ABSTRACT
This cross sectional study was conducted in 2018 in Côte d’Ivoire to assess PrEP acceptability among men who have sex with men (MSM). Two hundred and one men were asked on their intention to use PrEP if made available. Logistic regression accounting for the sampling design was used to analyze associations between high PrEP acceptability and different independent variables including barriers and facilitators. Participants were mostly young (mean age = 25 years), educated (82% with secondary/postsecondary education) and single (95.5%). On average, 3.4 episodes of anal sex were reported monthly and 37.8% of men did not use a condom at last sex. Most MSM (72.6%) had heard of PrEP before enrollment. Overall, 35.3% reported that they would use PrEP very probably if made available. In multivariate analysis, factors associated with high PrEP acceptability were condom use at last sexual intercourse (Odds ratio (OR) = 2.51; 95%Confidence interval (95%CI) = 1.45–4.33); insertive sex as compared to versatile sex (OR = 2.56; 95%CI = 1.14–5.67); free PrEP delivery (OR = 2.45; 95%CI = 1.07–5.59), concerns about side effects (OR = 0.66; 95%CI = 0.48–0.90), and being preoccupied by the fact that post-PrEP antiretroviral therapy could be inefficient (OR = 0.25; 95%CI = 0.14–0.44). PrEP implementation among MSM in Côte d’Ivoire should be accompanied by awareness raising campaigns explaining its utility.
Introduction
In West Africa, Côte d’Ivoire bears the second heaviest burden of the human immunodeficiency virus (HIV) epidemic (UNAIDS, Citation2019). In 2018, the number (uncertainty bounds) of new HIV infections among the general adult population was estimated at 14,200 (7700–27,000) (UNAIDS, Citation2019). HIV serodiscordant heterosexual couples and other key populations at higher risk such as men who have sex with other men (MSM) contribute disproportionally to these new HIV infections. HIV prevalence is estimated at 2.6% among the general adult population and at 12.3% among MSM (UNAIDS, Citation2019). Different interventions, including early access to antiretroviral therapy (ART), are being implemented countrywide to curtail HIV transmission. However, due to stigma and other contextual barriers, MSM have limited access to HIV prevention and care services (Diabaté et al., Citation2015). As such, targeting them with prevention tools like pre-exposure prophylaxis (PrEP) that are under their full control could enrich the global response to HIV transmission. Subject to good adherence, the combination of Tenofovir disoproxil fumarate and emtricitabin reduces HIV transmission among MSM by 44–86% (Grant et al., Citation2010; McCormack et al., Citation2016; Molina et al., Citation2015; Owens et al., Citation2019). Despite these positive results, PrEP acceptability among HIV-negative MSM may not be optimal in the real world because of individual and contextual barriers like the fear of side effects and concerns about adherence (Mugo et al., Citation2016; Rocha et al., Citation2014; Yang et al., Citation2013). The objective of this study conducted in Bouaké, Côte d’Ivoire, was to estimate PrEP acceptability and to identify key facilitators and barriers that could be addressed prior to its implementation among MSM in order to enhance uptake and adherence.
Methods
The MSM targeted by this study were men living in Bouaké, aged ≥18 years, who declared being HIV-negative or of unknown HIV serostatus, and who reported at least one episode of anal sex with other men during the last 12 months. A respondent driven sampling method was used for recruitment in June and July 2018. The recruitment process began with the selection of five MSM. These «seeds» were recruited to achieve a diversified sample regarding age, sexual orientation (active, passive or versatile) and education. They underwent face-to-face interviews using a standardized and validated questionnaire. Subsequently to the interview, each seed received five vouchers to be distributed to five other MSM that he knew. This process was renewed until reaching the minimum sample size estimated at 196 participants: sample size = z2 α/2x p (1−p)/i2; 2-tailed alpha level of 0.05; precision (i) of 0.05, and prevalence of acceptability at 0.5.
