ABSTRACT
Sweden has one of the best HIV treatment outcomes in the world and an estimated 95% of all diagnosed people living with HIV are virally suppressed, but the quality of life (QoL) is understudied. The aim of this study was to examine the associations between variables within sociodemographic, behavioural, clinical, psychological, sexual life, social support and personal resource component and the QoL of people living with HIV in Sweden. Data were derived from a cross-sectional, nation-wide survey completed by 15% (n = 1096) of all people living with HIV and collected at 15 infectious disease clinics and 2 needle exchange sites during 2014. Ordinal univariate and multivariate logistic regression analyses were used to examine associations between potential contributors and QoL. Respondents reported high QoL: 63% rated their QoL 7 or higher on a scale ranging from 0 to 10. QoL was independent of gender, age, mode of HIV transmission and country of origin. Lower QoL was associated with recent homelessness, hazardous alcohol consumption, comorbidities, treatment side-effects, HIV-related physical symptoms, hopelessness, negative self-image, sexual dissatisfaction, and negative changes in sex life after HIV. The QoL of people living with HIV in Sweden was high overall, but still significantly influenced by HIV.
Introduction
Effective antiretroviral treatment (ART) has transformed HIV into a chronic and manageable condition. An increasing number of people living with HIV are achieving viral suppression as a result of increased access, simpler dosages and fewer treatment side-effects (Joint United Nations Programme on HIV/AIDS (UNAIDS), Citation2014). As a result, a new paradigm beyond viral suppression has emerged focusing on healthy ageing and high quality of life (QoL) (Lazarus et al., Citation2016).
Studies report a relatively high QoL in people living with HIV during the era of ART (Aragonés-López, Pérez-Ávila, Smith Fawzi, & Castro, Citation2012; George, Bergin, Clarke, Courtney, & Codd, Citation2016; Nobre, Pereira, Roine, Sintonen, & Sutinen, Citation2017), but worse compared to people without HIV, particularly with regards to mental health (Miners et al., Citation2014; Pedersen et al., Citation2015). Research suggests that various sociodemographic, clinical and psychological factors are associated with the QoL of people living with HIV (Degroote, Vogelaers, & Vandijck, Citation2014). Despite significant improvements in disease management, people living with HIV continue to experience challenges associated with the disease such as stigma (Fuster-Ruizdeapodaca, Molero, Holgado, & Mayordomo, Citation2014; Holzemer et al., Citation2009; Rao et al., Citation2012; Reinius, Wiklander, Wettergren, Svedhem, & Eriksson, Citation2018; Rydstrom, Wiklander, Naver, Ygge, & Eriksson, Citation2016; Slater et al., Citation2015), loneliness (Vincent et al., Citation2017), depression (Niderost & Imhof, Citation2016; Nobre et al., Citation2017), comorbidities (Guaraldi et al., Citation2011; Hasse et al., Citation2011; Schouten et al., Citation2014), and financial stress (Niderost & Imhof, Citation2016; Nobre et al., Citation2017), all of which are found to be associated with QoL.
Few studies assessing the QoL of people living with HIV have considered the multidimensional contribution and interaction between various life domains that concurrently could influence QoL and only a handful include a representative sample (Aragonés-López et al., Citation2012; Douab et al., Citation2014).
Sweden is a low HIV prevalence country. It was the first country to reach the UNAIDS 90-90-90 targets of a continuum of care and an estimated 95% of all diagnosed people with HIV are virally suppressed (Gisslen et al., Citation2017). However, the QoL in this group remains unknown, as the few existing studies were mostly performed before the era of ART and viral suppression (Eriksson, Bratt, Sandström, & Nordström, Citation2005; Eriksson, Nordstrom, Berglund, & Sandstrom, Citation2000; Schönnesson, Citation1999).
The aim of this study was to examine the association between variables within sociodemographic, behavioural, clinical, psychological, sexual life, social support and personal resource component and self-reported QoL among people living with HIV in Sweden.
Materials and methods
Data collection
Data were collected through a nation-wide survey, “Living with HIV in Sweden”, designed to explore self-reported QoL and its correlates through an anonymous, self-reported questionnaire (Schönnesson et al., Citation2018). Data were collected at 15 clinics and two needle-exchange centres across the country, together covering 75% of all known patients living with HIV at the time of data collection. Between December 2013 and June 2014, eligible outpatients (>18 years old with known HIV diagnosis for >6 months) who visited one of the data collection sites were offered to participate in the study. The questionnaire was available in 10 languages in order to include migrants, and was developed and piloted in collaboration with the three largest non-governmental HIV organisations in Sweden: HIV-Sweden, National HIV Association Noah’s Ark and Stockholm’s Drug Users Union. The data collection procedures are described in further detail elsewhere (Schönnesson et al., Citation2018).
