.
To conclude, our study confirms that different mediators in the tear fluid could predict the progression of keratoconus and may underscore the important roles of NGF and IL-13, which together seem to be useful in the prediction of the progression with 100% specificity and PPV, 93% NPV, and 80% sensitivity. Locally released mediators serve as additional proof for considering corneal cross-linking treatment in an attempt to stop KC progression. As next steps, the critical levels of these mediators and the precise roles of the identified predictive biomarkers need to be defined on a larger cohort to reveal their potential use not only as diagnostic markers but as therapeutic targets as well. The potential roles of biomarkers include being components in a KC progression predictive system combined with other input variables such as Pentacam parameters, age, or other data available in a real-life clinical setting.
Disclosure of interest
No potential conflict of interest was reported by the authors.
The data that support the findings of this study are available from the corresponding author, [MF], upon reasonable request.
Additional information
Funding
References
- Krachmer JH, Eagle RC, Belin MD. Keratoconus and related non-inflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28:293–322. doi:https://doi.org/10.1016/0039-6257(84)90094-8.
- Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi:https://doi.org/10.1016/S0039-6257(97)00119-7.
- Godefrooij DA, de Wit GA, Uiterwaal CS, Imhof SM, Wisse RP, Incidence A-S. Prevalence of Keratoconus: A nationwide registration study. Am J Ophthalmol. 2017;175:169–172. doi:https://doi.org/10.1016/j.ajo.2016.12.015.
- Lema I, Duran JA. Inflammatory molecules in the tears of patients with keratoconus. Ophthalmology. 2005;112:654–659. doi:https://doi.org/10.1016/j.ophtha.2004.11.050.
- Lema I, Sobrino T, Duran JA, Brea D, Diez-Feijoo E. Subclinical keratoconus and inflammatory molecules from tears. British J Ophthalmol. 2009;93:820–824. doi:https://doi.org/10.1136/bjo.2008.144253.
- Ionescu C, Corbu CG, Tanase C, et al. Inflammatory biomarkers profile as microenvironmental expression in Keratoconus. Dis Markers. 2016;2016:1243819. doi:https://doi.org/10.1155/2016/1243819.
- Kenney MC, Chwa M, Atilano SR, et al. Increased levels of catalase and cathepsin V/L2 but decreased TIMP-1 in keratoconus corneas: evidence that oxidative stress plays a role in this disorder. Invest Ophthalmol Vis Sci. 2015;46:823–832. doi:https://doi.org/10.1167/iovs.04-0549.
- Balasubramanian SA, Wasinger VC, Pye DC, Willcox MD. Preliminary identification of differentially expressed tear proteins in keratoconus. Mol Vis. 2013;19:e2124–34.
- Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. Biomed Res Int. 2015;2015:795738. doi:https://doi.org/10.1155/2015/795738.
- Galvis V, Sherwin T, Tello A, Merayo J, Barrera R, Acera A. Keratoconus: an inflammatory disorder? Eye. 2015;29:843–885. doi:https://doi.org/10.1038/eye.2015.63.
- Yenihayat F, Ö A, Kasap M, Akpınar G, Güzel N, Çelik OS. Comparative proteome analysis of the tear samples in patients with low-grade keratoconus. Int Ophthalmol. 2018;38(5):1895–1905. doi:https://doi.org/10.1007/s10792-017-0672-6.
- McKay TB, Hjortdal J, Priyadarsini S, Karamichos D. Acute hypoxia influences collagen and matrix metalloproteinase expression by human keratoconus cells in vitro. PLoS One. 2017;2017:e0176017. doi:https://doi.org/10.1371/journal.pone.0176017.
- McKay TB, Hjortdal J, Sejersen H, Karamichos D. Differential effects of hormones on cellular metabolism in Keratoconus in vitro. Sci Rep. 2017;17:42896. doi:https://doi.org/10.1038/srep42896.
- Wisse RP, Kuiper JJ, Gans R, Imhof S, Radstake TR, Van der Lelij A. Cytokine expression in keratoconus and its corneal microenvironment: A systematic review. Ocul Surf. 2015;13:272–283. doi:https://doi.org/10.1016/j.jtos.2015.04.006.
- Yuksel E, Yalinbas D, Aydin B, Bilgihan K. Keratoconus progression induced by in vitro fertilization treatment. J Refract Surg. 2016;32:60–63. doi:https://doi.org/10.3928/1081597X-20151207-10.
- Shen Y, Han T, Jhanji V, et al. Correlation between corneal topographic, densitometry, and biomechanical parameters in Keratoconus eyes. Transl Vis Sci Technol. 2019;6;8:12. doi:https://doi.org/10.1167/tvst.8.3.12.