The questionnaire was enriched by the results of a qualitative analysis of acceptability that preceded this quantitative study (Pelletier et al., Citation2019). Two peer-educators trained on the study procedures and questionnaires led the interviews. They also publicized the study within the MSM community of Bouaké. The quantitative questionnaires were administered at the medical center administered by “Renaissance Santé Bouaké”, the main non-governmental organization offering community-based and medical services to MSM in Bouaké. To capture PrEP acceptability, participants were asked the extent to which they intended to use it if made available. A five-point Likert scale was used for answers: 1-definitely not, 2-probably not, 3-neutral, 4-probably, and 5-very probably. Answers were mainly distributed between level 5 (35.3%) and level 4 (63.7%). Hence, the dependent variable was dichotomized: level 5 (high PrEP acceptability) versus levels 1–4 (no high PrEP acceptability). The set of independent variables scrutinized was based on results of the qualitative component of this study and on a literature review on general concerns about PrEP uptake in sub-Saharan Africa (Ahouada et al., Citation2019; Molina et al., Citation2015; Mugo et al., Citation2016; Pelletier et al., Citation2019; Rocha et al., Citation2014; Yang et al., Citation2013). It included, but was not limited to, sociodemographic characteristics (age, education and occupation), the social network (number of MSM known in Bouaké and elsewhere in the country), risk taking and risk compensation behavior (condom use, number of partners and alcohol consumption), sexual role (being active, passive or versatile), PrEP knowledge, facilitators, and barriers.
Facilitators explored were related to: free access to HIV testing, PrEP, health care, and sexual surveillance; individual and social support regarding PrEP uptake; counseling and education on sexuality and adherence to PrEP; availability of PrEP at anytime, without constraints, and within the MSM communities; PrEP uptake for protection purpose and in case of risky behavior (multiple relationships and sex with HIV-positive men).
Barriers included worries about cost and complex procedures to get PrEP; increased stigma in health care centers; non receptive attitudes from the MSM community and the family; being suspiciously considered as HIV-positive; post-PrEP antiretroviral efficacy; side effects and long term health threatening events; size and taste of the pills; risk taking (unsafe sex, multiple partnerships and unfaithfulness); uncertainty about adherence; and PrEP relative efficacy.
The statistical analyses began with the description of participants’ profiles through means and medians for continuous variables, and proportions for categorical ones. Statistical associations were examined using univariate logistic regression models. Variables with a p-value < 0.20 in these analyses were then entered in multivariate logistic regression models where they were kept if their p-value was <0.05. A step-by-step manual procedure was used for this purpose. Potential confounding variables were those considered for the selection of the «seeds» i.e., age, sexual orientation and education. Even though age and education were not independently associated to PrEP acceptability, age was kept in model 2 because, contrary to education, it was responsible of a change >10% in the estimates of a couple of independent predictors of high PrEP acceptability (Rothman et al., Citation2008, pp. 261–262). Surveylogistic procedures using SAS 9.4 (SAS Institute Inc, Cary, NC, USA) were carried out to study the associations between PrEP acceptability and the set of independent variables. They took into account the sampling design and each participant’s network. Seeds were analyzed as clusters while probability weights based on the network sizes truncated at their 5th and 95th percentile were calculated using RDS Analyst statistical software, version 0.65 (Handcock et al., Citation2016; Volz & Heckathorn, Citation2008).
The national ethics committee of Côte d’Ivoire and the research ethics committee of the CHU de Québec-Université Laval (Canada) approved the study protocol. A written informed consent was obtained from participants before the interview. Each participant was given an amount of 2000 FCA (approximately 4 $US) to compensate for the travel cost and the time needed to complete the study procedures.
Results
General profile of the participants
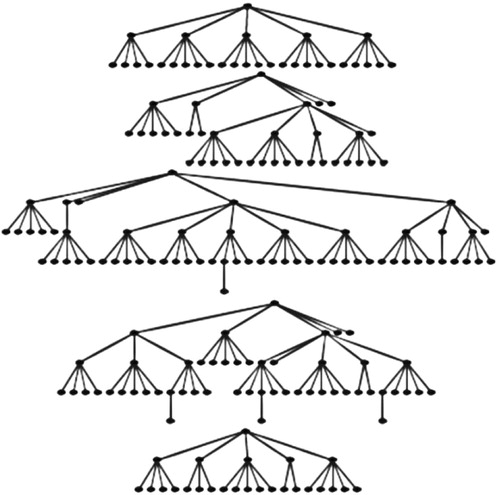
The majority of the 201 MSM were recruited during the third and the fourth waves ().
