ABSTRACT
Purpose: To describe the study design, interobserver variability of the questionnaires and clinical procedures of Hyderabad Ocular Morbidity in Elderly Study (HOMES) designed to, (a) to investigate the prevalence, causes and risk factors for visual impairment, and (b) to assess the impact of dispensing spectacles and cataract surgery on visual functions, fear of falls (FOF) and depression among the elderly in India.
Methods: Individuals aged ≥60 years are considered elderly. The non-clinical protocol was administered by two trained investigators and included collection of personal, sociodemographic information, ocular and systemic history, Indian Visual Function Questionnaire (IND-VFQ33), Patient Health Questionnaire (PHQ9), Mini-Mental State Examination (MMSE) questionnaire, Hearing Handicap Inventory for the Elderly Screening (HHIE), Short Falls Efficacy Scale (SFES) questionnaire. The eye examination was conducted by a trained optometrist and vision technicians in clinics set-up in the homes and included visual acuity (VA) assessment for distance and near, anterior segment examination and fundus examination, and imaging. The reliability assessments were carried out among 138 participants.
Result: The intraclass correlation (ICC) coefficients for MMSE, PHQ9, HHIE, SFES was 0.73 (95% CI: 0.62–0.81), 0.67 (95% CI: 0.54–0.77), 0.63 (95% CI: 0.48–0.74) and 0.70 (95% CI: 0.58–0.79) respectively. The ICC for INDVFQ domains ranged from 0.66 (95% CI: 0.55–0.74) for Psychosocial Impact to 0.88 (95% CI: 0.84–0.91) for activity limitation. The ICC for VA was 0.94 (95% CI: 0.92–0.96).
Conclusion: All questionnaires demonstrated acceptable reliability and can be applied in the main study. HOMES is expected to provide data that will help plan strategies to contribute towards ‘healthy aging’ in India.
Introduction
Globally, 253 million people are visually impaired, of which about 85% of them are 50 years of age and older.Citation1 India is home to 8.8 million blind individuals and nearly 50 million people with moderate-to-severe visual impairment (MSVI).Citation1 Over 75% of all visual impairment is avoidable (preventable or treatable). Both cataract and uncorrected refractive errors remain the leading causes of blindness, and uncorrected refractive errors remain the leading cause of SVI.Citation2 While cataract surgery is one of the most cost-effective interventions in healthcare,Citation3,Citation4 uncorrected refractive errors can be corrected using spectacles.
Visual impairment is more common among the elderly living in residential care when compared to those living in their own homes in the communities and non-institutionalized environments.Citation5–Citation8 A significant proportion of this visual impairment among the elderly in residential care can be corrected by simple interventions such as spectacles and cataract surgery.Citation9–Citation12 Studies have shown that visual impairment in the elderly affects all dimensions of their life including mobility, self-care, driving, participation in social and religious activities and overall quality of life.Citation13–Citation15 Visual impairment is also associated with an increased risk of mortality.Citation16–Citation18 Reports have shown a delay in the risk of mortality as a result of cataract surgery,Citation19,Citation20 and correction of refractive errors resulting in a significant improvement in the quality of life.Citation21,Citation22 Furthermore, visual impairment may lead to falls which may lead to fractures resulting in an adverse impact on the quality of life of the individuals.Citation23–Citation28
Even though the phenomenon of ‘homes for the aged’ centres is a recent concept in India, these are a well-organized sector and have been in existence for several decades in developed countries.Citation29 In India, the home for the aged centres are diverse both in terms of scope, amenities provided and the number of elderly living in each centre. These homes are typically run by non-governmental, religious or voluntary organizations with support from the government and philanthropists. In some homes, either the elderly person or their kin pay the ‘user fee’. Most of these homes offer food and accommodation, and private homes are even staffed with nursing staff to attend the medical needs and other support staff to assist elderly residents in daily routine tasks.Citation29
Sound epidemiological data on prevalence and causes of visual impairment are needed to formulate strategies to address vision loss in the elderly in residential care. Research on the prevalence and impact of visual impairment among the elderly population has been carried out in developed countries but such research is still in a stage of infancy in India.Citation5,Citation30–Citation35 To address this lacuna, a well-designed epidemiological study focused on the elderly is needed. In this background, The Hyderabad Ocular Morbidity in Elderly Study (HOMES) is being undertaken. HOMES is a longitudinal study designed (A) to investigate the prevalence, causes and risk factors for visual impairment among elderly individuals living in residential care facilities in Hyderabad, India, (B) to assess the impact of interventions such as spectacles and cataract surgery on visual functions in elderly living in residential care, and (C) to assess the prevalence of fear of falls (FOF), depression and hearing impairment, and their association with vision loss. This paper describes the study design and methodology adopted for HOMES.
