?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
This study aimed of validating a ten-item HIV stigma scale that was originally developed in the U.S.A. and adapting it for Japanese adults with HIV. To adapt the HIV stigma scale for Japanese adults with HIV, a forward–backward translation method was employed. We assessed its validity and reliability using questionnaire survey data collected from 463 Japanese adults with HIV between August 2017 and February 2018. Although the validity was acceptable, the internal consistency in two subcategories in the Japanese version of the HIV stigma scale was low (ω: 0.63, 0.60). Therefore, we performed exploratory factor analysis, which suggested a different model consisting of two subcategories. Then, we assessed the reliability and validity of the scale. The omega values were between 0.83 and 0.89, the absolute correlations (|r|) to other psychological scales for external validity were between 0.34 and 0.51, and the non-response rates for feasibility were between 0.9 and 1.8. The Japanese version of the HIV stigma scale therefore had sufficient reliability and validity. This questionnaire may help identify individuals that need increased care, which may improve their quality of life.
Introduction
Combination antiretroviral therapy was introduced two decades ago to suppress HIV in the blood and this suppressed state is maintained by adherence to medication (Lewden et al., Citation2007; Paterson et al., Citation2000; Rosenblum, Deeks, van der Laan, & Bangsberg, Citation2009), which has reduced the mortality (Lewden et al., Citation2007), HIV transmission rates (Cohen et al., Citation2011), and the number of patients diagnosed with HIV (Kominski, Citation2013), and increased their lifespan. Therefore, self-care, which includes patient adherence to medication, plays an important role in suppressing the HIV viral load. However, there are several obstacles to self-care for HIV-positive individuals such as negative thoughts and behaviors toward them by others. A high degree of stigma among patients with HIV is associated with lower medication adherence (Hemls et al., Citation2017; Rubens et al., Citation2018; Turan et al., Citation2016; Turan et al., Citation2017).
In addition to complying with combination antiretroviral therapy, it is important for individuals with HIV to use condoms to reduce the risk of infection of multiple STDs (Gallo et al., Citation2007; Warner, Stone, Macaluso, Buehler, & Austin, Citation2006) because HIV-positive individuals have a greater risk of contracting STDs (Cope et al., Citation2014). However, the rate of condom use is low among individuals who feel stigmatized by their HIV status (Hu et al., Citation2014; Molina & Ramirez-Valles, Citation2013). Furthermore, although a high quality of life (QOL) is important for individuals with HIV, HIV-related stigma negatively affects the QOL (Logie, Ahmed, Tharao, & Loutfy, Citation2017; Nobre, Pereira, Roine, Sutinen, & Sintonen, Citation2018; Nyamathi et al., Citation2017). Such stigmatizing attitudes in low-HIV prevalence countries is more influential than in high-HIV prevalence countries (Genberg et al., Citation2009). Japan is one of the low-HIV prevalence countries, with 0.03 per 1,000 adults who are between 15 and 49 (Joint United Nations Programme on HIV and AIDS [UNAIDS], Citation2018). However, a HIV stigma scale has not been developed for Japanese adults with HIV. A validated scale to measure stigma related to HIV is essential to clarify the impact of stigma among Japanese people with HIV.
Evaluating stigma is important to understand its association with self-care, which has led to the development of several psychological scales (Berger, Ferrans, & Lashley, Citation2001; Holzemer et al., Citation2007; Kalichman et al., Citation2009; Kang, Rapkin, Remien, Mellins, & Oh, Citation2005; Molina & Ramirez-Valles, Citation2013). The HIV stigma scale developed by Berger et al. (Citation2001) has been used in numerous studies to clarify the effects of stigma towards HIV (Carrasco et al., Citation2018; Rice et al., Citation2017; Turan et al., Citation2017; Valle et al., Citation2015), and consists of 40 items that are grouped into the following four categories: personalized stigma, disclosure concerns, negative self-image and concern with public attitude towards individuals with HIV. Construct and external validity were demonstrated by exploratory factor analysis and correlation coefficients between other measurements (self-esteem scale, depression scale, social support scale and social conflict scale), and the reliability was demonstrated by the alpha coefficient and test-retest correlations. The Berger HIV stigma scale has been translated from English to multiple other languages such as Tamil (Jeyaseelan et al., Citation2013), Spanish (Franke et al., Citation2010; Fuster-RuizdeApodaca, Molero, Holgado, & Ubillos, Citation2015), Thai (Rongkavilit et al., Citation2010), and Swedish (Lindberg, Wettergren, Wiklander, Svedhem-Johansson, & Eriksson, Citation2014). To reduce the length of the questionnaire, Wright, Naar-King, Lam, Templin, and Frey (Citation2007) developed a short version of the Berger HIV stigma scale that contains only ten items that are grouped into four categories. Although they initially developed this scale for young individuals with HIV, it was subsequently used for adults (Logie, Jenkinson, Earnshaw, Tharao, & Loutfy, Citation2016). The Wright’s HIV stigma scale is structured similarly to the Berger HIV stigma scale. However, multidimensional scales are recommended to contain at least three items for each factor to ensure validity and reliability (Raubenheimer, Citation2004; Tabachnick & Fidell, Citation2014) whereas Wright’s HIV stigma scale consists of four subcategories for ten items: personal stigma (three items), disclosure (two items), public attitude (two items) and negative self-image (three items). Therefore, this study aimed at developing a Japanese version of the HIV stigma scale and assessing its structure.
