ABSTRACT
Purpose: We set out to estimate the prevalence of trachoma and access to water and sanitation in seven suspected-trachoma-endemic districts of northern Congo, surveyed as a single evaluation unit.
Methods: From a complete list of rural villages in the seven districts, we systematically selected 22 with probability proportional to village size. In selected villages, we included all households where there were fewer than 25 in total, or used compact segment sampling to select a group of approximately 20 households by random draw. In each selected household, all consenting residents aged ≥1 year were examined by Global Trachoma Mapping Project-certified trachoma graders, and data collected on household-level access to water and sanitation.
Results: In November and December 2015, 466 households were visited in 22 villages, and 2081 (88%) of 2377 residents of those households were examined. No examined individual had trichiasis. The age-adjusted prevalence of the active trachoma sign trachomatous inflammation—follicular (TF) in 1–9-year-olds was 2.5% (95%CI 0.9–4.5%). Only 39% (95%CI 35–44%) of households had access to an improved source of drinking water. Only 10% (95%CI 7–13%) of households had access to an improved sanitation facility.
Conclusion: Trachoma is not a public health problem in this part of Congo. Access to water and sanitation is inadequate.
Introduction
The fight against blinding diseases is a public health priority for the Republic of the Congo. Political will to prevent visual impairment prompted the establishment of both a National Program to Fight Blindness and a National Program for Onchocerciasis Control.
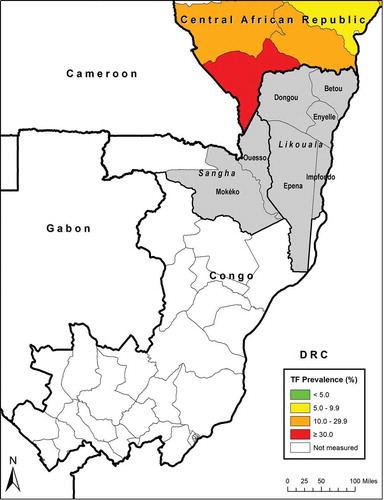
Congo does not feature in the existing scientific literature on trachoma.Citation1 However, the country borders districts of south-western Central African Republic that are reported to be heavily trachoma-endemic.Citation2 Health workers on a 2014 Médecins du Monde mission identified conjunctivitis consistent with active trachoma [unpublished data] in two departments of Congo adjacent to that Central African Republic focus: Sangha and Likouala departments (). Rather than plan widespread trachoma mapping in Congo, it was decided to undertake surveys in areas thought to be at particular risk, with the results to be used to determine whether further investigation in Congo would be needed. (An analogous approach was also undertaken in Democratic Republic of the Congo and Zimbabwe.Citation3,Citation4) The districts identified for mapping were Mokéko and Ouesso of Sangha Department, and Impfondo, Epéna, Dongou, Betou and Enyelle of Likouala Department (). These seven districts were grouped as a single evaluation unit (EU) with an estimated combined population of 189,656.
Trachoma mapping involves the conduct of population-based prevalence surveys, generally in EUs of 100,000–250,000 people.Citation5–Citation7 This allows programmes to identify populations in need of the surgical, medical, educational and environmental interventions of trachoma’s elimination strategy, which is summarized by the acronym SAFECitation8,Citation9: surgery for trachomatous trichiasis,Citation10 antibiotics to clear ocular Chlamydia trachomatis infection,Citation11 and facial cleanlinessCitation12 and environmental improvementCitation13 to reduce transmission of C. trachomatis.
The objectives of this cross-sectional survey were to estimate the prevalence of trachomatous inflammation—follicular (TF)Citation14 in 1–9-year-olds (a proxy for the prevalence of ocular C. trachomatis infectionCitation15,Citation16), to estimate the prevalence of trachomatous trichiasisCitation14 in ≥15-year-olds, and to estimate the prevalence of household-level access to water and sanitation.
