Abstract
Lean in healthcare has continued to attract practitioner and research interest over the past two decades yet lacks evidence of sustained application. This longitudinal case study examines Lean healthcare interventions through the lens of Programme Theory, to provide an understanding of the design and implementation of a Lean programme. Through a qualitative single case study of an NHS organisation implementing Lean, content analysis of 70 reports from a 6-year period was undertaken and supported by interview data from 12 respondents involved in Lean initiatives. Through Programme Theory, we identify contextual moderators, internal and external, informing the design and development of Lean efforts. The key to successful and sustained Lean efforts is staff acceptance of the Programme Theory for delivering and maintaining outcomes. This has been identified as a key social determinant for Lean sustainability. Results from the research provide practical implications for designing a programme that accommodates resource challenges while incorporating multiple contextual drivers. The case study highlights an organisation’s Lean journey and the best practices that evolved; however, further longitudinal investigations are required to validate the findings.
Keywords:
1. Introduction
The application of Lean within healthcare continues to be debated for applicability, its impact as healthcare policy (Gadolin Citation2019) and questioned for sustainability (Bortolotti et al. Citation2018).
Since the 2000s, the Lean improvement agenda has been applied in healthcare across the globe (Radnor, Holweg, and Waring Citation2012; Toussaint and Berry Citation2013; Al Owad et al. Citation2018). In the context of healthcare, Lean was recognised as having the potential to lower waiting times, improve service levels and reduce costs (Jones and Mitchell Citation2006). This agenda appears to be providing a potential way forward for health service managers, especially for those in the National Health Service (NHS) in the UK who face pressure from growing demand, patients who have heightened service expectations (compounded by government published targets), and tighter budget constraints (Matthias and Brown Citation2016; Samuel, Found, and Williams Citation2015).
There continues to be a focus on positive reporting of Lean interventions which highlights the opportunities open to the NHS and other healthcare organisations globally if they can successfully implement the concept. Roemeling, Land, and Ahaus (Citation2017) recorded improved laboratory throughput times in the Netherlands. Haddad et al. (Citation2016) found that applying Lean lowered waiting time in Lebanon and India. Bhat and Jnanesh (Citation2014) reported shorter cycle times in outpatients. Despite such successes and endorsement that there should be a systemic approach to Lean (Bowerman and Fillingham Citation2007; Radnor, Holweg, and Waring Citation2012), the existing evidence base continues to refer to examples of Lean ‘projects’ at their early stage of implementation (Al Owad et al. Citation2018) with limited assessment of Lean sustainability (Mazzocato et al. Citation2014; Hallam and Contreras Citation2018). It is not always clear beyond description of tools applied, how the Lean intervention was designed, monitored/modified and then evaluated for sustainability (Roemeling, Land, and Ahaus Citation2017, 142). This is particularly important for healthcare, which is often influenced by external contextual factors (e.g. government wait time targets and focus on priority areas) which can impact the direction and focus of improvement activities. As a result, Hallam and Contreras (Citation2018) in considering the contextual factors affecting healthcare, as well as the reporting on Lean in healthcare and the minimal evidence of sustainability, suggest the development of healthcare transformation roadmaps for each system to support sustainability. Sustainability requires a constant and lengthy learning process for managers (Maalouf and Gammelgaard Citation2016) but given the lack of long-term examples of Lean sustainability in healthcare, assessment and learning from the process is still in progress. Through examining longitudinal evidence, this research investigates the barriers and drivers of Lean sustainability including ‘respect for people’ (Monden Citation1983), resources (Adebanjo, Laosirihongthong, and Samaranayake Citation2016) and sharing of best practice (Sinha and Kohnke Citation2009). Developing an understanding of why Lean interventions in a healthcare setting sustain or dissipate over time, is required.
In evaluation and improvement science, how interventions are designed and then evaluated is articulated through Programme Theory. Reed et al. (Citation2014, 1041) define Programme Theory (PT) as ‘the articulation of an overall aim, potential intervention(s) that will be tested in an attempt to achieve this aim, hypothesised cause/effect relationships linking intervention(s) to the aim and measure concepts that link to the cause/effect chains to support evaluation’. PT offers two potential benefits for researchers. It can articulate the theory for how programme interventions are to work and deliver outcomes (Davidoff et al. Citation2015) and can also be used for evaluation of programme interventions (Lipsey and Cordray Citation2000; Donaldson Citation2005; Goicolea et al. Citation2015). This is particularly important, as PT evaluations can capture cultural, individual and team influences on interventions through acknowledging the complexity of the context and its inherent subtleties (Albaek Citation1989; Dahler-Larsen Citation2001; Goicolea et al. Citation2015). For healthcare, a PT lens provides the opportunity to understand how Lean interventions progress within an environment which is responsive to the needs of its patients and government. External contextual moderators are important as healthcare is a significant area of focus for politicians, lobbying groups and funding bodies. Planning changes within this environment is challenging for managers as they must balance the demands and issues that arise from the internal context of a resource-driven structure (Walley Citation2013). Within healthcare, specialists such as surgeons, are risk adverse and challenge any changes that may alter understood and tested processes (Aitken, Esain and Williams Citation2021). Cross-functional teams face similar cultural issues due to professional demarcations (Lindsay, Kumar, and Juleff Citation2020).
The overall aim of this paper is to assess a longitudinal Lean implementation programme through a PT lens to evaluate the sustainability of the Lean efforts undertaken and the approaches deployed. This research contributes to the existing knowledge in two ways. Firstly, the longitudinal assessment of interventions and outcomes, supported the evaluation of Lean as a sustainable improvement approach in healthcare. Through the lens of PT, an understanding of the design and barriers and drivers for implementation of Lean were examined. This allowed for the evaluation of sustainability. For Lean and continuous improvement initiatives to be successful, fidelity to one approach was found to be essential for supporting and sustaining over the longer term, though this is recognised as challenging (Jabbal Citation2017). Secondly, by examining an established Lean programme and the organisations PT, the importance of contextual moderators in programme design were identified.
Within the case study organisation, Lean interventions were known as ‘projects’ which represented a series of activities and interventions, over a period that underpinned the Lean effort related to the programme of work. The data comes from annual Lean programme reports and provide summaries of projects undertaken by the Lean project teams.
To provide these insights, this paper is structured as follows: in the next section, we review the literature on Lean in healthcare including an assessment of projects reported, implementation challenges and sustainability. PT will be introduced, as will the logic model underpinning this study. The methodology is then presented, followed by findings, discussion, and the conclusion.
2. Literature review
2.1. Lean interventions in healthcare
With the explosion of Lean literature in the 2000s, Brandão de Souza (Citation2009) was one of the first to provide a categorisation of Lean healthcare case studies. He recognised reports as falling into three main areas: Manufacturing like case studies (like contained manufacturing environments such as laundry, radiology, pathology, pharmacy); Managerial and Support (IT, medical secretaries, finance) and Patient Flow (length of stay, waiting list initiatives) (Brandão de Souza Citation2009). Where varied projects are reported, these are across multiple organisations rather than in-depth reporting of systemic application of Lean in one organisation (Graban Citation2013; Hallam and Contreras Citation2018).
System-wide studies in the NHS of Lean, which cross-departmental boundaries have been rare (Radnor and Osborne Citation2013), though hospital wide studies are increasing (Burgess and Radnor Citation2013; Costa and Godinho Filho Citation2016). What has been evident and highlighted as a recurring issue in the NHS is a piecemeal approach to Lean, with a focus on the application of tools and techniques. This focus on tools and techniques comes at the expense of a system-wide, holistic application of the Lean concept Matthias and Brown Citation2016; Roemeling, Land, and Ahaus Citation2017). Through a focus on minimising waste in processes and maximising the value-added, organisations can improve their performance in terms of cost, quality, and time (Bicheno Citation2008). This focus on wastes commonly comes at the expense of a focus on variability (Schmenner Citation2015; Roemeling, Land, and Ahaus Citation2017). Panwar et al. (Citation2015) reflect that Lean is a positive contributor to all types of organisations provided it is appropriately adapted to the environment being implemented within. The call for context dependency is critical given the highly professionalised environments and the political influences evident in healthcare delivery systems, in comparison to other sectors (Klein Citation2010).
2.2. Success factors and barriers in lean implementation
Although calls for context dependency are not new, they do inform the success factors that are recognised in Lean such as leadership, culture, strategy, the implementation process, and those involved (D’Andreamatteo et al. Citation2015; Noori Citation2015). Strategy in Lean implementations is an important area. Being able to communicate the vision and development and support information flows across and between organisational boundaries and hierarchical structures are viewed as instrumental in sustaining improvements (Tracey and Flinchbaugh Citation2006). With the general focus of Lean research having been on the operational instruments of continuous improvement, scholars reviewing original literature turned their attention to studying the ‘respect for people’ pillar of the Toyota way (Monden Citation1983; Ohno Citation1988). The use of Lean tools and techniques represents only 20% of the effort required in implementing Lean with the other 80% relating to changing the mind-set, culture, and soft skills of Lean leaders (Mann Citation2009). Haddad et al. (Citation2016, 221) similarly highlight the necessity to address social aspects as ‘Lean implementation typically requires continuous improvement of the social, as well as the technical systems’. Soft practices have been evaluated as critical for successful implementation in industrial contexts and can overcome some of the poor results associated with approaches which predominately focus on tools and techniques (Lander and Liker Citation2007; Matsui Citation2007). Later work supports this, by advocating that those successful Lean businesses are defined by their use of soft practices including activities related to ‘principles, managerial concepts, people, and relations’ (Bortolotti, Boscari, and Danese Citation2015, 184).
Within the healthcare context, ‘respect for people’ continues to be highlighted as a critical success factor in the implementation of Lean. This includes factors such as leadership, communication, autonomous working, and openness being at the forefront (Mannon Citation2014; Matthias and Brown Citation2016). Leadership is achieved through the delivery of a clear vision, providing the infrastructure to deliver training and problem solving, and appointing Lean champions to deliver bottom-up improvements (Eriksson Citation2017). Part of Lean improvement is standardisation (Ohno Citation1988) and through standardisation of processes and work routines in healthcare, Lean provides the opportunity for organisations to remove/reduce waste (Ballé and Régnier Citation2007).
2.2.1. Barriers evident in Lean implementation
However, where success factors are identified, it is not uncommon for the same factors to be also considered as barriers such as culture, leadership, strategy, the implementation process, and the human resources involved in Lean (D’Andreamatteo et al. Citation2015). Leite, Bateman, et al. (Citation2020) go onto focus on barriers for Lean in Healthcare, arguing that although there is much discussion on barriers, these have not been explored in depth, or clearly articulated. They categorise barriers as being ostensible but also through case study data, provide evidence of the barriers which are less visible, including those which focus on people involved in healthcare (patients, staff) and the healthcare context of the delivery system (Leite, Bateman, et al. Citation2020).
Establishing an environment characterised by openness to experimentation, driven by employee contributions, is critical in the development of Lean best practices (Ohno Citation1988). Healthcare organisations are complex, have clear hierarchical structures and are characterised by regulatory systems, which can influence Lean participants in whether they are feeling psychologically safe to discuss errors or embrace best practice (Guo and Hariharan Citation2012; Eriksson Citation2017; van Dun, Hicks, and Wilderom Citation2017; Lindsay, Kumar, and Juleff Citation2020; Aitken, Esain and Williams Citation2021). Although there are limited studies on psychological safety in healthcare, the healthcare culture, professional hierarchies, and leadership are viewed as being a barrier to employees at all levels being able to demonstrate psychological safety in sharing ideas and opinions (Remtulla et al. Citation2021). This in turn influences bottom-up improvement.