Figure 1. Selection trees for 201 men who have sex with men participating to a quantitative study of pre-exposure prophylaxis acceptability, Côte d’Ivoire, 2018. The five recruitment trees corresponding to the five seeds are presented.
Only 13.4% of the participants disclosed an unknown HIV serotatus. The others said they were HIV-negative. Seventy-one MSM representing 35.3% of the participants intended to accept PrEP very probably if it was made available. Overall, participants were mostly young, mean age (standard deviation) of 25 (5.52) years; educated (82.1% of secondary and postsecondary school) and single (95.5%) (). Slightly less than one-third (27.4%) had not heard of PrEP before enrollment in the study. For those who were aware of PrEP, friends were the most common source of information (96.6%, not shown in ). A majority of men (58.7%) would prefer PrEP on a daily basis rather than on demand.
Table 1. General profile of 201 men who have sex with other men participating to a quantitative study of pre-exposure prophylaxis (PrEP) acceptability, Côte d’Ivoire, 2018.
On average, 3.4 episodes of anal sex were reported monthly. HIV testing was common (87.6% during the last 12 months) and a slight majority of MSM evaluated their risk of acquiring HIV as low or very low. However, transactional sex was frequent and condom use was not consistent neither with men nor with women ().
Barriers and facilitators of PrEP
Reported facilitators and barriers to PrEP acceptability are summarized in . Most participants thought that free access to PrEP and to HIV testing as well as personal support regarding PrEP would facilitate its acceptability. Concerning the pills supply system, 74.7% of MSM agreed that it is very important to avoid stock-outs in order to encourage PrEP acceptability. One-quarter (26.4%) of the participants had a neutral point of view on whether or not engagement in multiple sexual partnerships may be a plausible reason for PrEP uptake.
Table 2. Main facilitators and barriers reported by 201 men who have sex with other men participating to a quantitative study of pre-exposure prophylaxis (PrEP) acceptability, Côte d’Ivoire, 2018.
Regarding barriers, a minority of the 201 MSM contributing to the analyses (43.8%) assumed that complex procedures will not undermine acceptability. Stigma in health care centers motivated by a PrEP program targeting MSM and non receptive attitudes by the community at large were not important issues for 84.0% and 98.0% of the participants, respectively. The proportions of participants who consider the taste/size of the medication and the lack of full protection conferred by PrEP, i.e., level of protection <100% as important barriers to PrEP acceptability were 38.3% and 30.9%, respectively.
Factors independently associated to the intention to use PrEP very probably
Five factors with a p-value < 0.20 in univariate analyses were independently associated to high acceptability of PrEP after performing the surveylogistic models (). They were composed of two behavioral factors, one facilitator and two barriers.
Table 3. Factors independently associated to acceptability of PrEP as a prevention tool among 201 men who have sex with other men (MSM) in Bouaké, Côte d’Ivoire, 2018.
According to behavioral factors, MSM practicing insertive anal sex were more likely to accept PrEP as compared to versatile ones’: Odds ratio (OR) = 2.56; 95%Confidence interval (95%CI) = 1.14–5.67, , model 1. There was a better preference for PrEP among men used to receptive roles compared to versatile practitioners. However, the difference was not statistically significant (OR = 1.46; 95%CI = 0.72–2.96). Men who reported condom use at last sex with a man were also more likely to accept it if made available.
The sole facilitator independently associated to high PrEP acceptability was the cost. Men who thought that it is very important to provide PrEP free of charge were more prone to use it once made available.
Regarding the barriers, men who had important concerns about side effects were reluctant to accept PrEP. Acceptability was also lesser in men who thought that it was important to be preoccupied by the fact that PrEP may reduce ART efficacy in case they become infected with HIV (OR = 0.25; 95%CI = 0.14–0.44). The reference category was composed of those thinking that this issue was not important. Willingness to use PrEP was lower among participants with a neutral point of view, but the difference was not statistically significant (OR = 0.46; 95%CI = 0.19–1.12). Further adjusting for age did not alter the results (, model 2). HIV serostatus (unknown versus HIV-negative) was not associated to acceptability neither in univariate analyses nor in multivariate ones.
