ABSTRACT
Purpose
Estimates of diabetic eye disease in American Indian and Alaska Natives (AI/AN) vary over time, region, and methods. This article reports recent prevalence of diabetic retinopathy (DR) and diabetic macular edema (DME) in AI/AN served by the Indian Health Services’ (IHS) teleophthalmology program, as identified using ultrawide field imaging (UWFI).
Methods
This was a retrospective analysis of 2016–2019 clinical data (n = 53,900). UWF images were acquired by certified imagers using a validated protocol, and graded by licensed, certified optometrists supervised by an ophthalmologist. Graders evaluated the extent/severity of retinal lesions in comparison to standard photographs. DR lesions predominantly in any peripheral field were considered “predominantly peripheral lesions” (PPL). The analyses calculated prevalence of any DR, any DME, DR and DME severity, sight-threatening disease, and PPL.
Results
Patients averaged 56 years of age with a 68 mmol/mol A1c and 55% had had diabetes for 5+ years. Prevalence of any DR, any DME, and sight-threatening disease was 28.6%, 3.0%, and 3.0%. In patients with mild nonproliferative DR, PPL was seen in 25.3%. PPL suggested a more severe level of DR in 8.7% of patients. DR increased with age. DME decreased with age. Males and patients in the Nashville IHS area had more diabetic eye disease.
Conclusion
AI/AN have a high burden of diabetes and its complications. The IHS is resource-constrained, making accurate disease estimates necessary for resource allocation and budget justifications to Congress. These data update the estimates of diabetic eye disease in Indian Country and suggest that UWFI identifies early DR.
Introduction
American Indians and Alaska Natives (AI/AN) have a higher burden of diabetes than any other race/ethnic group in the United States; e.g., recent estimates show that 14.7% of AI/AN have diabetes versus 7.5% of non-Hispanic whites.Citation1 Additionally, AI/AN more often develop disabling and/or life-threatening long-term complications from diabetes.Citation2 Diabetic retinopathy (DR) and diabetic macular edema (DME) are complications of poorly controlled diabetesCitation3 and, despite the availability of effective treatments to reduce vision loss, DR remains the leading cause of new blindness in people aged 18–64.Citation1
The rate of diabetes and its potential to lead to severe vision loss make current and accurate estimates of DR and DME necessary – to guide strategic distribution of eye care infrastructure, specialists, and public health education about how to mitigate disease. This is especially true in a resource-constrained system such as the Indian Health Service (IHS), the federal agency primarily responsible for providing healthcare to the members of eligible AI/AN tribes. Congressional funding to the IHS is lower per capita than other federal systemsCitation4,Citation5 and expenditure per user of health care services was $4,078 in fiscal year 2019.Citation6 Most of the IHS ambulatory care facilities are rural with limited availability of specialty providers.Citation7
Previous prevalence estimates of diabetic eye disease in AI/AN have been limited in that they were derived from studies of a single tribe or several tribes in one area (e.g.Citation8–11) They also did not report prevalence of DME. In contrast, Bursell and colleagues recently reported DR and DME prevalence for AI/AN using data from the IHS’s large, nationally-distributed teleophthalmology program for the surveillance and care management of diabetic eye disease.Citation12 But those estimates were obtained from evaluations performed primarily using multi-field, nonmydriatic 45° field of view fundus photography (NMFP), which can have a high ‘ungradable rate’ (approximately 27%).Citation13 When a teleophthalmology exam cannot be graded, the presence/absence of disease cannot be determined, potentially resulting in underestimates of prevalence in aggregate.
The present study reports prevalence of diabetic eye disease in AI/AN as found using macula-centered, nonmydriatic 200° field of view ultrawide field imaging (UWFI) in the IHS’s nationally-distributed teleophthalmology program. UWFI has a 80–90% lower ungradable rateCitation13,Citation14 than NMFP and, with a single image needed per eye, gives a greater than 80% view across the retina, into its periphery.Citation15,Citation16
Materials and methods
Design, setting and participants
This is a retrospective data analysis from the IHS’s nationally-distributed teleophthalmology program’s clinical data from November 2016–October 2019. The Phoenix Area IHS Institutional Review Board determined this study to be exempt and approved it as a performance improvement project linked to clinical care operations.