Although autonomous working is endorsed through respect for people (Monden Citation1983), research has also highlighted autonomous working as further area of complexity within Lean in healthcare. In healthcare, what is more difficult is standardising repetitive work without compromising the need to provide tailored and personalised treatment to patients, as this results in questioning the applicability of the concept in healthcare (Waring and Bishop Citation2010; Roemeling, Land, and Ahaus Citation2017). Despite earlier advocates calling for standardisation as part of stabilisation and readiness for Lean (Ballé and Régnier Citation2007), process standardisation can reduce the autonomy of professionals’ decision-making which is essential in delivering patient care and respecting the unique nature of each patient (Waring and Bishop Citation2010; Guo and Hariharan Citation2012; Mannon Citation2014; McCann et al. Citation2015). This can lead to resistance by professionals who undermine attempts to make their work more transparent and predictable through standardisation (Radnor and Osborne Citation2013). Standardisation has been shown to be beneficial in healthcare when professionals still have discretion to alter patients care plans if needed Eriksson Citation2017). However, the management of process simplification/standardisation versus motivational job design (self-motivation) continues to be a paradoxical issue faced by all organisations implementing Lean (Maalouf and Gammelgaard Citation2016). Other issues in relation to Lean in services, discuss experiences of work intensification as processes are standardised and job quality is reduced (Carter et al. Citation2013). Lack of best practice sharing, shortage of qualified staff and time constraints for improving operations are also highlighted as key issues (Adebanjo, Laosirihongthong, and Samaranayake Citation2016).
2.3. Lean sustainability
Sustainability of performance improvements gained through Lean requires organisations to recognise the importance of the human dimensions (Hines, Holweg, and Rich Citation2004). Soft skills continue to appear as prerequisites for sustainability of Lean (Hadid and Mansouri Citation2014) as well as taking a whole organisation view to improvement (Netland, Schloetzer, and Ferdows Citation2015; Piercy and Rich Citation2015). Considering Lean as resulting in organisational and cultural change (Mann Citation2009; Piercy and Rich Citation2015) would further support sustainability. However, beyond the examples of Virginia Mason @markgraban Citation2015) and Thedacare (Toussaint Citation2009), it is unknown if other healthcare providers have achieved Lean successes beyond early reports (Jabbal Citation2017), and improvement work conducted in traditional silos.
Structural tensions occur regularly in Lean which impact sustainability (Maalouf and Gammelgaard Citation2016) which include the power of medical professionals (Øvretveit Citation2005). Professionals impact Lean in their engagement and acceptance of the approach (Waring and Bishop Citation2010) with evidence that their lack of engagement determines the success and sustainability of Lean initiatives in an organisation (Lindsay, Kumar, and Juleff Citation2020; Leite, Bateman, et al. Citation2020).
Burgess and Radnor (Citation2013) reviewed Lean programmes in the NHS in England to see if they were sustained across non-consecutive years of reporting, and failures were evident. They also noted that a programme approach was common in NHS organisations, rather than a systemic approach to Lean. However, as per Barnas (Citation2011) discussion on Lean management systems, it is not always evident what the Lean management system is in healthcare organisations, and how it was designed and implemented (Costa and Godinho Filho Citation2016). The labelling of Lean improvement as a ‘programme’ of work is not uncommon in healthcare and has been evident elsewhere such as in Bolton (Doherty Citation2012), so considering programme design and its mechanisms as a PT, is relevant for Lean evaluation.
2.4. Programme theory
Programmes are constructed through developing a logical linking sequence of inputs, activities and outputs leading to intended or observed outcomes and impact (Rogers Citation2008). The articulation of the programme and the mechanisms to support this are regarded as a theory (Tilley Citation2004). We draw from Tilley (Citation2004, 256) in our assessment that programmes and the mechanisms supporting them are regarded as theories; ‘first, programmes comprise expectations that some problematic state or regularity can be altered for the better by introducing a set of measures. Second, they incorporate, as a rule, ideas about how that set of measures will bring about those changes. Programmes thus comprise theories both that change will occur and that it will be brought about by particular means.’
Programmes and their designers need to consider and address possible contextual moderators which can constrain as well facilitate planned changes (Legg et al. Citation2010). Moderators can occur within the internal operations of an organisation or can be located externally. Common contextual moderators within a healthcare scenario can include the political situation within the country, availability of specialist labour and resource-driven structure of care systems (Walley Citation2013). Understanding the nature of the contextual moderator and its role in the programme is essential in delivering the planned outcomes for programmes (Olsen, Legg, and Hasle Citation2012).
Lean interventions in healthcare are generally evaluated in terms of outputs not the process or mechanisms behind the programme to deliver change (Costa and Godinho Filho Citation2016). Additionally, there is a focus on the application of tools and techniques used, and a lack of reference to the mechanisms or underlying theory that make the programmes work (Costa and Godinho Filho Citation2016; Al Owad et al. Citation2018; Bortolotti et al. Citation2018). The mechanism that makes this logical sequence of events work, the programme, is known as the theory of change or PT (Reed et al. Citation2014). PT ‘provides the fundamental rationale and the underlying driver(s) that make a programme work’ (Olsen, Legg, and Hasle Citation2012, 6000) and are articulated as being ‘plausible and sensible models’ for how programmes are to work (Bickman Citation1987, Citation1996). PT design and articulation must be developed prior to the commencement of any work (Sharpe Citation2011). This then provides all involved, with clarity over processes, participants, intentions, tools applied in terms of data collection and measurement and the standards which will be used (Sharpe Citation2011; Davidoff et al. Citation2015). Goicolea et al. (Citation2015) explain that PT can be designed based on experience and then tested empirically in terms of what is being undertaken, why and how so to generate outcomes. The theory should be refined through subsequent rounds and learning from improvement and evaluation (Goicolea et al. Citation2015).
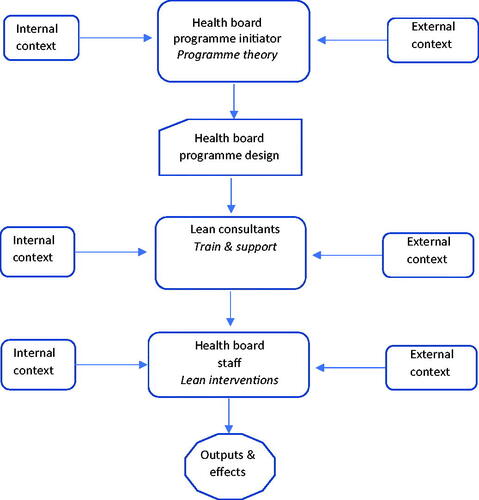
PT provides the framework to analyse the programme, interventions, outputs, and effects of the Lean healthcare programme. PT provides the scope to incorporate external and internal context issues and pressures that are evident in the sector. Contextualising the Lean initiative within the environs of healthcare, facilitates an understanding of constraints, resources and tensions that support or hinder change (Legg et al. Citation2010), and sustainability (Maalouf and Gammelgaard Citation2016). For the health board examined within this paper, the external contextual pressures from government to increase patient services led to the development of an improvement programme. The health board’s PT was that through upskilling its employees it would be able to build the capabilities with its organisation to sustainably improve patient services. With the assistance of external Lean consultants, the programme would develop knowledge of continuous improvement and provide Lean intervention support for colleagues. illustrates the simple logic model of the health board programme and its theory. Critically, the model performs in two ways to support the analysis in this paper. Firstly, it provides a PT to support the development and understanding of how the programme operates (Davidoff et al. Citation2015) and secondly this is used to guide its evaluation (Lipsey and Cordray Citation2000; Goicolea et al. Citation2015). How the programme operates, and its evaluation will be discussed in Section 4.
Figure 1. Health board programme model (adapted from Olsen, Legg, and Hasle Citation2012).
More research is required to evaluate the impact of Lean in healthcare and the starting point of this, is a full evaluation of Lean implementation to understand the process of implementation, the areas targeted and the successes and failures, which affect sustainability (Costa and Godinho Filho Citation2016). Assessing an organisational improvement approach allows us to evaluate the PT for Lean change. Within the operations domain, researchers need to understand if Lean in healthcare can move beyond short-term implementation, into longer-term sustainability (Radnor and Osborne Citation2013).
3. Research methodology
The focus of this research is a National Health Service (NHS) Board in Scotland providing public, government funded healthcare. For anonymity, it is referred to NHSB1. Healthcare in Scotland is provided by 14 territorial boards which deliver region specific healthcare services which includes acute hospital care, dentistry, primary care from general practitioners (GPs) and community care. Each NHS Board is directly accountable to Scottish Government Ministers (scot.nhs.uk, 2022). A single case study of one territorial board (NHSB1) forms the focus of this research in assessing PT. Our interest lies in assessing at an organisational level (NHSB1), the approach to Lean. Additionally, we also provide a further level of analysis in considering outcomes at a project level (Yin Citation2013), to support assessment of the PT and the consistency of its application. Meredith (Citation1998, 442) provides a definition of case study research as ‘a case study typically uses multiple methods and tools for data collection from a number of entities by a direct observer(s) in a single, natural setting that considers temporal and contextual aspects of the contemporary phenomenon under study, but without the experimental controls or manipulations.’ The research combines a retrospective and longitudinal case study approach as the data reported here is part of data that was gathered for a larger study. Reports on Lean interventions included retrospective analysis on earlier phases of work, i.e. from 2006 onwards.
NHSB1 can be considered an intrinsic case study (Stake Citation1995, 8) as it is considered as the first Scottish National Health Service (NHS) Board to embark on widespread Lean transformation which may provide unusual insights. The project was supported beyond NHSB1, as investment was received by the health board, from NHS Education for Scotland (NES), who were keen that learnings from this case could be shared across other health NHS boards in Scotland. NHSB1 was at the time also considered to be in the top five of NHS providers in the UK, in terms of healthcare provision across a region, hence being valid for a case study focus. Secondary data in the form of reports from NHSB1 Lean programme included 6 years of annual reports, which were subject to content analysis. These reports were published on the NHSB1 intranet, but were not freely available externally, hence preserving anonymity of the Health Board. The Lean interventions were referred to and labelled by the organisation in phases, aligned to their year of reporting, and this has been maintained in the content analysis provided in this paper. presents data on the reports used in the secondary data analysis.
Table 1. Secondary data reports.
The aim of content analysis is ‘to provide knowledge and understanding of the phenomenon under study’ (Downe-Wamboldt Citation1992, 314; cited in Hsieh and Shannon Citation2005). Krippendorff (Citation2004) is explicit that content analysis is a qualitative method in discussion of interpretation, context sensitivity and sense-making of the contents of the text. As context is a key aspect of PT (Legg et al. Citation2010), deductive elements were involved in the coding process, given the logic model already presented in . A deductive and inductive combined approach to content analysis is acceptable in healthcare research, especially where there is scope to contribute to theory and/or provide new insights to a recognised area of study (Elo and Kyngäs Citation2008). Three phases are involved in content analysis: Preparation, Organising and Reporting (Elo and Kyngäs Citation2008). In terms of preparation of data, this includes reading and note making, and using open coding of key words and phrases. Then reduction takes place, moving open coding into higher order themes before organising the data into categories (Elo and Kyngäs Citation2008). Throughout content analysis, data reduction is a key task and so we reduced data over three rounds to be able to finally report the categorisation. The coding of the data is shown in .