Ethics
The study was approved by the Regional Ethical Review Board in Stockholm (DNR 2013/1552-31/4). Study participation was voluntary and anonymous. Information about the study and consent was provided in the questionnaire.
Measures
Dependent variable
QoL was assessed by a single question asking participants to rate their quality of life on a visual analogue scale ranging from 0 (very poor QoL) to 10 (very good QoL). QoL is thus an ordinal variable with 11 categories.
Independent variables
The sociodemographic component included gender, age, birth origin, employment, relationship status and recent homelessness. Education level followed the standard Swedish education system: 0–9, 10–12 or >12 years. Monthly income was reported as one out of five income categories later dichotomised into lower income and middle/high income. Sexual orientation was coded to heterosexual, non-heterosexual or missing/do not want to answer.
The behavioural component
The behavioural component, indicating health-risk behaviours, comprised of smoking status (no, I never smoked; yes, but I quit; yes), drug-use, and alcohol consumption. Recent drug use was assessed by the question “have you taken any drugs or prescription medication over the past 6 months without a doctor’s orders?” (yes; no; do not want to answer/missing). Alcohol consumption was assessed using the Alcohol Use Disorders Identification Test (Audit-C) (Bush, Kivlahan, McDonell, Fihn, & Bradley, Citation1998), which comprises three questions about frequency of alcohol consumption, amount of alcohol consumed during a typical drinking session, and frequency of drinking six or more glasses during one session. Each question is scored 0–4 points and summed for a total score ranging from 1 to 12 points. Scores 6–12 (men) and 5–12 (women) indicate positive screens for hazardous alcohol consumption (The Public Health Agency of Sweden, Citation2016).
The clinical component
Time since HIV diagnosis was self-reported and categorised into: <1; 1–5; 5–10, and; >10 years. Self-reported mode of HIV transmission allowed respondents to choose multiple options if uncertain: sex with a man/sex with a woman/blood products; needles or syringes/from my mother/do not want to answer/other. The option “needles or syringes” was prioritised above all other options. The second prioritisation was sex with a man (in order to identify sex between men). All other options were prioritised over the “other” option. The variable comorbidities were dichotomised into “yes” (hepatitis C, diabetes, high blood pressure, cancer, substance abuse, mental illness) or “no”. The question “have you experienced any physical symptoms over the past six months that you associated with HIV?” (yes, no, I don’t know) was used to screen for HIV-related physical symptoms. Side-effects from ART were also analysed by asking respondents if they experienced any physical and/or psychological ART side-effects and if so, whether they were bothered by these side-effects (yes/no).
The psychological component
Psychological distress was assessed using the Beck Hopelessness Scale (Beck, Weissman, Lester, & Trexler, Citation1974), which includes 9 positive and 11 negative true/false statements about the future. After reverse scoring of positively worded items, items were summed to give a total score ranging from 0 to 20, with a higher score reflecting increased hopelessness (score 0–3 “absence of hopelessness”; scores 4–8 “mild”; scores 9–12 “moderate” and scores >12 “severe hopelessness”).
We used a 12 items Swedish short-form version (Lindberg et al., Citation2014; Reinius et al., Citation2017) of the HIV Stigma Scale (Berger, Ferrans, & Lashley, Citation2001) to assess four subscales of stigma (personalised stigma, negative self-image, concerns about public attitudes and disclosure concerns), each with three items rated on a four-point scale from “strongly disagree” (1) to “strongly agree” (4) (Reinius et al., Citation2017). Each subscale was then summed to a score from 3 to 12. Subscale scores 3–5 were considered “lower ratings”, scores 6–9 as “fairly high” and scores 10–12 as “high stigma”.
Satisfaction with HIV disclosure was assessed by the question “Are you as open about having HIV as you would like to be?” (yes/would like to be more open/would like to be less open/do not want to answer).
The sexual life component
Sexual satisfaction was assessed using an item from the Life Satisfaction checklist (Fugl-Meyer, Bränholm, & Fugl-Meyer, Citation1991): “With my sex life I am … ” (a 6-point Likert-like scale indicating satisfaction level), dichotomised into “satisfied” (very satisfied/satisfied/rather satisfied) versus “dissatisfied” (rather dissatisfied/dissatisfied/very dissatisfied). Changes in sex life due to HIV was assessed by asking “Has being HIV-positive changed your sex life?” (no change/positive change/negative change/too personal or cannot decide).
The social support component
HIV-related support was assessed by “how often do your partners, family members or friends support you in living with HIV?”. The variable was dichotomised into “have HIV-related support” (always, often, sometimes) and “limited/no HIV-related support” (rarely, never, I have not told anyone about my HIV).