Materials and methods
To develop an appropriate HIV stigma scale for Japanese adults with HIV, we conducted this study in three phases: In phase one, a Japanese version of the HIV stigma scale for adults was developed through a forward–backward translation method, and was subsequently revised based on suggestions by experts and Japanese individuals with HIV. In the second phase, we confirmed the goodness of fit and reliability from the original model using survey data from Japanese adults with HIV. In cases where the goodness of fit or reliability was not satisfactory, we improved the models by exploratory factor analysis. In the last phase, we evaluated the feasibility and external validity of the new models. Moreover, we also demonstrated internal consistency for these improved models.
HIV stigma scale questionnaire
We adopted Wright’s HIV stigma scale to measure the perceived stigma of HIV felt by HIV-infected individuals because of its confirmed reliability and criterion-related validity even though it was simple (Logie et al., Citation2016; Wright et al., Citation2007). The questionnaire included ten items grouped in the following four subcategories: personalized stigma, disclosure, negative self-image and public attitudes. These categories are the same as those in the Berger HIV stigma scale. Participants registered their level of agreement with each item on a scale from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s alpha values among adults with HIV for personalized stigma, disclosure, negative self-image and public attitudes were 0.86, 0.76, 0.87 and 0.76, respectively (Logie et al., Citation2016), which suggested good reliability.
Preliminary study
A forward–backward translation method was used to produce an accurate Japanese version of Wright’s HIV stigma scale. First, we translated Wright’s HIV stigma scale from English to Japanese as a forward translation. A professional English translator then back-translated the tentative Japanese version into English. Next, a bilingual Japanese HIV researcher who had worked in the U.S.A. for more than 20 years compared the original questionnaire with the back-translated version. If any connotative differences were found between the back-translated version and the original English questionnaire, they were corrected in the tentative Japanese version. The tentative Japanese version was also subjected to a backward translation method, and a Japanese bilingual researcher compared it with the original version. This process was repeated until the bilingual Japanese researcher was satisfied that there were no discrepancies between the original and back-translated versions of the questionnaire.
To adapt the scale for Japanese adults with HIV, a specialized committee comprising multidisciplinary specialists, such as nurses, psychological counselors and social workers, reviewed the Japanese version and discussed it with the authors. All members of this committee were Japanese and had at least two years of experience in HIV patient care. In the meeting, they examined the context and diction of the questionnaire, and found the items to have satisfactory Japanese descriptions. However, the committee members noted three items that may not reflect circumstances surrounding Japanese individuals with HIV. In Japan, approximately 40% of individuals with HIV do not reveal their HIV status to their parents or friends (Wakabayashi, Citation2015), which may result in several missing values on the HIV stigma scale. A shortened Swedish version of the Berger HIV stigma scale was also missing questions regarding experiences of discrimination (Wiklander et al., Citation2013). Therefore, the three items were modified from the present perfect to present tense as follows: “I have lost friends by telling them I have HIV” to “I lose friends by telling them I have HIV”, “I have been hurt by how people reacted to learning I have HIV” to “I am hurt by how people react to learning I have HIV”, and “I have stopped socializing with some people because of their reactions to my having HIV” to “I stop socializing with some people because of their reactions to my having HIV”. Word modification is often conducted when measurement tools are adapted to other languages to match their culture (Fuster-RuizdeApodaca et al., Citation2015; Pourmarzi, Khoramirad, Ahmari, & Abedini, Citation2015). Moreover, the Berger HIV stigma scale encourages respondents to guess and answer even if they have no experiences regarding the questions. The clarification in the original Berger HIV stigma scale states the following:
Many of the items in this next section assume that you have told other people that you have HIV or that others know. This may not be true for you. If the item refers to something that has not actually happened to you, please imagine yourself in that situation. Then, give your answer based on how you think you would feel or how you think others would react to you.
The Berger HIV stigma scale thus allows participants to incorporate and project their opinions even if they have not directly experienced discrimination. The modification from present perfect to present tense can be reasonably justified considering this clarification.