Materials and methods
Ethics approval
The study protocol was approved by the institutional review board of the Hyderabad Eye Research Foundation, L V Prasad Eye Institute, Hyderabad, India. The study is currently being carried out in accordance with the Declaration of Helsinki. The elderly residents are enrolled in the study after obtaining written informed consent. Approval from the administrative head of the home for the aged centre is also being obtained before starting the data collection process.
Study design and sampling method
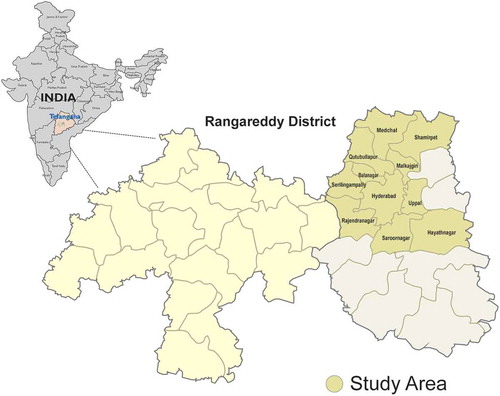
HOMES is a longitudinal study with pre and post-intervention phases and is being carried out in Hyderabad, a city in the south Indian state of Telangana and in its surrounding regions ().
For the purpose of the study, each ‘home for the aged’ centre is considered as a cluster. Based on an anticipated prevalence of avoidable visual impairment of 20%, a precision in the estimate of 20% of the prevalence, a non-response rate of 25%, a design effect of 1.4 to account for clustering, a sample size of 666 individuals is required. The prevalence estimates were based on our previous publication on visual impairment in the elderly in residential care.Citation34 We anticipate a lower prevalence in HOMES compared to our previous study which was done in rural areas whereas HOMES is carried out in urban locations.Citation34 shows the sample sizes for a cluster size of 40, 50 and 60 individuals with varying anticipated prevalence. For logistical reasons, only those homes with at least 10 freely mobile residents are included in the study.
Table 1. Sample size calculations for various cluster sizes, expected prevalence of visual impaiment (VI) and number of people with VI in the sample.
A list of homes was obtained from HelpAge India, a non-governmental organization working for the aged care and also from other resources such as governmental publications. There are 110 homes for the aged in this region. The number of residents in these homes ranges from 10 to over 80 with most institutions having about 40 to 50 residents. All the homes within 50-km radius of the L V Prasad Eye Institute are mapped and the required number of homes is randomly selected for the study. The residents aged ≥60 years at the time of enumeration and residing in these homes for at least a period of one month and agreed to participate are included in the study.
Definitions
Visual impairment is defined as presenting visual acuity worse than 6/18 in the better eye and included blindness (worse than 3/60), severe visual impairment (worse than 6/60 to 3/60) and moderate visual impairment (worse than 6/18 to 6/60). Visual impairment caused due to cataract and uncorrected refractive errors will be considered as avoidable visual impairment. Refractive error is defined as spherical equivalent (i.e. sphere + ½ cylinder) > ± 0.50 Diopter in the better eye and the functional definition of refractive error are defined as the change in at least one visual impairment category with the best refractive correction. Cataract is defined as the presence of any lenticular opacity that causes visual impairment. Presbyopia is deemed to be present if a presenting near vision is worse than N8 but improves to N8 or better with near correction.
The main cause of visual impairment is assigned by the clinician first for the eye and then for the person. In cases where there are multiple causes, based on the clinical examination and the retinal images, the cause that is more likely to explain the vision loss is considered as the main cause in that eye. At the person level, in cases, where there are different causes of visual impairment in both the eyes, the cause that is more easily correctable or treatable is given precedence over other causes. For example, if cataract is the cause for visual impairment in the right eye and uncorrected refractive error in the left eye, then at the person level, uncorrected refractive error is marked as the main cause and used for analysis.