Material and methods
Study population and sample size
A single survey was undertaken, covering all seven districts. The base population was all non-urban residents of those districts, as projected to 2015 from the 2007 population census.Citation17 After excluding the urban areas of Betou (estimated population 8188), Ouesso Town (31,882), Impfondo (29,823), and Pokola (18,040), an estimated 101,723 people remained as residents of the EU. We followed the principles and processes of the Global Trachoma Mapping Project (GTMP),Citation18 and determined sample size based on considerations relating to TF, as previously described.Citation19 To estimate with 95% confidence a hypothesized 10% TF prevalence in 1–9-year-olds, using a design effect of 2.65 and desired precision of ±3%, we aimed to examine 1019 children.Citation19 Since census data indicated that Congo households had a mean of 6.9 residents, 27% of whom would be aged 1–9 years,Citation17 and because we inflated the number of households to be visited by 20% to allow for non-response, we planned to include at least 656 households in the survey.
Team composition and training
Two field teams were trained. Each consisted of a Senior Ophthalmic Technician trained and certified as a grader by the GTMPCitation19; a data recorder; a driver-mechanic or experienced boat driver with knowledge of the locality; and a local guide, where necessary, to facilitate communication in local dialects. To ensure the presence of signs of trachoma for grader training and testing purposes,Citation19 training of graders and recorders was undertaken in Sudan, where many children have active trachoma,Citation20 in November 2015, with the full agreement of Sudanese authorities. Version 3 of the GTMP training systemCitation21 was used.
Sampling
From a complete list of villages in the seven districts, 22 villages (clusters) were systematically selected with probability proportional to the size of the village population.Citation5 In each village, we planned to have the Chief use random draw to select a compact segment of 30 households, anticipating, based on experience in other countries,Citation4,Citation22–Citation25 that a field team would be able to visit 30 households in one day. All households in the selected segment would then be visited and the residents of those households invited to participate, with 22 clusters of 30 households providing a total of 660 households for the survey. Conditions on the ground, however, made visiting 30 households per day difficult: many villages had fewer than 30 households, and it was often necessary to move from house to house by boat. After pilot fieldwork, the number of households to be visited per village was revised to 20. When selected villages had fewer than 25 households, field teams conducted an exhaustive survey of those households. In seven larger villages, a sketch map was drawn with the help of the village chief or another key informant, and blocks of 20 households were demarcated. One block was then selected by random draw. Where division of the village into segments of 20 households was politically or numerically problematic, a slightly larger (rather than slightly smaller) number was preferred. All persons aged 12 months and over who, at the time of the survey, were currently resident and had resided for at least the previous six months in a selected household, were asked to consent to be examined. Households and individuals who declined to participate were not replaced.
Fieldwork
Teams worked under the supervision of the National Coordinator of the Onchocerciasis Control Program (FM). At each household, the team recorded global positioning system coordinates, obtained informed verbal consent, and recorded residents’ responses to questions about access to water and sanitation, in inspecting (where present) the households latrine, in accordance with the GTMP standard protocol.Citation19 Both eyes of each consenting individual were examined by a GTMP-certified grader, who used a binocular loupe (magnification 2.5) and good light to examine for trichiasis, TF, and trachomatous inflammation—intense.Citation14 The definition of the WHO simplified trachoma grading schemeCitation14 were applied for each sign. Data were recorded in the GTMP Android smartphone app. Individuals with active trachoma were given topical 1% tetracycline ointment to be used twice daily for six weeks. Individuals with trichiasis were informed of the risks of the disease and referred to the nearest medical center for surgery. In order to prevent pathogens from being transferred from one examinee to the next, graders cleaned their hands with alcohol gel after each examination.
When a resident 1–9-year-old was absent at the time of the field team’s first visit, the team returned to the same home a second time in the same day. If the individual was not then found, he or she was declared “absent.”
Data were uploaded to the GTMP server at the end of each day, and cleaned, analyzed and approved as described in detail elsewhere.Citation19 In brief, cluster-level data on TF were adjusted for the age of those examined, and cluster-level data on trichiasis were adjusted by the age and gender of those examined. We used the arithmetic means of the adjusted cluster-level proportions as the evaluation-unit-level prevalence estimates of each of these signs. Confidence intervals (CIs) were determined by bootstrapping, with 10,000 replications. For the prevalence of access to water and sanitation at household level, CIs were calculated assuming a normal distribution.Citation26
Ethical considerations
Protocols were approved by the National Ethics/Bioethics Committee (000705/MSP/CAB/DGELM-15) and the London School of Hygiene & Tropical Medicine (6319 and 8355). Verbal consent was obtained from all participants (or their parents or guardians, in the case of children). Data were only collected on eligible, consenting subjects. As indicated above, antibiotics or referral for surgery were provided, as indicated. Both antibiotics and trichiasis surgery were available at no cost to participants who needed them.