The personal resource component
Change in perceived self-esteem due to HIV was assessed by asking “has being HIV-positive changed your sense of self-esteem?” (no change/positive/negative change). Meaningfulness of life after HIV was assessed by asking “has being HIV-positive changed your sense that life is meaningful?” (“life is as meaningful as before”, “life is more meaningful” and “life is less meaningful”).
Statistical analyses
Stata version 13.1 (StataCorp LLC, College Station, TX) was used for the analyses.
Univariate associations were assessed using ordinal logistic regression to examine each of the explanatory independent variables listed above with the outcome QoL. Subsequently, significant variables (p ≤ .05) from the univariate analyses were included in a multivariate ordinal logistic regression analysis. However, all sociodemographic and behavioural covariates listed above, and the variable “time since HIV diagnosis”, were included in the multivariate analysis, regardless of significance level in univariate analysis. The measures of association are presented as crude and adjusted odds ratios, with 95% confidence intervals.
Originally, 1100 respondents completed the survey. However, the final analysis includes 1086 respondents after removal of 4 ineligible respondents and 10 respondents who did not indicate their gender.
Management of missing data
A non-response or the response “do not want to answer” on the items sexual orientation, recent drug-use and mode of HIV transmission were coded as missing/do not want to answer. The reason being that these (non)responses could have had a negative association with QoL, an information that would have otherwise been lost if these (non)responses were treated as missing observations. Remaining missing data was managed by employing multiple imputations, using chained equations (White, Royston, & Wood, Citation2011). Twenty imputed datasets were used in the estimation of the analysis. In the imputation modelling, logistic regression was used for the binary variables, ordinal logistic regression for the ordinal variables, multinomial logistic regression for the nominal variables, and linear regression for the continuous variable. The dependent variable was also included in the imputation modelling, but excluding observations with missing values (von Hippel, Citation2007).
Results
Sociodemographic and HIV-related characteristics
details the descriptive data on the sociodemographic and HIV-related characteristics of the study respondents. Most respondents were men (70%), 29% were women and 1% reported another gender identity. The average age was 47.6 years and 41% had a migration background. Nearly half (47%) had higher education (>12 years) while 19% had not completed secondary education and 55% had lower monthly income. The majority worked or studied (75%), 43% were non-heterosexual and 57% had a partner. The most common mode of HIV transmission was sex between men (41%), followed by heterosexual sex (32%) and injecting drug use (11%). Nearly half (48%) had been living with HIV for >10 years, and 95% were on ART.
Table 1. Sociodemographic and HIV-related characteristics of study respondents (n = 1086).
Quality of life
On average, QoL was rated at 6.8 out of a maximum of 10, but 63% rated their QoL at 7 or higher.
Univariate logistic regression analyses predicting quality of life
In the univariate analysis (), the following variables within the sociodemographic component were significantly and negatively associated with QoL (p < .05): lower income, unemployment, not having a partner and recent homelessness.
Table 2. Univariate and multivariate regression analyses of the components associated with quality of life (n = 1086).
As to the behavioural component, current smoking, drug use during the last 6 months and hazardous alcohol consumption were negatively associated with lower QoL. Injecting drug use as the transmission mode for HIV, a comorbidity, experiencing HIV-related physical symptoms, and side-effects of ART were clinical component significantly and negatively associated with QoL.
With regards to variables within the psychological component, hopelessness was negatively associated with QoL, as well as personalised stigma, disclosure concerns, negative self-image, and concerns with public attitudes. Additionally, wishing that one could be more open about one’s HIV status and wishing that one could be less open were negatively associated with QoL.
Dissatisfaction with sex life, as well as negative changes in sex life after HIV (sexual life component), were strongly associated with lower QoL.
Having limited/no HIV-related support (social support component) also decreased QoL. As to the personal resource component, a negative change in perceived self-esteem due to HIV, and reporting a less meaningful life after receiving a diagnosis of HIV were negatively associated with QoL.
Multivariate logistic regression analysis predicting quality of life
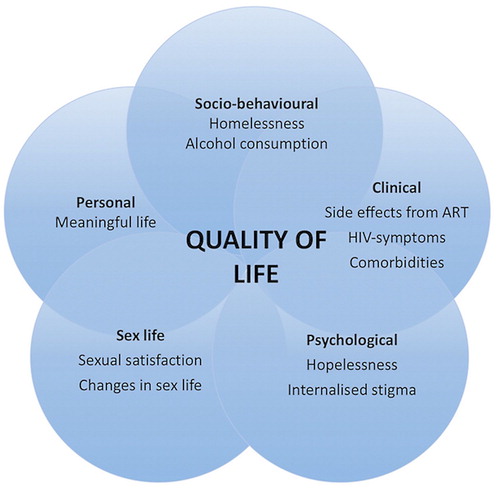
The variables within each component which were associated with QoL in the multivariate analysis are presented in and further illustrated in . Variables within the sociodemographic and behavioural components significantly associated with lower QoL were recent homelessness and hazardous alcohol consumption.