Table 2: Qualitative data coding (understanding programme design).
Content analysis can be hampered by missing or incomplete data (Krippendorff Citation2004). To mitigate against this, follow-up semi-structured interviews were conducted with 12 key stakeholders who had been involved in the Lean implementation projects under discussion. The same content analysis process was applied to interview data, and themes are also included as per those illustrated in .
Saunders and Townsend (Citation2016) validate this use of a smaller, targeted group of professionals when it is their expertise and/or experience, which is to be the focus of the discussion. All healthcare professionals interviewed as part of this research were specifically chosen for their involvement in Lean interventions that had been undertaken by NHSB1. Those involved included members of a ‘dedicated’ Lean team. Due to identifiable background information, interviewees are referred to by their role and experience only, as per .
Table 3. Interviewee’s by role and Lean experience.
Full institutional ethics approval was granted for this study. Additionally, approval was given from the Executive Team at NHSB1, with informed consent, given by all research participants.
4. Findings
In this section, we present the findings from the NHSB1 case study highlighting the PT contextual moderators, the programme design, and mechanisms that underpinned and supported the Lean initiative over a period of 6 years. The success factors, drivers, barriers, and resources associated with the programme and Lean initiatives will be explored through the identified projects. The evaluation of the programme will be based on the schematic model shown in .
4.1. Context to NHSB1 programme theory and initiation
Governmental pressures to drive down waiting times and increase the quality of patient services led the health board executive to initiate a continuous improvement programme. Through upskilling employees and furbishing them with the capabilities to drive change, it was anticipated that the organisation would develop a sustainable approach to enhancing patient services. This was supporting the executive team’s strategy of being in the top 25 of healthcare systems globally. Delivering this ambition required the programme to be impactful across all organisational levels, with healthcare staff of all grades and specialisms being involved, and broad in scope. This inclusive approach was determined from the outset as previous attempts to develop a continuous improvement ethos in healthcare institutions, including NHSB1, had failed. Discussions with NHSB1 had highlighted that ‘islands of excellence’, caused by functional and specialist silos, was not a sustainable approach as the gains made eventually dissipated. From the outset the executive team recognised that government demand for improvement would have to be incorporated into their programme for change through Lean. These external context drivers were expected to emphasise specific targets that the internal resources across the organisation would have to meet.
From the outset, a programme was designed to deliver, through inclusive activities across organisational boundaries, sustained improvements. This approach was expected to provide a more coherent understanding of the required process changes as well as the development of an improvement culture. The structured and inclusive nature of the initiative has been shown to promote improvements in other healthcare situations (Stentoft and Freytag Citation2020).
4.1.1. Programme design
Strategically the organisation decided to focus on key services/pathways which affected patient equity of access to service, and the equipment needed. Administrative as well as medical interventions were included in the project design therefore, utilising resources and knowledge from across the organisation. This approach reflected the need to improve the management of waiting-times lists across the region (as driven by government targets) and how referrals were triaged on reaching various regional hospitals from General Practitioners. The actual activities and pathways which were targeted for improvement were identified through three different routes each driven at a different level of the programme.
The Scottish Government set Health Improvement, Efficiency, Access, and Treatment (HEAT) targets each year which would require focus on specific specialities (NHSGGC 2019). These externally set targets were incorporated into the programme and translated into specific projects.
Some projects were defined as strategic priorities for the organisation and were not driven by government targets. These Lean initiatives included process and cultural change interventions as well as improvements in measurable outcomes.
Improvement projects could be selected and driven by staff through their own initiatives. These improvements were welcome by the health board as they indicated a cultural change through a ‘bottom-up’ approach with localised support and ownership.
Regardless of the type and source of the activity, each project leader would be required to provide feedback on performance changes to the health board. The improvement (or not) would be gauged through two forms of assessment namely, standardised quantitative metrics on issues such as reduction in waiting time lists (outputs focus to meet externally driven targets) and more qualitative outcomes such as morale. This balanced perspective on measures reflected the executive’s concerns with inclusivity and respect for people, while meeting the needs of external forces.
The improvement approach that would be used to deliver the health board strategy, provide leadership, and drive the programme was Lean Thinking. Due to limited internal knowledge and expertise, the executive decided that consultants would be engaged. Initially, after a full tendering process, NHSB1 engaged an external consultancy (Firm Z) to support Lean implementation, continuous improvement, and training. The use of external consultancy is not uncommon in healthcare organisations commencing Lean implementation (Fillingham Citation2007). The consultants were to work with NHSB1 staff from across the organisation, to support Lean interventions and embed skills transfer over a 2-year period. To commence the programme, 30 ‘key’ managers and senior partnership (trade union) representatives were to be receive Lean training from Firm Z. The following year a further 200 staff members would receive training and support linked to specific Lean interventions. This approach was deployed to grow the resources within the health board, improve processes as well as develop a continuous improvement culture. This provides evidence of best practice as recognised in the exemplar of Virginia Mason. Virginia Mason took external advice to develop their own Lean journey and embedded training to support their strategy. Critically, they have continued to sustain Lean for over 20 years and the success of this is attributed to employees being part of, and embracing, a continuous improvement culture (Virginia Mason Institute Citation2022). For NHSB1, encouraging employee contribution from staff across all areas and levels of the organisation was important to reduce potential barriers to change. Positively, this mirrors practices evident in the TPS (Monden Citation1983).
The health board expected that their strategic goal of being a top 25 health care provider would start to be realised through the programme that they had designed. The programme was expected to provide a framework that would incorporate externally generated contextual pressures and internally resourced change leaders from across the organisational spectrum. With the assistance of the Lean consultants and the engagement of colleagues, the capability to drive and deliver continuous improvement and service enhancement would be realised. Within 2 years the programme was expected to operate independently of the consultants as the internal capability to create and drive change would be institutionalised. The health board’s annual reporting on improvements and interviews with executives highlighted Lean as being the driver to deliver their strategy.
At that time [starting Lean] there were two things we needed. One was we needed an overall cultural organisational intervention that would essentially bind together the whole of NHSB1…we wanted stuff that front line staff would get. And then, I think the second thing is we could see without being unbelievably far-sighted, we could see that there was going to be a downturn in funding, we knew that the levels of growth were unsustainable…So two things: one, a cultural glue and secondly empowering front-line people to understand that they were able to fix things without necessarily recourse to money, given that money was going to become tighter (Executive 1).
Executive interviews explicitly mapped Lean to supporting the Human Resources (HR) people development strategy in NHSB1 so it would be ‘the way we do things.’ Resourcing change through developing a continuous improvement culture and up-skilling staff, were important internal contextual factors of the programme. This alignment to HR strategy received limited reporting in annual summaries but there is a mention by Year 4 that Lean is included in the corporate induction all new staff receive. Confirmation of Lean supporting the HR strategy was evident in interviews:
The Lean process was actually in support of the HR strategy and is also in the one just written and approved by the board which takes us up to about 10 years [from the start of Lean]. It was always the idea that it would be about how we do things around here because some of the stuff we do is process driven and this is about looking at processes and making them better and why would you not do that? (Executive 2).
From the start of designing the programme NHSB1 were focussed on establishing a PT that developed and recognised the potential of its internal resources yet, was sufficiently flexible to absorb the demands of external agents (Goicolea et al. Citation2015). In deploying the HR strategy, this was ‘the glue’ that would bind all staff together to drive improvements and was to underpin the programme.
Linking resource development to delivery of the NHSB1’s strategy was critical in providing the capacity to support governmental, executive team and staff derived improvement initiatives and targets. The holistic PT approach recognised the importance of the political, social, and technical aspects of developing a continuous improvements culture and approach, which can absorb and adjust to the dynamic environment of the healthcare sector (Haddad et al. Citation2016; Eriksson Citation2017).
4.1.2. Lean intervention approach
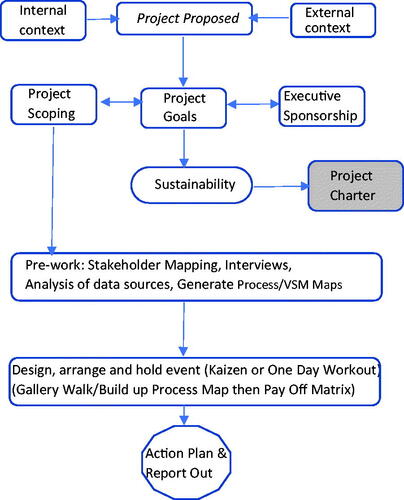
The data comes from annual Lean programme reports and provide summaries of projects undertaken by the Lean team. These reports provide an overview of the Lean intervention, drivers (including internal and external), implementation approaches, outcomes, and from year 2 onwards, sustainability of previous years’ work is reported. The process supporting the PT for Lean in NHSB1 is mapped out in . The figure illustrates the specific activities that take place in Lean projects, in terms of initiating projects, mechanisms involving staff groups, outcomes and sustainability considerations. Both annual reports and interviews correlate this PT and the consistency of application, over the years of activity being evaluated in this paper.
When a Lean intervention is identified, a Lean lead is aligned to the project. Participants include executive sponsors who are identified as the project is being scoped and goals articulated. Where Lean work moved beyond acute healthcare provision boundaries, executive sponsorship was also provided by an external (e.g. health and social care). A service lead (clinical or non-clinical manager) is also identified to be responsible for any work that will progress. Pre-work would be undertaken at the service level to identify stakeholders (healthcare staff of all grades/relevant disciplines) who are interviewed to understand the current state.
I suppose it’s like listening to staff and picking up the key themes and the recurrent themes and you get the sort of critical to quality indicators which are flagged up during the interviews (Lean lead 6).
The aim is that stakeholders represent multi-disciplinary teams and all those involved in the patient journey in the service under focus. Staff are also able to contribute their ideas here, as well as thoughts on other relevant stakeholders who should be involved. This means that staff driven ideas that are implemented, will be more acceptable and lead to an effective result. The Lean lead creates an initial process map and gathers any other relevant data sources. This results in the design of a Lean event in the form of a Kaizen held over five days or a ‘one day workout’ for small, targeted initiatives. Developing multi-disciplinary teams and creating a plan based on stakeholder input, demonstrates a programme design that is based on inclusiveness. Embracing the issues and challenges faced by the resources of NHSB1, reflected the drive by the board to change the culture and involve everyone on the continuous improvement journey. This approach provides direct line between the board and the team, emphasising the importance of the initiative to the direct participants and wider community (van Dun, Hicks, and Wilderom Citation2017).
The format of the reports changes over time showing learning from improvement, as does amendment of the Lean PT. The shaded box in highlights where a project charter was introduced to keep services focussed on improvement and sustainability required to meet the health boards’ ambitions. The new reporting tool aided the board and the Lean sponsors to track progress on the outputs and effects of the projects. This project charter was piloted in year 3 and formally introduced in year 4 for all projects. In year 4, the approach to training was also evaluated and adapted with e-resources being provided and a review of sessions. Support for previous trainees is provided in the form of network meetings, and evaluation of these saw positive responses and no change to the format offered because of feedback. Network meetings provided a basis for the exchange of best practice, sharing of experiences (positives and negatives) and underpinned the sustainability of previous gains.