Study team
The study team comprises two social investigators (professionals with a master’s degree in social work and trained is survey research methods). The clinical team includes an optometrist and vision technicians (personnel trained to provide primary eye care including basic eye examination, visual acuity assessment and refraction) who visit the home for the aged centres and conduct eye examinations. The logistics for the study is organized by a study coordinator, who also takes care of the referrals. At the data centre, two data entry personnel are involved in data entry. The study is led by the principal investigator who has overall responsibility for the scientific and administrative aspects of the study.
Non-clinical protocol
The non-clinical protocol included the administration of questionnaires by the trained investigators.
The questionnaires included personal, sociodemographic, ocular and systemic history, Indian Visual Function Questionnaire (IND-VFQ 33),Citation36,Citation37 Patient Health Questionnaire (PHQ-9),Citation38 Mini-Mental State Examination (MMSE) questionnaire,Citation39 Hearing Handicap Inventory for the Elderly Screening (HHIE-S),Citation40 Short Falls Efficacy Scale (SFES) questionnaire.Citation41,Citation42 Based on interviewers' observations, mobility status of the participants is classified as ‘independently mobile’, ‘mobile with assistance’ and ‘immobile/bedridden’.
Independent bilingual reviewers translated all the questionnaires from English language into the local language (Telugu) and also reverse translated into English to ensure that the content of the questionnaire remain unchanged. The questionnaire administration process is audio recorded for random reviews as a part of the quality control measure. A folder containing all the study instruments (forms) is prepared for each participant by the investigators who conduct the interviews in the homes. The consent form in the local language (Telugu) is also available in the folder. Once the interviews are completed, the folders are verified and handed over to the study coordinator who will, in turn, pass it on to the clinical team for an examination.
Participants who were bedridden are examined but not all questionnaires are administered. This shorter version of assessment included personal and demographic information, systemic and ocular history, Washington disability questionnaire and clinical examination. The interviews were attempted on all the independently mobile individuals. After the collection of personal and demographic information, mini-mental state examination (MMSE) assessment questionnaire is administered. If the MMSE score is less than 20 (suggestive of mild cognitive impairment), then questionnaires were restricted to systemic and ocular history, risk factors and complete clinical examinations. For all those individuals whose MMSE scores are greater than or equal to 20, the remaining set of questionnaires were administered, and complete examination protocol is carried out as shown in .
Table 2. Study questionnaires used in the HOMES project.
The questionnaire administration is always done before the clinical examination. After the administration of questionnaires, anthropometry measures and performance-based measures (PBM)Citation43 are carried out by the trained vision technician. This is followed by clinical eye examination by trained optometrist and vision technicians. Clinical competence of vision technicians in conducting the clinical examinations are published.Citation44,Citation45 The interviews and non-clinical examination are always scheduled on different days to ensure that elderly participants are not tired and ample time is provided to take rest in between the procedures if necessary.
Clinical examination protocol
The clinical examination protocol includes visual acuity assessment, stereopsis, near-vision assessment, refraction, slit-lamp biomicroscopy and fundus examination. Distance visual acuity (VA) is measured with the standard log MAR (logarithm of the minimum angle of resolution) chart with tumbling E and English alphabet optotypes under good illumination of at least 180 lux measured using a light meter.The VA is tested with the subject’s current refractive correction if glasses are being used. Apart from this, unaided VA and pinhole VA is recorded. Near VA is measured at a distance of 40 cm using the log MAR near vision “E” chart with the current refractive correction, if any, along with unaided acuity. For VA measurement with log MAR chart, letter by letter scoring method is used for distance and near vision. For participants uncooperative for VA assessment using the log MAR chart, fixation pattern, steadiness, and maintenance of fixation are assessed using a torchlight. Reverse contrast VA (white optotypes with a black ground) is also measured. Contrast sensitivity is measured with the MARS contrast sensitivity chart (Mars Perceptrix Corporation (Chappaqua, NY)). It consists of 48 letters of 1.75 cm height arranged in eight rows of six letters each. The contrast of the optotypes ranges from 91% (–0.04 log units) to 1.2% (1.92 log units) with the contrast of each letter decreasing by a constant factor of 0.04 log units. Each letter subtends 2° at the test distance of 50 cm (equivalent to 20/480). This test is conducted using habitual spectacle correction. Numerical optotypes are used in this study.