Figure 1. Significant components for quality of life among people living with HIV in a context of good treatment outcomes.
Variables within the clinical component significantly associated with lower QoL were comorbidity, HIV-related physical symptoms, and side-effects of ART.
Hopelessness and negative self-image (psychological component) were associated with lower QoL. Dissatisfaction with sex life and negative changes in sex life after HIV (sexual life component) also remained negatively associated with QoL in the multivariate analyses, as did perceiving life as less meaningful after HIV (personal resource component).
The variables age, gender, birth origin and sexual orientation were not associated with QoL neither in univariate nor multivariate analyses. Change in perceived self-esteem due to HIV and HIV-related support were not associated with QoL when adjusting for confounding in the multivariate model.
Discussion
This study, focusing on self-reported QoL and its associated salient components in a national, representative sample of people living with HIV in Sweden, found that the majority rated their overall QoL highly – 7 on a scale ranging from 0 to 10. As previous studies similarly found relatively high QoL among people living with HIV (Aragonés-López et al., Citation2012; George et al., Citation2016; Nobre et al., Citation2017), it is likely that our results are transferable to other European countries with similar epidemiological patterns that have reached the UNAIDS 90-90-90 targets. In the current study, most people were virally suppressed and were below the age of 50, suggesting that overall, QoL may not be significantly impaired by HIV. However, stigma and negative sex life changes remained a significant challenge for the majority of respondents, despite having lived with HIV for over 10 years, and thus having had time to adjust to their HIV diagnosis. QoL is believed to be a dynamic and a relative concept, people tend to adopt to changing aspirations and circumstances (de Haes & van Knippenberg, Citation1985). A significant proportion of respondents, however, reported QoL scores of lower magnitude. Some were related to HIV, but others to social circumstances which influence life negatively for most people.
Sociodemographic and behavioural component
Interestingly, we did not find significant associations between gender, employment, income level, relationship status and QoL, unlike recent findings from a similar setting (Nobre et al., Citation2017). Recent homelessness was correlated with lower QoL. It is probable that the effect of homelessness on QoL is more severe than the effect of HIV.
Hazardous alcohol consumption was correlated with lower QoL, which is echoed in previous findings (Tran, Nguyen, Do, Nguyen, & Maher, Citation2014).
Clinical component
Similarly to other studies (George et al., Citation2016; Maiese, Johnson, Bancroft, Hunter, & Wu, Citation2016; Rüütel, Pisarev, Loit, & Uusküla, Citation2009), HIV-related symptoms and side-effects from ART were associated with lower QoL. This association could be explained by the impairment that these symptoms may cause, their effect on overall health, and by making HIV more noticeable in one’s life. Consistent with other studies (George et al., Citation2016; Langebeek et al., Citation2017; Nobre et al., Citation2017), we found a link between comorbidities and lower QoL.
Psychological component
About one in four respondents experienced moderate or severe hopelessness (data not shown) which significantly decreased QoL. Hopelessness is a core characteristic of depression (Beck et al., Citation1974) and the association between depression and poorer QoL is well known (Engelhard et al., Citation2018; Langebeek et al., Citation2017; Miners et al., Citation2014; Nobre et al., Citation2017).
Our results demonstrated that negative self-image as a result of stigma predicted lower QoL, supporting earlier studies (Fuster-Ruizdeapodaca et al., Citation2014; Grov, Golub, Parsons, Brennan, & Karpiak, Citation2010; Reinius et al., Citation2018). Stigma may introduce barriers to everyday life, particularly with relation to social and sexual relationships, which in turn may have a negative impact on QoL.
Sexual life component
Negative changes in sex life after HIV diagnosis and dissatisfaction with sex life were significantly associated with lower QoL. Although sexual wellbeing is an important component of QoL, few HIV-related QoL studies include these aspects (Oberje, Dima, van Hulzen, Prins, & de Bruin, Citation2015). However, a recent Swedish study found that negative changes in sex life after HIV diagnosis correlated with sexual dissatisfaction. It is probable that negative changes in sex life after HIV are related to the Swedish Communicable Disease Act, which obligates people living with HIV to disclose their HIV status to sexual partners (unless this duty has been removed by their doctor under the condition that condoms are always used and that repeated measures of viral loads over the last six months confirm undetectable virus levels) (Schönnesson et al., Citation2018). This legal obligation may cause distress, concerns about rejection (Kaida et al., Citation2015), and relationship challenges including fear of transmitting HIV to sexual partners (Kapiriri, Tharao, Muchenje, Masinde, & Ongoiba, Citation2016; Mykhalovskiy, Citation2011).