Discussion
High acceptability of PrEP, as defined in this study i.e., Intention to adopt it very probably if made available, was determined by two behavioral factors (condom use and sexual role), one facilitator (free access to PrEP) and two obstacles (concerns about side effects and antiretroviral therapy efficacy once someone under PrEP becomes HIV-positive).
The level of PrEP acceptability among MSM varies across contexts and countries (Brooks et al., Citation2012; Rocha et al., Citation2014; Yang et al., Citation2013; Yi et al., Citation2017). This is due to diverse factors including the definition of acceptability and prior knowledge (Lim et al., Citation2017; Rana et al., Citation2018; Torres et al., Citation2018; Yi et al., Citation2017). A national Internet survey conducted in China in 2017 revealed that only 26% of MSM would definitely initiate PrEP (Han et al., Citation2019). Since the definition of high acceptability was quite similar in the study from China and the current one, the difference in levels may be reflective of prior knowledge that was lower in China (22.4%) as compared to Bouaké (72.6%). A study conducted among at-risk MSM in Toronto, Canada, revealed that PrEP acceptability rose with awareness from 2013 to 2016 (Rana et al., Citation2018). PrEP acceptability is generally high among West African MSM (Coulaud et al., Citation2018).
Providing PrEP for free was independently and positively associated with high acceptability. The cost of PrEP has already been described as an important barrier to its acceptability (Ahouada et al., Citation2019; Peng et al., Citation2018). Despite budgetary constraints, PrEP programs in resource limited settings like Côte d’Ivoire should consider offering it free of charge to MSM. In this respect and to reduce the overall economic burden for countries, PrEP programs could promote PrEP, where possible, to men at higher risk like those who have frequent unprotected sex, high number of sexual partners and HIV-positive sexual partners (Beyrer et al., Citation2012; Buchbinder et al., Citation2014; Mitchell et al., Citation2018). In Côte d’Ivoire, PrEP could be available free of charge for MSM in 2020.
Men who reported condom use at last sex were more inclined to accept PrEP. This is counter intuitive since one may expect MSM having unprotected sex to be more interested by PrEP than those who don’t (Frankis et al., Citation2016; Peng et al., Citation2018; Torres et al., Citation2018). This finding may suggest that some MSM would like to switch from condoms to PrEP or have strong concerns about their risk of acquiring HIV and are opened to combined prevention packages that upgrade their protection level. Among Toronto MSM, concerns about HIV risk was associated with willingness to use PrEP (OR = 2.85; 95%CI = 2.30–3.54) (Rana et al., Citation2018). Neither condom use nor PrEP protects fully against HIV. Hence, the predisposition of some men to adopt both methods, as seen here and also elsewhere with Brazilian MSM (Torres et al., Citation2018), is encouraging. Unprotected receptive anal sex accounts for a larger population-attributable fraction of new HIV infections than unprotected insertive anal sex (Buchbinder et al., Citation2014; Koblin et al., Citation2006). Accordingly, one would expect men practicing mostly receptive sex to be more prone to use PrEP. However, when compared to versatile men, it was those reporting insertive sex who were more likely to accept PrEP if made available. The absence of a positive relationship between receptive sex and high PrEP acceptability along with inconsistent condom use (37.8% of men did not use condom at last sex), and the relatively high proportion of men who did not hear of PrEP prior to the study (27.4%) call for continuing awareness-raising activities targeting MSM and addressing HIV risk factors and new prevention methods such as PrEP. PrEP education will also help MSM understand that if HIV is secondarily acquired, PrEP-selected resistance is rare. In PrEP trials, resistance was limited to participants with seronegative acute infection at the time of randomization (Baeten et al., Citation2013). Indeed, in adherent people under PrEP, drug pressure is high enough to prevent HIV infection and in non adherent ones, the pressure is too low to result in resistance selections (Baeten et al., Citation2013). Sensitization on ART resistance following PrEP is critical because, in this study, being less preoccupied by ART response after acquiring HIV was positively associated to acceptability.