Furthermore, a pilot study was conducted including five HIV-infected individuals (four men and one woman: average age = 41.4 years old: all had a good immune status) to assess whether there were any discomforting items or difficulty in understanding the terms used in the questionnaire. The eligible participants in the pilot study were Japanese, aged above 20 years, infected with HIV and had no cognitive disabilities. Convenience sampling was used in the pilot study. After the eligible patients agreed to participate, the first author asked the first participant to describe what he/she thought when filling out the questionnaire, and then recorded his/her responses. After the pilot test, some expressions were revised based on the responses and the next pilot test was performed with the second participant. This process was repeated up to the fifth participant, and no corrective responses were received from the last patient involved in the pilot study.
Additional scales to validate the HIV stigma scale
To assess the external validity criteria of the newly developed Japanese version of the HIV stigma scale (HSSj), participants were asked to complete the Japanese version of the Patient Health Questionnaire-9 (PHQ-9J: Inagaki et al., Citation2013) and self-esteem scale (Mimura & Griffiths, Citation2007), in addition to the HSSj. Both the PHQ-9J and self-esteem scale have been reported to have sufficient reliability and validity (Inagaki et al., Citation2013; Mimura & Griffiths, Citation2007; Uchida & Ueno, Citation2010), and are the most commonly used to diagnose and measure the severity of depression and evaluate self-esteem.
PHQ-9J comprises nine items and is a Japanese version of the PHQ-9, which was developed by Kroenke, Spitzer, and Williams (Citation2001) to diagnose depression and other mental disorders. Participants were asked the frequency of problems that had bothered them in the past two weeks. The responses were recorded on a scale from 0 (not at all) to 3 (almost every day). The PHQ-9j scores range between 0 and 27, with higher scores indicating a higher severity of depression. The self-esteem scale used is a Japanese version of the Rosenberg self-esteem scale (Rosenberg, Citation1965). Responses are assessed using a ten-item self-esteem scale ranging between 1 (strongly disagree) and 4 (strongly agree), with five reversed items. The self-esteem scale scores range between 10 and 40, with higher scores indicating higher self-esteem.
Study sample and methods of analysis
A cross-sectional questionnaire survey was conducted at nine hospitals in Japan between August 2017 and February 2018. The medical staff distributed the questionnaire to eligible participants who were Japanese, aged above 20 years and infected with HIV. Informed consent was received from the patients prior to participation. Completed questionnaires were returned by mail to the researchers.
Cross-sectional data obtained from the survey were analyzed using lavaan, SemTools, and psych for confirmatory factor analysis, omega values, exploratory factor analysis, and Spearman’s correlation coefficients within R software version 3.5.1, respectively. These non-parametric analysis methods were used because the total score of HSSj was not normally distributed.
As each factor in a multidimensional scale should contain at least three items to ensure validity and reliability, we first confirmed if the scale structure matched Japanese adults with HIV by confirmatory factor analysis and calculating omega values. We confirmed the goodness of fit by x2, comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR). The model was considered to have good construct validity if x2 p-values were greater than 0.05, CFI and TLI values were equal to or greater than 0.95, RMSEA values were less than 0.08 and SRMR values were less than 0.05 (Schermelleh-Engel, Moosbrugger, & Müller, Citation2003; Tabachnick & Fidell, Citation2014). Omega values greater than 0.7 were considered to reflect good internal consistency for reliability (Nunnally, Citation1978). Based on these criteria, we considered whether the scale was appropriate for Japanese adults with HIV. For cases that were inappropriate, we created a new satisfactory scale by exploratory factor analysis using polychoric correlation coefficients from the survey data. A factor number was determined by the results of a scree plot and a parallel analysis. After determining the factor number, factor loadings were obtained with promax rotations.
Next, we assessed the feasibility and external validity of the scale. The feasibility was evaluated by the number of missing values. If more than 5% of participants did not answer an item, it was considered unacceptable because missing values may indicate difficulties in answering the question (i.e., The context of the question was ambiguous). To demonstrate external validity, Spearman’s coefficients were calculated using the scores of the HSSj, and those of PHQ-9 and the self-esteem scale based on previous studies that demonstrated that HIV stigma was positively associated with depression (Berger et al., Citation2001; Brittain et al., Citation2017; Tanney, Naar-King, & MacDonnel, Citation2012; Wright et al., Citation2007) and negatively associated with self-esteem (Berger et al., Citation2001; Molina & Ramirez-Valles, Citation2013; Varni, Miller, McCuin, & Solomon, Citation2012). If the coefficients had values less than 0.3 and were not significantly associated, external validity was considered unacceptable.
Ethical considerations
This study was approved by the Ethical Committee for Epidemiology of Hiroshima University (No. E-860).
Results
Participants
Of the 819 questionnaires that were distributed, 451 were returned. The response rate was 55.1%. The mean age of the participants was 47.7 years (standard deviation = 10.7) and 90.9% were men, 73.8% of whom were men who have sex with men (MSM) ().