Teleophthalmology for identification of diabetic retinal disease is well-established.Citation17,Citation18 The IHS’s teleophthalmology program, initiated in 2000, is an American Telemedicine Category 3 program, meaning the program’s clinicians identify the Early Treatment Diabetic Retinopathy Study (ETDRS; the gold standard for DR diagnosis and treatment) defined clinical levels of DR and DME severity with a diagnostic accuracy that matches clinical retinal examination through dilated pupils or ETDRS photographs.Citation19–22 The technology used by the program does not require pupil dilation to achieve this diagnostic accuracy, however. Also, a Category 3 program provides DR management plans commensurate with the clinical recommendations that would have resulted from a traditional ophthalmology-based clinical retinal examination through dilated pupils.
The IHS teleophthalmology program operates in primary care clinics, imaging patients with diabetes when they present for their primary care appointments. UWF images are acquired using a validated protocol by certified imagers located at the clinics. When sight-threatening disease is identified or the images cannot be graded, the teleophthalmology program recommends the patient see an eye care specialist for timely (i.e., immediately, within a month, within 3 months, etc.) treatment and management. The referral to specialty eye care is made by the primary care provider.
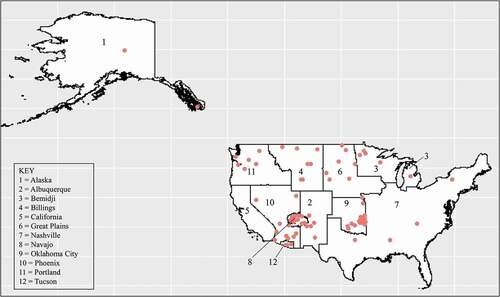
Data for this analysis are from the 78 clinics in 11/12 IHS administrative areas () that were actively imaging and using UWFI during the study’s selected time period.
Figure 1. Locations of the IHS teleophthalmology program sites (n = 78) for this analysis within the IHS administrative areas.
The analysis dataset included 53,900 unique patients with diabetes, aged 20+, specifically evaluated with UWFI (Optos®). Due to the maturity of the program, patients might have been evaluated in years prior to 2016. Also, due to the clinical practice recommendation that people with no evidence of DR should be screened annually as well as individual’s frequency of primary care visits or other factors, patients might have been imaged by the program more than once in the three-year timeframe of this study’s dataset. This analysis used the first evaluation in the time period of interest.
Measures
For the determination of DR and DME severity, previous studies have found that UWFI has perfect agreement with ETDRS photography in 84% of cases and agreement within one level of disease severity in 91% of cases (unweighted κ = 0.79).Citation23 Detailed protocols for evaluating UWF images have been described.Citation17 Graders, who are licensed, certified optometrists supervised by an ophthalmologist, evaluate images on standardized workstations at a centralized reading center at Phoenix Indian Medical Center. Each image is evaluated for distribution of hemorrhages and/or microaneurysms, venous beading, intraretinal microvascular abnormalities and new vessels on the retina. Any DR lesion type is considered predominantly peripheral when more than 50% of it is observed outside the ETDRS standard fields [i.e., ‘predominantly peripheral lesion’ (PPL)].Citation17 UWFI, due to its wide view of the retina, facilitates views of peripheral lesions that is not achievable with the aforementioned NMFP technology. Graders determine whether the presence of PPL increase overall DR severity.
This analysis consolidates the DR grading outcomes as: absent; mild nonproliferative DR (NPDR); moderate NPDR; severe/very severe NPDR; or proliferative DR (PDR). PDR includes ‘quiescent PDR’. DME grading outcomes are: absent; present, not clinically significant; or present and clinically significant (CSDME). This study also reports on presence of any DR, any DME, and sight-threatening disease. The latter is a composite measure defined as severe/very severe NPDR, PDR, and/or CSDME. If one eye was ungradable, the diagnosis for the other eye was used. Both eyes were ungradable in 4.5% (DR) and 5.4% (DME) of patients; those patients could not be included in the calculation of prevalence. If the diagnosis for eyes differed, the more severe level for DR and DME was used.