Results
Fieldwork was undertaken from November 28, 2015 to December 20, 2015. A total of 466 households were visited in 22 villages across the seven districts, and 2377 residents aged ≥1 year were enumerated; 2081 (88%) of them were examined. The number of households included per village ranged from 20 to 25 (mean 21.2).
In the ≥15-year-old age group, 963 individuals were enumerated, of whom 269 were absent, 0 refused to be examined and 694 were examined. No cases of trichiasis were identified.
In the 1–9-year-old age group, 1237 individuals were enumerated, of whom 15 were absent, 0 refused to be examined, and 1222 were examined. Three cases of TI and 33 cases of TF were identified in 1–9-year-olds. The age-adjusted prevalence of TF in 1–9-year-olds was 2.5% (95%CI 0.9–4.5%).
Only 39% (95%CI 35–44%) of households had access to an improved source of drinking water (a household mains connection, public standpipe, borehole, protected dug well, protected spring or rainwater collection) in the dry season. Only 10% (95%CI 7–13%) of households had access to their own improved sanitation facility (specifically, connection to a public sewer, connection to a septic system, a pour-flush latrine, a covered pit latrine, or a ventilated improved pit latrine).
Discussion
In this study, we employed the momentum,Citation18,Citation27 systemsCitation19,Citation28 and fundingCitation29 of the GTMP to investigate whether trachoma was a public health problem in an area felt to be the most at-risk part of the Republic of the Congo, a hitherto-unsurveyed country. This survey was set up as the epidemiological equivalent of a canary in the mine, with the understanding that finding trachoma at levels indicative of a public health problem here would prompt further trachoma surveys in surrounding health districts,Citation3,Citation4 and potentially further afield. We did not find trachoma at levels indicative of a public health problem, and (following the example of similar trachoma mapping exercises in Kogi and Kwara states of NigeriaCitation30,Citation31) do not now believe that such further mapping is justified (though refugee populations here may still need to be separately considered). This is good news for the global trachoma community, which is currently working to achieve global elimination targets set more than two decades ago.Citation32
As in many of the environments in which the GTMP operated,Citation3,Citation20,Citation33–Citation36 local conditions in Congo made fieldwork a complicated business. The villages sampled here were mostly distributed along more-or-less-navigable rivers, on land that was often flooded. Boats were usually the best—and sometimes the only—means of access. Completion of the survey was a credit to the field teams, who negotiated the terrain without complaint and returned data of high quality.Citation28,Citation37
There was, however, one particular shortcoming in our survey. Because of access issues and the spatial distribution of households, as noted in the Methods section above, it was not possible to include 30 households in each village. Trachoma clusters geographically at various scales,Citation38,Citation39 so the smaller number of households enrolled per cluster might have reduced the robustness of our prevalence estimates; the extent to which this is problematic is difficult to estimate. Fortunately, the average number of children resident in each household was considerably higher than we had planned for, based on national averages derived from census data. This meant that we achieved our sample size of 1–9-year-olds with a lower total number of households recruited than initially planned. However, we were able to enumerate only 963 ≥15-year-olds, and able to examine only 694 of them, the rest being absent from the household on the day it was visited. (The adults of these—mostly indigenous—communities, who are somewhat marginalized, were often unwilling to be examined or even enumerated.) A relatively wide confidence interval for a non-zero estimate of trichiasis prevalence could have been the result, had we observed any trichiasis cases. The lack of trichiasis in the individuals examined, and the informal corroborating accounts of local health workers (for whom trichiasis is not known as a presentation) give us some confidence in reporting a trichiasis prevalence of 0%. A systematic survey of eyecare workers nationally, asking about presentations of trichiasis, might help to further reinforce the view that trichiasis is rare or absent. In the meantime, in combination with the TF prevalence in 1–9-year-olds of 2.5%, we feel it is reasonable to propose that trachoma is unlikely to be a public health problem in this population.