Table 1. Participant characteristics.
Confirming the structure of the HIV stigma scale
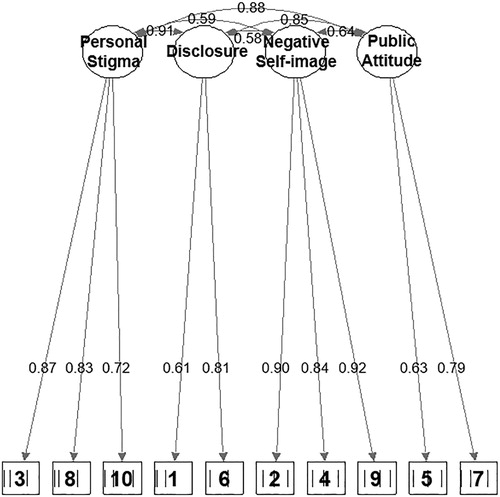
A confirmatory factor analysis was performed (estimator, diagonally weighted least squares) to obtain a goodness of fit to identify whether the HSSj matched the original model (). From the confirmatory factor analysis, the p-value was less than 0.05 by the chi-squared test, CFI and TLI values were greater than 0.95, the RMSEA value was less than 0.08 and the SRMS value was less than 0.05. Moreover, omega values were calculated to assess internal reliability. The omega value in the HSSj was 0.90 for the total items and greater than 0.7 for two subcategories, but those for the other two subcategories were less than 0.7.
The association among the four subcategories ranged between 0.58 and 0.91, and the standardized estimate of each item ranged between 0.61 and 0.92 ().
The goodness of fit was sufficient, but the reliability of two subcategories was insufficient. Therefore, we conducted exploratory factor analysis to create a better model ().
Table 2. Model fitness and reliability of the HSSj.
Creation of a new HSSj model
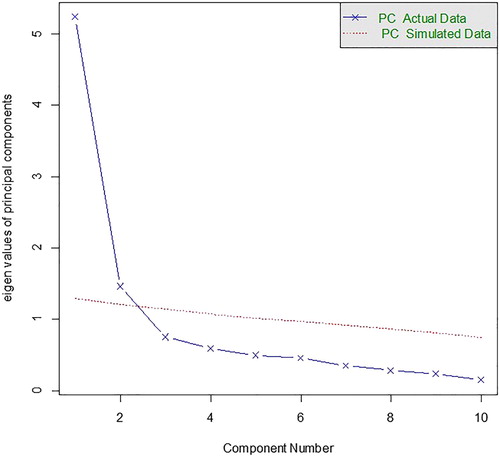
To create an HSSj of sufficient quality, parallel analysis (maximum likelihood) was conducted using a polychoric correlation matrix, which suggested that the HSSj had two more eigen values in the actual data than in the simulated data ().
Next, we performed exploratory factor analysis to clarify the HSSj factor structure. Factor analysis (promax rotation) revealed that the first factor was composed of seven items, the second factor was composed of three items, and the correlation coefficient between the two factors was 0.605 (). However, as the factor loading in item 5 was lower than 0.4, it was excluded from the HSSj. We considered the name of the subcategories after reading the items, and the first and second factors were named “concerned with public stigma” and “negative self-image”, respectively.
Table 3. Factor loadings of the HSSj from factor analysis and non-response number for each item.
Missing values in the HSSj
We calculated the percentage of missing values for each item in the HSSj. The highest rate of missing values was 1.8% for the item “most people with HIV are rejected when others find out”. The minimum missing rate was 0.9%, which was observed for four items; item 1, item 2, item 4 and item 6 ().
External validity assessment using other psychological scales
Data were analyzed using Spearman’s correlation coefficient, which was used to assess the external validity of the HSSj and its subcategories with respect to the PHQ-9J and self-esteem scale (). The total scores for the HSSj and the subcategories of “concern with public stigma” and “negative self-image” were significantly positively correlated with those of the PHQ-9J (r = 0.45, 0.43 and 0.37, respectively). The total scores for the HSSj and the subcategories were significantly negatively correlated with those of the self-esteem scale (r = −0.48, −0.51 and −0.34, respectively).
Table 4. Spearman’s correlation coefficients of the HSSj with respect to the two psychological questionnaires.
Internal consistency of the HSSj in two subcategories with nine items
To clarify the internal consistency of the HSSj in two subcategories, we calculated omega values. The omega values in the total HSSj, and the subcategories of “concern with public stigma” and “negative self-image” were 0.89, 0.83 and 0.87, respectively.
Discussion
We developed the HSSj by adapting Wright’s HIV stigma scale for Japanese adults with HIV. Using survey data in Japan, we evaluated the construct validity and reliability of the HSSj, which indicated insufficient reliability. Therefore, the structure was improved by exploratory factor analysis. The new improved model of the HSSj consisted of two subcategories and nine items, and had good reliability and validity by external validation with Spearman’s coefficients, good feasibility by non-response rates and good internal consistency by omega values using the survey data.