The IHS teleophthalmology program obtains demographics and known risk factors for the progression of diabetic eye disease from the electronic medical record, including: region where the patient was imaged, age, gender, A1c, diabetes duration, diabetes treatment, and presence of hypertension, hypercholesterolemia, cardiovascular disease, peripheral neuropathy, nephropathy, and anemia. The regions are: Alaska, Northwest/Portland, Northcentral/Great Plains (Bemidji, Great Plains, and Billings IHS areas), Nashville, Oklahoma, and Southwest (Phoenix, Navajo, Albuquerque, and Tucson IHS areas).
Analysis
The analysis calculated crude means or percentages (with 95% confidence intervals) for all measures. The percentage of patients who had PPL findings was also calculated. Direct adjusted prevalencesCitation24 for DR and DME were calculated using results from logistic regressions in which any DR, any DME, and DR and DME severity were regressed on age, gender, and region (base model). Regression coefficients from the base models and models with all background measures are not reported here because their relationships to diabetic eye disease are not the focus of this article, but they are available upon request from the corresponding author. Data preparation was completed using SAS 9.4 (SAS Institute, Cary, NC) and analyses were completed using R 4.0.4.Citation25
Results
The patients in this analysis were predominantly from the Southwest region of the IHS (52.2%), female (54.7%), were known to have diabetes for more than five years (55.1%), and were managing their diabetes with oral medication(s) only (48.2%) (). On average, they were 56 years of age and their A1c was 68 mmol/mol. Hypercholesterolemia (35.5%) and hypertension (57.7%) were common risk factors for these patients.
Table 1. Background characteristics of analytic sample (n = 53,900).
Crude prevalence of any DR was 28.6% (). With respect to level of DR, crude prevalence of mild and moderate NPDR was 12.3% and 13.4%. Severe NPDR and PDR, both of which are sight-threatening levels of DR, were present in 0.1% and 2.8% of patients.
Table 2. Crude prevalence of diabetic eye disease.
Among patients with any DR, PPL were present in 12.6%. For patients with mild NPDR, PPL were seen in 25.3%. Presence of PPL suggested a more severe DR diagnosis in 8.7% of patients with any DR. Of these, 86.4% were diagnosed with mild NPDR, 11.8% with moderate NPDR, 0.2% with severe/very severe NPDR, and 1.6% with PDR.
Crude prevalence of any DME was 3.0%. Less than 1% of patients had CSDME ().
Three percent of patients had a sight-threatening level of DR and/or CSDME. PDR was the most frequent contributor to this percentage.
Prevalence estimates of DR adjusting for age, gender and region showed that DR increased with age (), but prevalence of DME decreased with age. Within age groups, proportionately more males than females had DR and DME. Regions with the highest percentages of DR and DME in descending order were Nashville, Northcentral/Great Plains, and the Southwest.
Table 3. Adjusted prevalence of DR and DME, by region, gender and age.
Discussion
This study differs from and augments previous research on diabetic eye disease in AI/AN in three major ways. First, this study exclusively used UWFI. The UWFI modality is a newer technology that provides more consistent diagnoses due to its lower ungradable rate. It also provides a view of lesions beyond the ETDRS standard 7-fields – in the periphery of the retina – where early disease might also be present. Second, the IHS teleophthalmology program reaches more regions and tribes than in other studies of AI/AN, and it recruits patients from their primary care appointments, rather than from eye care clinics. The rural location of many IHS ambulatory clinics means that eye care clinics may not be easily accessible. Third, most prior studies did not report DME prevalence, whereas this study did.
