ABSTRACT
Prompt uptake of antiretroviral treatment (ART) is essential to ensure the success of universal test and treat (UTT) strategies to prevent HIV transmission in high-prevalence settings. We describe ART initiation rates and associated factors within an ongoing UTT cluster-randomized trial in rural South Africa. HIV-positive individuals were offered immediate ART in the intervention arm vs. national guidelines recommended initiation (CD4≤350 cells/mm3) in the control arm. We used data collected up to July 2015 among the ART-eligible individuals linked to TasP clinics before January 2015. ART initiation rates at one (M1), three (M3) and six months (M6) from baseline visit were described by cluster and CD4 count strata (cells/mm3) and other eligibility criteria: ≤100; 100–200; 200–350; CD4>350 with WHO stage 3/4 or pregnancy; CD4>350 without WHO stage 3/4 or pregnancy. A Cox model accounting for covariate effect changes over time was used to assess factors associated with ART initiation. The 514 participants had a median [interquartile range] follow-up duration of 1.08 [0.69; 2.07] months until ART initiation or last visit. ART initiation rates at M1 varied substantially (36.9% in the group CD4>350 without WHO stage 3/4 or pregnancy, and 55.2–71.8% in the three groups with CD4≤350) but less at M6 (from 85.3% in the first group to 96.1–98.3% in the three other groups). Factors associated with lower ART initiation at M1 were a higher CD4 count and attending clinics with both high patient load and higher cluster HIV prevalence. After M1, having a regular partner was the only factor associated with higher likelihood of ART initiation. These findings suggest good ART uptake within a UTT setting, even among individuals with high CD4 count. However, inadequate staffing and healthcare professional practices could result in prioritizing ART initiation in patients with the lowest CD4 counts.
Introduction
There is substantial evidence that antiretroviral treatment (ART) provides strong health benefits at both individual and population levels. ART improves morbidity and mortality, including in HIV-positive individuals with asymptomatic infection and high CD4 counts (INSIGHT START Study Group et al., Citation2015; TEMPRANO ANRS 12136 Study Group et al., Citation2015). ART at higher CD4 counts has also been shown to reduce HIV transmission to uninfected sexual partners by maintaining viral load at undetectable level (Cohen et al., Citation2011; Donnell et al., Citation2010). Furthermore, a recent study demonstrated that increased ART coverage at lower CD4 counts was associated with a significant decrease in HIV incidence at the population level (Tanser, Bärnighausen, Grapsa, Zaidi, & Newell, Citation2013). This inverse relationship between ART coverage and HIV incidence together with the clear clinical benefits of extended ART use are the principles underlying the adoption of the universal test and treat (UTT) strategy to prevent HIV transmission in high-prevalence settings.
However, challenges in the HIV-care cascade are well documented (Iwuji et al., Citation2015) with low HIV test uptake as well as poor linkage to care and delay in initiating ART amongst eligible individuals in care often cited as barriers to achieving these benefits (Fox et al., Citation2014; Kranzer, Govindasamy, Ford, Johnston, & Lawn, Citation2012; McNairy et al., Citation2015; Musheke et al., Citation2013).
In recent years, the CD4 criterion for ART initiation evolved towards earlier initiation in WHO's recommendations and subsequent national recommendations: ≤350 cells/mm3 in 2010, ≤500 cells/mm3 in 2013, regardless of CD4 count in 2015 (WHO, Citation2010, Citation2013, Citation2015), based on evidence from clinical trials (TEMPRANO ANRS 12136 Study Group et al., Citation2015). However, there is little evidence from “real life” settings on the acceptability and uptake of early ART in mostly asymptomatic individuals in care who have a CD4 > 350 count cells/mm3.
The UTT TasP trial which is ongoing in rural South Africa provides the opportunity to study this issue. We aimed to describe the uptake of ART according to CD4 count strata and associated factors among HIV-positive individuals who linked to care after home-based HIV testing.
Methods
Study setting and design
The ANRS 12249 TasP trial is a cluster-randomized trial implemented in the Hlabisa sub-district, located in northern KwaZulu-Natal in South-Africa, which is a largely rural area with scattered homesteads and an estimated HIV prevalence of 29% (Zaidi, Grapsa, Tanser, Newell, & Bärnighausen, Citation2013). The protocol of the TasP trial is described in detail elsewhere (Iwuji et al., Citation2013; Orne-Gliemann et al., Citation2015). In summary, the trial was implemented in 22 geographic clusters over time: 4 clusters opened in March 2012, 6 clusters opened in January 2013 and 12 additional clusters opened in July 2014. Each cluster is composed of an average population of about 1000 residents ≥16 years old. The main hypothesis of the TasP trial is that HIV testing of all adult members of a community, followed by immediate ART initiation of all, or nearly all, HIV-infected participants regardless of immunological or clinical staging, will prevent onward transmission and reduce HIV incidence in this population. Only individuals aged 16 years or older and resident in the trial clusters are eligible for trial participation.