Data on access to water and sanitation are useful to trachoma and other neglected tropical disease programmes, for advocacy and monitoring purposes.Citation40 The fact that a trachoma elimination programme will not be needed here does not devalue the water and sanitation information we collected, which suggests that most people in these health districts live in households in which the water source, means of solid human waste disposal, or both, are unimproved. Low levels of access to sanitation are linked to a number of infectious diseases and adverse health outcomes.Citation41,Citation42 There is an urgent need in this part of Congo for provision of better infrastructure for water and sanitation.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the writing and content of this article.
Additional information
Funding
References
- Smith JL, Flueckiger RM, Hooper PJ, et al. The geographical distribution and burden of trachoma in Africa. PLoS Negl Trop Dis. 2013;7(8):e2359. doi:10.1371/journal.pntd.0002359.
- International Trachoma Initiative. Global Atlas of Trachoma [www.trachomaatlas.org]. Atlanta: Task Force for Global Health; 2018.
- Kilangalanga J, Ndjemba JM, Uvon PA, et al. Trachoma in the Democratic Republic of the Congo: results of 46 baseline prevalence surveys conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2018;25(Sup 1):192–200.
- Phiri I, Manangazira P, Macleod CK, et al. The burden of and risk factors for trachoma in selected districts of Zimbabwe: results of 16 population-based prevalence surveys. Ophthalmic Epidemiol. 2018;25(Sup 1):181–191.
- Solomon AW, Zondervan M, Kuper H, Buchan JC, Mabey DCW, Foster A. Trachoma Control: A Guide for Programme Managers. Geneva: World Health Organization; 2006.
- World Health Organization. Report of the 3rd global scientific meeting on trachoma, Johns Hopkins University, Baltimore, MA, 19–20 July 2010 (WHO/PBD/2.10). Geneva: World Health Organization; 2010.
- Smith JL, Sturrock HJ, Olives C, Solomon AW, Brooker SJ. Comparing the performance of cluster random sampling and integrated threshold mapping for targeting trachoma control, using computer simulation. PLoS Negl Trop Dis. 2013;7(8):e2389. doi:10.1371/journal.pntd.0002389.
- Francis V, Turner V. Achieving Community Support for Trachoma Control (WHO/PBL/93.36). Geneva: World Health Organization; 1993.
- Kuper H, Solomon AW, Buchan J, Zondervan M, Foster A, Mabey D. A critical review of the SAFE strategy for the prevention of blinding trachoma. Lancet Infect Dis. 2003;3:372–381.
- Burton M, Habtamu E, Ho D, Gower EW. Interventions for trachoma trichiasis. Cochrane Database Syst Rev. 2015;11:CD004008.
- Evans JR, Solomon AW. Antibiotics for trachoma. Cochrane Database Syst Rev. 2011;3:CD001860.
- Ejere HO, Alhassan MB, Rabiu M. Face washing promotion for preventing active trachoma. Cochrane Database Syst Rev. 2015;2:CD003659.
- Rabiu M, Alhassan MB, Ejere HODEvans JR. Environmental sanitary interventions for preventing active trachoma. Cochrane Database of Systematic Reviews. 2012;2:CD004003. DOI: 10.1002/14651858.CD004003.pub4
- Thylefors B, Dawson CR, Jones BR, West SK, Taylor HR. A simple system for the assessment of trachoma and its complications. Bull World Health Organ. 1987;65:477–483.
- Solomon AW, Foster A, Mabey DC. Clinical examination versus Chlamydia trachomatis assays to guide antibiotic use in trachoma control programmes. Lancet Infect Dis. 2006;6(1):5–6. doi:10.1016/S1473-3099(05)70304-2.
- Solomon AW, Peeling RW, Foster A, Mabey DC. Diagnosis and assessment of trachoma. Clin Microbiol Rev. 2004;17(4):982–1011. doi:10.1128/CMR.17.4.982-1011.2004.
- Centre National de la Statistique et des Etudes Economiques. Recensement Général de la Population et de l’Habitation. Brazzaville: République du Congo, Ministère de l’économie, du plan, de l’aménagement du territoire et de l’intégration; 2010.