Personal resource component
Perceiving life as less meaningful after HIV diagnosis correlated with lower QoL. Meaningfulness with life might change for some who experience that HIV have a negative effect on their health, relationships, and experiences of stigma (Audet, Wagner, & Wallston, Citation2015).
Limitations and strengths
We cannot make assumptions about the temporality of the associations found due to the cross-sectional character of our data. The data were self-reported and potentially affected by social desirability. However, the study was anonymous which decreased the risk of this type of bias. No existing Swedish studies have measured QoL in the general population as thoroughly as our study did, undermining direct comparisons. This is also by far the largest and most inclusive Swedish study about QoL among people living with HIV in a context of highly successful treatment outcomes. It includes previously understudied populations including migrants and injecting drug users and is considered representative for people living with HIV in Sweden.
Conclusion
Our results indicate that despite major improvements in disease management, HIV still has a major bearing on people’s lives. There is a need to adopt an integrated and multidisciplinary care approach for people living with HIV, catering for a wide range of concerns including prevention and early detection of comorbidities, in order to improve the QoL in this group. Addressing various psychological, clinical, and sexual issues is a precondition to ensure high overall QoL alongside viral suppression. Our results have clinical implications which are listed below.
Clinical implications
Hopelessness is an important issue that needs to be better addressed by health care providers. Perceiving life as less meaningful after an HIV diagnosis could cause hopelessness. Internalised stigma is closely related to these experiences. Healthcare providers should, therefore, be aware of these experiences and identify symptoms of poor mental health and internalised stigma, in order to be able to address these issues.
Non-communicable diseases that typically affect people living with HIV (Guaraldi et al., Citation2011) require regular screening, which may involve addressing lifestyle-related risk factors.
Our findings suggest that patients’ experience ART side-effects to be more prevalent than many clinicians would expect. Some side-effects could be confused with disease symptoms, but it is more likely that some of the symptoms experienced by patients, were, in fact, attributable to other factors unrelated to ART or HIV-infection. These findings reinforce the importance of communication between the treating physician and the patient, which requires careful attention to the patients’ concerns and treatment experiences in order to mitigate potential symptoms that could affect QoL or adherence to ART.
In the present study, 28% of respondents expressed doubt about being able to discuss sexual matters with their HIV physician and 23% reported not having sex with anybody since their HIV-diagnosis (data not shown). Given the importance of sexual satisfaction for QoL, it is important that healthcare providers and counsellors initiate discussions on sexual matters and relationship challenges with patients.
Acknowledgements
Authors’ contributions: G.Z.A was involved in data collection, data analyses and preparation of the article. L.E.E, L.N.S and P.M were involved in the design of the study and interpretation of study results. J.H performed the statistical analyses and A.M.E is the principal investigator of the study “Living with HIV in Sweden” and was involved in the design of the study, data collection and results interpretation. All authors critically reviewed and revised the article and approved the final version of the article.
We would like to thank all study participants for contributing to this study. The authors would also like to thank Maria Lindberg Reinius for her contribution to the analytical approach of this study.
We are grateful to all 17 data collection sites and the persons who recruited patients:
Marie Hultén and Mira Karlsson (Karolinska University Hospital, Stockholm), Lars Navér (Astrid Lindgren Children’s hospital, Stockholm), Henning Montelius and Olof Blivik (Blekinge Hospital, Karlskrona), Niklas Eklund (S. tockholm’s Drug Users Union, Needle exchange programme by Gullmarsplan, Stockholm), Kristina Landås and Nils Kuylenstierna (Falu Hospital, Falun), Ann-Louise, Muhren-Tysklind and Farshad Azimi (Gävle Hospital, Gävle), Björn Nordberg (Helsingborg Hospital, Helsingborg), Erika Spångberg and Martin Kåberg (Needle exchange programme at S:t Görans Hospital, Stockholm and Karolinska University Hospital, Stockholm), Marianne Schlaug (Skaraborg Hospital, Skövde), Annica Boija and Jonas Bonnedahl (Kalmar Hospital, Kalmar), Helena Lindmark and Carolina Lundberg (University Hospital of Umeå, Umeå), Anneli Eriksson, Anette Forsberg, Peter Lanbeck and Leo Flamholc (Skåne University Hospital, Malmö), Suzanne Wendahl (Sunderby Hospital, Luleå), Lisbeth Scott, Ann-Sofie Johansson Swedberg and Per Josefson (Örebro University Hospital, Örebro), Lena Lindborg and Kajsa Flisager (Venhälsan, Stockholm South General Hospital (SöS), Stockholm), Sture Persson (Visby Hospital, Visby) and, Aylin Yilmaz (Sahlgrenska University Hospital, Göteborg).