- Collier SA. Is the corneal degradation in keratoconus caused by matrix-metalloproteinases? Clin Exp Ophthalmol. 2001;29:340–344. doi:https://doi.org/10.1046/j.1442-9071.2001.d01-17.x.
- Saghizadeh M, Chwa M, Aoki A, et al. Altered expression of growth factors and cytokines in Keratoconus, bullous keratopathy and diabetic corneas. Exp Eye Res. 2001;73:179–189. doi:https://doi.org/10.1006/exer.2001.1028.
- Mackiewicz Z, Määttä M, Stenman M, Konttinen L, Tervo T, Konttinen YT. Collagenolytic proteinases in keratoconus. Cornea. 2006;25:603–610. doi:https://doi.org/10.1097/01.ico.0000208820.32614.00.
- Matthews FJ, Cook SD, Majid MA, Dick AD, Smith VA. Changes in the balance of the tissue inhibitor of matrix metalloproteinases (TIMPs)-1 and −3 may promote keratocyte apoptosis in keratoconus. Exp Eye Res. 2007;84:1125–1134. doi:https://doi.org/10.1016/j.exer.2007.02.013.
- Lema I, Brea D, Rodríguez-González R, Díez-Feijoo E, Sobrino T. Proteomic analysis of the tear film in patients with keratoconus. Mol Vis. 2010;16:2055–2061.
- Pannebaker C, Chandler HL, Nichols JJ. Tear proteomics in keratoconus. Mol Vis. 2010;16:1949–1957.
- Jun AS, Cope L, Speck C, et al. Subnormal cytokine profile in the tear fluid of keratoconus patients. PLoS One. 2011;6:e16437. doi:https://doi.org/10.1371/journal.pone.0016437.
- Acera A, Vecino E, Rodríguez-Agirretxe I, et al. Changes in tear protein profile in keratoconus disease. Eye. 2011;25:1225–1233. doi:https://doi.org/10.1038/eye.2011.105.
- Sakimoto T, Sawa M. Metalloproteinases in corneal diseases: degradation and processing. Cornea. 2012;31(Suppl1):S50–6. doi:https://doi.org/10.1097/ICO.0b013e318269ccd0.
- Balasubramanian SA, Mohan S, Pye DC, Willcox MD. Proteases, proteolysis and inflammatory molecules in the tears of people with keratoconus. Acta Ophthalmol. 2012;90:e303–e309. doi:https://doi.org/10.1111/j.1755-3768.2011.02369.x.
- Balasubramanian SA, Pye DC, Willcox MD. Levels of lactoferrin, secretory IgA and serum albumin in the tear film of people with keratoconus. Exp Eye Res. 2012;96:132–137. doi:https://doi.org/10.1016/j.exer.2011.12.010.
- Kolozsvári BL, Petrovski G, Gogolák P, et al. Association between mediators in the tear fluid and the severity of keratoconus. Ophthalmic Res. 2014;51:46–51. doi:https://doi.org/10.1159/000351626.
- Sorkhabi R, Ghorbanihaghjo A, Taheri N, Ahoor MH. Tear film inflammatory mediators in patients with keratoconus. Int Ophthalmol. 2015;35:467–472. doi:https://doi.org/10.1007/s10792-014-9971-3.
- Shetty R, Ghosh A, Lim RR, et al. Elevated expression of matrix metalloproteinase-9 and inflammatory cytokines in keratoconus patients is inhibited by cyclosporine A. Invest Ophthalmol Vis Sci. 2015;56:738–750. doi:https://doi.org/10.1167/iovs.14-14831.
- Pásztor D, Kolozsvári BL, Csutak A, et al. Scheimpflug imaging parameters associated with tear mediators and bronchial asthma in Keratoconus. J Ophthalmol. 2016;2016:e9392640.
- Nishtala K, Pahuja N, Shetty R, Nuijts RM, Ghosh A. Tear biomarkers for keratoconus. Eye Vis (Lond). 2016;3:e19. 4. doi:https://doi.org/10.1186/s40662-016-0051-9.
- Shetty R, Deshmukh R, Ghosh A, Sethu S, Jayadev C. Altered tear inflammatory profile in Indian keratoconus patients - the 2015 col rangachari award paper. Indian J Ophthalmol. 2017;65:1105–1108. doi:https://doi.org/10.1016/j.jcrs.2011.08.041.
- Sharif R, Bak-Nielsen S, Hjortdal J, Karamichos D. Pathogenesis of Keratoconus: The intriguing therapeutic potential of Prolactin-inducible protein. Prog Retin Eye Res. 2018;67:150–167. doi:https://doi.org/10.1016/j.preteyeres.2018.05.002.