The UTT strategy being tested in the TasP trial has two main components. In both trial arms, rounds of home-based counselling and HIV testing are repeated every six months. All trial participants identified as HIV-infected are then referred to a TasP trial clinic located at less than 5 km from their homes. Each TasP trial clinic is staffed by one nurse and one counsellor irrespective of population size. Busier clinics are occasionally supported by additional staff depending on availability. In the control clusters, HIV-infected adults are offered ART according to South African guidelines which from study inception to December 2014 was having one of the following criteria: CD4 count ≤350 cells/mm3, WHO stage 3 or 4 or pregnancy (National Department of Health, Republic of South Africa, Citation2013). These criteria were expanded in January 2015 to include those with CD4 ≤ 500 cells/mm3, hepatitis B surface antigen positivity and HIV-positive partner in a serodiscordant relationship regardless of CD4 count (National Department of Health, Republic of South Africa, Citation2015). In the intervention clusters, ART initiation is offered regardless of CD4 count or clinical staging. HIV-care is also available in the public sector ART programme where HIV-positive individuals can receive ART according to the South African guidelines.
The trial was approved by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal (BFC 104/11) and the Medicines Control Council of South Africa.
Study population
This study used data collected up to 15 July 2015 in the first 10 clusters including both arms of the trial (5 × 2). The study population included HIV-positive individuals who linked to care before 1 January 2015 (prior to change in ART guidelines in South Africa), and were not on ART at the baseline clinic visit but eligible for ART initiation according to the trial protocol.
Variables
The event of interest is ART initiation defined as the first time antiretroviral therapy was dispensed to the participant in a TasP clinic.
Explanatory variables used in the analysis included data obtained through face-to-face questionnaires during home-based visits as well as information collected at the baseline clinic visit (Iwuji et al., Citation2013; Orne-Gliemann et al., Citation2015). Information obtained during home visits () were: sex, age, education, occupational status, household wealth, food insecurity, acceptability of “immediate” ART, perception of stigma towards people living with HIV and straight line distance between homesteads and clinic. Information obtained at the baseline clinic visit included: having a regular partner, HIV-status disclosure, social support, psychological distress [Patient Health Questionnaire-4 score (Kroenke, Spitzer, Williams, & Löwe, Citation2009; Löwe et al., Citation2010)], time between referral and baseline clinic visit, being newly diagnosed at referral, being ART-naïve and CD4 count at baseline combined with other eligibility criteria (WHO stage 3 or 4 and pregnancy for women). Clusters have been grouped to construct a three-category variable: (i) clusters A–D, opened in 2012, stratified as having lower HIV prevalence (21.7–24.5%), relatively high staff–patient ratios (2.1–3.1 per 100 patients) and fixed clinics; (ii) clusters E and F, opened in 2013, having comparable HIV prevalence (21.1–22.5%), high staff–patient ratios (2.7–5.7 per 100 patients) and mobile clinics opened during week days only; (iii) clusters G–J, opened in 2013, having higher HIV prevalence (32.5–39.8%), low staff–patient ratios (0.6–1.3 per 100 patients) and mobile clinics opened weekdays and Saturdays.
Table 1. Factors associated with ART initiation in patients eligible to ART (according to trial protocol) not treated at baseline clinic visit, univariate and multivariate analyses (ANRS 12249 TasP trial, rural South Africa, N = 514).
Statistical analysis
Follow-up period was defined as the period between baseline clinic visit and ART initiation, with right-censoring at last follow-up clinic visit of each patient. The follow-up time for patients having only the baseline visit was defined as one day (Howards, Hertz-Picciotto, & Poole, Citation2007).
The association between the explanatory variables and ART initiation was assessed using an extension of the Cox proportional hazard (PH) model which includes an interaction with a step function that takes into account that covariate effects may change over time. Two different effects were tested: a “main effect” corresponding to the hazard ratio (HR) over the first month of follow-up, and a change in the main effect after 30 days (“effect change after one month”). The 30-day threshold was assessed by plotting the Kaplan–Meier survival curves (i.e., the cumulative probability of not being ART treated) according to the different categories of the covariates. The introduction of an interaction with time through a step function was also justified by the results of the test of PH assumption, based on the rescaled Schoenfeld residuals (Grambsch & Therneau, Citation1994) performed in the standard Cox model which showed that the PH assumption was violated for some covariates.