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Galit Zeluf-Andersson http://orcid.org/0000-0001-6715-1792
Lars E. Eriksson http://orcid.org/0000-0001-5121-5325
Additional information
Funding
References
- Aragonés-López, C., Pérez-Ávila, J., Smith Fawzi, M. C., & Castro, A. (2012). Quality of life of people with HIV/AIDS receiving antiretroviral therapy in Cuba: A cross-sectional study of the national population. American Journal of Public Health, 102(5), 884–892. doi: 10.2105/AJPH.2011.300450
- Audet, C. M., Wagner, L. J., & Wallston, K. A. (2015). Finding meaning in life while living with HIV: Validation of a novel HIV meaningfulness scale among HIV-infected participants living in Tennessee. BMC Psychology, 3, 15. doi: 10.1186/s40359-015-0070-7
- Beck, A. T., Weissman, A., Lester, D., & Trexler, L. (1974). The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology, 42(6), 861–865. doi: 10.1037/h0037562
- Berger, B. E., Ferrans, C. E., & Lashley, F. R. (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24(6), 518–529. doi: 10.1002/nur.10011
- Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory care quality improvement project (ACQUIP). Alcohol use disorders identification test. Archives of Internal Medicine, 158(16), 1789–1795. doi: 10.1001/archinte.158.16.1789
- Degroote, S., Vogelaers, D., & Vandijck, D. M. (2014). What determines health-related quality of life among people living with HIV: An updated review of the literature. Archives of Public Health, 72(1), 40. doi: 10.1186/2049-3258-72-40
- de Haes, J. C., & van Knippenberg, F. C. (1985). The quality of life of cancer patients: A review of the literature. Social Science & Medicine, 20(8), 809–817. doi: 10.1016/0277-9536(85)90335-1
- Douab, T., Marcellin, F., Vilotitch, A., Protopopescu, C., Préau, M., Suzan-Monti, M., … Dray-Spira, R. (2014). Health-related quality of life of people living with HIV followed up in hospitals in France: Comparing trends and correlates between 2003 and 2011 (ANRS-VESPA and VESPA2 national surveys). AIDS Care, 26(sup1), S29–S40. doi: 10.1080/09540121.2014.906553
- Engelhard, E. A. N., Smit, C., van Dijk, P. R., Kuijper, T. M., Wermeling, P. R., Weel, A. E., … Nieuwkerk, P. T. (2018). Health-related quality of life of people with HIV: An assessment of patient related factors and comparison with other chronic diseases. AIDS, 32(1), 103–112. doi: 10.1097/QAD.0000000000001672
- Eriksson, L. E., Bratt, G. A., Sandström, E., & Nordström, G. (2005). The two-year impact of first generation protease inhibitor based antiretroviral therapy (PI-ART) on health-related quality of life. Health and Quality of Life Outcomes, 3(1), 32. doi: 10.1186/1477-7525-3-32
- Eriksson, L. E., Nordstrom, G., Berglund, T., & Sandstrom, E. (2000). The health-related quality of life in a Swedish sample of HIV-infected persons. Journal of Advanced Nursing, 32(5), 1213–1223. doi: 10.1046/j.1365-2648.2000.01592.x
- Fugl-Meyer, A. R., Bränholm, I.-B., & Fugl-Meyer, K. S. (1991). Happiness and domain-specific life satisfaction in adult northern Swedes. Clinical Rehabilitation, 5. doi: 10.1177/026921559100500105
- Fuster-Ruizdeapodaca, M. J., Molero, F., Holgado, F. P., & Mayordomo, S. (2014). Enacted and internalized stigma and quality of life among people with HIV: The role of group identity. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 23(7), 1967–1975. doi: 10.1007/s11136-014-0653-4
- George, S., Bergin, C., Clarke, S., Courtney, G., & Codd, M. B. (2016). Health-related quality of life and associated factors in people with HIV: An Irish cohort study. Health and Quality of Life Outcomes, 14(1), 115. doi: 10.1186/s12955-016-0517-4
