Abstract
Aims
To explore suggestions for clinicians on the most effective treatment for hydrosalpinx undergoing IVF-ET.
Materials and Methods
We reviewed 936 women with hydrosalpinx and 6715 tubal infertile women without hydrosalpinx who underwent IVF/ICSI between January 2014 and August 2019 in our center. Hydrosalpinx patients received different treatments including laparoscopic surgery (only salpingectomy and proximal tubal occlusion/ligation were included), ultrasonic-guided aspiration and hysteroscopic tubal occlusion. Outcomes were analyzed by One-way ANOVA, Chi-Square test and logistic regression.
Results
The live birth rate (LBR) of laparoscopic surgery was significantly higher compared with hydrosalpinx aspiration (48.3% vs 39.6%, p = .024). The cumulative live birth rate (CLBR) of subsequent laparoscopic surgery was significantly higher compared with subsequent hysteroscopic occlusion (65.1% vs 34.1%, p = .001) and no subsequent treatment (65.1% vs 44.9%, p < .005). Subsequent laparoscopic surgery significantly improved the CLBR of hydrosalpinx patients who received ultrasonic-guided aspiration and didn't get clinical pregnancy in fresh cycles (Odds Ratio (OR) =1.875; 95%CI = 1.041–3.378, p = .036).
Conclusions
Laparoscopic surgery leads to significantly higher LBR than ultrasonic-guided aspiration and significantly higher CLBR than hysteroscopic occlusion and no treatment.
Introduction
Tubal infertility accounts for 25% to 35% of female infertility [Citation1,Citation2]. Hydrosalpinx is a serious type of tubal disease [Citation3,Citation4], and tubal infertile patients with hydrosalpinx were proven to have negative consequences on pregnancy outcomes [Citation5–8]. Although salpingectomy was the most recommended treatment for hydrosalpinx in clinical practice [Citation9–13], there are also some other common treatments used for hydrosalpinx before IVF such as ultrasonic-guided hydrosalpinx aspiration, tubal sclerotherapy, hysteroscopic tubal occlusion and antibiotic treatment, etc [Citation9,Citation12–14].
Ultrasonic-guided hydrosalpinx aspiration was considered less invasive, safer, easier to perform under dense adhesion, and had a shorter hospital stay [Citation15]. Hydrosalpinx aspiration was also proven to improve pregnancy outcomes of hydrosalpinx patients [Citation16,Citation17] and it was also widely applied in clinical practice. Hysteroscopic occlusion was also proved to be an effective option for the management of hydrosalpinx in women before IVF [Citation18]. A cross-sectional survey of Society for Reproduction Endocrinology and Infertility(SREI)/Society of Reproductive Surgeons (SRS) members showed that although laparoscopic salpingectomy was the preferred method of surgical management, nearly one-half of members responded that hysteroscopic tubal occlusion should have a role as a primary method of intervention [Citation19]. However, a meta-analysis found ultrasonic-guided hydrosalpinx aspiration and hysteroscopic occlusion had lower LBR compared with salpingectomy [Citation12,Citation20]. So far, more evidence is needed to give advice to clinicians on the most effective treatment for hydrosalpinx before IVF-ET (in vitro fertilization and embryo transfer). Our retrospective study compared the baseline data and pregnancy outcomes of patients with hydrosalpinx from 2014 to 2019 in order to explore the effectiveness of laparoscopic surgery, ultrasonic-guided hydrosalpinx aspiration and hysteroscopic occlusion on pregnancy outcomes in patients with hydrosalpinx.
Materials and methods
Study design
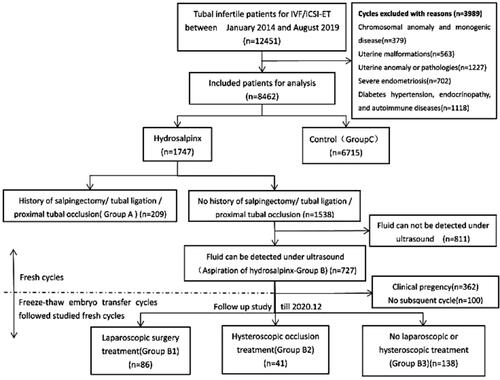
In our retrospective study, 12,451 tubal infertile patients who underwent IVF/ICSI-ET at the Reproductive Center of The First Affiliated Hospital of Zhengzhou University between January 2014 and August 2019 were included and 8462 of them meet our acceptance criteria. The laparoscopic surgery group was defined as Group A including 209 hydrosalpinx patients with a history of laparoscopic surgery such as salpingectomy, and proximal tubal occlusion/ligation. The aspiration group was defined as Group B including 727 hydrosalpinx patients with fluid that can be detected under ultrasound yet without a history of laparoscopic surgery. The control group was defined as Group C including 6715 tubal infertile patients without hydrosalpinx.