The external examination, including ocular motility using broad H test and cover tests, is done on all subjects. Ocular alignment is assessed by the Hirschberg test using a pen torch light with the refractive correction being used by the subject. Refraction is done for all subjects who have presenting distance worse than 6/12 or near vision worse than N8 in either eye. Both manual and autorefraction and acceptance are also done. Best-corrected distance and near VA are assessed and documented. Slit lamp Examination is conducted using a portable slit lamp (BA 904 Haag-Streit Clement Clarke International, UK). The eyelids, conjunctiva, cornea, anterior chamber, iris/pupil and lens are examined. Intraocular pressure (IOP) is measured using hand-held Perkins applanation tonometer (Mk3 Haag-Streit Clement Clarke International, UK) after administration of topical anesthetic eye drops and fluorescein stain. The probe of the tonometer is cleaned with alcohol swabs after examining each participant. Intraocular pressure is estimated digitally for those who are uncooperative with tonometry or have an active infection. Fundus examination and retinal photography is done using a non-mydriatic fundus camera (Zeiss Visuscout). Images are reviewed by experts and are graded.
Intervention for visual impairment
Participants with visual impairment in one or both eyes are referred to L V Prasad Eye Institute for a comprehensive eye examination. All services including eye examinations, surgeries, ophthalmic lasers and spectacles are provided at ‘no-cost’ to the participants. Clinical consultations at the institute are facilitated and transportation assistance is provided wherever required. The clinical protocol and the questionnaires are administered twice to all participants, once at the baseline and then again after 3–6 months after the intervention for cataract, refractive errors and other conditions. Only one complete assessment is done after the intervention.
Reliability study
A reliability study was set up to assess the inter-examiner reliability of the questionnaires and the clinical measurements. The inter-examiner reliability assessment was done between the two examiners for Mini-Mental State Examination (MMSE), Indian Visual Function (IND-VFQ) Questionnaire, Patient Health Questionnaire (PHQ-9), Hearing Handicap Inventory (HHIE), Short Falls Efficacy Scale (SFES) questionnaires. Intraclass Correlation Coefficient (ICC) was used to assess inter-examiner reliability.Citation46 ICC estimates and their 95% confident intervals were calculated using Stata Statistical Software version 14 based on a mean-rating (k = 2), consistency definition, single rater type, two-way mixed-effects model. For visual acuity assessment, a senior optometrist was used as the gold standard. All instruments have shown acceptable reliability of at least 0.6 or more (). After the reliability study, a pilot study was done in four home for the aged centres with an aim to understand the workflow dynamics and to fine-tune the protocols for the main study.
Table 3. Results of the reliability study.
Pilot study
In total, 64 elderly participants were examined from four home for the aged centres. The mean age of these participants was 76.7 years (standard deviation of 9.3 years; range 60 to 99 years). Among those examined, 50% were women. In total, 59 (92.2%) of the participants were freely mobile and 5 (7.8%) were bed-ridden. Based on presenting visual acuity, visual impairment was present in 28.1% (95% CI: 17.6–40.8) of the participants which decreased to 17.2% (95% CI: 8.9–28.7) with the best correction suggestive of a large unmet need for spectacles. Of the 50 participants to whom questionnaires were administered, 18% had moderate to severe depression on PHQ-9 questionnaire, 50% had moderate to high concern of falls on Short Falls Efficacy Scale (SFES) questionnaire, 26% reported mild to significant hearing impairment on the Hearing Handicap Inventory for Elderly (HHIE) questionnaire. A ‘make-shift’ clinic was made in each of the homes and all the study instruments were administered successfully. Based on the outcomes of the pilot study, the main study is being conducted. The flow chart of the examination protocol finalized for the main study is shown in .
Data management and analysis plan
Data on each participant are recorded on HOMES data collection forms. After interviews and clinical examination, all the completed data folders are received at the data centre and entered the database developed in Microsoft Access® with built-in validation checks for minimizing data entry errors using double data entry. The data are backed up daily and stored securely in a network server. The hard copies of the folders are stored in an iron cupboard in termite-free environment in the data centre under lock and key accessible only to the data entry personnel and principal investigator. Data analysis is conducted using Stata Statistical Software for Windows, version 14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). The statistical tools used for data analysis include prevalence estimates with their confidence intervals, chi-square and t-tests for univariate analyses, and logistic regression for multivariate analyses. The regression models will be assessed using variance inflation factors (VIF) and goodness of fit tests. The digital images and audio files of the interviews are systematically archived using the participant identification numbers which is a unique number allotted to every participant and this number common across all the databases.