- Gisslen, M., Svedhem, V., Lindborg, L., Flamholc, L., Norrgren, H., Wendahl, S., … Sonnerborg, A. (2017). Sweden, the first country to achieve the joint United Nations programme on HIV/AIDS (UNAIDS)/World Health Organization (WHO) 90-90-90 continuum of HIV care targets. HIV Medicine, 18(4), 305–307. doi: 10.1111/hiv.12431
- Grov, C., Golub, S. A., Parsons, J. T., Brennan, M., & Karpiak, S. E. (2010). Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care, 22(5), 630–639. doi: 10.1080/09540120903280901
- Guaraldi, G., Orlando, G., Zona, S., Menozzi, M., Carli, F., Garlassi, E., … Palella, F. (2011). Premature age-related comorbidities Among HIV-infected persons compared with the general population. Clinical Infectious Diseases, 53(11), 1120–1126. doi: 10.1093/cid/cir627
- Hasse, B., Ledergerber, B., Furrer, H., Battegay, M., Hirschel, B., Cavassini, M., … Weber, R. (2011). Morbidity and aging in HIV-infected persons: The Swiss HIV cohort study. Clinical Infectious Diseases, 53(11), 1130–1139. doi: 10.1093/cid/cir626
- Holzemer, W. L., Human, S., Arudo, J., Rosa, M. E., Hamilton, M. J., Corless, I., … Maryland, M. (2009). Exploring HIV stigma and quality of life for persons living with HIV infection. Journal of the Association of Nurses in AIDS Care, 20(3), 161–168. doi: 10.1016/j.jana.2009.02.002
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2014). 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS. Retrieved from http://www.unaids.org/en/resources/documents/2017/90-90-90
- Kaida, A., Carter, A., de Pokomandy, A., Patterson, S., Proulx-Boucher, K., Nohpal, A., … Loutfy, M. (2015). Sexual inactivity and sexual satisfaction among women living with HIV in Canada in the context of growing social, legal and public health surveillance. Journal of the International AIDS Society, 18(Suppl 5), 20284.
- Kapiriri, L., Tharao, W., Muchenje, M., Masinde, K. I., & Ongoiba, F. (2016). ‘ … They should understand why … ’ The knowledge, attitudes and impact of the HIV criminalisation law on a sample of HIV+ women living in Ontario. Global Public Health, 11(10), 1231–1245. doi: 10.1080/17441692.2016.1146318
- Langebeek, N., Kooij, K. W., Wit, F. W., Stolte, I. G., Sprangers, M. A. G., Reiss, P., & Nieuwkerk, P. T. (2017). Impact of comorbidity and ageing on health-related quality of life in HIV-positive and HIV-negative individuals. AIDS, 31(10), 1471–1481. doi: 10.1097/QAD.0000000000001511
- Lazarus, J. V., Safreed-Harmon, K., Barton, S. E., Costagliola, D., Dedes, N., Del Amo Valero, J., … Rockstroh, J. K. (2016). Beyond viral suppression of HIV - the new quality of life frontier. BMC Medicine, 14(1), 94. doi: 10.1186/s12916-016-0640-4
- Lindberg, M. H., Wettergren, L., Wiklander, M., Svedhem-Johansson, V., Eriksson, L. E. & Federici, S. (2014). Psychometric evaluation of the HIV stigma scale in a Swedish context. PLOS ONE, 9(12), e114867. doi: 10.1371/journal.pone.0114867
- Maiese, E. M., Johnson, P. T., Bancroft, T., Hunter, A. G., & Wu, A. W. (2016). Quality of life of HIV-infected patients who switch antiretroviral medication due to side effects or other reasons. Current Medical Research and Opinion, 32(12), 2039–2046. doi: 10.1080/03007995.2016.1227776
- Miners, A., Phillips, A., Kreif, N., Rodger, A., Speakman, A., Fisher, M., … Lampe, F. C. (2014). Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: A cross-sectional comparison with the general population. The Lancet HIV, 1(1), e32–40. doi: 10.1016/S2352-3018(14)70018-9
- Mykhalovskiy, E. (2011). The problem of “significant risk”: exploring the public health impact of criminalizing HIV non-disclosure. Social Science & Medicine, 73(5), 668–675. doi: 10.1016/j.socscimed.2011.06.051
- Niderost, S., & Imhof, C. (2016). Aging With HIV in the Era of Antiretroviral Treatment: Living Conditions and the Quality of Life of People Aged Above 50 Living With.