Hydrosalpinx patients who didn't get clinically pregnant after ultrasonic-guided aspiration and had subsequent freeze-thaw embryo transfer cycles till December 2020 were included in the follow-up research. Subsequent laparoscopic surgery group was defined as Group B1 including 86 hydrosalpinx patients who received subsequent laparoscopic surgery treatment. The hysteroscopic occlusion group was defined as Group B2 including 41 hydrosalpinx patients who received subsequent hysteroscopic occlusion treatment. No treatment group was defined as Group B3 including 138 hydrosalpinx patients who received neither subsequent laparoscopic surgery treatment nor hysteroscopic occlusion treatment.
Inclusion criteria and exclusion criteria
The inclusion criteria were as follows [Citation1]: tubal infertility women with age ≤40 years, BMI < 30 kg/m2 [Citation2], at least one high-quality embryo (blastocyst morphology score ≥3BB or embryo level Ι or ΙΙ) transferred [Citation3], no history of intrauterine manipulation in the past 3 months [Citation4], not in the oocyte donation program [Citation5], not with preimplantation genetic diagnosis (PGD).
The exclusion criteria were as follows [Citation1]: chromosomal anomaly and monogenic disease [Citation2], uterine malformations [Citation3], uterine anomaly or pathologies such as intrauterine adhesion, endometrial polyps or endometrial hyperplasia [Citation4], severe endometriosis (grade III and IV) [Citation5], diabetes, hypertension, endocrinopathy, and autoimmune diseases [Citation6], undetectable fluid under ultrasound [Citation7], no subsequent cycle after aspiration due to pregnancy or personal reason.
Outcome measurements
The primary outcome measures of this study were LBR and CLBR while the secondary outcome measures were clinical pregnancy rate (CPR), cumulative clinical pregnancy rate (CCPR), implantation rate, multiple pregnancy rate, miscarriage rate, and ectopic pregnancy rate. LBR was calculated as the ratio of the number of live-born events divided by the number of transferred cycles. The cumulative live birth rate (CLBR) was calculated as the ratio of the number of patients whose freeze-thaw embryo transfer cycles following this studied fresh cycle had live-born events till December 2020 divided by the number of included patients in a subsequent study. Clinical pregnancy was defined as at least one intrauterine gestational sac detected by ultrasound 5 or 6 weeks after embryo transfer. The cumulative clinical pregnancy was defined as at least one intrauterine gestational sac detected by ultrasound 5 or 6 weeks after all freeze-thaw embryo transfer following this studied fresh cycle till December 2020.
ART procedures
Controlled ovarian hyperstimulation protocols were determined according to each patient's characteristics (age, body mass index (BMI), antral follicle count (AFC), and AMH [Citation21]. We regularly monitored follicle growth by trans-vaginal ultrasound and the serum estradiol, progesterone and LH levels during the cycle. When 1 dominant follicle diameter ≥ 20 mm, 3 follicles ≥ 17 mm in diameter, or 2 ∼ 3 follicles with a diameter ≥16 mm, different procedures such as Aizer 250 μg or hCG 5000–10,000 U et al. were used for trigger. Oocyte retrievals were done 36 h later, and subsequent fresh embryo transfers were performed on day 3 or 5. Progesterone (60 mg) was injected intramuscularly on the day of oocyte retrieval. Progesterone gel (Xenotong, Merck Sherano, Switzerland) and oral dydrogesterone (10 mg (Duphaston); Solvay Pharmaceuticals B.V., Veenendaal, The Netherlands) were given vaginally from the day of embryo transfer for luteal phase support.