Potential explanatory variables having a p-value <0.25 for the main effect or for an effect change, for at least one category (Wald test) in the univariate analyses, were considered eligible for inclusion in the multivariate analysis. A backward stepwise procedure was then used to select variables in the final multivariate model with a p-value ≤0.05 (Wald test). A main effect after one month of follow-up was also computed for the multivariate model, corresponding to the product of the main effect and the effect change after one month. A global Chi-square test was performed to test the Cox specification using the interaction with time vs. the standard Cox specification in the final multivariate model.
Stata/SE 12.1 for Windows software (StataCorp, Citation2011) was used for all analyses.
Results
Study population
The study population included 514 individuals (). Baseline characteristics are presented in : 70.4% were women, 35.6% less than 30 years old. Most of them had a poor socio-economic status: only 22.6% completed secondary or higher education, 77.2% reported being inactive (not employed and not student) and 61.7% declared food insecurity (not having enough food for adult household members). Most reported having a regular partner (77.2%), while 15.0% had not disclosed their HIV status to anyone and nearly a quarter reported no social support (21.6%). Most of the patients (73.0%) entered into care within three months of referral. A small minority (8.8%) had less than 100 CD4/mm3 at baseline and 45.3% more than 350 CD4/mm3.
Descriptive analysis of ART initiation
The 514 study patients had a median [interquartile range (IQR)] duration of follow-up of 1.08 [0.69; 2.07] months until ART initiation or last visit, representing 1206.4 person-months. Among them, 451 (87.7%) initiated ART during the follow-up period. presents the rates (cumulative probabilities) of ART initiation by cluster and overall, at one month (M1), three months (M3) and six months (M6) from the baseline visit. The overall rate of ART initiation at M1 was 49.5%, increasing to 82.2% and 88.7% at M3 and M6, respectively. We also observed a large variability across clusters, especially at M1, with rates varying between 38.4% and 83.3%.
Table 2. Cumulative probability of ART initiation, time to ART initiation and clinics staff–patient ratios by cluster (ANRS 12249 TasP trial, rural South Africa).
and show, respectively, the cumulative probability of ART initiation, estimated using Kaplan–Meier curves, and the corresponding estimated rates at M1, M3 and M6 (both overall and according to CD4 count and other eligibility criteria). Rates of ART initiation at M6 were quite similar and ranged from 85.3% to 96.1% (except for the specific subgroup with CD4 ≥ 350 cells/mm3 and WHO stage 3/4 or pregnancy who had a rate of ART initiation of 60.5% at M6) (). However, rates of ART initiation at M1 varied substantially according to CD4 and other eligibility criteria; ranging from 55.2% to 71.8% in those with CD4 ≤ 350 cells/mm3 compared to 30.7% in the category WHO stage 3/4 or pregnancy and 36.9% in the category without WHO stage 3/4 or pregnancy, in those with CD4 > 350 cells/mm3.
Figure 2. (a) Overall cumulative probability of not being ART treated among ART-eligible patients (according to trial protocol) at baseline clinic visit (Kaplan–Meier curves, ANRS 12249 TasP trial, rural South Africa, N = 514). (b) Cumulative probability of not being ART treated according to eligibility criteria among ART-eligible patients (according to trial protocol) at baseline clinic visit (Kaplan–Meier curves, ANRS 12249 TasP trial, rural South Africa, N = 514).
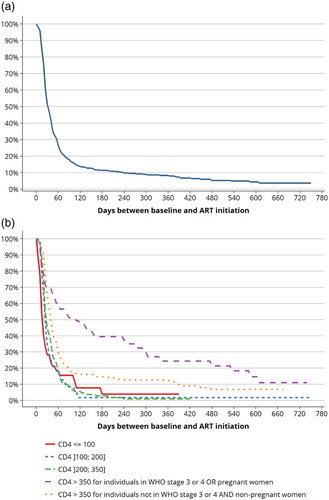
Table 3. Cumulative probabilitya of ART initiation among ART-eligible patients (according to trial protocol) at baseline clinic visit, overall and according to eligibility criteria (ANRS 12249 TasP trial, rural South Africa, N = 514).
Factors associated with ART initiation
presents factors associated with ART initiation in univariate and multivariate analyses.
Explanatory variables included in the multivariate analysis included age, educational level, household assets, food insecurity, agreeing to start ART immediately if diagnosed HIV-positive, disclosure of HIV status to partner, social support, psychological distress score, distance to clinic, CD4 count combined with WHO stage 3/4 and pregnancy for women and cluster profile.