- Nobre, N., Pereira, M., Roine, R. P., Sintonen, H., & Sutinen, J. (2017). Factors associated with the quality of life of people living with HIV in Finland. AIDS Care, 29(8), 1074–1078. doi: 10.1080/09540121.2017.1281879
- Oberje, E. J. M., Dima, A. L., van Hulzen, A. G. W., Prins, J. M., & de Bruin, M. (2015). Looking beyond health-related quality of life: Predictors of subjective well-being among people living with HIV in the Netherlands. AIDS and Behavior, 19(8), 1398–1407. doi: 10.1007/s10461-014-0880-2
- Pedersen, K. K., Eiersted, M. R., Gaardbo, J. C., Pedersen, M., Gerstoft, J., Troseid, M., & Nielsen, S. D. (2015). Lower self-reported quality of life in HIV-infected patients on cART and with low comorbidity compared with healthy controls. JAIDS Journal of Acquired Immune Deficiency Syndromes, 70(1), 16–22. doi: 10.1097/QAI.0000000000000697
- The Public Health Agency of Sweden (Folkhälsomyndigheten). (2016). Syfte och bakgrund till frågorna i nationella folkhälsoenkäten (Aim and background to the questions in the Swedish national public health survey). Retrieved from https://www.folkhalsomyndigheten.se/globalassets/statistik-uppfoljning/enkater-undersokningar/nationella-folkhalsoenkaten/syfte-bakgrund-fragorna-hlv.pdf
- Rao, D., Chen, W.-T., Pearson, C., Simoni, J., Fredriksen-Goldsen, K., Nelson, K., … Zhang, F. (2012). Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. International Journal of STD & AIDS, 23(7), 481–484. doi: 10.1258/ijsa.2009.009428
- Reinius, M., Wettergren, L., Wiklander, M., Svedhem, V., Ekstrom, A. M., & Eriksson, L. E. (2017). Development of a 12-item short version of the HIV stigma scale. Health and Quality of Life Outcomes, 15(1), 115. doi: 10.1186/s12955-017-0691-z
- Reinius, M., Wiklander, M., Wettergren, L., Svedhem, V., & Eriksson, L. E. (2018). The relationship between stigma and health-related quality of life in people living with HIV who have full access to antiretroviral treatment: An assessment of Earnshaw and Chaudoir’s HIV stigma framework using empirical data. AIDS and Behavior, 22(12), 3795–3806. doi: 10.1007/s10461-018-2041-5
- Rüütel, K., Pisarev, H., Loit, H.-M., & Uusküla, A. (2009). Factors influencing quality of life of people living with HIV in Estonia: A cross-sectional survey. Journal of the International AIDS Society, 12, 13–13. doi: 10.1186/1758-2652-12-13
- Rydstrom, L.-L., Wiklander, M., Naver, L., Ygge, B.-M., & Eriksson, L. E. (2016). HIV-related stigma and health-related quality of life among children living with HIV in https://doi.org/10.1080/09540121.2015.1120267
- Schönnesson, L. N. (1999). Med livet i fokus. En Studie Kring Livskvalitet Hos Homosexuella Män Och Heterosexuella Kvinnor Med Hiv. Göteborgs Universitet, Institutionen För Socialt Arbete. Skriftserien, 3.
- Schönnesson, L. N., Zeluf, G., Garcia-Huidobro, D., Ross, M. W., Eriksson, L. E., & Ekström, A. M. (2018). Sexual (dis)satisfaction and its contributors among people living with HIV infection in Sweden. Archives of Sexual Behavior, 47(7), 2007–2026. doi: 10.1007/s10508-017-1106-2
- Schouten, J., Wit, F. W., Stolte, I. G., Kootstra, N. A., van der Valk, M., Geerlings, S. E., … Mulder, W. M. C. (2014). Cross-sectional comparison of the prevalence of age-associated comorbidities and their risk factors between HIV-infected and uninfected individuals: The AGEhIV cohort study. Clinical Infectious Diseases, 59(12), 1787–1797. doi: 10.1093/cid/ciu701
- Slater, L. Z., Moneyham, L., Vance, D. E., Raper, J. L., Mugavero, M. J., & Childs, G. (2015). The multiple stigma experience and quality of life in older Gay Men With HIV. Journal of the Association of Nurses in AIDS Care, 26(1), 24–35. doi: 10.1016/j.jana.2014.06.007
- Tran, B. X., Nguyen, L. T., Do, C. D., Nguyen, Q. L., & Maher, R. M. (2014). Associations between alcohol use disorders and adherence to antiretroviral treatment and quality of life amongst people living with HIV/AIDS. BMC Public Health, 14(1), 27. doi: 10.1186/1471-2458-14-27
- Vincent, W., Fang, X., Calabrese, S. K., Heckman, T. G., Sikkema, K. J., & Hansen, N. B. (2017). HIV-related shame and health-related quality of life among older, HIV-positive adults. Journal of Behavioral Medicine, 40(3), 434–444. doi: 10.1007/s10865-016-9812-0
- von Hippel, P. T. (2007). 4. Regression with missing Ys: An improved strategy for analyzing multiply imputed data. Sociological Methodology, 37(1), 83–117. doi: 10.1111/j.1467-9531.2007.00180.x
- White, I. R., Royston, P., & Wood, A. M. (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30(4), 377–399. doi: 10.1002/sim.4067