Worries about side effects have been pointed out as major barriers to high PrEP acceptability in both qualitative and mixed methods studies (Eakle et al., Citation2019; Peng et al., Citation2018). This consideration is reflected in this quantitative study where men not expressing concerns about side effects were more attracted by PrEP. Recently, the US Preventive Services Task Force has stated that there was evidence that PrEP is associated with small harms, including kidney and gastrointestinal adverse effects (Owens et al., Citation2019). Hence, apprehension about side effects is understandable because MSM eligible to PrEP are HIV-negative and generally healthy. However, it should be acknowledged that PrEP substantially reduces the risk of acquiring HIV in men at higher risk. For those men, the advantages of PrEP far outweigh the drawbacks (Huang et al., Citation2018; Owens et al., Citation2019). Before prescribing PrEP, mens’ reluctance should be addressed by health care workers through personalized discussion sessions on side effects, their tolerability and options like on demand use that may minimize the repercussion of side effects on daily life. PrEP awareness enhances the likelihood of accepting it despite side effects. In Texas, USA, Latino MSM unaware of PrEP were less likely to accept it due to their fear of common side effects (Garcia & Harris, Citation2017). Overall, a misunderstanding of PrEP objectives, advantages and drawbacks will impede its implementation among MSM.
The establishment of a strong and flexible medication supply system that minimize stock-outs and the improvement of the relationship between MSM and health care providers are among the other general considerations a PrEP implementation program should account for in light of the findings of this study (Eakle et al., Citation2019; Ripin et al., Citation2014). Dealing with PrEP-related stigma in general and in health care centers in particular will reduce inequities in access and foster PrEP uptake among MSM (Peng et al., Citation2018). In line with results from other settings (Jenness et al., Citation2017; Kimani et al., Citation2019), some participants expressed concerns about risk taking following PrEP. However, this issue was not independently associated with high acceptability in this study. In any case, a mathematical model of HIV transmission dynamics among MSM in the United States of America showed that risk compensation was unlikely to decrease the impact of PrEP in preventing HIV infection (Jenness et al., Citation2017).
Even though high PrEP acceptability has been used previously to assess acceptability (Han et al., Citation2019), some men who reported less probable use may adopt PrEP if made available. Sensitive questions related to sexual, or even to PrEP acceptability, may have resulted in social desirability biases. However, the friendly-environment and the fact that interviews were led by peer-educators may have limited its effect. The study was carried out in one city, Bouaké. Its rank, second largest of the country, and its localization, central Côte d’Ivoire, made it a major transit point for many people from Côte d’Ivoire and neighboring countries, such as Mali and Burkina Faso. In addition, the reported mean numbers (SD) of MSM known in Bouaké (27.0 (26.07)) and elsewhere in Côte d’Ivoire (28.9 (45.28)) were quite similar. Accordingly, the findings can be apropos beyond Bouaké.
Conclusion
PrEP should be part of the combination prevention package offered to MSM in Côte d’Ivoire. Its implementation should be preceded by awareness-raising campaigns on its advantages and drawbacks and on HIV-risk behavior.