Treatments
Patients received laparoscopic surgery before fresh cycles or freeze-thaw embryo transfer cycles. Laparoscopic surgery mentioned here only included salpingectomy or proximal tubal occlusion/ligation. Salpingostomy or other surgery was excluded. Salpingectomy directly removes the fluid, while proximal tubal occlusion uses electrocoagulation or ligature suture to cut off the interstitial part and the isthmus of the fallopian tube to block the reflux of fluid into the uterine cavity.
Ultrasound-detectable hydrosalpinx was defined as a sausage-like tubular anechoic image detected by ultrasound. Bilateral hydrosalpinx means an anechoic image detected on both sides of the slapinges of one patient. Ultrasonic-guided aspiration was conducted during oocyte retrieval procedure in fresh cycles. An ultrasound puncture needle was used to remove the fluid in the fallopian tube away.
Hysteroscopic tubal occlusion was conducted before freeze-thaw embryo transfer cycles. Before the freeze-thaw embryo transfer cycles, the Essure intrauterine device was placed under the hysteroscope to block the fallopian tubes and block reflux.
Statistical analysis
Continuous data were presented as mean ± SD(Standard Deviation). Difference comparison would be tested by One-way ANOVA, and LSD test or Tamhane T2 test were used to put up multiple comparisons. Qualitative variables were given in frequency. Differences among groups would be tested by Chi-Square test. To adjust the influence of potential confounders, logistic regression analyses were performed. All statistical analyses were performed using SPSS (version 22.0; IBM Corp., Armonk, NY, USA) software. A statistically significant difference was defined as p < .05. In logistic regression analyses, odds ratio (OR) and their 95% confidence intervals (95% CI) were calculated from the model's coefficients and their standard deviations.
Results
Patient and cycle characteristics
There were 12,451 tubal infertile women who meet our inclusion criteria undergoing IVF/ICSI cycle in our centre between January 2014 and August 2019. A total of 3989 patients were excluded from the study according to the exclusion criteria. The grouping is presented in .
Patient and IVF/ICSI cycle characteristics of groups are presented in . The duration of infertility of the aspiration group (Group B) was significantly longer compared with the control group (Group C) (4.7(3.5) vs 4.0(3.0), p < .001), and the primary infertility rate of Group B was significantly increased compared with both Group C (43.6% vs 36.5%, p < .001) and Group A (43.6% vs 35.9%, p = .046). The endometrial thickness, Gn dosage (IU), the rate of IVF and the rate of two embryos transferred to Group B were significantly higher than the control group. Both Group A and Group B had significantly higher FSH compared with Group C, and Group A had significantly lower AMH and higher Gn dosage (IU) compared with Group C. The rate of bilateral hydrosalpinx in Group A was significantly higher than in Group B (23.9% vs 7.6%, 2 p < .001). The percentage of long/super long protocol used in Group B (97.8% vs 95.2%, p = .045) and Group C (97.9% vs 95.2%, p = .016) were significantly higher than in Group A. The age, BMI, number of oocytes retrieved and the stage of embryos transferred did not differ in these three groups (p > .05).
Table 1. Characteristics of tubal infertile patients with or without hydrosalpinx.
IVF outcomes
The pregnancy outcomes of the groups are listed in . The pregnancy outcomes of Group A were similar compared with Group C. Compared with Group C, Group B had significantly lower biochemical pregnancy rate (53.5.1% vs 63.7%, p < .001), implantation rate (32.1% vs 43.6%, p < .001), CPR (49.8% vs 59.5%, p < .001), and LBR (39.6% vs 51.1%, p < .001), and significantly higher ectopic pregnancy rate (7.7% vs 2.3%, p < .001). It is worth noticing that the LBR was significantly higher (48.3% vs 39.6%, p = .024) in Group A compared with Group B. There were no differences in the multiple pregnancy rate and miscarriage rate in the three groups (p > .05). shows the main results of the logistic regression analysis. The following variables were found to be independently associated with the LBR of tubal infertile patients: age (OR = 0.947; 95% CI: [0.931–0.964], p < 0.001); duration of infertility (OR = 0.958; 95% CI: [0.936–0.982], p = .001); type of infertility (OR = 1.199; 95% CI: [1.037–1.386], p = .014); endometrial thickness (OR = 1.096; 95% CI: [1.067–1.126], p < .001); number of embryos transferred (OR = 1.705; 95% CI: [1.430–2.033], p < 0.001) and hydrosalpinx aspiration compared to control group (OR = 0.672; 95% CI: [0.563–0.802], p < .001).