These steps of providing executive sponsorship across organisational boundaries, appointing project leadership, and gaining stakeholder insights before any initiatives are undertaken, demonstrates a structured deployment approach. Developing an understanding of the resources and the issues faced in NHSB1, provided a platform from which to develop project plans and focus. These actions address the limitations previously highlighted by Costa and Godinho Filho (Citation2016).
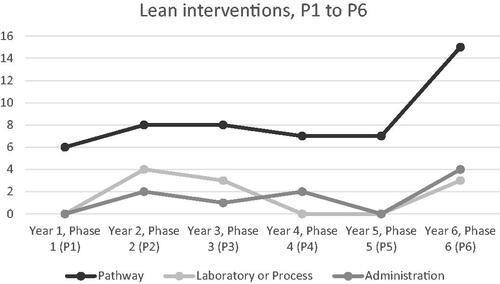
4.2. Evaluation of the programme
Six years of annual reports were analysed which led to the classification, as shown in , of the types of Lean interventions undertaken by NHSB1. As referred to in section ‘Research methodology’, NHSB1 labelled these reports as a phase of work so Year one was Phase 1 (P1) and so on, as shown in . These include pathway, laboratory or process and administration projects across a range of services. This aligns to previous project evaluations conducted by Brandão de Souza (Citation2009), although our case considers these from a single organisational study of Lean activity. The reporting labels the Lean interventions as ‘projects’ and so this wording has been maintained in the analysis of the reports. Staff in interviews also referred to being involved in Lean projects.
70 projects are written up in NHSB1 reporting by Year 6, highlighting the diffusion of the Lean programme across multiple processes and functions. Pathways received a focus in 51 out of the 70 projects conducted. Improving specific processes (pathways) provided a boundary to the initiative and focus for the resources involved, permitted clear definition of results and outcomes related to the improvements implemented. Laboratory or reviewing of a specific process, for example in pathology, hospital sterilising and scanning services such as Computerised Tomography (CT) and Magnetic Resonance Imaging (MRI), were evident in 10 projects and administration (paperwork and IT projects), received a focus on its own with work around Ethics, Estates and Gynaecology administration of patient notes. Cancer pathways received an on-going focus throughout the years of work assessed (Breast, Pathology and Colorectal) in Years 1–4 and then in Year 6. Colorectal work in Year 3 included specific projects on administration within the service. Dermatology work first commenced in Year 3 due to rising demand for Dermatology services outstripping capacity and resources, but this work also extended into cancer pathways. Cross-service projects delivered with Plastic Surgery saw work being conducted in Year 3, Year 4, and Year 6. This demonstrates sustainability and development of initiatives over several years. Sustainability has been recognised as a major challenge within Lean in healthcare (Leite, Lindsay, et al. Citation2020).
Year 1 saw the first project that would stretch beyond typical acute service boundaries. Work on delayed discharge, bed availability and social care packages was undertaken in conjunction with regional health and social care. This initiative was driven by pressure from external bodies to improve waiting times. This required cross-boundary sponsors and cross-functional teams. The result of the external pressure and unified, cross-boundary resources response was significant. Year 2 saw further work undertaken beyond acute boundaries and projects winning international quality awards. This is an important illustration, given that previous work has criticised Lean for failing to move beyond organisational boundaries when considering healthcare provision (Radnor and Osborne Citation2013).
Administration work was undertaken with the Health Board Research and Development Administration and this work was to later link into ethics procedures in Year 6. Child Protection cases in conjunction with Social Work received a focus in Year 2 and the first stage of work in Substance Misuse pathways began in Year 2, continued in Year 4 and was to spread across the region by Year 6. Year 2 saw the Hospital Sterilisation and Decontamination Unit (HSDU) win an award for improvement.
The expansion, duration and success of the projects and programme reflected the strategy of the NHSB1 board and its HR. Encompassing not just staff but also HR practitioners in Lean, is something that has received little previous consideration in Lean research, even though HR with their roles in people selection, training and reward are recognised as supporting Lean maturity (Zirar, Trusson, and Choudhary Citation2020). A 10-year horizon was established at the beginning of the programme to create the ‘glue’ that would change the culture of the organisation. The framework that was established at the outset was designed to accommodate externally generated changes, supported by HR practices. The drive to reduce waiting times was addressed through a cross-functional medical and social care team that utilised resources from separate domains to deliver success.
4.2.1. Programme projects and targets
Realising the health board’s strategic objectives, through upskilling and developing the improvement capabilities of staff, required the programme to accommodate three sources of projects and targets. These sources reflected the external and internal context that the programme would have to operate within.
4.2.1.1 External context
The political influence on healthcare is evident as 36 out of 70 reported projects are specifically linked to external targets which are set. shows the Lean project by their year and how many of the projects conducted are related to targets. The focus on targets varied across the reporting period where targets drove most of the work in Years one and two and were 50% of the Lean projects in Years three and four. By Year 6, 36% of projects were related to targets, although clarity of reporting of projects declines in this period. Referral to Treatment Times guarantee’s (RTTs) are set to determine waiting times for treatment by the Scottish Government but vary depending on the speciality. In substance misuse, targets were originally set at 8 weeks and then by Year 4, the RTT was three weeks. Substance abuse projects featured twice in Year 6 reporting. These projects involved acute healthcare, council, community and third sector as Lean was applied in other areas across the region after the successes in previous years.
Table 4. Lean projects related to targets.
Analysis yielded a depth of detail for the drivers for projects beyond a focus on targets. Dermatology had struggled to meet RTTs which were at 18 weeks, shortly to reduce to 12 weeks across four pathways. To meet RTTs, the service was scheduling additional evening and weekend clinics as 7.3% of all NHSB1 outpatients were for Dermatology. Other social and political factors beyond targets impacted challenges in balancing demand with capacity, as a 20% increase in referrals to Dermatology services was evident in Scotland. By Year 6, in a bid to sustain earlier work related to targets and successful outcomes, a further Lean project was targeted at Primary Care and the management of Dermatology referrals from General Practitioners.
Cancer pathways received a large focus in NHSB1, and informed pathway work over successive phases, primarily due to Scottish Government set targets. Cancer data collection linked into strategic work undertaken on cancer projects as this data collection supports identification of waiting times and provides research data on patients and their journeys. Duplication was evident as patients enter pathways at different points in their treatment journeys. Further to this, there were challenges in sharing data across services due to different systems in use.
4.2.1.2 Internal context
Some projects were defined as strategic priorities for the health board, so were not driven by external government targets. Work on Wheelchairs and Seating Pathways received a focus in Year 3. Three services had been merged into one, but variation and missing information impacting patient flow had been identified. This resulted in the service being unable to consistently provide all patients with assistance equipment without delays. Addressing issues flagged by pathway stakeholders, as well as managing multiple examples of external initiatives, supported the progress of the Lean initiative, by including the views of the staff involved on a day-to-day basis. The PT accommodated changing priorities, and this has been shown to be important in the success of Lean initiatives (Goicolea et al. Citation2015).
As well as government targets and strategic health board priorities, individual departments and services could drive their own Lean projects. These were undertaken by service staff who had participated in NHSB1 Lean training. These were specifically labelled as such and reported in Years 5 and 6. A trainee project was focussed on Hospital at Night (HAN) handover in Year 5 which was linked to the organisations’ strategic focus of safety. Night-time and weekend care has been flagged for safety concerns elsewhere (Han et al. Citation2017). In NHSB1, the HAN handover is the largest handover in the three major acute sites but variation in protocols, training and communication had been identified thus highlighting the large potential for error. Further trainee projects were reported on in Year 6 reporting where seven ‘trainee’ projects were illustrated in the annual reports. These projects included work in Medical Physics who were struggling with poor turnaround times for equipment repairs, urgent repairs that were not supported by a clear process, and a poor working environment. The different organisational levels participating in Lean initiatives concurrently, reflects a structure with flexibility, and is scaffolded to manage and control multiple inputs. This reflects the development and management of a PT approach to generate outcomes that deliver tangible value (Goicolea et al. Citation2015), as shown in which details the impact of contextual changes on the programme. The readiness of the organisation to respond in such a manner, was supported through the change commitment and efficacy of the organisation’s members and its evolving improvement culture (Narayanamurthy et al. Citation2018).
Table 5. Contextually derived projects.
4.2.2. Intervention approach
Although it was not always transparent in the reporting why some projects were supported by Kaizen events or 1 day workouts, interviewees highlighted time as having an impact. As aligned to reporting, there was a recognition that at least initially, 5-day kaizen events were more predominant but latterly, it was more challenging to take staff out of a service for that length of time, so one-day workouts were used to mitigate against time restrictions:
We can have anything from a one-day work out to a five-day Kaizen. We used to do more of the longer Kaizen’s than we do now. The service is under a lot of pressure, and they feel it difficult to realise people for that length of time (Lean lead 2).
One operational manager who had experience of Lean events in and across services explained that at least initially, her experience had been through involvement in Kaizen events. She has fully engaged in Lean, undertaken training and had been involved in running her own project. Time and space for improvement was prioritised then. During the interview she reflected on the differences between that and what she had experienced more recently, resulting in a critique of the approach, and attributing it as being typical of the organisation.
It (the Kaizen) was watered down, much like ‘oh no we need to get these people off the shop floor, I know, we’ll compress it all into kind of five hours’ which is quite a NHSB1 thing to do, so do all the ‘this is what we’d like, this is what the pressures are, lets kind of muddle through with some kind of thing which is a watered down version because we are so time pressured’. So yes, it was kind of a five-hour session and then something like a 3-hour afternoon meeting after that and then the follow ups (Operational Manager 2).
Resource constraints were apparent on occasions as the programme progressed. The pressures on time became more evident, reducing the level of support provided to staff in the development of knowledge and planning of projects. These important findings, during the progression of the programme, highlight the sensitivity of resources and time to the on-going success and sustainability of Lean implementations within healthcare (Adebanjo, Laosirihongthong, and Samaranayake Citation2016; Stentoft and Freytag Citation2020).
4.2.3. Programme outcomes
From Year 1 to Year 6, outcomes from projects have been reported, demonstrating alignment with programme intentions to improve service and support the development of a continuous improvement capability. In reporting of the projects, some typical metrics are provided such as reduction in length of stay, improvement of safety and outcomes from treatment or working with GPs and shared services to better meet referral to treatment times. Balancing capacity with demand was improved through changes to ward routines, especially in the areas of Occupational Therapy and Physiotherapy as reported in multiple projects such as Medicine of the Elderly (MoE) reduction of length of stay. These changes to routines were also evident in projects in Year 3 and Year 5. Balancing capacity with demand was explicitly discussed in reporting for Stroke, Geriatric Orthopaedic Rehabilitation Unit (GORU) and Inpatient Flow in Year 5 and for cohesive structuring for multi-agency service provision in Substance Misuse (Year 2, Year 4, and Year 6). This was extended into changes in staff roles to better meet service pressures and included work on staff and medical consultant’s work plans (Substance Misuse in Year 6; Dermatology projects (multiple); and consultant work plans in annual leave planning (Year 5).
In reporting outcomes, the focus in the annual reports has been firmly on the benefits achieved in the patient services. There is discussion on ‘cost avoidances and savings’ but this is not as prominent as the reporting of other outcomes. Cost savings and avoidances are rarely featured in the reporting of individual projects in earlier phases, the exception being Year 4 which broke down cost savings and avoidances for 4 projects out of the 12 conducted. As an average, cost savings and avoidances are listed as being £1–£1.4 million per year of reporting. However, by Year 4 reporting, savings are estimated at over £6 million but costs and the need for savings are articulated in a section on challenges and explicitly linking Lean with efficiency savings; ‘the current financial climate means that NHSB1 must use Lean to make efficiency savings. The focus of Lean in NHSB1 will always be to improve services for patients, but the financial impact of projects is also important and is identified as well’ (Year 4).