Acknowledgements
The authors thank the participants, the MSM community of Bouaké, and all team members in Côte d’Ivoire.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ahouada, C., Diabate, S., Gning, N. N., Hessou, S., Batona, G., Guedou, F. A., … Alary, M. (2019). Acceptability of pre-exposure prophylaxis (PrEP) among men who have sex with men (MSM) in Benin: A qualitative study. AIDS Care, https://doi.org/10.1080/09540121.2019.1622643
- Baeten, J. M., Haberer, J. E., Liu, A. Y., & Sista, N. (2013). Preexposure prophylaxis for HIV prevention: Where have we been and where are we going? JAIDS Journal of Acquired Immune Deficiency Syndromes, 63(Suppl 2), S122–S129. https://doi.org/10.1097/QAI.0b013e3182986f69
- Beyrer, C., Baral, S. D., van Griensven, F., Goodreau, S. M., Chariyalertsak, S., Wirtz, A. L., & Brookmeyer, R. (2012). Global epidemiology of HIV infection in men who have sex with men. The Lancet, 380(9839), 367–377. https://doi.org/10.1016/S0140-6736(12)60821-6
- Brooks, R. A., Landovitz, R. J., Kaplan, R. L., Lieber, E., Lee, S. J., & Barkley, T. W. (2012). Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: A mixed methods study. AIDS Patient Care and STDs, 26(2), 87–94. https://doi.org/10.1089/apc.2011.0283
- Buchbinder, S. P., Glidden, D. V., Liu, A. Y., McMahan, V., Guanira, J. V., Mayer, K. H., Goicochea, P., & Grant, R. M. (2014). HIV pre-exposure prophylaxis in men who have sex with men and transgender women: A secondary analysis of a phase 3 randomised controlled efficacy trial. The Lancet Infectious Diseases, 14(6), 468–475. https://doi.org/10.1016/S1473-3099(14)70025-8
- Coulaud, P. J., Sagaon-Teyssier, L., M'Madi Mrenda, B., Maradan, G., Mora, M., Bourrelly, M., Dembélé Keita, B., Keita, A. A., Anoma, C., Babo Yoro, S.-A., Dah, T. T. E., Coulibaly, C., Mensah, E., Agbomadji, S., Bernier, A., Couderc, C., Laurent, C., & Spire, B. (2018). Interest in HIV pre-exposure prophylaxis in men who have sex with men in West Africa (CohMSM ANRS 12324 – Expertise France). Tropical Medicine & International Health, 23(10), 1084–1091. https://doi.org/10.1111/tmi.13129
- Diabaté, S., Maheu-Giroux, M., Vesga, J. F., Boily, M. C., & Alary, M. (2015). Plan d’accélération de la réponse nationale au VIH en Côte d’Ivoire. Rapport d’enquête de l’ONUSIDA. http://www.crchudequebec.ulaval.ca/files/Rapport_ONUSIDA_RCI_final.pdf
- Eakle, R., Weatherburn, P., & Bourne, A. (2019). Understanding user perspectives of and preferences for oral PrEP for HIV prevention in the context of intervention scale-up: A synthesis of evidence from sub-Saharan Africa. Journal of The international Aids Society, 22(Suppl 4), e25306. https://doi.org/10.1002/jia2.25306
- Frankis, J., Young, I., Flowers, P., & McDaid, L. (2016). Who will use pre-exposure prophylaxis (PrEP) and why?: Understanding PrEP awareness and acceptability amongst men who have sex with men in the UK–A mixed methods study. PLoS One, 11(4), e0151385. https://doi.org/10.1371/journal.pone.0151385
- Garcia, M., & Harris, A. L. (2017). PrEP awareness and decision-making for Latino MSM in San Antonio, Texas. PLoS One, 12(9). Article e0184014. https://doi.org/10.1371/journal.pone.0184014
- Grant, R. M., Lama, J. R., Anderson, P. L., McMahan, V., Liu, A. Y., Vargas, L., Goicochea, P., Casapía, M., Guanira-Carranza, J. V., Ramirez-Cardich, M. E., Montoya-Herrera, O., Fernández, T., Veloso, V. G., Buchbinder, S. P., Chariyalertsak, S., Schechter, M., Bekker, L.-G., Mayer, K. H., Kallás, E. G., … Glidden, D. V. (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine, 363(27), 2587–2599. https://doi.org/10.1056/NEJMoa1011205
