ABSTRACT
HIV prevention needs among urban refugee and displaced youth engaged in transactional sex are understudied. We examined associations between transactional sex and the HIV prevention cascade among urban refugee/displaced youth in Kampala, Uganda. We conducted a cross-sectional survey with a peer-driven sample of refugee/displaced adolescent girls and young women (n = 324) and adolescent boys and young men (n = 88) aged 16–24 living in Kampala’s informal settlements. We conducted gender-disaggregated multivariable linear and logistic regressions to examine associations between past 12-month transactional sex and: lifetime HIV testing, condom self-efficacy, and recent [past 3-month] consistent condom use. Among the 27% of young women reporting transactional sex, 63% reported HIV testing. In multivariable analyses with young women, transactional sex was associated with higher condom self-efficacy, increased consistent condom use, but not HIV testing. Among the 48% of young men reporting transactional sex, 50% reported HIV testing. In multivariable analyses with young men, transactional sex was associated with lower HIV testing but not with condom self-efficacy or consistent condom use. Young men were 68% less likely to report HIV testing if transactional sex engaged. Findings point to urgent HIV testing gaps among transactional sex engaged urban refugee/displaced youth and a need for gender-tailored HIV prevention strategies.
Introduction
There are 70 million forcibly displaced persons in the world, half under 18 years old (UNHCR, Citation2019a). Many refugees across the globe live in urban areas in informal settlements, often referred to as “slums” (UNHCR, Citation2019b). Young refugee and displaced persons in informal settlements experience social and economic marginalization and constrained access to health resources; these converge to harm sexual and reproductive health (Culbreth et al., Citation2020; Kamara et al., Citation2019). Uganda is an important global context to explore sexual and reproductive health among refugee and displaced youth, as it hosts Sub-Saharan Africa’s largest refugee population (UNHCR, Citation2019a, Citation2019b).
Transactional sex among youth may be common in Uganda. A review reported the prevalence of selling sex in the past 12 months ranged from 4% to 75% among girls and 2% to 35% among boys (Krisch et al., Citation2019). Transactional sex refers to exchanging sexual services in return for material (e.g., money, clothing, shelter) and non-material (e.g., status, protection) compensation (Krisch et al., Citation2019). It is distinct from commercial sex work (Krisch et al., Citation2019; Stoebenau et al., Citation2016), as persons engaged in transactional sex may not consider themselves sex workers and may not see their partner(s) as a client (Krisch et al., Citation2019; Stoebenau et al., Citation2016).
Poverty, food insecurity, precarious legal status, and lack of formal employment opportunities contribute to selling sex among refugee and displaced persons (Williams et al., Citation2018; Women’s Refugee Commission, Citation2016). Refugee sex workers may experience language barriers, discrimination, and legal restrictions in their host country that reduce access to formal employment as well as health services (Ferguson et al., Citation2017; Rosenberg & Bakomeza, Citation2017; Scorgie et al., Citation2011; Women’s Refugee Commission, Citation2016). Social and economic marginalization experienced by refugee sex workers contributes to poor sexual health outcomes (Women’s Refugee Commission, Citation2016), including HIV and sexually transmitted infections (STI) exposure alongside sexual and reproductive health care barriers (Burton et al., Citation2010; Ferguson et al., Citation2017; Rosenberg & Bakomeza, Citation2017). These contribute to refugee sex workers’ unmet HIV prevention needs (Rosenberg & Bakomeza, Citation2017).
There may be gender differences in experiences of transactional sex (Krisch et al., Citation2019). Adolescent girls and young women who sell sex may have higher odds of depression (Svedin & Priebe, Citation2007) and sexual violence (Choudhry et al., Citation2014) compared with adolescent boys and young men who sell sex. Adolescent boys and young men who sell sex are understudied (Baral et al., Citation2015; Krisch et al., Citation2019; Wendland et al., Citation2019), although they share similar HIV vulnerabilities as adolescent girls and young women associated with condomless sex, multiple sex partners, co-occurring STIs, and substance use (Ballester-Arnal et al., Citation2014; Baral et al., Citation2015). Criminalization of same-sex sexual practices, HIV non-disclosure, and sex work contribute to stigma and poor sexual health outcomes among persons who sell sex (Baral et al., Citation2015; Brookfield et al., Citation2020; Okanlawon et al., Citation2013).