Although data analysis and Lean interventions could generate demonstrable outcomes such as reductions in waiting times for meeting HEAT targets; softer, qualitative outcomes such as improved communication, morale and relationships were also reported. The first discussion of relationships impacting on services is Year 2. Strained relationships as a result in a breakdown between administration and clinical staff, were evident in reporting of a project in Outpatients. Outcomes in this project are noted as ‘staff satisfaction’ and ‘improved working relationships’ (Year 2). Morale and communication affecting relationships is again discussed within projects as three out of 12 projects had related to this in the Year 3 reporting. Lean interventions supported the management of these issues and are listed as an outcome such as improved working and communication in multi-agency projects (Social work referral, assessment and allocation processes project and the Scottish Ambulance Service/turnaround times project) as well as work within acute services (Colorectal information flow within Outpatients).
NHSB1 reporting in Year 4 makes clear that although metrics produce validation of successful outcomes from projects, the Lean methodology has softer, qualitative benefits that are harder to measure.
‘Benefits we can’t measure: As well as enhancements to the patient experience through reduced waiting times and improved environments, the organisation benefits from increased capacity and achievement of targets. The benefits to the staff are not often measured and can be difficult to quantify.
• Rapid improvement events allow staff from different departments involved in the same process to come together. Pressures at different points in the process are seen and understood by the whole group and hierarchy disappears for those few days.
• When staff are given protected time and empowered to make changes in their place of work, their morale improves’
The importance of developing internal collaborative and productive Lean resources is a recurring theme in the analysis of the Lean initiatives. On occasions, projects are deployed specifically to support this collaboration. Cross-functional and boundary spanning activities are also evident, reflecting the strategy of executive board to develop a sustainable Lean approach to enhancing patient services across all organisational levels and functions. These findings add weight to growing demands for an enhanced focus on social aspects within implementations, given the outcomes that can result (Bortolotti, Boscari, and Danese Citation2015; Costa and Godinho Filho Citation2016; Bortolotti et al. Citation2018; Lindsay, Kumar, and Juleff Citation2020).
The executive team’s planned outcomes from the PT approach were two-fold in nature. Firstly, it was intended to deliver ‘hard’ quantifiable benefits in terms of financial savings, service quality improvements and RTT’s. Secondly, improvements in ‘soft’ socially important indicators such as staff morale and skills development were actively encouraged. This combination of ‘hard’ and ‘soft’ deliverables is shown in . Embedding the continuous improvement culture through attaining tangible cross-departmental boundary performance improvements while recognising intangible ‘respect for people’ benefits was viewed as pivotal to the success of the programme. From the outset the PT was designed to demonstrate leadership, commitment, and openness, through enhanced communication, to support staff in developing their own improvement initiatives. This positive and encouraging approach reflects the findings of other researchers in terms of the deployment attributes of successful healthcare Lean implementations (Matthias and Brown Citation2016).
Table 6. PT deliverables.
4.2.4. Sustainability
In Lean annual reports, there has been positive reporting and Dermatology saw a focus over multiple phases. This work is reported as successful and sustained, with involvement in follow-on projects. Work was undertaken on pathways, linkages to plastic surgery and cancer targets, equity of patient access to services across the region and GP support for potential referrals, which were successful and sustained. Staff in the service verified that this was an accurate reflection of what had happened, as well as the service also being involved in other services’ projects due to patient pathway linkages.
99% of outcomes were achieved [in Dermatology Lean projects]. There were huge numbers of staff involved like - everywhere that Dermatology has links with: Pathology, Plastic Surgeons, and I’ve just realised that we also did another Lean for Plastic Surgery and because Dermatology and Plastic Surgery work quite closely together, we went along to that. It wasn’t actually ours, but we were invited for our side for how we refer onto them and things like that (Administrator 1).
Certain groups of staff were recognised for their contributions to Lean work, for being accountable and ensuring results. Occupational Therapists and Physiotherapists were involved in multiple projects, especially in relation to Medicine for the Elderly pathways, and were described as ‘real movers and shakers’.
Having the right people in the room is important as if they engage in the project then accountability, success and sustainability is viewed to follow. Substance Misuse was a multi-agency initiative. Although there were initially tensions between healthcare and social work staff, bringing everyone together through Kaizen, was a turning point.
Some of the people that I worked with (who have been really hard to work with) have then done full turnabout and once they are part of an event and especially in Substance Misuse, social workers were phenomenal, they were fantastic. They were really driven to take things forward (Lean lead 1).
There is also recognition from staff, that not all outcomes are viewed as measurable, in respect of meeting waiting times targets, ensuring equity of access to services, or reducing complaints. Softer, qualitative outcomes were recognised from Lean in NHSB1 from interviewees such as better departmental working, equity of decision making and input to process improvement.
We seemed to come together more closely as a department instead of just admin, nurses, and doctors. We were all involved in the process together so not one main decision – everything was discussed in the open at the meeting and everybody’s views got portrayed across as being useful in changes and things (Administrator 1).
As part of the articulated ‘Lean in NHSB1’ PT, projects are revisited/audited on an annual basis by the Lean leads. Reporting of sustainability of projects was covered from Year 2, through to Year 5. However, analysis of reports shows that there is a ‘drop off’ in what is described under sustainability from Year 4 onwards with the reporting forgoing mention of sustainability. The term ‘sustainability’ is last used in Year 4 with ‘insights’ appearing in Year 5. Where sustainability is discussed, these reports are positive with discussions of how outcomes have not only been sustained but also how staff have progressed further Lean initiatives (Dermatology in Year 3 and Year 4). However, by Year 6 there are no summaries provided of where projects have been revisited or even ‘insights’. In the Year 6 report, there is a summary of work which looks forward into Year 7 as ‘future plans’. Some of these projects include areas already visited such as pharmacy prescribing which had projects undertaken in Year 2 and Year 3. This time the prescribing pathways within Prison Healthcare will be reviewed which includes those at two prisons within the Health Board region. Complaints were to be revisited in Year 7, following on from work conducted in Year 4. HSDU, was an award-winning project in Year 2 but was to be revisited in Year 7 for process improvement. There is no further discussion as to why projects which had initially been the focus in previous phases are being highlighted as part of the Year 7 work plan. Previously where drivers built on previous work, this was articulated so it was clear that there was not just sustainability of earlier work but further progression of it in services.
Issues over sustainability may be because of work that has not been progressed, despite positive reports from Kaizen/workout events held previously. A series of strategic pathway projects had been undertaken for Medicine of the Elderly (MoE) and within day hospitals for rapid assessment appointments which general practitioners could refer into. This was designed to avoid admissions with extended lengths of stay. The PT of change very much endorsed acceptance and accountability from staff which would lead to an effective result. Although there were initial successes which had been sustained, when this was attempted to be replicated across the region to other day hospitals it failed. Staff perceived the improvement to be driven top down, without the same investment which had been evident elsewhere. This resulted in staff sabotaging attempts at improvement, so the project was later abandoned.
First of all, we were imposing something from the top down on all the other day hospitals. A couple of them bought into it, we managed to get them along as far as we possibly could along the lines of putting it in but there was resource issues which couldn’t be resolved without any funding and at one particular day hospital, the day was just a disaster because no-body was bought into it, and most of the staff were just there to sabotage it (Lean lead 3).
There are some areas of the reporting (Years 5 and 6) that start to highlight issues over ‘acceptance’ or engagement with Lean as a mechanism for improvement which may jeopardise the sustainability and quality of the solution/outcomes. This also came up in staff discussions and the medical staff group (consultants) were highlighted as not accepting change through Lean:
Consultants… a lot of them don’t work as teams. They might be a team, they might be a group of people who all do the same thing but they might not see themselves as a team so they might not be happy for doctor A&B to represent them and to then come back and say ‘right we’ve done this event and this is what was decided’ and it doesn’t matter of this was a good or bad idea, it’s just that they won’t be told what to do by A&B. It’s this whole first amongst equal’s things, you know? (Lean lead 5).
Another Lean lead spoke on the same theme and how part of the pre-work with services was to also understand where the troublemakers in the service could be:
I think a couple of them are anti-everything so I think I’m learning to find out a bit more about individual personalities and what the stumbling blocks could be. I had some very honest discussions with the service management about who the potential troublemakers were or could be, and it’s kind of been proved right but I think they are anti-anything new or anything, they think Lean is a waste of money or a waste of spending money on us (Lean lead 4).
It is clear when evaluating annual reports that sustainability was initially reported in terms of continuing projects and the positive outcomes that were achieved. Latterly, reporting using the label ‘sustainability’ declined and was eventually stopped. It is not apparent why this is the case however, successful projects continued to be evident in the published outputs and the executive team demonstrated on-going commitment to the programme, as Lean became part of organisational culture. Sustainability for NHSB1 reflected sustained learning and improvements for the organisation which was shown through the reports and interviews with staff members. Success for the programme and its sustainability was measured in terms of fiscal, service and staff morale improvements. This rounded approach to sustaining Lean based improvements in NHSB1 was aligning with ‘respect for people’ and coupled to the external pressures for service quality and cost enhancements.
highlights the success factors and barriers to sustainability associated with the PT approach of NHSB1. Early focus on organisational readiness for change, involvement of external consultants to facilitate quick Lean knowledge transfer, development of Lean champions, and executive sponsorship of projects contributed to a significant and organisationally important start to the sustainable journey. Challenges to sustain and initiate change within and across departments became evident as resources became constrained.
Table 7. Sustainability success factors and barriers within a PT approach.
As we have articulated the PT for Lean in NHSB1 and used this to evaluate the progress of Lean in the organisation whilst paying attention to sustainability, now we will present the discussion.
5. Discussion
The lack of longitudinal studies has limited the contribution of previous studies into Lean interventions and their sustainability (Mazzocato et al. Citation2014; Stentoft and Freytag Citation2020). The existing knowledge developed from ‘snap shots’ of current practice reduces their usefulness for practitioners in understanding the impact and sustainability of Lean over the longer-term (Jabbal Citation2017; Roemeling, Land, and Ahaus Citation2017). Usually, Lean projects are reviewed over a period of 1 − 2 years (Fillingham Citation2007), and this temporally truncated view of interventions means many existing studies are unable to evaluate sustainability. Through assessing 6 years of reported interventions, with reports correlated by interviews, this research begins to address these limitations through providing assessment on the successes and failures of using Lean as an on-going continuous improvement mechanism. This retrospective and longitudinal study has identified how successful projects, such as Dermatology, were not only sustained, but were further developed into subsequent initiatives across multiple years and multiple pathways including into Plastic Surgery and linked into work with primary care. Substance Misuse spread across the region, moved beyond acute care boundaries, and demonstrated that Lean can be applied and sustained in interventions which involve multiple, external stakeholders. The key to successful projects has been the multi-disciplinary staff involved, and their acceptance of the PT for delivering and sustaining outcomes. In having longitudinal data, it is clear Lean leads, supported by executive sponsors, engaged with staff from the outset as part of the programme design. This included a programme design that supported qualitative data gathering, rather than a reliance on hard metric data only. The assessment of qualitative benefits in terms of working relationships, improved communication, and empowering staff groups identified that engagement across the full process, leads to outcomes being derived and sustained across multiple initiatives.