- Solomon AW, Kurylo E. The global trachoma mapping project. Community Eye Health. 2014;27:18.
- Solomon AW, Pavluck A, Courtright P, et al. The Global Trachoma Mapping Project: methodology of a 34-country population-based study. Ophthalmic Epidemiol. 2015;22(3):214–225. doi:10.3109/09286586.2015.1037401.
- Elshafie BE, Osman KH, Macleod C, et al. The Epidemiology of Trachoma in Darfur States and Khartoum State, Sudan: results of 32 population-based prevalence surveys. Ophthalmic Epidemiol. 2016;23(6):381–391. doi:10.1080/09286586.2016.1243718.
- Courtright P, Gass K, Lewallen S, et al. Global trachoma mapping project: training for mapping of trachoma (version 3). London: International Coalition for Trachoma Control; 2014. Available from: http://www.trachomacoalition.org/node/122.
- Mwingira UJ, Kabona G, Kamugisha M, et al. Progress of trachoma mapping in Mainland Tanzania: results of Baseline Surveys from 2012 to 2014. Ophthalmic Epidemiol. 2016;23(6):373–380. doi:10.1080/09286586.2016.1236974.
- Omar FJ, Kabona G, Abdalla KM, et al. Baseline Trachoma surveys in Kaskazini A and Micheweni Districts of Zanzibar: results of two population-based prevalence surveys conducted with the global trachoma mapping project. Ophthalmic Epidemiol. 2016;23(6):412–417. doi:10.1080/09286586.2016.1235206.
- Sokana O, Macleod C, Jack K, et al. Mapping trachoma in the solomon islands: results of three baseline population-based prevalence surveys conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2016;23(sup1):15–21. doi:10.1080/09286586.2016.1238946.
- Meng N, Seiha D, Thorn P, et al. Assessment of Trachoma in Cambodia: trachoma is not a public health problem. Ophthalmic Epidemiol. 2016;23(Sup 1):3–7. doi:10.1080/09286586.2016.1230223.
- Kirkwood BR. Essentials of Medical Statistics. Oxford: Blackwell Science; 1988.
- Courtright P, Rotondo LA, MacArthur C, et al. Strengthening the links between mapping, planning and global engagement for disease elimination: lessons learnt from trachoma. Br J Ophthalmol. 2018;102(10):1324–1327. doi:10.1136/bjophthalmol-2018-312476.
- Solomon AW, Willis R, Pavluck AL, et al. Quality assurance and quality control in the Global Trachoma Mapping Project. Am J Trop Med Hyg. 2018;99(4):858–863. doi:10.4269/ajtmh.18-0082.
- Trotignon G, Jones E, Engels T, et al. The cost of mapping trachoma: data from the Global Trachoma Mapping Project. PLoS Negl Trop Dis. 2017;11(10):e0006023. doi:10.1371/journal.pntd.0006023.
- Alada JJ, Mpyet C, Florea VV, et al. Prevalence of Trachoma in Kogi State, Nigeria: results of four local government area-level surveys from the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2018;25(Sup 1):33–40. doi:10.1080/09286586.2017.1409359.
- Alada J, Mpyet C, Florea VV, et al. Prevalence of and risk factors for trachoma in Kwara State, Nigeria: results of 8 population-based surveys from the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2018;25(Sup 1): 53–61. doi:10.1080/09286586.2018.1437188.
- Solomon AW, Emerson PM, Resnikoff S. Trachoma then and now: update on mapping and control. Community Eye Health. 2017;30:90–91.
- Ko R, Macleod C, Pahau D, et al. Population-based trachoma mapping in six evaluation units of Papua New Guinea. Ophthalmic Epidemiol. 2016;23(Sup 1):22–31. doi:10.1080/09286586.2016.1235715.
- Sherief ST, Macleod C, Gigar G, et al. The Prevalence of Trachoma in Tigray Region, Northern Ethiopia: results of 11 population-based prevalence surveys completed as part of the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2016;23(Sup 1):94–99. doi:10.1080/09286586.2016.1250917.
- Negash K, Macleod C, Adamu A, et al. Prevalence of trachoma in the Afar Region of Ethiopia: results of seven population-based surveys from the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2018;25(Sup 1): 3–10. doi:10.1080/09286586.2017.1362008.