HIV prevention needs are understudied among refugee and displaced adolescents and youth engaged in transactional sex – particularly adolescent boys and young men (Ballester-Arnal et al., Citation2014; Ferguson et al., Citation2017; Okanlawon et al., Citation2013; Singh, Aryasinghe, et al., Citation2018; Wendland et al., Citation2019). A systematic review on sex workers in conflict-affected and humanitarian settings found that sex workers remain underserved in HIV prevention, education, testing and treatment (Ferguson et al., Citation2017). Another systematic review on sexual and reproductive health services in humanitarian settings reported knowledge gaps regarding adolescents’ sexual and reproductive health outcomes (Singh, Smith, et al., Citation2018). A qualitative study with sex working adult refugee women in Kampala reported experiences of stigma, silence, violence, and barriers to sexual and reproductive health information and services (Rosenberg & Bakomeza, Citation2017). Commercial sex work was associated with HIV/STI infection among youth living in Kampala’s informal settlements, however this study did not examine refugee status or transactional sex (Culbreth et al., Citation2020). In sum there are knowledge gaps regarding transactional sex among urban refugee and displaced youth and its associations with HIV testing and prevention uptake.
Gender differences in transactional sex are understudied yet important to examine in Uganda – where HIV prevalence among adolescent girls and young women is four-fold higher than among adolescent boys and young men (Uganda Ministry of Health, Citation2019). The HIV prevention cascade describes the process involved in effectively implementing HIV prevention strategies, including demand (e.g., awareness), supply (e.g., availability, access), and adherence (e.g., efficacy and empowerment to use strategies) (Hargreaves et al., Citation2016). To address these knowledge gaps, our study examines associations between transactional sex and lifetime HIV testing uptake, recent consistent condom use, and condom efficacy, among urban refugee and displaced adolescents and youth in Kampala. Our secondary objective was to examine associations between transactional sex and pre-exposure prophylaxis (PrEP) awareness, access, and uptake among this population.
Methods
In collaboration with refugee-led community-based and government agencies, we implemented a cross-sectional survey from January–April 2018 in Kampala, Uganda. Eligible participants included young women and men aged 16–24 who self-identified: as a refugee or displaced person or having refugee or displaced parents; living in one of Kampala’s informal settlements of Kabalagala, Rubaga, Kansanga, Katwe, or Nsambya; and able to provide informed consent. We recruited and trained 12 refugee-identified peer research assistants (PRA) (n = 12; four young men, eight young women) aged 18–24 years. PRAs administered the tablet-based survey at a location of the participant’s choice (e.g., football pitch, community agency). The survey duration was approximately 35–45 min, and each participant received a UGX 12,500-shilling (∼USD 3.74) honorarium.
The PRAs recruited participants using convenience sampling, including peer outreach and word-of-mouth. PRAs gave each participant a recruitment “coupon” with their contact information and invited them to recruit a maximum of five refugee/displaced youth from their social networks. We oversampled adolescent girls and young women to account for their overrepresentation in Uganda’s HIV epidemic. The study protocol was approved by the University of Toronto, Canada, and the Uganda Ministry of Health (ADM: 105/261/01).
Measures
Outcome variables included: (1) condom efficacy, (2) recent (past 3-month) consistent condom use, and (3) lifetime HIV testing. Condom efficacy was assessed with the Condom Efficacy scale (Shaweno & Tekletsadik, Citation2013) to evaluate confidence in the ability to correctly use and negotiate condom use (Cronbach’s α = 0.95, range 7–35). Recent consistent condom use was assessed using a dichotomous question: “In the last three months, how frequently did you or your sexual partner(s) use a condom during sexual intercourse?” This variable was recoded into a binary variable: 0 = never, infrequent, sometimes, and 1 = every time. Lifetime HIV testing was assessed using a dichotomous question: “I have had an HIV test in my lifetime”.
We examined PrEP awareness, access, and uptake. PrEP awareness was assessing by asking, “Pre-exposure prophylaxis (HIV medication taken before sex to avoid becoming HIV infected) is available in my area.” Knowledge of PrEP access was assessed with: “I know how to access PrEP.” Recent PrEP uptake was assessed with the item: “I have accessed PrEP in the last 3 months.”
The independent variable of interest was transactional sex, assessed by asking if participants had been provided with any of the following in exchange for sex in the past 12-months: money, drugs; shelter; food; gifts; clothes; services; other. An affirmative response was coded as transactional sex engagement.