- Sharif R, Bak-Nielsen S, Sejersen H, Ding K, Hjortdal J, Karamichos D. Prolactin-Induced Protein is a novel biomarker for Keratoconus. Exp Eye Res. 2019;179:55–63. doi:https://doi.org/10.1016/j.exer.2018.10.015.
- Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. doi:https://doi.org/10.1016/S0002-9394(02)02220-1.
- Raiskup-Wolf F, Hoyer A, Spoerl E, Pillunat LE. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term results. J Cataract Refract Surg. 2008;34:796–801. doi:https://doi.org/10.1016/j.jcrs.2007.12.039.
- Vinciguerra P, Albè E, Trazza S, Seiler T, Epstein D. Intraoperative and postoperative effects of corneal collagen cross-linking on progressive keratoconus. Arch Ophthalmol. 2009;127:1258–1265. doi:https://doi.org/10.1001/archophthalmol.2009.205.
- Greenstein SA, Fry KL, Hersh MJ, Hersh PS. Higher-order aberrations after corneal collagen crosslinking for keratoconus and corneal ectasia. J Cataract Refract Surg. 2012;38:292–302. doi:https://doi.org/10.1016/j.jcrs.2011.08.041.
- Arora R, Jain P, Goyal JL, Gupta D. Comparative analysis of refractive and topographic changes in early and advanced Keratoconic eyes undergoing corneal collagen crosslinking. Cornea. 2013;32:1359–1364. doi:https://doi.org/10.1097/ICO.0b013e3182a02ddb.
- Rabinowitz YS. Videokeratographic indices to aid in screening for keratoconus. J Refract Surg. 1995;11:371–379.
- De Bernardo M, Capasso L, Lanza M, et al. Long-term results of corneal collagen crosslinking for progressive keratoconus. J Optom. 2015;8:180–186. doi:https://doi.org/10.1016/j.optom.2014.05.006.
- Spadea L, Salvatore S, Verboschi F, Vingolo EM. Corneal collagen cross-linking followed by phacoemulsification with IOL implantation for progressive keratoconus associated with high myopia and cataract. Int Ophthalmol. 2015;35:727–731. doi:https://doi.org/10.1007/s10792-015-0107-1.
- Waszczykowska A, Jurowski P. Two-year accelerated corneal cross-linking outcome in patients with progressive keratoconus. Biomed Res Int. 2015;2015:325157.
- Fodor M, Kolozsvári BL, Petrovski G, et al. Effect of contact lens wear on the release of tear mediators in keratoconus. Eye Contact Lens. 2013;39:147–152. doi:https://doi.org/10.1097/ICL.0b013e318273b35f.
- Wei Y, Gadaria-Rathod N, Epstein S, Asbell P. Tear cytokine profile as a noninvasive biomarker of inflammation for ocular surface diseases: standard operating procedures. Invest Ophthalmol Vis Sci. 2013;54:8327–8336. doi:https://doi.org/10.1167/iovs.13-12132.
- Martínez-Abad A, Piñero DP, Chorro E, Bataille L, Alió JL. Development of a reference model for Keratoconus progression prediction based on characterization of the course of nonsurgically treated cases. Cornea. 2018;37:1497–1505. doi:https://doi.org/10.1097/ICO.0000000000001673.
- Karaca EE, Özmen MC, Ekici F, Yüksel E, Türkoğlu Z. Neutrophil-to-lymphocyte ratio may predict progression in patients with keratoconus. Cornea. 2014;33:1168–1173. doi:https://doi.org/10.1097/ICO.0000000000000260.
- Lee HK, Lee KS, Kim HC, Lee SH, Kim EK. Nerve growth factor concentration and implications in photorefractive keratectomy vs laser in situ keratomileusis. Am J Ophthalmol. 2005;139:965–971. doi:https://doi.org/10.1016/j.ajo.2004.12.051.
- Nguyen DH, Beuerman RW, Thompson HW, DiLoreto DA. Growth factor and neurotrophic factor mRNA in human lacrimal gland. Cornea. 1997;16:192–199.
- Lambiase A, Micera A, Sacchetti M, Cortes M, Mantelli F, Bonini S. Alterations of tear neuromediators in dry eye disease. Arch Ophthalmol. 2011;129:981–986. doi:https://doi.org/10.1001/archophthalmol.2011.200.
- Lambiase A, Manni L, Bonini S, Rama P, Micera A, Aloe L. Nerve growth factor promotes corneal healing: structural, biochemical, and molecular analyses of rat and human corneas. Invest Ophthalmol Vis Sci. 2000;41:1063–1069.
- Pouliquen Y, Bureau J, Mirshahi M, Mirshahi SS, Assouline M, Lorens G. Keratoconus and inflammatory processes. Bull Soc Belge Ophtalmol. 1996;262:25–28.