Due to the aforementioned differences between this and prior studies, inter-study comparisons of DR and DME prevalence are difficult. Nonetheless, it is clear that the prevalence of any DR reported here is nearly 50% lower than 1980s–1990s publications.Citation9,Citation10 Our DR results are similar to findings from the 2005–2008 National Health and Nutrition Examination Survey (NHANES), which shows 28.5% had any DR (vs. 28.6% in the present study).Citation26 Sight-threatening DR was slightly higher in NHANES than in this study, at 4.4% (versus 3.0% in the present study).Citation26 The minimum age in the NHANES study was 40 years, however, whereas it was 20 years in this study, which might account for the higher percentage of sight-threatening disease in the NHANES participants.
In this analysis, any DR prevalence was found to be approximately 8.6% higher than in a prior recent report from the same teleophthalmology program (28.6% vs. 20.0%).Citation12 Some of the difference is because DR lesions beyond the ETDRS standard 7-fields – visible with UWFI – were identified in over 25% of patients with mild NPDR and led to a higher level of DR diagnosis for 8.7% of patients with any DR. Early identification of DR in this cross-sectional, prevalence study is important because that is when timely education, ocular evaluation and medical management can be effective in preserving vision. The retinal imaging encounter could provide a powerful education moment within the primary care environment because the provider could point to the PPL in the images, concretely discuss the implications of them, and strategize with the patient about how to change behaviors to slow progression.
Systemwide changes have contributed to decline in diabetic eye disease as reported in older studies of AI/AN. These systemwide changes include the IHS’s own Special Diabetes Program for Indians (SDPI), the Government Performance and Results Act (GPRA), and the IHS teleophthalmology program itself. The SDPI awards grants to improve patient awareness of prediabetes/diabetes and supports improving self-care behaviors such as increased physical activity and healthier nutrition choices. GPRA requires the IHS to track diabetes care performance measures annually. IHS audit data show improvements in blood glucose, blood pressure, and cholesterol corresponding to these system-wide changes.Citation27 The IHS teleophthalmology program itself had over 226,333 patient encounters from 2001–2019,Citation19 likely reducing the impact of diabetic eye disease in the IHS user population. As noted above, the teleophthalmology program identifies level of disease, including disease not yet considered sight-threatening. When severe disease is found, the program notifies the primary care provider that referral to eye or other specialty care is needed. When mild and moderate disease are found, the program gives specific care management guidance. Lastly, the program’s curriculum for new frontline personnel (taking the retinal images) includes training on communicating with patients about the importance and care of diabetic eye disease, something that previous research suggested was needed in Indian country.Citation28
Regarding the possibly counterintuitive inverse relationship between age and DME reported here, patients with macular edema causing decreased vision may present directly to an eye clinic, bypassing the teleophthalmology program. Patients referred by the program to an eye clinic for follow-up are not tracked systematically yet and, due to the large number of patients, tracking them retrospectively is beyond the scope of this study. These factors might have resulted in an undercounting of DME. Nevertheless, this analysis advances a literature that has rarely reported DME in AI/AN. A systematic literature review found that DME is becoming the major cause of vision loss worldwide,Citation18 underscoring the need to better understand its epidemiology in AI/AN further.
A limitation of this study is that the prevalence estimates exclude AI/AN who do not receive their health care from the IHS as well as all IHS patients who live in California. The IHS serves approximately 2.56 million AI/AN,Citation6 about half of the 5.2 million people who identified as AI/AN in the 2010 Census.Citation29 The gap between the number of AI/AN in the United States and the number of people in the IHS’s patient population is partly the result of eligibility criteria for IHS coverage (e.g., individual enrollment in a federally-recognized tribe) as well as tribal and/or personal preferences about interacting with federal agencies in general. In California, only about 13% of nonelderly AI/AN report getting health care from the IHS, which would limit the number of patients included in a report of prevalence based on IHS health/clinical data.Citation30 Moreover, California has several non-IHS DR surveillance programs [e.g., EyePACS (Eye Picture Archive Communication System)Citation31 and no California clinics have enrolled in the IHS teleophthalmology program yet.