Table 2. Pregnancy outcomes of tubal infertile patients with or without hydrosalpinx.
Table 3. Logistic regression analysis of the risk factors affecting the live birth rate of tubal infertile patients of IVF/ICSI-ET.
Baseline characteristics and outcomes of follow-up patients
As for all patients who had received ultrasonic-guided aspiration (Group B) but did not get clinically pregnant, we conducted follow-up research on their freeze-thaw embryo transfer cycles and followed these studied fresh cycles until 2020.12. shows baseline characteristics and cumulative freeze-thaw embryo transfer cycle pregnancy outcomes of the patients. No differences were observed in age, BMI, AMH, Gn dosage in fresh cycles, recurrent rate of hydrosalpinx, bilateral hydrosalpinx rate, IVF rate and primary infertility rate in these three groups (p > .05). The duration of infertility was different in three groups (p = .038), and the duration of infertility of groupB3 was significantly higher than groupB1 (5.3 ± 3.8 vs 3.9 ± 3.2, p = .029). The CCPR (70.9% vs 34.1%/51.4%, p < .005) and CLBR (65.1% vs 34.1%/44.9%, p < .005) were significantly higher in the laparoscopic surgery group (Group B1) compared with both hysteroscopy occlusion group (Group B2) and control group (Group B3). However, no difference was observed in the CCPR and CLBR in Group B2 and Group B3 (p > .05). describes the variables that were independently associated with the CLBR of hydrosalpinx patients who didn't get pregnant after aspiration: age (OR =0.911; 95% CI: [0.860–0.964], p = .001) and having subsequent laparoscopic surgery compared with no treatment (OR =1.875; 95% CI = 1.041–3.378, p = .036).
Table 4. Cumulative pregnancy outcomes of the freeze-thaw embryo transfer cycles of hydrosalpinx patients who didn't get clinical pregnancy after aspiration in fresh cycles.
Table 5. Logistic regression analysis of the risk factors affecting the cumulative live birth rate of the freeze-thaw embryo transfer cycles of hydrosalpinx patients who didn't get clinical pregnancy after aspiration.
Discussion
Hydrosalpinx is one of the most serious tubal disorders that adversely affect the outcomes of assisted reproductive technologies (ART) [Citation3–8]. The occlusion of the distal end of the fallopian tube leads to fluid accumulation, which directly enters and contaminates the uterine cavity, adversely resulting in decreased endometrial receptivity [Citation22–24], contributing to the unsynchronized status of the embryo and the endometrium [Citation25], preventing the successful implantation of embryos produced by IVF [Citation4,Citation26] or it can indirectly by causing toxic effects on implanted embryos to cause embryonic developmental disorders [Citation26–28]. The presence of fluid in the fallopian tubes can disrupt their normal function, including the transport of the embryo toward the uterus. What's more, hydrosalpinx can affect the hormonal environment in the reproductive system, which is crucial for embryo implantation. Patients with hydrosalpinx had significantly lower implantation and pregnancy rates and a higher incidence of spontaneous abortion and ectopic pregnancy compared to other types of tubal disease [Citation3,Citation24,Citation29]. In clinical practice, laparoscopic salpingectomy surgery was proven to be effective for hydrosalpinx patients and can increase the chance of clinical pregnancy [Citation6,Citation14,Citation30,Citation31]. Proximal tubal occlusion was also proved to result in similar improvement in IVF outcome in patients with hydrosalpinx [Citation12,Citation32]. Our study showed significantly higher LBR and CLBR of the laparoscopic surgery group and confirmed previous theories and provide support for laparoscopic surgery to be the preferred treatment of hydrosalpinx before IVF. However, salpingectomy may affect ovarian blood supply and thus reduce ovarian response in subsequent ART cycles [Citation33,Citation34], which can be reconfirmed by the lower AMH and higher FSH of the laparoscopic group in our study. More use of GnRH-Ant/Mild stimulation/Natural protocol in patients with a history of laparoscopic salpingectomy or proximal tubal occlusion surgery might also support the adverse effects of surgery on ovarian response. More research should be conducted to study the long-term effects of laparoscopic surgery on ovarian response.