The final multivariate model confirmed most of the statistically significant associations found in univariate analyses. First, all categories of eligible patients according to national guidelines (with CD4 between [100–200], [200–350] and CD4 > 350 for individuals in WHO stage 3/4 or pregnancy) experienced lower ART within M1 compared to those with CD4 ≤ 100 cells/mm3, with a gradient according to CD4 categories (main HR [95% CI]= 0.6 [0.4; 1.0], 0.5 [0.3; 0.8] and 0.2 [0.1; 0.4], respectively). This main effect was no longer statistically significant after the first month (p = 0.188, 0.055 and 0.098, respectively). Similarly, patients with CD4 count >350 cells/mm3 but without WHO stage 3/4 or pregnancy were less likely to initiate ART within M1 compared with those with CD4 count ≤100 cells/mm3 (HR [95% CI] = 0.3 [0.2; 0.4]) but this association was no longer significant beyond M1 (p = .495). Second, reporting a regular partner was not significantly associated with ART initiation within M1 in the multivariate analysis (p = .090), but the effect change after one month was significant, suggesting that patients without a regular partner were less likely to initiate ART after M1 (change HR [95% CI] = 0.4 [0.2; 0.7], main HR after M1 [95% CI] = 0.5 [0.4; 0.8]). Moreover, individuals in Clusters G–J were significantly less likely to initiate ART within the first month (HR [95% CI] = 0.4 [0.3; 0.6]), compared to those in Clusters A–D. However, a significant effect change after M1 (change HR [95% CI] = 1.7 [1.0; 2.9]) compensates the main effect to give a non-significant main effect after M1 (p = .245). Finally, despite no significant association between age and ART initiation in univariate analysis, and also no significant association over the first month of follow-up in multivariate analysis, we observed a significant effect change after M1 for the patients older than 50 years compared with those aged 16–29 years (change HR [95% CI] = 2.0 [1.1; 3.6] and main HR after M1 [95% CI] = 1.5 [1.0; 2.3]).
The result of the global Chi-square test (p < 10−3) confirmed Cox specification using the interaction with time vs. the standard Cox specification in the final multivariate model.
Discussion
This study presents early findings on ART uptake and factors associated with ART initiation among HIV-positive individuals who had linked to care in the trial clinics and were eligible for ART at their first clinic visit within the setting of an ongoing UTT cluster randomized trial in rural KwaZulu-Natal, South Africa.
Our results show that ART uptake was high, with more than four of five individuals initiating ART within the first three months of entering care, a promising observation. Furthermore, the rates of those with CD4 > 350 cells/mm3 and without WHO stage 3/4 or pregnancy who initiated ART were as high as 79.8% at month 3 and 85.3% at M6. However, the concept of “immediate ART” needs to be nuanced. Even in the context of overall high ART uptake, only half the individuals initiated ART within one month with our findings suggesting a more rapid initiation in sicker patients.
Furthermore, participants’ clinical characteristics and cluster of residence were dominant in the first month amongst the factors associated with ART initiation, while the additional effects of socio-demographic variables were observed beyond the first month. Individuals with higher CD4 counts at baseline were indeed less likely to initiate ART compared to those with CD4 ≤ 100 cells/mm3 within the first month of entering care. However, this difference was not observed beyond the first month. Previous studies conducted at a time when ART prescription was still restricted according to clinical and immunological criteria have suggested that individuals with asymptomatic HIV disease or who do not feel sick as a result of their HIV infection are less aware of the need to initiate ART (Fox et al., Citation2010; Plazy, Dray-Spira, Orne-Gliemann, Dabis, & Newell, Citation2014). A study from the same district showed that between 2007 and 2011, only 65.5% of ART-eligible individuals initiated ART; with ART initiation being more likely in females, those ≥25 years and those with low CD4 counts (Plazy et al., Citation2014). However, an alternative explanation for the lack of a difference in ART initiation by CD4 count category after the first month could be that the initial difference observed was driven by healthcare professionals’ (HCPs) practices and may reflect the emergency perceived by physicians to start ART as soon as possible in individuals with CD4 count ≤100 cells/mm3. Conversely, for patients with CD4 count >350 cells/mm3, informal discussions with local HCPs suggest that more time is taken both to assess the potential risks of side effects and to prepare patients to initiate lifelong ART.
In addition, we observed a significant cluster effect on ART initiation with individuals from higher prevalence clusters who attend clinics with low staff–patient ratio being less likely to initiate ART within the first month compared to their counterparts with a higher ratio. This difference is further buttressed by the descriptive analysis showing large variations in ART initiation rates between clusters. As previously, the difference observed in ART initiation rates between clusters disappeared after the first month. This suggests that the initial delay observed was not due to patients with higher CD4 counts being reluctant to start ART but was rather due to clinics’ characteristics such as staffing capacity and workload, and potentially due to triage according to CD4 cell counts by HCP.