The representativeness of the sample was confirmed by comparing with survey data. The demographic composition of participants in the survey was similar to that of the Japanese population with HIV. According to the HIV/AIDS surveillance in Japan (AIDS Surveillance Committee, Citation2018), there are more Japanese men (94.3%) than women (5.7%) with the disease. Furthermore, MSM was the highest risk (60.0%), followed by heterosexuals (26.0%). The proportions of intravenous drug users and vertical transmitted groups were low at 0.3% and 0.2%, respectively. Data from the HIV/AIDS surveillance were collected from clinics, hospitals and public health centers, and reports from these institutes were collected via face-to-face medical interviews. In Japan, MSM had more difficulty in divulging their sexuality to the medical staff than heterosexuals because of the public stigma attached to this sexual group minority. MSM with HIV may be more comfortable acknowledging their sexuality in an anonymous questionnaire than declaring it in a face-to-face interview, which was demonstrated by an anonymous online questionnaire (Inoue, Takaku, Yajima, & Ikushima, Citation2015). This study found that 23% of Japanese MSM with HIV provided untrue responses during face-to-face interviews for HIV/AIDS surveillance at HIV test sites. Therefore, a higher percentage of MSM and a lower percentage of heterosexuals were identified than those found by the HIV/AIDS surveillance in Japan. In addition, as the HSSj was developed for adults, children infected with HIV by their mothers were not included. As indicated above, the representativeness of the sample in this study was sufficient to assess the reliability and validity of the HSSj.
Using the data, we used confirmatory factor analysis to confirm the quality of the questionnaire. The goodness of fit was assessed by x2, CFI, TLI, RMSEA and SRMR. The x2 p-value for the goodness of fit was less than 0.05 because the x2 p-value is often less than 0.05 when the sample size is large even when the model is good. Therefore, the goodness of fit of this model was considered to be sufficient. Although the goodness of fit was sufficient, internal consistency in two subcategories, “disclosure” and “public attitude”, was insufficient. The low internal consistency of the original model may be related to cultural differences. As HIV-related stigma is influenced by social environments, the outcome of certain items may differ across different social environments (Franke et al., Citation2010; Jeyaseelan et al., Citation2013; Lindberg et al., Citation2014; Reinius et al., Citation2017; Rongkavilit et al., Citation2010; Valle et al., Citation2015). For example, the item “I am very careful who I tell that I have HIV” is in the subcategory of disclosure in Wright’s HIV stigma scale. In contrast, in the Tamil version of the Berger HIV stigma scale (Jeyaseelan et al., Citation2013), the same item was in “public attitude” and “disclosure”, with high factor loadings. This difference between the two scales suggested that the same items belong to different subcategories, which likely reflects the culture where the survey was conducted. Furthermore, certain items may consist of other subcategories to varying degrees, which also depends on where the survey was conducted.
This phenomenon also affected the result of the parallel analysis. Parallel analysis revealed that the HSSj had two factors that may have been caused by modifications to three items in the subscale of “personal stigma”, which became similar to other subcategories, “public attitude” and “disclosure”. Correlations among the three subcategories were high (0.85–0.90) in the confirmatory factor analysis, and these three categories were grouped into one category. Moreover, factor analysis revealed that item five, “most people think that a person with HIV is disgusting”, had low factor loading in “concerned with public stigma” (0.325), and it was removed from the HSSj. These data suggest that responses to a certain item by individuals from different cultures differ.
Results from Spearman’s correlation coefficient analysis demonstrated that the HSSj had reasonably satisfactory correlations with other psychological measurement tools. Associations between HIV stigma and depression have previously been identified (Brittain et al., Citation2017; Rao et al., Citation2012). Moreover, in our analysis, the PHQ-9J score, which reflects the severity of depression, was positively correlated with the total scores of the HSSj and each of its two subcategories, as well as with Wright’s HIV stigma scale. Based on the association between Wright’s HIV stigma scale and the score of the brief symptom inventory for depression (Wright et al., Citation2007), the correlation coefficients of the total score and subcategories ranged between 0.351 and 0.414. Spearman’s correlation coefficients were consistent with the results by Wright et al. The self-esteem scale was negatively correlated with the total HSSj score, and scores of each of the subcategories were similar to those by the Berger HIV stigma scale. We therefore found that the HSSj had sufficient external validity. Futhermore, the reliability of the HSSj in two subcategories was improved by exploratory factor analysis in the second phase because the omega values were greater than 0.80 after grouping several categories.