Multiple previous randomized controlled trials (RCTs) and retrospective studies have found that trans-vaginal ultrasonic aspiration also improved pregnancy rates after embryo transfer compared with non-aspiration patients [Citation12,Citation16,Citation17]. However, a 20–30% recurrence rate of hydrosalpinx was also found within 2 weeks after aspiration which adversely affected the outcomes of aspiration [Citation12,Citation35]. In our study, we defined hydrosalpinx recurrence as detectable ultrasonic images with tube-like anechoic after treatment. We found no significant differences in the recurrence rate of the three follow-up groups. A possible reason is that laparoscopic surgery cut off the interstitial part and the isthmus of the fallopian tube. It blocked the reflux of fluid into the uterine cavity and caused better clinical outcomes but the hydrosalpinx which is recurrent in broken ends can still be detected by trans-vaginal ultrasonic examination. What is more, the LBR and CPR in the salpingectomy group were significantly higher than the aspiration group was also proved by several meta-analyses [Citation12,Citation15].
Hysteroscopic occlusion was used for hydrosalpinx patients [Citation18,Citation20]. The CPR, IR and LBR of hysteroscopic occlusion were significantly lower than those of the laparoscopic surgery which had been proved by a review and a meta-analysis [Citation20,Citation36]. An RCT research conducted by K. Dreyer and colleagues advised salpingectomy remaining the procedure of choice for hydrosalpinx patients after comparing hysteroscopic proximal tubal occlusion and laparoscopic salpingectom [Citation37].
For hydrosalpinx patients who didn't get pregnant in fresh cycles in the aspiration group, subsequent laparoscopic surgery before freeze-thaw embryo transfer cycles highly increased cumulative outcomes of them than hysteroscopic occlusion and no treatment. Our results suggest that laparoscopic surgery like salpingectomy or proximal tubal occlusion/ligation significantly improves outcomes of hydrosalpinx patients undergoing IVF-ET. For hydrosalpinx patients, having laparoscopic surgery before fresh cycles improves live birth outcomes. What's more, for hydrosalpinx patients who didn't get pregnancy in fresh cycles, having subsequent laparoscopic surgery before freeze-thaw embryo transfer cycles highly increases cumulative outcomes in long-term consideration.
In conclusion, laparoscopic surgery is more effective for hydrosalpinx patients and leads to significantly higher LBR than ultrasonic-guided aspiration and significantly higher CLBR than hysteroscopic occlusion and no treatment. We highly recommend laparoscopic surgery as a preferred treatment for hydrosalpinx patients.
Author contributions
Beibei Bi and Xiao Han were responsible for collecting data and analyzing the data and they were the major contributors to the manuscript writing. LinLi Hu was the supervisor. All other authors participated in the invention of the study design and critically reviewed the concept of the study.
Acknowledgments
We are grateful to Prof. Aaron JW Hsueh (Stanford University School of Medicine) for reviewing the English language of the manuscript. We also thank Xiaoyi Guo from the Medical School of California Institute of Technology for her advice on data analysis and manuscript writing.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Additional information
Funding
References
- G M H, A E H, R S S. Pathophysiology and management of proximal tubal blockage. Fertil Steril. 1999;71(5):1–6. doi:10.1016/s0015-0282(99)00014-x.
- Serafini P, Batzofin J. Diagnosis of female infertility. A comprehensive approach. J Reprod Med. 1989;34(1):1–6.
- Andersen AN, Yue Z, Meng FJ, et al. Low implantation rate after in-vitro fertilization in patients with hydrosalpinges diagnosed by ultrasonography. Hum Reprod. 1994;9(10):1935–1938. doi:10.1093/oxfordjournals.humrep.a138362.
- Melo P, Georgiou EX, Johnson N, et al. Surgical treatment for tubal disease in women due to undergo in vitro fertilisation. Cochrane Database Syst Rev. 2020;10(10):CD002125. doi:10.1002/14651858.CD002125.pub4.
- Camus E, Poncelet C, Goffinet F, et al. Pregnancy rates after in-vitro fertilization in cases of tubal infertility with and without hydrosalpinx: a meta-analysis of published comparative studies. Hum Reprod. 1999;14(5):1243–1249. doi:10.1093/humrep/14.5.1243.