Covariates included sociodemographic variables: age (continuous), education level (dichotomous: no formal education/less than secondary school vs. post-secondary education and above), employment status (dichotomous: employed/student vs. unemployed), and time lived in Uganda (categorical: <one year, 1–5 years, >5 years).
Statistical analysis
We first conducted descriptive analyses of all variables to determine frequencies and proportions. Descriptive analyses included all participants with available data. We conducted gender-disaggregated analyses. First, we conducted bivariate analyses (T-test, χ²) to determine differences by transactional sex engagement for adolescent girls and young women (n = 324) and adolescent boys and young men (n = 88). Second, we conducted multivariable linear (condom efficacy) and logistic (lifetime HIV testing, recent consistent condom use) regression to examine associations with transactional sex, adjusting for sociodemographic (age, education, time in Uganda) factors. We report the standardized coefficient for multiple regression and adjusted odds ratios (aORs) for the multivariable logistic regression, highlighting those significant at the p < 0.05 level. Missing responses were excluded from the analyses; the number of complete responses were reported for each variable. All statistical analyses were performed using Stata version 14 software.
Results
Among 324 adolescent girls and young women, 26.54% (n = 86) reported past 12-month transactional sex engagement (67.4% for money only, 32.6% for money and other goods [e.g., accommodation, food, transport, drugs]). Of adolescent girls and young women who reported transactional sex, 62.8% (n = 54) reported a lifetime HIV test and 73.8% (n = 59) reported past 3-month consistent condom use. Among 88 adolescent boys and young men, 47.7% (n = 42) reported past 12-month transactional sex (21.4% for money only; 78.6% for money and other goods). Among transactional sex engaged adolescent boys and young men, 50.0% reported receiving a lifetime HIV test and 53.3% (n = 16) reported past 3-month consistent condom use ().
Table 1. Factors associated with transactional sex engagement among urban refugee and displaced youth living in informal settlements in Kampala, Uganda (N = 412).
Associations between transactional sex engagement and PrEP availability, knowledge, and recent access
Using chi-square independence tests (see ), we found no statistically significant differences in PrEP outcomes among participants by transactional sex involvement. Among transactional sex engaged adolescent girls and young women, 7.0% (n = 6/86) reported awareness of PrEP in their community, 7.0% (n = 6/86) reported knowing where to access PrEP, and 1.2% (n = 1/86) reported past 3-month PrEP access. Among adolescent boys and young men, 2.4% (n = 1/42) of transactional sex engaged participants reported PrEP awareness, 4.8% (n = 2/42) knowledge of how to access PrEP, and none reported recent PrEP uptake.
Associations between transactional sex engagement and HIV prevention cascades among urban refugee and displaced adolescent girls and young women
In adjusted analyses, transactional sex engaged adolescent girls and young women reported significantly higher condom efficacy scores (β = 0.21, p < 0.0001, 95% CI = 2.07, 5.89) and increased odds of recent consistent condom use (aOR 7.83, 95% CI = 3.63, 16.82) than those not involved in transactional sex (, , ). Transactional sex, however, was not associated with differences in lifetime HIV testing among adolescent girls and young women (aOR 0.76, 95% CI = 0.42, 1.37) (, ).
Figure 1. Past 3-month consistent condom use and lifetime HIV testing by gender and transactional sex engagement among urban refugee and displaced youth aged 16–24 in Kampala, Uganda (N = 412). Legend: adolescent girls and young women: AGYW; adolescent boys and young men: ABYM.
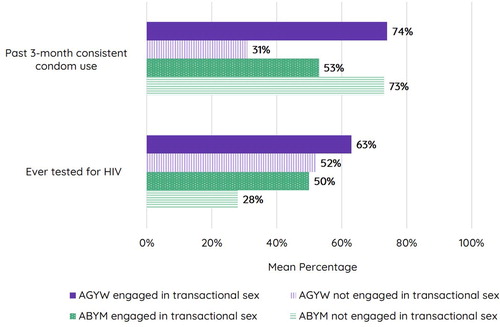
Figure 2. Condom efficacy by gender and transactional sex engagement among urban refugee and displaced youth aged 16–24 in Kampala, Uganda (N = 412). Legend: adolescent girls and young women: AGYW; adolescent boys and young men: ABYM.