Another limitation is that selection bias may be introduced when a dataset is created from a mature, ongoing clinic program such as this one. There is not a clear ‘baseline’ for all patients. The dataset for this study selected the first evaluation for patients who had multiple evaluations in the three-year timeframe, about 30% of the patients. Other options were to select those patients’ last teleophthalmology evaluation within the time period of interest or the evaluation with the highest level of disease. When we look at prevalence according to the maximum level of disease, 2.7% more patients have any DR and 0.4% more patients have any DME. Mild NPDR, moderate NPDR, and PDR are higher by 1.1%, 1.2%, and 0.4%, respectively, and CSDME is higher by 0.1%.
Important questions that are beyond the scope of this report include the incidence and progression of DR in AI/AN, the role of PPL in this progression, and patient adherence to follow-up eye care when it is recommended by program. The most recent reports of incidence of DR in AI/AN were published in the 1980s and 1990s,Citation32–34 prior to systemwide changes in the IHS as well as the availability of new medications for diabetes management, thus updated estimates from the IHS teleophthalmology program’s nationally-distributed clinic-based sample may be warranted. PPL should be considered as part of this analysis given research in other populations has found that the presence of PPL is associated with underlying retinal nonperfusion,Citation35 with a 3.2-fold increased risk of a 2 or more step DR progression, and with a 4.7-fold increased risk of developing PDR over 4 years.Citation36 Also, patients are not tracked by the teleophthalmology program when they are referred to specialty eye care, therefore true adherence rates are not yet known. A small, supplementary examination for this report found that 50.9% of patients imaged at Phoenix Indian Medical Center (PIMC) and diagnosed with sight-threatening disease went for follow-up care within nine months of the teleophthalmology exam. Further data collection and analysis are underway to examine adherence/retention and provide insights into how a primary-care based teleophthalmology program might improve poor adherence to standard of care and follow-up (especially among minoritiesCitation37,Citation38).
These findings may have policy implications for the IHS. The IHS’s per capita budget from Congress is less than other federal programs, yet diabetes burden is higher for AI/AN than other race/ethnic groups in the United States. Also, the location of IHS ambulatory care facilities in rural areas means access to specialty care is difficult for many patients. Thus, accurate and current measures of disease, including diabetic eye disease, are critical for planning the allocation of limited resources and for IHS budget justifications to Congress. The updated prevalence estimates reported here show that diabetic eye disease is lower than in previous decades but that the burden is still substantial to AI/AN served by the IHS. Rates of diabetic eye disease were highest in the Nashville area, where AI/AN population density is lower and where there are fewer IHS clinics than other regions. This implies the Nashville area clinics need to focus on more surveillance of diabetic eye disease, education of its significance, and recruiting eye care specialist to mitigate significant disease.
Financial Support
Estenda Solutions, Inc. is subcontracted by the Indian Health Service Tele-retinal program to provide required infrastructure, technology, and research support. This work was supported under that subcontract.
Acknowledgments
The opinions expressed in this paper are those of the authors and do not necessarily reflect the views of the Indian Health Service.
Disclosure statement
Stephanie Fonda is Vice President for Research, Estenda Solutions Inc. Sven-Erik Bursell is a scientific consultant for SocialEyes Corp., and sub-contractor for Estenda Solutions, Inc. Drew Lewis is President, Estenda Solutions Inc. Dawn Clary and Dara Shahon are federal employees of the IHS. Paolo Silva has three sources of nonfinancial research support to report: Optos Plc; Optomed; and Hillrom. We have no other proprietary interests to report.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020.National Diabetes Statistics Report, 2020. https://www.cdc.gov/diabetes/library/features/diabetes-stat-report.html. Accessed April 20, 2021.
- McLaughlin S. Traditions and diabetes prevention: a healthy path for Native Americans. Diabetes Spectr. 2010;23(4):271–277. doi:10.2337/diaspect.23.4.272.
- Frank RN. Diabetic retinopathy. N Engl J Med. 2004;350(1):48–58. doi:10.1056/NEJMra021678.
- Warne D. Policy challenges in American Indian/Alaska Native health professions education. J Interprof Care. 2007;21(sup2):11–19. doi:10.1080/13561820701520426.