Prevalence and causes of visual impairment
The prevalence and causes of visual impairment will be calculated and presented with 95% confidence intervals. Multivariable analysis will be conducted using binary logistic regression analysis to assess the association between visual impairment and age, gender, education, systemic conditions such as diabetes, hypertension and other risk factors.
Impact of interventions to improve vision
The Indian Visual Function questionnaire scores of those with and without visual impairment will be compared at the baseline. Post-intervention, re-assessment and comparisons of the visual function scores will be made between baseline and post-intervention for each participant. The baseline performance-based measure scores will be compared with the post-intervention scores.
Falls, fear of falling and visual impairment
The prevalence of falls and fear of falling will be estimated and presented with 95% confidence intervals. Multivariable analysis will be conducted using binary logistic regression analysis to assess the association between falls, fear of falls and visual impairment, age, gender, education, systemic conditions such as diabetes, hypertension, hearing, cognition and frailty measures.
Discussion
The HOMES study is one of the most comprehensive eye health studies being done on the elderly age group living in residential care in India. This study also aims to understand factors such as cognition, depression, hearing, falls and their association with vision loss. At this juncture when India is experiencing a demographic shift with an increasing proportion of the elderly population, the results from this study can provide valuable insights to develop long-term comprehensive geriatric health strategies including eye care services in India.
The methodology and the clinical procedures adopted in this study are based on several published studies. The study protocols are adapted to suit the Indian context and local applicability. For example, the Indian Visual Function questionnaire is country-specific and the use of this questionnaire in this study is expected to provide valuable insights on visual functions and change in visual functions due to intervention. The performance-based measures are modified to suit the local context. All the protocols were successfully field-tested in the pilot study and necessary modifications were done before applying in the main study.
Though the limitation of generalizability of the reulst of this study to the general population at large remains as the study is restricted to home for the aged centres, it is expected to provide useful insights on the impact of interventions for vision loss in the elderly in India. As interviews of elderly who are bed-ridden are restricted to socio-demographic information only, this will remain a limitation as the reason for illness due to which the elderly have become bed-ridden is not readily available.
In conclusion, the HOMES study is one of the most comprehensive eye health studies on the elderly age group living in residential care in India. The pilot study has provided valuable insights on several factors such as clinic setup and time duration for each eye examination for the main study. A clear workflow was established for various study procedures. It also provided information for planning logistics for the main study. The data collection is expected to take two years. The information from this study is expected to contribute significantly to the development of strategies to achieve the overarching goal of ‘healthy aging’ and ‘happy aging’ in India in the years to come.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Acknowledgments
The authors thank the volunteers for their participation in the study. Mr. Hira B Pant, Mr. Ratnakar Yellapragada, and Ms. Muni Rajya Lakshmi are acknowledged for their support in data management. Ms. Madhuri Bakki is acknowledged for her assistance in conducting the study procedures. The authors also thank Dr. Cynthia Owsley (University of Alabama at Birmingham, USA), Dr. Shobha Mocherla and Ms. Neha Hassija for inputs on earlier versions of the manuscript.
Disclosure statement
The authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
Additional information
Funding
References
- Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–e897. doi:10.1016/S2214-109X(17)30293-0.
- Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–e1234. doi:10.1016/S2214-109X(17)30393-5.
- Baltussen R, Sylla M, Mariotti SP. Cost-effectiveness analysis of cataract surgery: a global and regional analysis. Bull World Health Organ. 2004;82:338–345.
- Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114:1670–1678. doi:10.1016/j.ophtha.2006.12.013.
- Mitchell P, Hayes P, Wang JJ. Visual impairment in nursing home residents: the Blue mountains eye study. Med J Aust. 1997;166:73–76. doi:10.5694/mja2.1997.166.issue-2.
- Owsley C, McGwin G, Scilley K, Meek GC, Dyer A, Seker D. The visual status of older persons residing in nursing homes. Arch Ophthalmol. 2007;125:925–930. doi:10.1001/archopht.125.7.925.
- Sinoo MM, Kort HS, Duijnstee MS. Visual functioning in nursing home residents: information in client records. J Clin Nurs. 2012;21:1913–1921. doi:10.1111/j.1365-2702.2012.04128.x.
- Eichenbaum JW, Burton WB, Eichenbaum GM, Mulvihill M. The prevalence of eye disease in nursing home and non-nursing home geriatric populations. Arch Gerontol Geriatr. 1999;28:191–204. doi:10.1016/S0167-4943(99)00009-6.