- Asrm PCO. Salpingectomy for hydrosalpinx prior to in vitro fertilization. Fertil. Steril. 2008;90(5):S66–S68. doi:10.1016/j.fertnstert.2008.08.089.
- Ng K, Cheong Y. Hydrosalpinx - Salpingostomy, salpingectomy or tubal occlusion. Best Pract Res Clin Obstet Gynaecol. 2019;59:41–47. doi:10.1016/j.bpobgyn.2019.01.011.
- Schlaff WD. A reconsideration of salpingectomy for hydrosalpinx before in vitro fertilization: why bother? Fertil Steril. 2019;111(4):650–651. doi:10.1016/j.fertnstert.2019.02.014.
- Asrm PCOT. Role of tubal surgery in the era of assisted reproductive technology: a committee opinion. Fertil. Steril. 2015;103(6):e37-43. doi:10.1016/j.fertnstert.2015.03.032.
- Chu J, Harb HM, Gallos ID, et al. Salpingostomy in the treatment of hydrosalpinx: a systematic review and meta-analysis. Hum Reprod. 2015;30(8):1882–1895. doi:10.1093/humrep/dev135.
- Johnson N, van Voorst S, Sowter MC, et al. Surgical treatment for tubal disease in women due to undergo in vitro fertilisation. Cochrane Database Syst Rev. 2010;2010(1):CD002125. doi:10.1002/14651858.CD002125.pub3.
- Volodarsky-Perel A, Buckett W, Tulandi T. Treatment of hydrosalpinx in relation to IVF outcome: a systematic review and meta-analysis. Reprod Biomed Online. 2019;39(3):413–432. doi:10.1016/j.rbmo.2019.04.012.
- Xiaona Lin GHHS. Chinese expert consensus on diagnosis and treatment of tubal infertility. J. Reprod. Med. 2018;27(11):1048–1056. doi:10.3969/j.issn.1004-3845.2018.11.002.
- Uk NCCF. Fertility: assessment and treatment for people with fertility problems. Royal College of Obstetricians & Gynaecologists, London. 2013.
- Tsiami A, Chaimani A, Mavridis D, et al. Surgical treatment for hydrosalpinx prior to in-vitro fertilization embryo transfer: a network meta-analysis. Ultrasound Obstet Gynecol. 2016;48(4):434–445. doi:10.1002/uog.15900.
- Hammadieh N, Coomarasamy A, Ola B, et al. Ultrasound-guided hydrosalpinx aspiration during oocyte collection improves pregnancy outcome in IVF: a randomized controlled trial. Hum Reprod. 2008;23(5):1113–1117. doi:10.1093/humrep/den071.
- Zhou Y, Jiang H, Zhang WX, et al. Ultrasound-guided aspiration of hydrosalpinx occurring during controlled ovarian hyperstimulation could improve clinical outcome of in vitro fertilization-embryo transfer. J Obstet Gynaecol Res. 2016;42(8):960–965. doi:10.1111/jog.13013.
- Arora P, Arora RS, Cahill D. Essure(®) for management of hydrosalpinx prior to in vitro fertilisation-a systematic review and pooled analysis. BJOG. 2014;121(5):527–536. doi:10.1111/1471-0528.12533.
- Omurtag K, Grindler NM, Roehl KA, et al. How members of the society for reproductive endocrinology and infertility and society of reproductive surgeons evaluate, define, and manage hydrosalpinges. Fertil Steril. 2012;97(5):1095–1100. doi:10.1016/j.fertnstert.2012.02.026.
- D'Arpe S, Franceschetti S, Caccetta J, et al. Management of hydrosalpinx before IVF: a literature review. J Obstet Gynaecol. 2015;35(6):547–550. doi:10.3109/01443615.2014.985768.
- Hu L, Bu Z, Guo Y, et al. Comparison of different ovarian hyperstimulation protocols efficacy in poor ovarian responders according to the Bologna criteria. Int J Clin Exp Med. 2014;7(4):1128–1134.
- Seli E, Kayisli UA, Cakmak H, et al. Removal of hydrosalpinges increases endometrial leukaemia inhibitory factor (LIF) expression at the time of the implantation window. Hum Reprod. 2005;20(11):3012–3017. doi:10.1093/humrep/dei188.