- GAO-19-74R. Indian health service: spending levels and characteristics of IHS and three other federal health care programs. December 10, 2018. https://www.gao.gov/assets/700/695871.pdf. Accessed April 21, 2020.
- Indian Health Service. IHS Profile. August 2020. https://www.ihs.gov/newsroom/factsheets/ihsprofile/. Accessed April 20, 2012.
- US Department of Agriculture, Economic Research Service. American Indians remain disproportionally rural. 2016. https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=77893. Accessed August 2019.
- Park D-W, Mansberger SL. Eye disease in patients with diabetes screened with telemedicine. Telemed J E Health. 2017;23(2):113–118. doi:10.1089/tmj.2016.0034.
- Newell SW, Tolbert B, Bennett J, Parsley TL. The prevalence and risk of diabetic retinopathy among Indians of southwest Oklahoma. J Okla State Med Assoc. 1989;82:414–424.
- Berinstein DM, Stahn RM, Welty TK, Leonardson GR, Herlihy JJ. The prevalence of diabetic retinopathy and associated risk factors among Sioux Indians. Diabetes Care. 1997;20(5):757–759. doi:10.2337/diacare.20.5.757.
- Lee ET, Russell D, Morris T, Warn A, Kingsley R, Ogola G. Visual impairment and eye abnormalities in Oklahoma Indians. Arch Ophthalmol. 2005;123(12):1699–1704. doi:10.1001/archopht.123.12.1699.
- Bursell SE, Fonda SJ, Lewis DG, Horton MB. Prevalence of diabetic retinopathy and diabetic macular edema in a primary care-based teleophthalmology program for American Indians and Alaskan Natives. PLoS One. 2018;13:e0198551. doi:10.1371/journal.pone.0198551.
- Silva PS, Horton MB, Clary D, et al. Identification of diabetic retinopathy and ungradable image rate with ultrawide field imaging in a national teleophthalmology program. Ophthalmology. 2016;123(6):1360–1367. doi:10.1016/j.ophtha.2016.01.043.
- Silva PS, Cavallerano JD, Tolls D, et al. Potential efficiency benefits of nonmydriatic ultrawide field retinal imaging in an ocular telehealth diabetic retinopathy program. Diabetes Care. 2014;37(1):50–55. doi:10.2337/dc13-1292.
- Aiello LP, Odia I, Glassman AR, et al. Comparison of early treatment diabetic retinopathy study standard 7-field imaging with ultrawide-field imaging for determining severity of diabetic retinopathy. JAMA Ophthalmol. 2019;137(1):65–73. doi:10.1001/jamaophthalmol.2018.4982.
- Singh RP, Hsueh J, Han MM, et al. Protecting vision in patients with diabetes with ultra-widefield imaging: a review of current literature. Ophthalmic Surg Lasers Imaging Retina. 2019;50(10):639–648. doi:10.3928/23258160-20191009-07.
- Silva PS, Cavallerano JD, Aiello LM, Aiello LP. Telemedicine and diabetic retinopathy: moving beyond retinal screening. Arch Ophthalmol. 2011;129(2):236–242. doi:10.1001/archophthalmol.2010.365.
- Sabanayagam C, Yip W, Ting DS, Tan G, Wong TY. Ten emerging trends in the epidemiology of diabetic retinopathy. Ophthalmic Epidemiol. 2016;23(4):209–222. doi:10.1080/09286586.2016.1193618.
- Fonda SJ, Bursell S-E, Lewis DG, Clary D, Shahon D, Horton MB. The Indian health service primary care-based teleophthalmology program for diabetic eye disease surveillance and management. Telemed J E Health. 2020;26(12):1466–1474. doi:10.1089/tmj.2019.0281.
- Li HK, Horton M, Bursell S-E, et al. Telehealth practice recommendations for diabetic retinopathy, second edition. Telemed J E Health. 2011;17(10):814–837. doi:10.1089/tmj.2011.0075.
- Horton MB, Brady CJ, Cavallerano J, et al. Practice guidelines for ocular telehealth-diabetic retinopathy, third edition. Telemed J E Health. 2020;26(4):495–543. doi:10.1089/tmj.2020.0006.
- Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—and extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98(5):786–806. doi:10.1016/S0161-6420(13)38012-9.
- Silva PS, Cavallerano JD, Sun JK, Noble J, Aiello LM, Aiello LP. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am J Ophthalmol. 2012;154(3):549–559. doi:10.1016/j.ajo.2012.03.019.
- Wilcosky TC, Chambless LE. A comparison of direct adjustment and regression adjustment of epidemiologic measures. J Chron Dis. 1985;38(10):849–856. doi:10.1016/0021-9681(85)90109-2.
- R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2003. ISBN 3-900051-07-0, http://www.R-project.org/.
- Zhang X, Saaddine JB, Chou C, et al. Prevalence of diabetic retinopathy in the United States, 2005-2008. JAMA. 2010;304(6):649–656. doi:10.1001/jama.2010.1111.
- Wilson C, Gilliland S, Cullen T, et al. Diabetes outcomes in the Indian health system during the era of the special diabetes program for Indians and the government performance and results act. Am J Public Health. 2005;95(9):1518–1522. doi:10.2105/AJPH.2004.053710.
- Silver K, Williams M, Macario E. The national eye health education program: increasing awareness of diabetic eye disease among American Indians and Alaska Natives. Ethn Dis. 2006;16:920–925.
- Norris T, Vines PL, Hoeffel EM The American Indian and Alaska Native population: 2010. 2010 Census Brief (C2010BR-10). January 2012. https://www.census.gov/library/publications/2012/dec/c2010br-10.html. Accessed August 20, 2020.
- UCLA Center for Health Policy Research. Health Disparities. American Indian and Alaska Native diabetes: critical information for researchers and policy-makers. May 2012. http://healthpolicy.ucla.edu/publications/Documents/PDF/AIANDiabetesmay2012.pdf. Accessed April 21, 2021.
- Cuadros J, Bresnick G. EyePACS: an adaptable telemedicine system for diabetic retinopathy screening. J Diabetes Sci Technol. 2009;3(3):509–516. doi:10.1177/193229680900300315.
- Lee ET, Lee VS, Kingsley RM, et al. Diabetic retinopathy in Oklahoma Indians with NIDDM: incidence and risk factors. Diabetes Care. 1992;15(11):1620–1627. doi:10.2337/diacare.15.11.1620.
- Rith-Najarian SJ, Valway SE, Gohdes DM. Diabetes in a Northern Minnesota Chippewa tribe: prevalence and incidence of diabetes and incidence of major complications, 1986-1988. Diabetes Care. 1993;16(1):266–270. doi:10.2337/diacare.16.1.266.
- Knowler WC, Bennett PH, Ballintine EJ. Increased incidence of retinopathy in diabetics with elevated blood pressure. A six-year follow-up study in Pima Indians. N Engl J Med. 1980;20:645–650. doi:10.1056/NEJM198003203021201.
- Silva PS, Dela Cruz AJ, Ledesma MG, et al. Diabetic retinopathy severity and peripheral lesions are associated with nonperfusion on ultrawide field angiography. Ophthalmology. 2015;122(12):2465–2472. doi:10.1016/j.ophtha.2015.07.034.
- Silva PS, Cavallerano JD, Haddad NM, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122(5):949–956. doi:10.1016/j.ophtha.2015.01.008.
- Aleo CL, Murchison AP, Dai Y, et al. Improving eye care follow-up adherence in diabetic patients with ocular abnormalities: the effectiveness of patient contracts in a free, pharmacy-based eye screening. Public Health. 2015;129(7):996–999. doi:10.1016/j.puhe.2015.05.012.
- Keenum Z, McGwin G Jr, Witherspoon CD, Haller JA, Clark ME, Owsley C. Patients’ adherence to recommended follow-up eye care after diabetic retinopathy screening in a publicly funded county clinic and factors associated with follow-up eye care use. JAMA Ophthalmol. 2016;134(11):1221–1228. doi:10.1001/jamaophthalmol.2016.3081.