- Evans BJ, Rowlands G. Correctable visual impairment in older people: a major unmet need. Ophthalmic Physiol Opt. 2004;24:161–180. doi:10.1111/j.1475-1313.2004.00197.x.
- Foran S, Rose K, Wang JJ, Mitchell P. Correctable visual impairment in an older population: the blue mountains eye study. Am J Ophthalmol. 2002;134:712–719. doi:10.1016/S0002-9394(02)01673-2.
- Fung MM, Yap M, Cheng KK. Correctable visual impairment among people with diabetes in Hong Kong. Clin Exp Optom. 2010;93:453–457. doi:10.1111/j.1444-0938.2010.00539.x.
- Hollands H, Brox AC, Chang A, et al. Correctable visual impairment and its impact on quality of life in a marginalized Canadian neighbourhood. Can J Ophthalmol. 2009;44:42–48. doi:10.3129/i08-167.
- Lamoureux EL, Fenwick E, Moore K, Klaic M, Borschmann K, Hill K. Impact of the severity of distance and near-vision impairment on depression and vision-specific quality of life in older people living in residential care. Invest Ophthalmol Vis Sci. 2009;50:4103–4109. doi:10.1167/iovs.08-3294.
- Varma R, Wu J, Chong K, Azen SP, Hays RD. Los Angeles Latino eye study G. Impact of severity and bilaterality of visual impairment on health-related quality of life. Ophthalmology. 2006;113:1846–1853. doi:10.1016/j.ophtha.2006.04.028.
- Jacobs JM, Hammerman-Rozenberg R, Maaravi Y, Cohen A, Stessman J. The impact of visual impairment on health, function and mortality. Aging Clin Exp Res. 2005;17:281–286. doi:10.1007/BF03324611.
- Karpa MJ, Mitchell P, Beath K, et al. Direct and indirect effects of visual impairment on mortality risk in older persons. Arch Ophthalmol. 2009;127:1347–1353. doi:10.1001/archophthalmol.2009.240.
- Foong AW, Fong CW, Wong TY, Saw SM, Heng D, Foster PJ. Visual acuity and mortality in a chinese population. The Tanjong Pagar study. Ophthalmology. 2008;115:802–807. doi:10.1016/j.ophtha.2007.04.066.
- Freeman EE, Egleston BL, West SK, Bandeen-Roche K, Rubin G. Visual acuity change and mortality in older adults. Invest Ophthalmol Vis Sci. 2005;46:4040–4045. doi:10.1167/iovs.05-0687.
- Fong CS, Mitchell P, Rochtchina E, de Loryn T, Tan AG, Wang JJ. Visual impairment corrected via cataract surgery and 5-year survival in a prospective cohort. Am J Ophthalmol. 2014;157(163–170):e161. doi:10.1016/j.ajo.2013.08.018.
- Fong CS, Mitchell P, Rochtchina E, Teber ET, Hong T, Wang JJ. Correction of visual impairment by cataract surgery and improved survival in older persons: the Blue mountains eye study cohort. Ophthalmology. 2013;120:1720–1727. doi:10.1016/j.ophtha.2013.02.009.
- Lamoureux EL, Saw SM, Thumboo J, et al. The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay eye study. Invest Ophthalmol Vis Sci. 2009;50:2614–2620. doi:10.1167/iovs.08-2164.
- Owsley C, McGwin G Jr., Scilley K, Meek GC, Seker D, Dyer A. Effect of refractive error correction on health-related quality of life and depression in older nursing home residents. Arch Ophthalmol. 2007;125:1471–1477. doi:10.1001/archopht.125.11.1471.
- Cox A, Blaikie A, MacEwen CJ, et al. Visual impairment in elderly patients with hip fracture: causes and associations. Eye (Lond). 2005;19:652–656. doi:10.1038/sj.eye.6701610.
- Felson DT, Anderson JJ, Hannan MT, Milton RC, Wilson PW, Kiel DP. Impaired vision and hip fracture. The Framingham study. J Am Geriatr Soc. 1989;37:495–500. doi:10.1111/j.1532-5415.1989.tb05678.x.
- Ivers RQ, Norton R, Cumming RG, Butler M, Campbell AJ. Visual impairment and risk of hip fracture. Am J Epidemiol. 2000;152:633–639. doi:10.1093/aje/152.7.633.
- Lord SR. Visual risk factors for falls in older people. Age Ageing. 2006;35(Suppl 2):ii42–ii45. doi:10.1093/ageing/afl085.