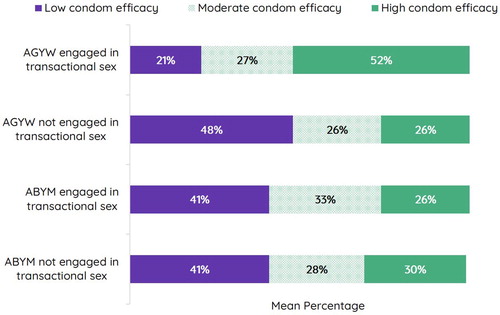
Table 2. Association between transactional sex engagement and HIV prevention cascades among urban refugee and displaced youth living in informal settlements in Kampala, Uganda (N = 412).
Associations between transactional sex engagement and HIV prevention cascades among urban refugee and displaced adolescent boys and young men
In adjusted analyses, we found no associations between transactional sex engagement and condom efficacy (β = −.09, p > .050, 95% CI = −3.35, 1.26) or recent consistent condom use (aOR 0.49, 95% CI = 0.14, 1.74) among adolescent boys and young men (, , ). Holding other factors constant, transactional sex was associated with lower odds of lifetime HIV testing (aOR 0.32, 95% CI = 0.11, 0.89) (, ). Adolescent boys and young men engaged in transactional sex were 68% less likely to have ever received an HIV test compared to their non-transactional sex involved counterparts (, ).
Discussion
Our findings signal that transactional sex engaged refugee and displaced adolescents and youth in Kampala fall far short of the UNAIDS target of 90% of persons knowing their HIV status. This is particularly concerning for transactional sex engaged youth as they may have elevated HIV exposure due to behavioral, interpersonal, and social factors (Logie et al., Citation2018; Rosenberg & Bakomeza, Citation2017). We found important gender differences. While transactional sex was not associated with HIV testing among adolescent girls and young women, transactional sex was associated with a lower likelihood of testing among adolescent boys and young men. Transactional sex among adolescent girls and young women was associated with higher recent condom use and condom self-efficacy – suggesting increased HIV prevention engagement. Yet among adolescent boys and young men, there was no association between transactional sex and recent condom use or condom self-efficacy, again revealing HIV vulnerabilities. In sum, findings point to urgent gaps in HIV testing among transactional sex engaged refugee and displaced youth and a need for gender tailored strategies to address HIV vulnerabilities, particularly among adolescent boys and young men.
Findings corroborate research that documents unmet HIV prevention needs for transactional sex engaged young men (Ballester-Arnal et al., Citation2014; Okanlawon et al., Citation2013; Wendland et al., Citation2019). This could be due to intersecting stigma (e.g., sex work stigma, HIV-related stigma) and a lack of tailored HIV outreach and services for refugee sex working men in Kampala. A Jamaican study also reported that selling sex was associated with men’s HIV vulnerabilities, including lower safer sex self-efficacy and reduced condom use (Logie et al., Citation2018). It is plausible that transactional sex offers less opportunities for networking, connections to HIV prevention resources, and sex worker social support than in formal commercial sex work (Baral et al., Citation2015; Valente et al., Citation2020). Increased condom use and condom self-efficacy among transactional sex engaged adolescent girls and young women may reflect the benefits of refugee specific sex work agencies for women in Kampala that enhance HIV information, prevention access, and solidarity (Rosenberg & Bakomeza, Citation2017; Uganda Ministry of Health, Citation2019).
Study limitations include the cross-sectional design that precludes establishing causality. We intentionally oversampled AGYW due to their overrepresentation in Uganda’s epidemic, yet that reduced the sample size for adolescent boys and young men. Data collectors did not collect refusal rates; using standardized instruments to record refusals and reasons for refusals would improve data quality. We included self-reported HIV status; findings would be stronger with serological data. We did not assess gender of sex partners for adolescent boys and young men, and this could enhance understanding of their risk profile. We also did not assess sex work stigma or sex work social cohesion, and these could have highlighted social factors important to HIV outcomes. Despite these limitations, we contribute to the nascent literature on transactional sex engagement among refugee and displaced youth to point to critical gaps in HIV testing and prevention and the need for a gender-based analysis.