Through the lens of PT, the programme design was identified providing a framework to assess the challenges and contributors to sustaining Lean based efforts. Through this longitudinal study, the programme design was shown to accommodate the contextual pressures and inputs (external and internal) in which it operated. Programme theories, and their designs, are expected to adapt to contextual moderators which were not considered at the outset (Goicolea et al. Citation2015). This ability to adapt to external contextual moderators was important within the design of the programme, as it was anticipated that political and social demands would change the focus on areas to improve. For NHSB1 the ability to flex was also demonstrated internally, through the development of project charters to ensure accountability for sustainability of Lean change. Through embedding flexibility into the programme design, the executive team could select initiatives to meet current external needs without compromising their overall objective.
Recognition of contextual influences on programme theories is important given their potential impact on any outcomes (Albaek Citation1989; Dahler-Larsen Citation2001). Contextual moderators have a direct impact on programme design and delivery (Olsen, Legg, and Hasle Citation2012) and for the case study organisation, they continued to remain at the heart of the programme and delivery of improvements. In assessing context, we show how these external contextual moderators are built into the PT and design. The target driven nature of healthcare, which is frequently reported in literature (Ham Citation2004; Klein Citation2010; Radnor, Holweg, and Waring Citation2012; Walley Citation2013), was evident in the case study. In NHSB1 this came from Scottish Government set targets such as HEAT and RTTs, which influenced interventions for more than half of all projects conducted. It is often documented that Lean is implemented as a response to budgetary constraints and thus studies focussing on context, often refer to the external context as the impetus for Lean (Waring and Bishop Citation2010; Radnor, Holweg, and Waring Citation2012; Gadolin Citation2019), rather than wider considerations of contextual moderators being encompassed within a programme design. There has been limited strategic linkage to Lean in previous studies (Burgess and Radnor Citation2013; Matthias and Brown Citation2016) but we evidence the clear alignment of Lean with NHSB1s organisational strategy. We go on to identify that there is a further internal contextual moderator, and these projects are ‘service priorities’ from service staff who nominate their services for Lean intervention. This results in three sources of contextual moderators, which influence the choice of Lean interventions as external and internal priorities change over time. The PT lives within, responds to contextual moderators, and will ultimately determine what the programme outcomes and effects are, while moving forward to achieve NHSB1s overall objective.
As observed in NHSB1, PT articulates the process design as evident in the programme design in where we see a clear focus on respect for people to understand the current state of services, any subjective influences as well as the process of intervention and generating outcomes. This comes through stakeholder mapping and interviews in pre-work stages as well as employee derived improvement and accountability in Kaizen events. Executive interviews also confirmed that Lean was aligned to organisational and the HR strategy over a 10-year period. Lean was not just to be implemented to drive change in the organisation but to empower front line staff to make those changes.
The programme design offers a further contribution as this can act as a guide for other Lean healthcare implementations. For NHSB1, this design provided a strong and sustainable platform for change through Lean. This consistency of approach is evident in the reporting and is contrary to general assessments of Lean in the NHS, about a lack of fidelity to one approach (Jabbal Citation2017). The study of NHSB1 involves 6 years of projects and reports where sustainability is evident, providing an example of Lean sustainability which has been illusive (Burgess and Radnor Citation2013; Mazzocato et al. Citation2014). As well as context, another key input into the PT is the role of people. Part of the PT of change in NHSB1, makes clear that accountability and acceptance will generate effective results. We provide evidence of ‘bottom-up’ acceptance of Lean (Ohno Citation1988; van Dun, Hicks, and Wilderom Citation2017) and this generation of team derived improvement supports engagement in Lean (Drotz and Poksinska Citation2014). Empowerment and improved morale are recognised as less quantifiable outcomes from strategic projects undertaken, and here we contribute to recognising the impact Lean has on the working environment (Adebanjo, Laosirihongthong, and Samaranayake Citation2016).
Where project analysis highlights failures in Lean interventions, these clearly link to social determinants in implementing and sustaining Lean. This emerged in the example of HSDU which was an award-winning strategic project in Year 2 and was regarded by the Lean lead as being successful due to a clear process and clear process owner. However, when there was a change in process owner, the project was ‘picked apart’ so was in scope to be revisited in Year 7. Middle managers resistance to Lean is important, given their typical role as change agents when initiatives are determined to be strategic and therefore are passed top-down (Pedersen and Huniche Citation2011).
Strategic, top-down driven change has not ensured Lean success across sites and has resulted in instances of failure in NHSB1 due to a lack of staff empowerment and engagement (Mann Citation2009). Further social aspects relating to power and hierarchy within healthcare, can also impact sustainability, regardless of the profile of any external or internal strategic intervention (Leite et al. Citation2022). The impact of professionalism is apparent in annual reports. A lack of engagement from orthopaedic surgeons is reported, highlighting non-attendance at events which then will impact outcomes and sustainability of Lean in the service. Professionalism continues to attract an academic focus as a social determinant influencing Lean (Drotz and Poksinska Citation2014; Lindsay, Kumar, and Juleff Citation2020; Leite, Bateman, et al. Citation2020). There is scope within developing PTs for Lean implementation, to further encompass this as another internal contextual moderator, given healthcare structures and professional demarcations.
5.1. Practical implications
Our findings here demonstrate the value of applying PT to a service environment, but we also extend these to consider Lean more widely across other industrial contexts. Although PT has been widely applied in healthcare (Reed et al. Citation2014; Goicolea et al. Citation2015), it has had limited application within service operations management when assessing from a Lean perspective. Although our focus here is healthcare, PT is applicable to other domains and may counter some of the reported challenges as assessed in organisations implementing Lean. A tools-based approach dominates assessment of Lean within the literature base in industrial contexts (Panwar et al. Citation2015; Piercy and Rich Citation2015; Costa and Godinho Filho Citation2016). Lean failures and poor outcomes are often attributed to a lack of strategic alignment (Piercy and Rich Citation2015), absence of a systematic and adaptive approach (Narayanamurthy et al. Citation2018) and a tool, rather than soft focus (Matsui Citation2007). For manufacturing organisations, recognising the need to plan and develop Lean interventions aligned to strategy and developing programmes that can sustain improvement while accommodating context change, is an important finding. Key learning points from our case study include PT encompassing strategic alignment, boundary spanning work involving cross-disciplinary teams, and enabling a respect for people focus. All of which have previously been identified as important elements supporting Lean success when assessing Lean progress in different sectors (Matsui Citation2007; Bortolotti, Boscari, and Danese Citation2015; Piercy and Rich Citation2015; Costa and Godinho Filho Citation2016).
However, Lean in NHSB1 was not without its challenges. Although the PT was evident throughout the years of activity we assess here, interviewees referred to resourcing constraints in terms of time and space to work on Lean activity. These resource challenges have been recognised as having an impact on Lean implementation and outcomes (Adebanjo, Laosirihongthong, and Samaranayake Citation2016).
Critically, as we are still amid a global Covid-19 pandemic and experiencing waves of infections, PT is developed to be responsive to external and internal changes. The flexibility which is inherent in the design is worthy of note and needs to be taken into consideration when looking to implement Lean in a service environment more generally, beyond healthcare. Lean is viewed as evolving (Hines, Holweg, and Rich Citation2004; Pawar et al. 2015) so PT that adapts to both internal and external contextual moderators will contribute to fidelity to one approach and sustainability. Lean has already been assessed as supporting services being able to adapt to Covid derived changes and achieving enhanced performance results (Tortorella et al. Citation2021). This was also attributed to culture and behaviours (ibid). We demonstrate the criticality of human resources and cross functional groups in deriving outcomes from Lean. The clear alignment of senior management sponsorship and support, mapped to strategy to support culture change and underpinned by appropriate resources, could go some way in supporting non-healthcare organisations in aligning Lean to strategy if they designed their own PT for Lean implementation. PT supports a multi-layered approach to encouraging, recognising, supporting, and including people from across the hierarchy and breadth of the institution. This was important in sustaining and growing interventions. The programme was designed to involve the entire organisation and respect the people it employs. This approach was critical in overcoming the ‘islands of excellence’ issue frequently reported (Hines, Holweg, and Rich Citation2004).
6. Conclusions
Through the application of a PT lens, the longitudinal study revealed how a sustained approach to Lean implementation can be achieved. Fidelity to one approach to improvement is evident through the programme design. This important finding addresses the concern that healthcare organisations often engage improvement activities in a piecemeal fashion before abandoning for the latest initiative (Proudlove, Moxham, and Boaden Citation2008; Jabbal Citation2017). Our research has also demonstrated the importance of considering and incorporating contextual moderators into the PT and design, when utilising Lean as an improvement mechanism. Recognition of internal resources, their development, support, and limitations were an important aspect of sustaining the Lean interventions. Balancing the needs of fiscal, political, and social pressures while, having ‘respect for people’ was a major theme of the programme. PT enabled us to illustrate and make a further contribution through our analysis of reporting and interview data, in assessing the impact of social determinants on sustainability, which influenced successes and failures in NHSB1 Lean interventions.
6.1. Limitations and implications for future research
This study is based on a single organisational case study, based in a publicly funded, regional, National Health Service acute care provider in the UK. We acknowledge the limitations of secondary data and missing ‘unexplained’ elements, though the supporting interview data has gone some way to address these inadequacies, resulting in rich data evaluating Lean in NHSB1. However, the existing context and data used may affect generalisability of our findings across developed and developing country contexts with varying healthcare funding structures.
We echo calls from Costa and Godinho Filho (Citation2016) for future studies to be focussed on the implementation process and focussing on articulating and evaluating a PT of change, allows for this. Different country contexts and funding structures would allow for the comparison of PTs to illustrate how contextual moderators are built into the programme and if they differ from those we have identified. Aligned to this, longitudinal studies of Lean over the longer term (10–15 years) may provide successful examples of navigating the social determinants affecting programmes and provide much needed examples of sustained Lean implementations.
As strategy is a contextual moderator within our PT, we also call for research which can further assess how Lean supports strategy. NHSB1 was able to align Lean in support of organisational strategy and this was embedded in the HR strategy over a 10-year period. Matthias and Brown (Citation2016) have already recognised a ‘vague’ link between Lean and strategy in the NHS in England, but there is scope for further assessment to determine if HR strategies support Lean interventions. HR is recognised as having critical role in influencing employee attitudes and behaviours, which in turn affects organisational performance. However, this has been noted as being complex in the healthcare sector due to long standing issues over ‘crude’ performance indicators (Bruce and Hill Citation1994; Klein Citation2010).
The current global Covid-19 pandemic offers the opportunity for further PT based research. There has been evidence of Lean practices supporting Covid-19 responses in healthcare (Leite, Lindsay, et al. Citation2020), as well as in services (Tortorella et al. Citation2021), but how/if Lean programmes survive and are sustained during periods of crisis, offers additional avenues for research.
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
Additional information
Notes on contributors

Claire F. Lindsay
Dr Claire F. Lindsay is an Associate Professor in Supply Chain at Edinburgh Business School, Heriot-Watt University. Her work has an empirical focus on how policy translates into practice, and her research areas include operational improvement, sustainability, legislation and wider procurement and supply chain activities. She has conducted research with the NHS and Scottish Courts and Tribunal Services. Prior to entering academia, Claire held a variety of operational and supply chain roles whilst working for a major UK food manufacturer.