- Hiep NX, Ngondi JM, Anh VT, et al. Trachoma in Viet Nam: results of 11 surveillance surveys conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2018;25(Sup 1):93–102. doi:10.1080/09286586.2018.1477964.
- Engels D. The Global Trachoma Mapping Project: a catalyst for progress against neglected tropical diseases. Ophthalmic Epidemiol. 2016;23(sup1):1–2. doi:10.1080/09286586.2016.1257139.
- Polack SR, Solomon AW, Alexander ND, et al. The household distribution of trachoma in a Tanzanian village: an application of GIS to the study of trachoma. Trans R Soc Trop Med Hyg. 2005;99(3):218–225. doi:10.1016/j.trstmh.2004.06.010.
- Smith JL, Sivasubramaniam S, Rabiu MM, Kyari F, Solomon AW, Gilbert C. Multilevel analysis of trachomatous trichiasis and corneal opacity in Nigeria: the role of environmental and climatic risk factors on the distribution of disease. PLoS Negl Trop Dis. 2015;9(7):e0003826. doi:10.1371/journal.pntd.0003826.
- Boisson S, Engels D, Gordon BA, et al. Water, sanitation and hygiene for accelerating and sustaining progress on neglected tropical diseases: a new Global Strategy 2015–20. Int Health. 2016;8(Suppl. 1):19–21. doi:10.1093/inthealth/ihv073.
- Freeman MC, Garn JV, Sclar GD, et al. The impact of sanitation on infectious disease and nutritional status: a systematic review and meta-analysis. Int J Hyg Environ Health. 2017;220(6):928-949. doi: 10.1016/j.ijheh.2017.05.007.
- Garn JV, Boisson S, Willis R, et al. Sanitation and water supply coverage thresholds associated with active trachoma: modeling cross-sectional data from 13 countries. PLoS Negl Trop Dis. 2018;12(1):e0006110. doi:10.1371/journal.pntd.0006110.
Appendix
The Global Trachoma Mapping Project Investigators are: Agatha Aboe (1,11), Liknaw Adamu (4), Wondu Alemayehu (4,5), Menbere Alemu (4), Neal D. E. Alexander (9), Ana Bakhtiari (2,9), Berhanu Bero (4), Sarah Bovill (8), Simon J. Brooker (1,6), Simon Bush (7,8), Brian K. Chu (2,9), Paul Courtright (1,3,4,7,11), Michael Dejene (3), Paul M. Emerson (1,6,7), Rebecca M. Flueckiger (2), Allen Foster (1,7), Solomon Gadisa (4), Katherine Gass (6,9), Teshome Gebre (4), Zelalem Habtamu (4), Danny Haddad (1,6,7,8), Erik Harvey (1,6,10), Dominic Haslam (8), Khumbo Kalua (5), Amir B. Kello (4,5), Jonathan D. King (6,10,11), Richard Le Mesurier (4,7), Susan Lewallen (4,11), Thomas M. Lietman (10), Chad MacArthur (6,11), Colin K. Macleod (3,9), Silvio P. Mariotti (7,11), Anna Massey (8), Els Mathieu (6,11), Siobhain McCullagh (8), Addis Mekasha (4), Tom Millar (4,8), Caleb Mpyet (3,5), Beatriz Muñoz (6,9), Jeremiah Ngondi (1,3,6,11), Stephanie Ogden (6), Alex Pavluck (2,4,10), Joseph Pearce (10), Serge Resnikoff (1), Virginia Sarah (4), Boubacar Sarr (5), Alemayehu Sisay (4), Jennifer L. Smith (11), Anthony W. Solomon (1,2,3,4,5,6,7,8,9,10,11), Jo Thomson (4); Sheila K. West (1,10,11), Rebecca Willis (2,9).
1. Advisory Committee, 2. Information Technology, Geographical Information Systems, and Data Processing, 3. Epidemiological Support, 4. Ethiopia Pilot Team, 5. Master Grader Trainers, 6. Methodologies Working Group, 7. Prioritisation Working Group, 8. Proposal Development, Finances and Logistics, 9. Statistics and Data Analysis, 10. Tools Working Group, 11. Training Working Group.