Situating our findings within the HIV prevention cascade can inform targets for refugee and displaced youth interventions to increase demand (e.g., accurate risk perception, awareness and acceptability of HIV testing, condoms, and PrEP), supply (e.g., strategies to improve availability and access of HIV testing and condoms), and adherence (e.g., condom efficacy) (Hargreaves et al., Citation2016). Most participants were unaware of PrEP – an actionable gap as PrEP is available at no cost to persons selling sex at government clinics across Kampala. We need innovative (Davies & Pinto, Citation2015), rights-based strategies tailored by gender, age and transactional sex engagement to advance HIV prevention with refugee and displaced youth. Urgent focus on the HIV prevention cascade is needed for refugee and displaced young men engaged in transactional sex.
Acknowledgements
We acknowledge all of the peer navigators and participants, as well as collaborating agencies: Ugandan Ministry of Health, Office of the Prime Minister, Young African Refugees for Integral Development (YARID), Tomorrow Vijana, Most At Risk Populations Initiative (MARPI), and InterAid Uganda.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ballester-Arnal, R., Gil-Llario, M. D., Salmeron-Sánchez, P., & Giménez-García, C. (2014). HIV prevention interventions for young male commercial sex workers. Current HIV/AIDS Reports, 11(1), 72–80. https://doi.org/10.1007/s11904-013-0195-3
- Baral, S. D., Friedman, M. R., Geibel, S., Rebe, K., Bozhinov, B., Diouf, D., Sabin, K., Holland, C. E., Chan, R., & Cáceres, C. F. (2015). Male sex workers: Practices, contexts, and vulnerabilities for HIV acquisition and transmission. The Lancet, 385(9964), 260–273. https://doi.org/10.1016/S0140-6736(14)60801-1
- Brookfield, S., Dean, J., Forrest, C., Jones, J., & Fitzgerald, L. (2020). Barriers to accessing sexual health services for transgender and male sex workers: A systematic qualitative meta-summary. AIDS and Behavior, 24(3), 682–696. https://doi.org/10.1007/s10461-019-02453-4
- Burton, A., Butler, J., Marwah, P., Mazzacurati, C., Schilperoord, M., & Steen, R. (2010). Addressing HIV and sex work. Forced Migration Review, 25–27. https://www.fmreview.org/AIDS/Burton-et-al.htm
- Choudhry, V., Östergren, P.-O., Ambresin, A.-E., Kyagaba, E., & Agardh, A. (2014). Giving or receiving something for sex: A cross-sectional study of transactional sex among Ugandan University students. PLoS ONE, 9(11), e112431. https://doi.org/10.1371/journal.pone.0112431
- Culbreth, R., Swahn, M. H., Salazar, L. F., Ametewee, L. A., & Kasirye, R. (2020). Risk factors associated with HIV, sexually transmitted infections (STI), and HIV/STI co-infection among youth living in the slums of Kampala, Uganda. AIDS and Behavior, 24(4), 1023–1031. https://doi.org/10.1007/s10461-019-02444-5
- Davies, M. A., & Pinto, J. (2015). Targeting 90-90-90 - don’t leave children and adolescents behind. Journal of the International AIDS Society, 18(Suppl. 6), 1–6. https://doi.org/10.7448/IAS.18.7.20745
- Ferguson, A., Shannon, K., Butler, J., & Goldenberg, S. M. (2017). A comprehensive review of HIV/STI prevention and sexual and reproductive health services among sex workers in conflict-affected settings: Call for an evidence- and rights-based approach in the humanitarian response. Conflict and Health, 11(1), 1–20. https://doi.org/10.1186/s13031-017-0124-y
- Hargreaves, J. R., Delany-Moretlwe, S., Hallett, T. B., Johnson, S., Kapiga, S., Bhattacharjee, P., Dallabetta, G., & Garnett, G. P. (2016). The HIV prevention cascade: Integrating theories of epidemiological, behavioural, and social science into programme design and monitoring. The Lancet HIV, 3(7), e318–e322. https://doi.org/10.1016/S2352-3018(16)30063-7
- Kamara, J. K., Namugambe, B. M., Egessa, R., Kamanga, G., & Renzaho, A. M. N. (2019). The socioeconomic and sexual health status of young people living in urban slum areas of Kampala, Uganda. Journal of Urban Health, 96(4), 616–631. https://doi.org/10.1007/s11524-019-00347-3