Based on the rate of missing values, the HSSj was demonstrated to be feasible. The rate of missing values was less than 5% for each item, suggesting that participants had little difficulty in answering all of the questions in the HSSj. Furthermore, modification of expressions for three items may have reduced the amount of missing values because those who had not disclosed their HIV status may fear discrimination and not naturally respond to the original questions. Without such modifications, possible bias cannot be excluded.
Limitations and future proposals
Although the HSSj consisted of two categories that had good reliability and validity, there were several limitations. As the total score of the HSSj was not normally distributed, it must be treated as an ordinal variable. Moreover, to ensure reliability, a test-retest method should be employed to assess the temporal stability (DeVellis, Citation2012) of the HSSj.
In future studies, the impact of stigma among Japanese adults with HIV can be measured using the HSSj. Studies using the HSSj will clarify whether stigma influences health-related problems, such as QOL, self-care and depression, among Japanese adults with HIV.
Conclusions
As HIV is a chronic disease, factors related to low self-care and the effects of HIV stigma on poor self-care among individuals with HIV are important. Using the HSSj, scores from the two subcategories may help identify the type of care that these individuals need and may subsequently improve self-care. In addition, simplified psychological scales are becoming more common because of their ease of use. Based on its validity and reliability, the HSSj is a useful tool for measuring stigma among Japanese adults with HIV.
Supplemental Material
Download Zip (379.8 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- AIDS Surveillance Committee. (2018). 2017 Annual report. Retrieved from http://api-net.jfap.or.jp/status/2017/17nenpo/17nenpo_menu.html
- Berger, B. E., Ferrans, C. E., & Lashley, F. R. (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24(6), 518–529.
- Brittain, K., Mellins, C. A., Phillips, T., Zerbe, A., Abrams, E. J., Myer, L., & Remien, R. H. (2017). Social support, stigma and antenatal depression among HIV-infected pregnant women in South Africa. AIDS and Behavior, 21(1), 274–282.
- Carrasco, M. A., Nguyen, T. Q., Barrington, C., Perez, M., Donastorg, Y., & Kerrigan, D. (2018). HIV stigma mediates the association between social cohesion and consistent condom use among female sex workers living with HIV in the Dominican Republic. Archives of Sexual Behavior, 47(5), 1529–1539.
- Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., … Fleming, T. R. (2011). Prevention of HIV-1 infection with early antiretroviral therapy. The New England Journal of Medicine, 365(6), 493–505.
- Cope, A. B., Crooks, A. M., Chin, T., Kuruc, J. D., McGee, K. S., Eron, J. J., … Gay, C. L. (2014). Incident sexually transmitted infection as a biomarker for high-risk sexual behavior after diagnosis of acute HIV. Journal of Sexually Transmitted Diseases, 41(7), 447–452.
- DeVellis, R. F. (2012). Scale development and applications (3rd ed.). Thousand Oaks, CA: Sage.
- Franke, M. F., Munoz, M., Finnegan, K., Zeladita, J., Sebastian, J. L., Bayona, J. N., & Shin, S. S. (2010). Validation and abbreviation of an HIV stigma scale in an adult spanish-speaking population in urban Peru. AIDS and Behavior, 14(1), 189–199.
- Fuster-RuizdeApodaca, M. J., Molero, F., Holgado, F. P., & Ubillos, S. (2015). Adaptation of the HIV stigma scale in Spaniards with HIV. The Spanish Journal of Psychology, 18(E66), 1–15.
- Gallo, M. F., Steiner, M. J., Warner, L., Hylton-Kong, T., Figueroa, J. P., Hobbs, M. M., & Behets, F. M. (2007). Self-reported condom use is associated with reduced risk of chlamydia, gonorrhea, and trichomoniasis. Journal of Sexually Transmitted Diseases, 34(10), 829–833.
- Genberg, B. L., Hlavka, Z., Konda, K. A., Maman, S., Chariyalertsak, S., Chingono, A., … Celentano, D. D. (2009). A comparison of HIV/AIDS-related stigma in four countries: Negative attitudes and perceived acts of discrimination towards people living with HIV/AIDS. Social Science & Medicine, 68(12), 2279–2287.
- Hemls, C. B., Turan, J. M., Atkins, G., Kempf, M. C., Clay, O. J., Raper, J. L., … Turan, B. (2017). Interpersonal mechanisms contributing to the association between HIV-related internalized stigma and medication adherence. AIDS and Behavior, 21(1), 238–247.
- Holzemer, W. L., Uys, L. R., Chirwa, M. L., Greeff, M., Makoae, L. N., Kohi, T. W., … Durrheim, K. (2007). Validation of the HIV/AIDS stigma instrument - PLWA (HASI-P). AIDS Care, 19(8), 1002–1012.
- Hu, Y., Lu, H., Raymond, H. F., Sun, Y., Sun, J., Jia, Y., … Ruan, Y. (2014). Measures of condom and safer sex social norms and stigma towards HIV/AIDS among Beijing MSM. AIDS and Behavior, 18(6), 1068–1074.