South Africa will likely implement soon the 2015 WHO guidelines recommending universal ART, that is, regardless of CD4 count (WHO, Citation2015). This will lead to large numbers of individuals in care becoming eligible for ART. It is conceivable that after many years of guidelines for ART initiation emphasizing the need to focus on HIV-positive individuals with lower CD4 counts who are at increased risk of opportunistic diseases, HCPs may continue to prioritize those with lower CD4 counts over those with higher CD4 counts. Individual benefits of ART would thus remain high [although recent clinical trials indicate clear additional benefits of early ART initiation (INSIGHT START Study Group et al., Citation2015; TEMPRANO ANRS 12136 Study Group et al., Citation2015] but the public health impact of preventing transmission may not be optimal unless the health system is strengthened to deal with the challenges of high patient flow. Innovative approaches to decongest the health system would be required such as adherence clubs, support by peers, three-monthly drug pick-ups and less frequent clinic attendance for stable patients (Duncombe et al., Citation2015; Ellman, Citation2015; Grimsrud, Lesosky, Kalombo, Bekker, & Myer, Citation2016; Khabala et al., Citation2015). Their combination will be necessary to create additional capacity in clinics to see most HIV-positive individuals initiating ART rapidly.
Regarding socio-demographic characteristics, we found that having a regular partner was associated with higher likelihood of ART initiation after one month despite no significant association during the first month. This variable may capture the psychosocial benefit of being in a stable relationship and of mutual support. This association has also been shown in adherence behaviour studies in Cameroon (Boyer et al., Citation2011). Furthermore, while some studies showed that women were more likely to initiate ART that men (Mugglin et al., Citation2012; Plazy et al., Citation2014), we did not find any significant association between ART initiation and gender. This result is however consistent with several recent studies conducted in Nigeria, Malawi and Uganda (Aliyu et al., Citation2014; Feldacker, Johnson, Hosseinipour, Phiri, & Tweya, Citation2012; Katz et al., Citation2011; MacPherson et al., Citation2012). In addition, two studies carried out within our trial population showed no significant association between linkage to care and gender (Plazy et al., Citation2015) but a significant association between HIV testing and gender with a lower acceptability of home-based HIV testing among men (Larmarange et al., Citation2014).
Our study has some limitations. First, our sample size may have limited the statistical power to detect some effects. Second, recent changes in South Africa regarding the adoption in January 2015 of the 2013 WHO guidelines as well as the expected adoption in the near future of the 2015 WHO guidelines may have some implications for the study's results, analysis and interpretation. As patients with CD4 count >350 cells/mm3 will then become eligible for ART according to national guidelines, it is possible that the delay observed during the first month of care in ART initiation amongst individuals with higher CD4 counts may not be replicated. However, considering that large numbers of patients will become immediately eligible to initiate ART with the universal treatment guidelines, coupled with existing health-care system constraints in terms of human resources (Coovadia, Jewkes, Barron, Sanders, & McIntyre, Citation2009; Health Systems Trust, Citation2008), the delay observed in our study may be accentuated, at least at the beginning of the implementation of the new guidelines.
Our results also suggest that in the context of UTT where all HIV-positive individuals are eligible for ART, and where the concept of “pre-ART” care will gradually disappear, ART initiation could be seen as one of the last steps of a shortened entry into the care process starting with HIV diagnosis. Hence, it could be relevant to change our perspective from considering “linkage to care” and “ART initiation” as two separate processes to a global “linkage to ART” perspective, from the first “90” to the second “90” to echo UNAID's 90–90–90 target (UNAIDS, Citation2014).
To conclude, our results can help inform policy on the challenges related to ART initiation in the setting of any UTT strategy. These early findings suggest a good acceptability of ART within a UTT setting, even among individuals with high CD4 counts, but revealed that ART initiation among sicker patients could remain prioritized over those with higher CD4 counts due to staffing capacity as well as HCPs’ practices that will probably take time to change.
Acknowledgements
ANRS (France REcherche Nord & sud Sida-hiv Hépatites) is the sponsor of the TasP trial. The ANRS and the Deutsche Gesellschaft fur Internationale Zusammenarbeit (GIZ) GmbH provided funding for the first phase of the trial. The ANRS and the International Initiative for Impact Evaluation (3ie) provided funding for the second phase of the trial. The trial is conducted with the support of MERCK & Co., Inc. and Gilead Sciences that provided Atripla® drug supply. The Africa Centre receives core funding from the Wellcome Trust (UK), which provides the basis for the population- and clinic-based research at the Centre.
Disclosure statement
C.I. has received honoraria for services rendered to Gilead Sciences. All other authors declare no competing interests.