James Aitken
James Aitken is a Professor of Operations Management at the University of Surrey. Professor Aitken has over 25 years of industrial and commercial experience in the electronics, construction, consultancy and logistics sectors. During his time in manufacturing he established one of the first examples of an agile enterprise in Europe. He studied for his PhD on a part-time basis at Cranfield University and completed his doctorate ‘Supply Chain Integration within the Context of a Supplier Association’ in 1998. Since his graduation he has continued to publish papers on supply chain management and operations. He worked full-time in industry until 2009 when he joined the University of Surrey as an FME fellow.
References
- Adebanjo, Dotun, Tritos Laosirihongthong, and Premaratne Samaranayake. 2016. “Prioritizing Lean Supply Chain Management Initiatives in Healthcare Service Operations: A Fuzzy AHP Approach.” Production Planning & Control 27 (12): 953–966. doi:10.1080/09537287.2016.1164909.
- Aitken, James, Ann E. Esain, and Sharon Williams. 2021. “Management of Complexity in the Care Ecosystem.” Supply Chain Management: An International Journal 26 (4): 481–494. doi:10.1108/SCM-05-2020-0207.
- Al Owad, Ali, Premaratne Samaranayake, Azharul Karim, and Kazi Badrul Ahsan. 2018. “An Integrated Lean Methodology for Improving Patient Flow in an Emergency Department–Case Study of a Saudi Arabian Hospital.” Production Planning & Control 29 (13): 1058–1081. doi:10.1080/09537287.2018.1511870.
- Albaek, Erik. 1989. “Policy Evaluation: Design and Utilization.” Knowledge in Society 2 (4): 6–19. doi:10.1007/BF02687230.
- Ballé, Michael, and Anne Régnier. 2007. “Lean as a Learning System in a Hospital Ward.” Leadership in Health Services (Bradford, England) 20 (1): 33–41. doi:10.1108/17511870710721471.
- Barnas, Kim. 2011. “Thedacare’s Business Performance System: Sustaining Continuous Daily Improvement Through Hospital Management in a Lean Environment.” The Joint Commission Journal on Quality and Patient Safety 37 (9): 387–AP8. doi:10.1016/S1553-7250(11)37049-3.
- Bhat, Shreeranga, and N. A. Jnanesh. 2014. “Application of Lean Six Sigma Methodology to Reduce the Cycle Time of out-Patient Department Service in a Rural Hospital.” International Journal of Healthcare Technology and Management 14 (3): 222. doi:10.1504/IJHTM.2014.064257.
- Bicheno, John. 2008. The Lean Toolbox for Service Systems, Buckingham: Picsie Books
- Bickman, Leonard. 1987. “The Functions of Program Theory.” New Directions for Program Evaluation 1987 (33): 5–18. doi:10.1002/ev.1443.
- Bickman, Leonard. 1996. “The Application of Program Theory to the Evaluation of a Managed Mental Health Care System.” Evaluation and Program Planning 19 (2): 111–119. doi:10.1016/0149-7189(96)00002-X.
- Bortolotti, Thomas, Stefania Boscari, and Pamela Danese. 2015. “Successful Lean Implementation: Organizational Culture and Soft Lean Practices.” International Journal of Production Economics 160 (February): 182–201. doi:10.1016/j.ijpe.2014.10.013.
- Bortolotti, Thomas, Stefania Boscari, Pamela Danese, Hebert Alonso Medina Suni, Nicholas Rich, and Pietro Romano. 2018. “The Social Benefits of Kaizen Initiatives in Healthcare: An Empirical Study.” International Journal of Operations & Production Management 38 (2): 554–578. doi:10.1108/IJOPM-02-2017-0085.
- Bowerman, Jennifer, and David Fillingham. 2007. “Can Lean save Lives?” Leadership in Health Services (Bradford, England) 20 (4): 231–241. 10.1108/17511870710829346.
- Brandão de Souza, Luciano. 2009. “Trends and Approaches in Lean Healthcare.” Leadership in Health Services 22 (2): 121–139. doi:10.1108/17511870910953788.
- Bruce, Alan, and Sandra Hill. 1994. “Relationships Between Doctors and Managers: The Scottish Experience.” Journal of Management in Medicine 8 (5): 49–57. 10.1108/02689239410073358.
- Burgess, Nicola, and Zoe Radnor. 2013. “Evaluating Lean in Healthcare.” International Journal of Health Care Quality Assurance 26 (3): 220–235. 10.1108/09526861311311418.
- Carter, Bob., Andy Danford, Debra Howcroft, Helen Richardson, Andrew Smith, and Phil Taylor. 2013. “Stressed out of My Box’: Employee Experience of Lean Working and Occupational Ill-Health in Clerical Work in the UK Public Sector.” Work, Employment and Society 27 (5): 747–767. doi:10.1177/0950017012469064.
- Costa, Luana Bonome Message, and Moacir Godinho Filho. 2016. “Lean Healthcare: Review, Classification and Analysis of Literature.” Production Planning & Control 27 (10): 823–836. doi:10.1080/09537287.2016.1143131.
- Dahler-Larsen, Peter. 2001. “From Programme Theory to Constructivism.” Evaluation 7 (3): 331–349. doi:10.1177/13563890122209711.
- D'Andreamatteo, Antonio, Luca Ianni, Federico Lega, and Massimo Sargiacomo. 2015. “Lean in Healthcare: A Comprehensive Review.” Health Policy 119 (9): 1197–1209. doi:10.1016/j.healthpol.2015.02.002
- Davidoff, Frank, Mary Dixon-Woods, Laura Leviton, and Susan Michie. 2015. “Demystifying Theory and Its Use in Improvement.” BMJ Quality & Safety 24 (3): 228–238. 10.1136/bmjqs-2014-003627.
- Doherty, Lesley. 2012. “Striving for Excellence Succeeding with Lean Thinking in Healthcare.” Accessed 29 July 2020. http://www.boltonft.nhs.uk/wp-content/uploads/2012/12/bics_lesley_doherty_succeeding_with_lean_thinking_healthcare12.pdf
- Donaldson, Stewart. I. 2005. “Using Program Theory-Driven Evaluation Science to Crack the Da Vinci Code.” New Directions for Evaluation 2005 (106): 65–84. doi:10.1002/ev.152
- Downe-Wamboldt, Barbara. 1992. “Content Analysis: Method, Applications, and Issues.” Health Care for Women International 13 (3): 313–321. doi:10.1080/07399339209516006.
- Drotz, Erik, and Bozena Poksinska. 2014. “Lean in Healthcare from Employees’ Perspectives.” Journal of Health Organization and Management 28 (2): 177–195. doi:10.1108/JHOM-03-2013-0066.
- Dun, Desirée H. van, Jeff N. Hicks, and Celeste P. M. Wilderom. 2017. “Values and Behaviors of Effective Lean Managers: Mixed-Methods Exploratory Research.” European Management Journal 35 (2): 174–186. doi:10.1016/j.emj.2016.05.001.
- Elo, Satu, and Helvi Kyngäs. 2008. “The Qualitative Content Analysis Process.” Journal of Advanced Nursing 62 (1): 107–115. doi:10.1111/j.1365-2648.2007.04569.x.
- Eriksson, Nomie. 2017. “Hospital Management from a High Reliability Organizational Change Perspective: A Swedish Case on Lean and Six Sigma.” International Journal of Public Sector Management 30 (1): 67–84. doi:10.1108/IJPSM-12-2015-0221.
- Fillingham, David. 2007. “Can Lean Save Lives?” Accessed 29 July 2020. doi:10.1108/17511870710829346.
- Gadolin, Christian. 2019. “The Influence of Policy Makers Over Lean Implementations in Healthcare.” International Journal of Health Governance 24 (3): 222–229. doi:10.1108/IJHG-02-2019-0016.
- Goicolea, Isabel, Anna Karin Hurtig, Miguel San Sebastian, Carmen Vives-Cases, and Bruno Marchal. 2015. “Developing a Programme Theory to Explain How Primary Health Care Teams Learn to Respond to Intimate Partner Violence: A Realist Case-Study.” BMC Health Services Research 15 (1): 228. doi:10.1186/s12913-015-0899-8.
- Graban, Mark. 2013. Lean Hospitals. 2nd ed. New York: Productivity Press.
- Guo, Lin, and Selena Hariharan. 2012. “Patients Are Not Cars and Staff Are Not Robots: Impact of Differences between Manufacturing and Clinical Operations on Process Improvement.” Knowledge and Process Management 19 (2): 53–68. doi:10.1002/kpm.1386.
- Haddad, Marc G., Pierrette P. Zouein, Joseph Salem, and Rami Otayek. 2016. “Case Study of Lean in Hospital Admissions to Inspire Culture Change.” EMJ - Engineering Management Journal 28 (4): 209–223. doi:10.1080/10429247.2016.1234896.
- Hadid, Wael, and S. Afshin Mansouri. 2014. “The Lean-Performance Relationship in Services: A Theoretical Model.” International Journal of Operations & Production Management 34 (6): 750–785. doi:10.1108/IJOPM-02-2013-0080.
- Hallam, Cory R. A, and Carolina Contreras. 2018. “Lean Healthcare: Scale, Scope and Sustainability.” International Journal of Health Care Quality Assurance 31 (7): 684–696. doi:10.1108/IJHCQA-02-2017-0023
- Ham, Christopher. 2004. Improving Health Policy in Britain. 5th ed. Basingstoke: Palgrave McMillan.
- Han, Lu., Matt Sutton, Stuart Clough, Richard Warner, and Tim Doran. 2018. “Impact of out-of-Hours Admission on Patient Mortality: longitudinal Analysis in a Tertiary Acute Hospital.” BMJ Quality and Safety 27 (6): 445–454. doi:10.1136/bmjqs-2017-006784
- Hines, Peter, Matthias Holweg, and Nick Rich. 2004. “Learning to Evolve: A Review of Contemporary Lean Thinking.” International Journal of Operations and Production Management 24 (10): 994–1011. doi:10.1108/01443570410558049.
- Hsieh, Hsiu Fang, and Sarah E. Shannon. 2005. “Three Approaches to Qualitative Content Analysis.” Qualitative Health Research 15 (9): 1277–1288. doi:10.1177/1049732305276687.
- Jabbal, Joni. 2017. “Embedding a Culture of Quality Improvement.” The Kings Fund. Accessed 20 July 2020. https://www.kingsfund.org.uk/publications/embedding-culture-quality-improvement
- Jones, Daniel, and Alan Mitchell. 2006. Lean Thinking for the NHS: A Report Commissioned by the NHS Confederation. London: NHS Confederation.
- Klein, Rudolf. 2010. The New Politics of the NHS. 6th ed. Oxford: Radcliffe Publishing Ltd.
- Krippendorff, Klaus. 2004. “Content Analysis.” Accessed 29 July 2020. http://repository.upenn.edu/asc_papers.
- Lander, Eduardo, and Jeffrey K. Liker. 2007. “The Toyota Production System and Art: Making Highly Customized and Creative Products the Toyota Way.” International Journal of Production Research 45 (16): 3681–3698. doi:10.1080/00207540701223519.
- Legg, Stephen, Kirsten Olsen, Felicity Lamm, Ian Laird, Leigh-Ann Harris, and Peter Hasle. 2010. “Understanding the Programme Theories Underlying National Strategies to Improve the Working Environment in Small Businesses.” Policy and Practice in Health and Safety 8 (2): 5–35. doi:10.1080/14774003.2010.11667746.