- Wood JM, Lacherez P, Black AA, Cole MH, Boon MY, Kerr GK. Risk of falls, injurious falls, and other injuries resulting from visual impairment among older adults with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52:5088–5092. doi:10.1167/iovs.10-6644.
- Lamoureux EL, Chong E, Wang JJ, et al. Visual impairment, causes of vision loss, and falls: the singapore malay eye study. Invest Ophthalmol Vis Sci. 2008;49:528–533. doi:10.1167/iovs.07-1036.
- Ara S. Old-age homes & the profile of their residents. Indian J Med Res. 1997;106:409–412.
- Tielsch JM, Javitt JC, Coleman A, Katz J, Sommer A. The prevalence of blindness and visual impairment among nursing home residents in Baltimore. N Engl J Med. 1995;332:1205–1209. doi:10.1056/NEJM199505043321806.
- van der Pols JC, Bates CJ, McGraw PV, et al. Visual acuity measurements in a national sample of British elderly people. Br J Ophthalmol. 2000;84:165–170. doi:10.1136/bjo.84.2.165.
- VanNewkirk MR, Weih L, McCarty CA, Stanislavsky YL, Keeffe JE, Taylor HR. Visual impairment and eye diseases in elderly institutionalized Australians. Ophthalmology. 2000;107:2203–2208. doi:10.1016/S0161-6420(00)00459-0.
- Wang JJ, Mitchell P, Cumming RG, Smith W. Blue Mountains eye S. Visual impairment and nursing home placement in older Australians: the Blue mountains eye study. Ophthalmic Epidemiol. 2003;10:3–13. doi:10.1076/opep.10.1.3.13773.
- Marmamula S, Ravuri CS, Boon MY, Khanna RC. A cross-sectional study of visual impairment in elderly population in residential care in the South Indian state of Andhra Pradesh: a cross-sectional study. BMJ Open. 2013;3:e002576. doi:10.1136/bmjopen-2013-002576.
- Marmamula S, Ravuri LV, Boon MY, Khanna RC. Spectacle coverage and spectacles use among elderly population in residential care in the south Indian state of Andhra Pradesh. Biomed Res Int. 2013;2013:183502. doi:10.1155/2013/183502.
- Gothwal VK, Bagga DK, Sumalini R. Rasch analysis of the Indian vision function questionnaire. Br J Ophthalmol. 2012;96:619–623. doi:10.1136/bjophthalmol-2011-300092.
- Finger RP, Kupitz DG, Holz FG, et al. The impact of the severity of vision loss on vision-related quality of life in India: an evaluation of the IND-VFQ-33. Invest Ophthalmol Vis Sci. 2011;52:6081–6088. doi:10.1167/iovs.11-7388.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi:10.1046/j.1525-1497.2001.016009606.x.
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi:10.1016/0022-3956(75)90026-6.
- Ventry IM, Weinstein BE. The hearing handicap inventory for the elderly: a new tool. Ear Hear. 1982;3:128–134. doi:10.1097/00003446-198205000-00006.
- Kempen GI, Yardley L, van Haastregt JC, et al. The short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing. 2008;37:45–50. doi:10.1093/ageing/afm157.
- Reed-Jones RJ, Solis GR, Lawson KA, Loya AM, Cude-Islas D, Berger CS. Vision and falls: a multidisciplinary review of the contributions of visual impairment to falls among older adults. Maturitas. 2013;75:22–28. doi:10.1016/j.maturitas.2013.01.019.
- Owsley C, McGwin G Jr., Sloane ME, Stalvey BT, Wells J. Timed instrumental activities of daily living tasks: relationship to visual function in older adults. Optom Vis Sci. 2001;78:350–359. doi:10.1097/00006324-200105000-00019.
- Paudel P, Cronje S, O’Connor PM, Rao GN, Holden BA. Clinical competency of 1-year trained vision technicians in Andhra Pradesh, India. Ophthalmic Epidemiol. 2015;22:409–416. doi:10.3109/09286586.2015.1082605.
- Suram V, Addepalli UK, Krishnaiah S, Kovai V, Khanna RC. Accuracy of vision technicians in screening ocular pathology at rural vision centres of southern India. Clin Exp Optometry. 2016;99:183–187. doi:10.1111/cxo.12345.
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. doi:10.1016/j.jcm.2016.02.012.