Additional information
Funding
References
- Aliyu, M. H., Blevins, M., Parrish, D. D., Megazzini, K. M., Gebi, U. I., Muhammad, M. Y., … Wester, C. W. (2014). Risk factors for delayed initiation of combination antiretroviral therapy in rural north central Nigeria. JAIDS Journal of Acquired Immune Deficiency Syndromes, 65(2), e41–49. Retrieved from http://doi.org/10.1097/QAI.0b013e31829ceaec doi: 10.1097/QAI.0b013e31829ceaec
- Boyer, S., Clerc, I., Bonono, C.-R., Marcellin, F., Bilé, P.-C., & Ventelou, B. (2011). Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: Individual and healthcare supply-related factors. Social Science & Medicine, 72(8), 1383–1392. Retrieved from http://doi.org/10.1016/j.socscimed.2011.02.030 doi: 10.1016/j.socscimed.2011.02.030
- Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., … HPTN 052 Study Team. (2011). Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine, 365(6), 493–505. Retrieved from http://doi.org/10.1056/NEJMoa1105243 doi: 10.1056/NEJMoa1105243
- Coovadia, H., Jewkes, R., Barron, P., Sanders, D., & McIntyre, D. (2009). The health and health system of South Africa: Historical roots of current public health challenges. Lancet, 374(9692), 817–834. Retrieved from http://doi.org/10.1016/S0140-6736(09)60951-X doi: 10.1016/S0140-6736(09)60951-X
- Donnell, D., Baeten, J. M., Kiarie, J., Thomas, K. K., Stevens, W., Cohen, C. R., … Partners in Prevention HSV/HIV Transmission Study Team. (2010). Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: A prospective cohort analysis. Lancet, 375(9731), 2092–2098. Retrieved from http://doi.org/10.1016/S0140-6736(10)60705-2 doi: 10.1016/S0140-6736(10)60705-2
- Duncombe, C., Rosenblum, S., Hellmann, N., Holmes, C., Wilkinson, L., Biot, M., … Garnett, G. (2015). Reframing HIV care: Putting people at the centre of antiretroviral delivery. Tropical Medicine & International Health, 20(4), 430–447. Retrieved from http://doi.org/10.1111/tmi.12460 doi: 10.1111/tmi.12460
- Ellman, T. (2015). Demedicalizing AIDS prevention and treatment in Africa. New England Journal of Medicine, 372(4), 303–305. Retrieved from http://doi.org/10.1056/NEJMp1414730 doi: 10.1056/NEJMp1414730
- Feldacker, C., Johnson, D., Hosseinipour, M., Phiri, S., & Tweya, H. (2012). Who starts? Factors associated with starting antiretroviral therapy among eligible patients in two, public HIV clinics in Lilongwe, Malawi. PLoS ONE, 7(11), e50871. Retrieved from http://doi.org/10.1371/journal.pone.0050871 doi: 10.1371/journal.pone.0050871
- Fox, M. P., Mazimba, A., Seidenberg, P., Crooks, D., Sikateyo, B., & Rosen, S. (2010). Barriers to initiation of antiretroviral treatment in rural and urban areas of Zambia: A cross-sectional study of cost, stigma, and perceptions about ART. Journal of the International AIDS Society, 13, 8. Retrieved from http://doi.org/10.1186/1758-2652-13-8 doi: 10.1186/1758-2652-13-8
- Fox, M. P., Shearer, K., Maskew, M., Meyer-Rath, G., Clouse, K., & Sanne, I. (2014). Attrition through multiple stages of pre-treatment and ART HIV care in South Africa. PLoS ONE, 9(10), e110252. Retrieved from http://doi.org/10.1371/journal.pone.0110252 doi: 10.1371/journal.pone.0110252
- Grambsch, P. M., & Therneau, T. M. (1994). Proportional hazards tests and diagnostics based on weighted residuals. Biometrika, 81(3), 515–526. Retrieved from http://doi.org/10.2307/2337123 doi: 10.1093/biomet/81.3.515
- Grimsrud, A., Lesosky, M., Kalombo, C., Bekker, L.-G., & Myer, L. (2016). Implementation and operational research: Community-based adherence clubs for the management of stable antiretroviral therapy patients in Cape Town, South Africa: A cohort study. Journal of Acquired Immune Deficiency Syndromes, 71(1), e16–23. Retrieved from http://doi.org/10.1097/QAI.0000000000000863
- Health Systems Trust (South Africa). (2008). South African health review, 2008. Durban: Health Systems Trust. Retrieved from http://www.hst.org.za/publications/south-african-health-review-2008
- Howards, P. P., Hertz-Picciotto, I., & Poole, C. (2007). Conditions for bias from differential left truncation. American Journal of Epidemiology, 165(4), 444–452. doi: 10.1093/aje/kwk027