- Inagaki, M., Ohtsuki, T., Yonemoto, N., Kawashima, Y., Saitoh, A., Oikawa, Y., … Yamada, M. (2013). Validity of the patient health questionnaire (PHQ)-9 and PHQ-2 in general internal medicine primary care at a Japanese rural hospital: A cross-sectional study. General Hospital Psychiatry, 35(6), 592–597.
- Inoue, Y., Takaku, Y., Yajima, T., & Ikushima, Y. (2015). A survey comparing the route of HIV transmission reported by patients to their physicians and the self-reported “actual route”. [nihon Koshu Eisei Zasshi] Japanese Journal of Public Health, 62(3), 106–116.
- Jeyaseelan, L., Kumar, S., Mohanraj, R., Rebekah, G., Rao, D., & Manhart, L. E. (2013). Assessing HIV/AIDS stigma in south India: Validation and abridgement of the Berger HIV stigma scale. AIDS and Behavior, 17(1), 434–443.
- Joint United Nations Programme on HIV and AIDS: UNAIDS. (2018). Country fact sheets, Japan 2017. Retrieved from http://www.unaids.org/en/regionscountries/countries/japan
- Kalichman, S. C., Simbayi, L. C., Cloete, A., Mthembu, P. P., Mkhonta, R. N., & Ginindza, T. (2009). Measuring AIDS stigmas in people living with HIV/AIDS: The internalized AIDS-related stigma scale. AIDS Care, 21(1), 87–93.
- Kang, E., Rapkin, B. D., Remien, R. H., Mellins, C. A., & Oh, A. (2005). Multiple dimensions of HIV stigma and psychological distress among Asians and Pacific Islanders living with HIV illness. AIDS and Behavior, 9(2), 145–154.
- Kominski, G. F. (2013). Changing the US health care system: Key issues in health services policy and management (4th ed.). San Francisco, CA: Jossey-Bass.
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613.
- Lewden, C., Chene, G., Morlat, P., Raffi, F., Dupon, M., Dellamonica, P., … Leport, C. (2007). HIV-infected adults with a CD4 cell count greater than 500 cells/mm3 on long-term combination antiretroviral therapy reach same mortality rates as the general population. Journal of Acquired Immune Deficiency Syndromes, 46(1), 72–77.
- Lindberg, M. H., Wettergren, L., Wiklander, M., Svedhem-Johansson, V., & Eriksson, L. E. (2014). Psychometric evaluation of the HIV stigma scale in a Swedish context. PLoS One, 9(12), e114867.
- Logie, C. H., Ahmed, U., Tharao, W., & Loutfy, M. R. (2017). A structural equation model of factors contributing to quality of life among African and Caribbean women living with HIV in Ontario, Canada. AIDS Research and Human Retroviruses, 33(3), 290–297.
- Logie, C. H., Jenkinson, J. I., Earnshaw, V., Tharao, W., & Loutfy, M. R. (2016). A structural equation model of HIV-related stigma, racial discrimination, housing insecurity and wellbeing among African and Caribbean black women living with HIV in Ontario, Canada. PLoS One, 11(9), e0162826.
- Mimura, C., & Griffiths, P. (2007). A Japanese version of the Rosenberg self-esteem scale: Translation and equivalence assessment. Journal of Psychosomatic Research, 62(5), 589–594.
- Molina, Y., & Ramirez-Valles, J. (2013). HIV/AIDS stigma: Measurement and relationships to psycho-behavioral factors in Latino gay/bisexual men and transgender women. AIDS Care, 25(12), 1559–1568.
- Nobre, N., Pereira, M., Roine, R. P., Sutinen, J., & Sintonen, H. (2018). HIV-related self-stigma and health-related quality of life of people living with HIV in Finland. The Journal of the Association of Nurses in AIDS Care: JANAC, 29(2), 254–265.
- Nunnally, J. C. (1978). Psychometric theory (2nd ed.). New York, NY: McGraw-Hill.
- Nyamathi, A. M., Ekstrand, M., Yadav, K., Ramakrishna, P., Heylen, E., Carpenter, C., … Sinha, S. (2017). Quality of life among women living with HIV in Rural India. The Journal of the Association of Nurses in AIDS Care: JANAC, 28(4), 575–586.
- Paterson, D. L., Swindells, S., Mohr, J., Brester, M., Vergis, E. N., Squier, C., … Singh, N. (2000). Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine, 133(1), 21–30.
- Pourmarzi, D., Khoramirad, A., Ahmari, T. H., & Abedini, Z. (2015). Validity and reliability of Persian version of HIV/AIDS related stigma scale for people living With HIV/AIDS in Iran. Journal of Family Reproductive Health, 9(4), 164–171.