- Krisch, M., Averdijk, M., Valdebenito, S., & Eisner, M. (2019). Sex trade among youth: A global review of the prevalence, contexts and correlates of transactional sex among the general population of youth. Adolescent Research Review, 4(2), 115–134. https://doi.org/10.1007/s40894-019-00107-z
- Logie, C., Lacombe-Duncan, A., Kenny, K., Levermore, K., Jones, N., Baral, S. D., Wang, Y., Marshall, A., & Newman, P. A. (2018). Social-ecological factors associated with selling sex among men who have sex with men in Jamaica: Results from a cross-sectional tablet-based survey. Global Health Action, 11(1), 1. https://doi.org/10.1080/16549716.2018.1424614
- Okanlawon, K., Adebowale, A. S., & Titilayo, A. (2013). Sexual hazards, life experiences and social circumstances among male sex workers in Nigeria. Culture, Health and Sexuality, 15(Suppl. 1), 22–33. https://doi.org/10.1080/13691058.2012.754053
- Rosenberg, J. S., & Bakomeza, D. (2017). Let’s talk about sex work in humanitarian settings: Piloting a rights-based approach to working with refugee women selling sex in Kampala. Reproductive Health Matters, 25(51), 95–102. https://doi.org/10.1080/09688080.2017.1405674
- Scorgie, F., Nakato, D., Akoth, D. O., Netshivhambe, M., Chakuvinga, P., Nkomo, P., Abdalla, P., Sibanda, S., & Richter, M. (2011). “I expect to be abused and I have fear”: Sex workers’ experiences of human rights violations and barriers to accessing healthcare in four African countries. African Sex Worker Alliance.
- Shaweno, D., & Tekletsadik, E. (2013). Validation of the condom use self-efficacy scale in Ethiopia. BMC International Health and Human Rights, 13(1), 22. https://doi.org/10.1186/1472-698X-13-22
- Singh, N. S., Aryasinghe, S., Smith, J., Khosla, R., Say, L., & Blanchet, K. (2018). A long way to go: A systematic review to assess the utilisation of sexual and reproductive health services during humanitarian crises. BMJ Global Health, 3(2), 1–12. https://doi.org/10.1136/bmjgh-2017-000682
- Singh, N. S., Smith, J., Aryasinghe, S., Khosla, R., Say, L., & Blanchet, K. (2018). Evaluating the effectiveness of sexual and reproductive health services during humanitarian crises: A systematic review. PLoS ONE, 13(7), e0199300. https://doi.org/10.1371/journal.pone.0199300
- Stoebenau, K., Heise, L., Wamoyi, J., & Bobrova, N. (2016). Revisiting the understanding of “transactional sex” in sub-Saharan Africa: A review and synthesis of the literature. Social Science and Medicine, 168, 186–197. https://doi.org/10.1016/j.socscimed.2016.09.023
- Svedin, C. G., & Priebe, G. (2007). Selling sex in a population-based study of high school seniors in Sweden: Demographic and psychosocial correlates. Archives of Sexual Behavior, 36(1), 21–32. https://doi.org/10.1007/s10508-006-9083-x
- Uganda Ministry of Health. (2019). Uganda population-based HIV impact assessment (UPHIA) 2016-2017: Final report.
- UNHCR. (2019a). Global trends: Forced displacement in 2018.
- UNHCR. (2019b). Uganda: Country refugee response plan.
- Valente, P. K., Mimiaga, M. J., Mayer, K. H., Safren, S. A., & Biello, K. B. (2020). Social capital moderates the relationship between stigma and sexual risk among male sex workers in the US Northeast. AIDS and Behavior, 24(1), 29–38. https://doi.org/10.1007/s10461-019-02692-5
- Wendland, E. M., Bessel, M., Comerlato, J., Horvath, J. D. C., Falcetta, F., Mendes Pereira, G. F., De Souza, F. M. A., Domingues, C., Maranhão, A. G. K., & Kops, N. L. (2019). Evaluating sexual health in sex workers and men who have sex with men: The SMESH cross-sectional protocol study. BMJ Open, 9(11), 1–7. https://doi.org/10.1136/bmjopen-2019-031358
- Williams, T. P., Chopra, V., & Chikanya, S. R. (2018). “It isn’t that we’re prostitutes”: Child protection and sexual exploitation of adolescent girls within and beyond refugee camps in Rwanda. Child Abuse and Neglect, 86, 158–166. https://doi.org/10.1016/j.chiabu.2018.09.015
- Women’s Refugee Commission. (2016). Mean streets identifying and responding to urban refugees’ risks of gender-based violence.