- INSIGHT START Study Group, Lundgren, J. D., Babiker, A. G., Gordin, F., Emery, S., Grund, B., … Neaton, J. D. (2015). Initiation of antiretroviral therapy in early asymptomatic HIV infection. New England Journal of Medicine, 373(9), 795–807. Retrieved from http://doi.org/10.1056/NEJMoa1506816 doi: 10.1056/NEJMoa1506816
- Iwuji, C., McGrath, N., de Oliveira, T., Porter, K., Pillay, D., Fisher, M., … Newell, M.-L. (2015). The art of HIV elimination: Past and present science. Journal of AIDS & Clinical Research, 6(11). Retrieved from http://doi.org/10.4172/2155-6113.1000525
- Iwuji, C. C., Orne-Gliemann, J., Tanser, F., Boyer, S., Lessells, R. J., Lert, F., … ANRS 12249 TasP Study Group. (2013). Evaluation of the impact of immediate versus WHO recommendations-guided antiretroviral therapy initiation on HIV incidence: The ANRS 12249 TasP (Treatment as Prevention) trial in Hlabisa sub-district, KwaZulu-Natal, South Africa: Study protocol for a cluster randomised controlled trial. Trials, 14, 230. Retrieved from http://doi.org/10.1186/1745-6215-14-230 doi: 10.1186/1745-6215-14-230
- Katz, I. T., Essien, T., Marinda, E. T., Gray, G. E., Bangsberg, D. R., Martinson, N. A., & De Bruyn, G. (2011). Antiretroviral therapy refusal among newly diagnosed HIV-infected adults. AIDS, 25(17), 2177–2181. Retrieved from http://doi.org/10.1097/QAD.0b013e32834b6464 doi: 10.1097/QAD.0b013e32834b6464
- Khabala, K. B., Edwards, J. K., Baruani, B., Sirengo, M., Musembi, P., Kosgei, R. J., … Reid, T. (2015). Medication adherence clubs: A potential solution to managing large numbers of stable patients with multiple chronic diseases in informal settlements. Tropical Medicine & International Health, 20(10), 1265–1270. Retrieved from http://doi.org/10.1111/tmi.12539 doi: 10.1111/tmi.12539
- Kranzer, K., Govindasamy, D., Ford, N., Johnston, V., & Lawn, S. D. (2012). Quantifying and addressing losses along the continuum of care for people living with HIV infection in sub-Saharan Africa: A systematic review. Journal of the International AIDS Society, 15(2), 17383. Retrieved from http://doi.org/10.7448/IAS.15.2.17383 doi: 10.7448/IAS.15.2.17383
- Kroenke, K., Spitzer, R. L., Williams, J. B. W., & Löwe, B. (2009). An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics, 50(6), 613–621. Retrieved from http://doi.org/10.1176/appi.psy.50.6.613
- Larmarange, J., Balestre, É., Orne-Gliemann, J., Iwuji, C., Okesola, N., Newell, M.-L., … Lert, F. (2014). HIV ascertainment through repeat home-based testing in the context of a treatment as prevention trial (ANRS 12249 TasP) in rural South Africa. AIDS Research and Human Retroviruses, 30(S1), A287–A287. Retrieved from http://doi.org/10.1089/aid.2014.5650.abstract doi: 10.1089/aid.2014.5650.abstract
- Löwe, B., Wahl, I., Rose, M., Spitzer, C., Glaesmer, H., Wingenfeld, K., … Brähler, E. (2010). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders, 122(1–2), 86–95. Retrieved from http://doi.org/10.1016/j.jad.2009.06.019 doi: 10.1016/j.jad.2009.06.019
- MacPherson, P., MacPherson, E. E., Mwale, D., Bertel Squire, S., Makombe, S. D., Corbett, E. L., … Desmond, N. (2012). Barriers and facilitators to linkage to ART in primary care: A qualitative study of patients and providers in Blantyre, Malawi. Journal of the International AIDS Society, 15(2), 18020. Retrieved from http://doi.org/10.7448/IAS.15.2.18020 doi: 10.7448/IAS.15.2.18020
- McNairy, M. L., Lamb, M. R., Abrams, E. J., Elul, B., Sahabo, R., Hawken, M. P., … Identifying Optimal Models of HIV Care and Treatment in Sub-Saharan Africa Study. (2015). Use of a comprehensive HIV care cascade for evaluating HIV program performance: Findings from 4 Sub-Saharan African countries. JAIDS Journal of Acquired Immune Deficiency Syndromes, 70(2), e44–51. Retrieved from http://doi.org/10.1097/QAI.0000000000000745 doi: 10.1097/QAI.0000000000000745
- Morris, S. S., Carletto, C., Hoddinott, J., & Christiaensen, L. J. (2000). Validity of rapid estimates of household wealth and income for health surveys in rural Africa. Journal of Epidemiology and Community Health, 54(5), 381–387. doi: 10.1136/jech.54.5.381