- Ersahin AA, Ersahin S, Gungor ND. Surgical removal of hydrosalpinx improves endometrium receptivity by decreasing nuclear factor-kappa B expression. Reprod Sci. 2020;27(3):787–792. doi:10.1007/s43032-019-00136-y.
- Strandell A, Waldenström U, Nilsson L, et al. Hydrosalpinx reduces in-vitro fertilization/embryo transfer pregnancy rates. Hum Reprod. 1994;9(5):861–863. doi:10.1093/oxfordjournals.humrep.a138606.
- Ajonuma LC, Ng EH, Chan HC. New insights into the mechanisms underlying hydrosalpinx fluid formation and its adverse effect on IVF outcome. Hum Reprod Update. 2002;8(3):255–264. doi:10.1093/humupd/8.3.255.
- Mukherjee T, Copperman AB, McCaffrey C, et al. Hydrosalpinx fluid has embryotoxic effects on murine embryogenesis: a case for prophylactic salpingectomy. Fertil Steril. 1996;66(5):851–853. doi:10.1016/s0015-0282(16)58652-x.
- Bao H, Qu Q, Huang X, et al. Impact of hydrosalpinx fluid on early human embryos. Syst Biol Reprod Med. 2017;63(4):279–284. doi:10.1080/19396368.2017.1319993.
- Ng EH, Ajonuma LC, Lau EY, et al. Adverse effects of hydrosalpinx fluid on sperm motility and survival. Hum Reprod. 2000;15(4):772–777. doi:10.1093/humrep/15.4.772.
- Vandromme J, Chasse E, Lejeune B, et al. Hydrosalpinges in in-vitro fertilization: an unfavourable prognostic feature. Hum Reprod. 1995;10(3):576–579. doi:10.1093/oxfordjournals.humrep.a135992.
- Strandell A, Lindhard A, Waldenström U, et al. Hydrosalpinx and IVF outcome: a prospective, randomized multicentre trial in Scandinavia on salpingectomy prior to IVF. Hum Reprod. 1999;14(11):2762–2769. doi:10.1093/humrep/14.11.2762.
- Strandell A, Lindhard A, Waldenström U, et al. Hydrosalpinx and IVF outcome: cumulative results after salpingectomy in a randomized controlled trial. Hum Reprod. 2001;16(11):2403–2410. doi:10.1093/humrep/16.11.2403.
- Kontoravdis A, Makrakis E, Pantos K, et al. Proximal tubal occlusion and salpingectomy result in similar improvement in in vitro fertilization outcome in patients with hydrosalpinx. Fertil Steril. 2006;86(6):1642–1649. doi:10.1016/j.fertnstert.2006.05.032.
- Gelbaya TA, Nardo LG, Fitzgerald CT, et al. Ovarian response to gonadotropins after laparoscopic salpingectomy or the division of fallopian tubes for hydrosalpinges. Fertil Steril. 2006;85(5):1464–1468. doi:10.1016/j.fertnstert.2005.10.036.
- Almog B, Wagman I, Bibi G, et al. Effects of salpingectomy on ovarian response in controlled ovarian hyperstimulation for in vitro fertilization: a reappraisal. Fertil Steril. 2011;95(8):2474–2476. doi:10.1016/j.fertnstert.2011.03.032.
- Fouda UM, Sayed AM. Effect of ultrasound-guided aspiration of hydrosalpingeal fluid during oocyte retrieval on the outcomes of in vitro fertilisation-embryo transfer: a randomised controlled trial (NCT01040351). Gynecol Endocrinol. 2011;27(8):562–567. doi:10.3109/09513590.2010.507290.
- Xu B, Zhang Q, Zhao J, et al. Pregnancy outcome of in vitro fertilization after essure and laparoscopic management of hydrosalpinx: a systematic review and meta-analysis. Fertil Steril. 2017;108(1):84–95.e5. doi:10.1016/j.fertnstert.2017.05.005.
- Dreyer K, Lier MC, Emanuel MH, et al. Hysteroscopic proximal tubal occlusion versus laparoscopic salpingectomy as a treatment for hydrosalpinges prior to IVF or ICSI: an RCT. Hum Reprod. 2016;31(9):2005–2016. doi:10.1093/humrep/dew050.