- Leite, Higor, Claire Lindsay, and Maneesh Kumar. 2020. “COVID-19 Outbreak: Implications on Healthcare Operations.” The TQM Journal 33 (1): 247–256. doi:10.1108/TQM-05-2020-0111.
- Leite, Higor, Nicola Bateman, and Zoe Radnor. 2020. “Beyond the Ostensible: An Exploration of Barriers to Lean Implementation and Sustainability in Healthcare.” Production Planning & Control 31 (1): 1–18. doi:10.1080/09537287.2019.1623426.
- Leite, Higor, Sharon Williams, Zoe Radnor, and Nicola Bateman. 2022. “Emergent Barriers to the Lean Healthcare Journey: Baronies, Tribalism and Scepticism.” Production Planning & Control: 1–18. doi:10.1080/09537287.2022.2054386.
- Lindsay, Claire F., Maneesh Kumar, and Linda Juleff. 2020. “Operationalising Lean in Healthcare: The Impact of Professionalism.” Production Planning & Control 31 (8): 629–643. doi:10.1080/09537287.2019.1668577.
- Lipsey, Mark. W, and David. S. Cordray. 2000. “Evaluation Methods for Social Intervention.” Annual Review of Psychology 51 (1): 345–375. doi:10.1146/annurev.psych.51.1.345
- Maalouf, Malek, and Britta Gammelgaard. 2016. “Managing Paradoxical Tensions During the Implementation of Lean Capabilities for Improvement.” International Journal of Operations & Production Management 36 (6): 687–709. doi:10.1108/IJOPM-10-2014-0471.
- Mann, David. 2009. “The Missing Link: Lean Leadership.” Frontiers of Health Services Management 26 (1): 15–26.
- Mannon, Melissa. 2014. “Lean Healthcare and Quality Management: The Experience of ThedaCare.” Quality Management Journal. American Society for Quality 21 (1): 7–10. doi:10.1080/10686967.2014.11918371.
- @markgraban 2015. “Lean in Healthcare.” Twitter.
- Matsui, Yoshiki. 2007. “An Empirical Analysis of Just-in-Time Production in Japanese Manufacturing Companies.” International Journal of Production Economics 108 (1–2): 153–164. doi:10.1016/j.ijpe.2006.12.035.
- Matthias, Olga, and Steve Brown. 2016. “Implementing Operations Strategy through Lean Processes within Health Care: The Example of NHS in the UK.” International Journal of Operations & Production Management 36 (11): 1435–1457. doi:10.1108/IJOPM-04-2015-0194.
- Mazzocato, Pamela, Johan Thor, Ulrika Bäckman, Mats Brommels, Jan Carlsson, Fredrik Jonsson, Magnus Hagmar, and Carl Savage. 2014. “Complexity Complicates Lean: Lessons From Seven Emergency Services.” Journal of Health Organization and Management 28 (2): 266–288. doi:10.1108/JHOM-03-2013-0060.
- McCann, Leo., John. S. Hassard, Edward Granter, and Paula. J. Hyde. 2015. “Casting the Lean Spell: The Promotion, Dilution and Erosion of Lean Management in the NHS.” Human Relations 68 (10): 1557–1577. doi:10.1177/0018726714561697.
- Meredith, Jack. 1998. “Building Operations Management Theory Through Case and Field Research.” Journal of Operations Management 16 (4): 441–454. doi:10.1016/S0272-6963(98)00023-0.
- Monden, Yasuhiro. 1983. Toyota Production System. Georgia: Industrial Engineering and Management Press.
- Narayanamurthy, G., A. Gurumurthy, N. Subramanian, and R. Moser. 2018. “Assessing the Readiness to Implement Lean in Healthcare Institutions–a Case Study.” International Journal of Production Economics 197: 123–142. doi:10.1016/j.ijpe.2017.12.028.
- Netland, Torbjørn. H., Jason. D. Schloetzer, and Kasra Ferdows. 2015. “Implementing Corporate Lean Programs: The Effect of Management Control Practices.” Journal of Operations Management 36 (1): 90–102. doi:10.1016/j.jom.2015.03.005.
- Noori, Behroz. 2015. “Identifying Critical Issues in Lean Implementation in Hospitals.” Hospital Topics 93 (2): 44–52. doi:10.1080/00185868.2015.1052299
- Ohno, Taiichi. 1988. Toyota Production System - Beyond Large Scale Production. New York: Productivity Press.
- Olsen, Kirsten, Stephen Legg, and Peter Hasle. 2012. “How to Use Programme Theory to Evaluate the Effectiveness of Schemes Designed to Improve the Work Environment in Small Businesses.” Work 41: 5999–6006. doi:10.3233/WOR-2012-0036-5999.
- Øvretveit, John. 2005. “Leading Improvement.” Journal of Health Organization and Management 19 (6): 413–430. doi:10.1108/14777260510629661.
- Panwar, Avinash, Bimal P. Nepal, Rakesh Jain, and Ajay Pal Singh Rathore. 2015. “On the Adoption of Lean Manufacturing Principles in Process Industries.” Production Planning & Control 26 (7): 564–587. doi:10.1080/09537287.2014.936532.
- Pedersen, Esben Rahbek Gjerdrum, and Mahad Huniche. 2011. “Determinants of Lean Success and Failure in the Danish Public Sector: A Negotiated Order Perspective.” International Journal of Public Sector Management 24 (5): 403–420. doi:10.1108/09513551111147141.
- Piercy, Niall, and Nick Rich. 2015. “The Relationship Between Lean Operations and Sustainable Operations.” International Journal of Operations & Production Management 35 (2): 282–315. doi:10.1108/IJOPM-03-2014-0143.
- Proudlove, Nathan, Claire Moxham, and Ruth Boaden. 2008. “Lessons for Lean in Healthcare from Using Six Sigma in the NHS.” Public Money and Management 28 (1): 27–34. doi:10.1111/j.1467-9302.2008.00615.x.
- Radnor, Zoe J., Matthias Holweg, and Justin Waring. 2012. “Lean in Healthcare: The Unfilled Promise?” Social Science & Medicine (1982) 74 (3): 364–371. doi:10.1016/j.socscimed.2011.02.011.
- Radnor, Zoe, and Stephen P. Osborne. 2013. “Lean: A Failed Theory for Public Services?” Public Management Review 15 (2): 265–287. doi:10.1080/14719037.2012.748820.
- Reed, Julie E., Christopher McNicholas, Thomas Woodcock, Laurel Issen, and Derek Bell. 2014. “Designing Quality Improvement Initiatives: The Action Effect Method, a Structured Approach to Identifying and Articulating Programme Theory.” BMJ Quality & Safety 23 (12): 1040–1048. doi:10.1136/bmjqs-2014-003103.
- Remtulla, Ridhaa, Arwa Hagana, Nour Houbby, Kajal Ruparell, Nivaran Aojula, Anannya Menon, Santhosh G. Thavarajasingam, and Edgar Meyer. 2021. “Exploring the Barriers and Facilitators of Psychological Safety in Primary Care Teams: A Qualitative Study.” BMC Health Services Research 21 (1): 269–212. doi:10.1186/s12913-021-06232-7.
- Roemeling, Oskar, Martin Land, and Kees Ahaus. 2017. “Does Lean Cure Variability in Health Care?” International Journal of Operations & Production Management 37 (9): 1229–1245. doi:10.1108/IJOPM-07-2015-0452.
- Rogers, Patricia J. 2008. “Using Programme Theory to Evaluate Complicated and Complex Aspects of Interventions.” Evaluation 14 (1): 29–48. doi:10.1177/1356389007084674.
- Samuel, Donna, Pauline Found, and Sharon J. Williams. 2015. “How Did the Publication of the Book the Machine That Changed the World Change Management Thinking? Exploring 25 Years of Lean Literature.” International Journal of Operations and Production Management 13 (10): 1386–1407. doi:10.1108/IJOPM-12-2013-0555.
- Saunders, Mark N. K., and Keith Townsend. 2016. “Reporting and Justifying the Number of Interview Participants in Organization and Workplace Research.” British Journal of Management 27 (4): 836–852. doi:10.1111/1467-8551.12182.
- Schmenner, Roger W. 2015. “The Pursuit of Productivity.” Production and Operations Management 24 (2): 341–350. doi:10.1111/poms.12230.
- Sharpe, Glynn. 2011. “A Review of Program Theory and Theory-Based Evaluations.” American International Journal of Contemporary Research 1 (3): 72–75.
- Sinha, K. K., and E. J. Kohnke. 2009. “Health Care Supply Chain Design: Toward Linking the Development and Delivery of Care Globally.” Decision Sciences 40 (2): 197–212. doi:10.1111/j.1540-5915.2009.00229.x.
- Stake, Robert. 1995. The Art of Qualitative Research. Edited by N. Denzin and Y. Lincoln. California: Sage.
- Stentoft, Jan, and Per Vagn Freytag. 2020. “Improvement Culture in the Public Mental Healthcare Sector: Evaluation of Implementation Efforts.” Production Planning & Control 31 (7): 540–556. doi:10.1080/09537287.2019.1657978.
- Tilley, Nick. 2004. “Applying Theory-Driven Evaluation to the British Crime Reduction Programme.” Criminal Justice 4 (3): 255–276. doi:10.1177/1466802504048465.
- Tortorella, Guilherme, Gopalakrishnan Narayanamurthy, Moacir Godinho Filho, Alberto Portioli Staudacher, and Alejandro F. Mac Cawley. 2021. “Pandemic’s Effect on the Relationship Between Lean Implementation and Service Performance.” Journal of Service Theory and Practice 31 (2): 203–224. doi:10.1108/JSTP-07-2020-0182.
- Toussaint, John S., and Leonard L. Berry. 2013. “The Promise of Lean in Health Care.” Mayo Clinic Proceedings 88 (1): 74–82. doi:10.1016/j.mayocp.2012.07.025.
- Toussaint, John. 2009. “Writing the New Playbook for U.S. Health Care: Lessons from Wisconsin.” Health Affairs (Project Hope) 28 (5): 1343–1350. 10.1377/hlthaff.28.5.1343.
- Tracey, Monica W., and Jamie W. Flinchbaugh. 2006. “How Human Resource Departments Can Help Lean Transformation.” Accessed 30 July 2020. https://www.lean.org.za/wp-content/uploads/2015/03/How_HR_Helps_Lean1.pdf
- Virginia Mason Institute. 2022. “Lean.” Accessed 13 June 2022. https://www.virginiamasoninstitute.org/?s=Lean
- Walley, Paul. 2013. “Does the Public Sector Need a More Demand-Driven Approach to Capacity Management?” Production Planning & Control 24 (10–11): 877–890. doi:10.1080/09537287.2012.666886.
- Waring, Justin J., and Simon Bishop. 2010. “Lean Healthcare: Rhetoric, Ritual and Resistance.” Social Science & Medicine (1982) 71 (7): 1332–1340. doi:10.1016/j.socscimed.2010.06.028.
- Yin, Robert. K. 2013. Case Study Research: Design and Methods. 5th ed. Thousand Oaks: Sage.
- Zirar, Araz, Clive Trusson, and Alok Choudhary. 2020. “Towards a High-Performance HR Bundle Process for Lean Service Operations.” International Journal of Quality & Reliability Management 38 (1): 25–45. doi:10.1108/IJQRM-10-2019-0330.