- Mugglin, C., Estill, J., Wandeler, G., Bender, N., Egger, M., Gsponer, T., … IeDEA Southern Africa. (2012). Loss to programme between HIV diagnosis and initiation of antiretroviral therapy in sub-Saharan Africa: Systematic review and meta-analysis. Tropical Medicine & International Health, 17(12), 1509–1520. Retrieved from http://doi.org/10.1111/j.1365-3156.2012.03089.x doi: 10.1111/j.1365-3156.2012.03089.x
- Musheke, M., Ntalasha, H., Gari, S., McKenzie, O., Bond, V., Martin-Hilber, A., & Merten, S. (2013). A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health, 13, 220. Retrieved from http://doi.org/10.1186/1471-2458-13-220 doi: 10.1186/1471-2458-13-220
- National Department of Health, Republic of South Africa. (2013, March). The South African antiretroviral treatment guidelines 2013. Retrieved from http://www.sahivsoc.org/upload/documents/2013%20ART%20Guidelines-Short%20Combined%20FINAL%20draft%20guidelines%2014%20March%202013.pdf
- National Department of Health, Republic of South Africa. (2015, April). National Consolidated Guidelines for the prevention of mother-to-child transmission of HIV (PMTCT) and the management of HIV in Children, adolescents and adults. Retrieved from http://www.sahivsoc.org/upload/documents/ART%20Guidelines%2015052015.pdf
- Orne-Gliemann, J., Larmarange, J., Boyer, S., Iwuji, C., McGrath, N., Bärnighausen, T., … ANRS 12249 TasP Group. (2015). Addressing social issues in a universal HIV test and treat intervention trial (ANRS 12249 TasP) in South Africa: Methods for appraisal. BMC Public Health, 15, 209. Retrieved from http://doi.org/10.1186/s12889-015-1344-y doi: 10.1186/s12889-015-1344-y
- Plazy, M., Dray-Spira, R., Orne-Gliemann, J., Dabis, F., & Newell, M.-L. (2014). Continuum in HIV care from entry to ART initiation in rural KwaZulu-Natal, South Africa. Tropical Medicine & International Health, 19(6), 680–689. Retrieved from http://doi.org/10.1111/tmi.12301 doi: 10.1111/tmi.12301
- Plazy, M., El Farouki, K., Iwuji, C., Okesola, N., Orne-Gliemann, J., Larmarange, J., … ANRS 12249 TasP Study Group. (2015). Entry into care following universal home-based HIV testing in rural KwaZulu-Natal, South Africa: The ANRS TasP 12249 cluster-randomised trial. Presented at the 8th IAS conference on HIV Pathogeneis, Treatment & Prevention, Vancouver, Communication orale n°WEAD0103.
- StataCorp. (2011). Stata statistical software: Release 12. College Station TSL.
- Tanser, F., Bärnighausen, T., Grapsa, E., Zaidi, J., & Newell, M.-L. (2013). High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science, 339(6122), 966–971. Retrieved from http://doi.org/10.1126/science.1228160 doi: 10.1126/science.1228160
- TEMPRANO ANRS 12136 Study Group, Danel, C., Moh, R., Gabillard, D., Badje, A., Le Carrou, J., … Anglaret, X. (2015). A trial of early antiretrovirals and isoniazid preventive therapy in Africa. New England Journal of Medicine, 373(9), 808–822. Retrieved from http://doi.org/10.1056/NEJMoa1507198 doi: 10.1056/NEJMoa1507198
- UNAIDS. (2014). 90-90-90. An ambitious treatment target to help end the AIDS epidemic. Retrieved from http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf
- WHO. (2010). Antiretroviral therapy for HIV infection in adults and adolescents: Recommendations for a public health approach. World Health Organization. Retrieved from http://apps.who.int/iris/bitstream/10665/44379/1/9789241599764_eng.pdf
- WHO. (2013). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva: World Health Organization. Retrieved from http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf
- WHO. (2015). Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. World Health Organization. Retrieved from http://apps.who.int/iris/bitstream/10665/186275/1/9789241509565_eng.pdf
- Zaidi, J., Grapsa, E., Tanser, F., Newell, M.-L., & Bärnighausen, T. (2013). Dramatic increase in HIV prevalence after scale-up of antiretroviral treatment. AIDS, 27(14), 2301–2305. Retrieved from http://doi.org/10.1097/QAD.0b013e328362e832 doi: 10.1097/QAD.0b013e328362e832