- Rao, D., Feldman, B. J., Fredericksen, R. J., Crane, P. K., Simoni, J. M., Kitahata, M. M., & Crane, H. M. (2012). A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS and Behavior, 16(3), 711–716.
- Raubenheimer, J. (2004). An item selection procedure to maximize scale reliability and validity. South African Journal of Industrial Psychology, 30(4), 59.
- Reinius, M., Wettergren, L., Wiklander, M., Svedhem, V., Ekstrom, A. M., & Eriksson, L. E. (2017). Development of a 12-item short version of the HIV stigma scale. Health and Quality of Life Outcomes, 15(1), 115.
- Rice, W. S., Crockett, K. B., Mugavero, M. J., Raper, J. L., Atkins, G. C., & Turan, B. (2017). Association between internalized HIV-related stigma and HIV care visit adherence. JAIDS Journal of Acquired Immune Deficiency Syndromes, 76(5), 482–487.
- Rongkavilit, C., Wright, K., Chen, X., Naar-King, S., Chuenyam, T., & Phanuphak, P. (2010). HIV stigma, disclosure and psychosocial distress among Thai youth living with HIV. International Journal of STD & AIDS, 21(2), 126–132.
- Rosenberg, M. (1965). Society and the adolescent self-image. Princeton, N.J: Princeton University Press.
- Rosenblum, M., Deeks, S. G., van der Laan, M., & Bangsberg, D. R. (2009). The risk of virologic failure decreases with duration of HIV suppression, at greater than 50% adherence to antiretroviral therapy. PLoS One, 4(9), e7196.
- Rubens, M., Saxena, A., Ramamoorthy, V., McCoy, H. V., Beck-Sague, C., Jean-Gilles, M., … Devieux, J. G. (2018). HIV-related stigma, quality of care, and coping skills: Exploring factors affecting treatment adherence among PLWH in Haiti. The Journal of the Association of Nurses in AIDS Care: JANAC, 29(4), 570–579.
- Schermelleh-Engel, K., Moosbrugger, H., & Müller, H. (2003). Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods of Psychological Research Online, 8, 22–74.
- Tabachnick, B. G., & Fidell, F. S. (2014). Using multivariate statistics (6th ed.). New York, NY: Pearson Education Limited.
- Tanney, M. R., Naar-King, S., & MacDonnel, K. (2012). Depression and stigma in high-risk youth living with HIV: A multi-site study. Journal of Pediatric Health Care, 26(4), 300–305.
- Turan, B., Budhwani, H., Fazeli, P. L., Browning, W. R., Raper, J. L., Mugavero, M. J., & Turan, J. M. (2017). How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial Outcomes. AIDS and Behavior, 21(1), 283–291.
- Turan, B., Smith, W., Cohen, M. H., Wilson, T. E., Adimora, A. A., Merenstein, D., … Turan, J. M. (2016). Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: The mediating roles of social isolation and depression. Journal of Acquired Immune Deficiency Syndromes, 72(2), 198–205.
- Uchida, T., & Ueno, T. (2010). Rosenberg Jisonkanjyou shakudo no sinraisei oyobi datousei no kentou [reliability and validity of the Rosenberg self esteem scale; using the Japanese version of the RESES by Mimura & Griffiths]. Annual Report Graduate School of Education, 58, 257–266.
- Valle, A., Trevino, A. C., Zambrano, F. F., Urriola, K. E., Sanchez, L. A., & Elizondo, J. E. (2015). Perceived HIV-associated stigma among HIV-seropositive men: Psychometric study of HIV stigma scale. Frontiers in Public Health, 3, 171.
- Varni, S. E., Miller, C. T., McCuin, T., & Solomon, S. E. (2012). Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. Journal of Social and Clinical Psychology, 31(2), 123–150.
- Wakabayashi, C. (2015). HIV Youseisha no seikatu to shakaisanka ni kansuru kenkyu [ Research on life and social participation of HIV-positive patients (1st ed. Final report)]. Tokyo: Nonprofit Organization Place TOKYO/ Keio University.
- Warner, L., Stone, K. M., Macaluso, M., Buehler, J. W., & Austin, H. D. (2006). Condom use and risk of gonorrhea and Chlamydia: A systematic review of design and measurement factors assessed in epidemiologic studies. Sexually Transmitted Diseases, 33(1), 36–51.
- Wiklander, M., Rydstrom, L. L., Ygge, B. M., Naver, L., Wettergren, L., & Eriksson, L. E. (2013). Psychometric properties of a short version of the HIV stigma scale, adapted for children with HIV infection. Health and Quality of Life Outcomes, 11, 195.
- Wright, K., Naar-King, S., Lam, P., Templin, T., & Frey, M. (2007). Stigma scale revised: Reliability and validity of a brief measure of stigma for HIV+ youth. The Journal of Adolescent Health, 40(1), 96–98.