- Han, J., Bouey, J. Z. H., Wang, L., Mi, G., Chen, Z., He, Y., Viviani, T., & Zhang, F. (2019). PrEP uptake preferences among men who have sex with men in China: Results from a national Internet survey. Journal of the International AIDS Society, 22(2). Article e25242. https://doi.org/10.1002/jia2.25242
- Handcock, M. S., Fellows, I. E., & Gile, K. J. (2016). RDS analyst: Software for the analysis of respondent-driven sampling data (Version 0.65) [Computer software]. http://hpmrg.org
- Huang, X., Hou, J., Song, A., Liu, X., Yang, X., Xu, J., Zhang, J., Hu, Q., Chen, H., Chen, Y., Meyers, K., & Wu, H. (2018). Efficacy and safety of oral TDF-based pre-exposure prophylaxis for men who have sex with men: A systematic review and meta-analysis. Frontiers in Pharmacology, 9, 799. https://doi.org/10.3389/fphar.2018.00799
- Jenness, S. M., Sharma, A., Goodreau, S. M., Rosenberg, E. S., Weiss, K. M., Hoover, K. W., Smith, D. K., Sullivan, P., & Prestage, G. (2017). Individual HIV risk versus population impact of risk compensation after HIV preexposure prophylaxis initiation among men who have sex with men. PLoS One, 12(1), e0169484. https://doi.org/10.1371/journal.pone.0169484
- Kimani, M., van der Elst, E. M., Chiro, O., Oduor, C., Wahome, E., Kazungu, W., Shally, M., Rinke de Wit, T. F., Graham, S. M., Operario, D., & Sanders, E. J. (2019). PrEP interest and HIV-1 incidence among MSM and transgender women in coastal Kenya. Journal of the International AIDS Society, 22(6). Article e25323. https://doi.org/10.1002/jia2.25323
- Koblin, B. A., Husnik, M. J., Colfax, G., Huang, Y., Madison, M., Mayer, K., Barresi, P. J., Coates, T. J., Chesney, M. A., & Buchbinder, S. (2006). Risk factors for HIV infection among men who have sex with men. AIDS, 20(5), 731–739. https://doi.org/10.1097/01.aids.0000216374.61442.55
- Lim, S. H., Mburu, G., Bourne, A., Pang, J., Wickersham, J. A., Wei, C. K. T., … Azwa, I. (2017). Willingness to use pre-exposure prophylaxis for HIV prevention among men who have sex with men in Malaysia: Findings from an online survey. PLoS One, 12(9). Article e0182838. https://doi.org/10.1371/journal.pone.0182838
- McCormack, S., Dunn, D. T., Desai, M., Dolling, D. I., Gafos, M., Gilson, R., Sullivan, A. K, Clarke, A., Reeves, I., Schembri, G., Mackie, N., Bowman, C., Lacey, C. J., Apea, V., Brady, M., Fox, J., Taylor, S., Antonucci, S., Khoo, S. H., … Gill, O. N. (2016). Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet, 387(10013), 53–60. https://doi.org/10.1016/S0140-6736(15)00056-2
- Mitchell, K. M., Dimitrov, D., Hughes, J. P., Xia, F., Donnell, D., Amico, K. R., Bokoch, K., Chitwarakorn, A., Bekker, L.-G., Holtz, T. H., Mannheimer, S., Grant, R. M., & Boily, M. C. (2018). In what circumstances could nondaily preexposure prophylaxis for HIV substantially reduce program costs? AIDS, 32(6), 809–818. https://doi.org/10.1097/QAD.0000000000001766
- Molina, J.-M., Capitant, C., Spire, B., Pialoux, G., Cotte, L., Charreau, I., Tremblay, C., Le Gall, J.-M., Cua, E., Pasquet, A., Raffi, F., Pintado, C., Chidiac, C., Chas, J., Charbonneau, P., Delaugerre, C., Suzan-Monti, M., Loze, B., Fonsart, J., … Delfraissy, J.-F. (2015). On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. New England Journal of Medicine, 373(23), 2237–2246. https://doi.org/10.1056/NEJMoa1506273
- Mugo, N. R., Ngure, K., Kiragu, M., Irungu, E., & Kilonzo, N. (2016). PrEP for Africa: What we have learnt and what is needed to move to program implementation. Current Opinion in HIV and AIDS, 11(1), 80–86. https://doi.org/10.1097/COH.0000000000000224
- Owens, D. K., Davidson, K. W., Krist, A. H., Barry, M. J., Cabana, M., Caughey, A. B., Curry, S. J., Doubeni, C. A., Epling, J. W., Kubik, M., Landefeld, C. S., Mangione, C. M., Pbert, L., Silverstein, M., Simon, M. A., Tseng, C.-W., Wong, J. B., & Wong, J. B. (2019). Preexposure prophylaxis for the prevention of HIV infection: US preventive services task force recommendation statement. JAMA, 321(22), 2203–2213. https://doi.org/10.1001/jama.2019.6390
- Pelletier, S. J., Gagnon, M.-P., Diabaté, S., Kra, O., Biékoua, Y. J., Osso, G. D., Diané, B., N’Dhatz-Ebagnitchié, M., Ahouada, C., & Alary, M. (2019). Preexposure prophylaxis (PrEP) in men who have sex with men in Bouaké, côte d'Ivoire: A qualitative evaluation of acceptability. The Open AIDS Journal, 13(1), 49–58. https://doi.org/10.2174/1874613601913010049
- Peng, P., Su, S., Fairley, C. K., Chu, M., Jiang, S., Zhuang, X., & Zhang, L. (2018). A global estimate of the acceptability of pre-exposure prophylaxis for HIV among men who have sex with men: A systematic review and meta-analysis. AIDS and Behavior, 22(4), 1063–1074. https://doi.org/10.1007/s10461-017-1675-z
- Rana, J., Wilton, J., Fowler, S., Hart, T. A., Bayoumi, A. M., & Tan, D. H. S. (2018). Trends in the awareness, acceptability, and usage of HIV pre-exposure prophylaxis among at-risk men who have sex with men in Toronto. Canadian Journal of Public Health, 109(3), 342–352. https://doi.org/10.17269/s41997-018-0064-3
- Ripin, D. J., Jamieson, D., Meyers, A., Warty, U., Dain, M., & Khamsi, C. (2014). Antiretroviral procurement and supply chain management. Antiviral Therapy, 19(Suppl 3), 79–89. https://doi.org/10.3851/IMP2903
- Rocha, L. M., Campos, M. J., Brito, J., Fuertes, R., Rojas, J., Pinto, N., Mendão, L., & Esteves, J. (2014). Acceptability of PrEP among HIV negative Portuguese men who have sex with men that attended 2014 Lisbon pride fair. Journal of the International AIDS Society, 17(4 Suppl 3), 19734. https://doi.org/10.7448/IAS.17.4.19734
- Rothman, K. J., Greenland, S., & Lash, T. L. (2008). Modern epidemiology (3rd ed.). Philadelphia: Lippincott Williams & Wilkins, 263. pp. 261–262.
- Torres, T. S., De Boni, R. B., de Vasconcellos, M. T., Luz, P. M., Hoagland, B., Moreira, R. I., Veloso, V. G., & Grinsztejn, B. (2018). Awareness of prevention strategies and willingness to use preexposure prophylaxis in Brazilian men who have sex with men using apps for sexual encounters: Online cross-sectional study. JMIR Public Health and Surveillance, 4(1), e11. https://doi.org/10.2196/publichealth.8997
- UNAIDS. (2019). UNAIDS data 2019. https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf
- Volz, E., & Heckathorn, D. D. (2008). Probability based estimation theory for respondent driven sampling. JOS, 24(1), 79–97.
- Yang, D., Chariyalertsak, C., Wongthanee, A., Kawichai, S., Yotruean, K., Saokhieo, P., Guadamuz, T., Suwanvanichkij, V., Beyrer, C., Chariyalertsak, S., & Graham, S. M. (2013). Acceptability of pre-exposure prophylaxis among men who have sex with men and transgender women in Northern Thailand. PLoS One, 8(10), e76650. https://doi.org/10.1371/journal.pone.0076650
- Yi, S., Tuot, S., Mwai, G. W., Ngin, C., Chhim, K., Pal, K., Igbinedion, E., Holland, P., Choub, S. C., & Mburu, G. (2017). Awareness and willingness to use HIV pre-exposure prophylaxis among men who have sex with men in low- and middle-income countries: A systematic review and meta-analysis. Journal of the International AIDS Society, 20(1), 21580. https://doi.org/10.7448/IAS.20.1.21580
