ABSTRACT
Sexual satisfaction can be challenging for people living with HIV (PLWH). To investigate self-reported sexual satisfaction in PLWH and its association with HIV-related biomarkers, a retrospective observational cohort study with data on sociodemographic characteristics and changes in PLWH’s assessment of their sexual satisfaction over time were retrieved from the Swedish National Quality Assurance Registry (InfCareHIV) where patient-related outcomes are reported annually. PLWH who had assessed self-reported sexual satisfaction 2011–2016 were included. Sexual satisfaction was dichotomized into sexual “satisfaction and dissatisfaction” and associations were analysed. In total, 3798 patients (66% men) answered 8202 questionnaires. Overall, 67% reported sexual satisfaction, with women more satisfied than men (72% vs 64%, p < 0.0001). Sexual satisfaction did not differ between patients on antiretroviral treatment (ART) >6 months whether the viral load was suppressed or not. Overall, the probability of reporting sexual satisfaction increased by 4% annually (p < 0.001). This increase may be explained by evolving knowledge about the minimal risks of sexual HIV transmission when on ART together with Sweden’s concomitant revision of legal restrictions. The use of patient-related outcomes in clinical practice is an important tool for facilitating conversations about sexuality in order to promote the health and well-being of PLWH.
Introduction
Sexual satisfaction is challenging for many people living with HIV (PLWH), resulting in lower levels of quality of life (Zeluf-Andersson et al., Citation2019). In settings with high access to antiretroviral therapy (ART), HIV is considered a chronic condition (Nakagawa et al., Citation2012). With an ageing HIV population with increasing comorbidities and a burden of psychological and social problems, a need has emerged for knowledge about factors such as sexual satisfaction that affect the health and well-being of PLWH (Lazarus et al., Citation2016). A good health-related quality of life for PLWH has thus been proposed as the fourth “90” goal in addition to the UNAIDS 90-90-90 targets, with patient-reported outcomes (PROs) providing information about patients’ experience of treatment, care or symptoms, yielding a more holistic view of their health and well-being (Kall et al., Citation2020).
Although there is no risk of sexually transmitting HIV when the HIV viral load is suppressed (Rodger et al., Citation2019; Vernazza et al., Citation2008), many still fears transmitting HIV to a sexual partner, which negatively affects their sexual satisfaction (Peyre et al., Citation2019). However, sexual satisfaction is complex and has no consistent definition. It can be described as both a part of sexuality and a subjective evaluation of one’s sexual relationship (Lawrance & Byers, Citation1995). Sexual satisfaction can be influenced by biological, psychological, and even legal factors, and it can be measured in different ways (Mark et al., Citation2013). On the life satisfaction scale, sexual satisfaction is measured by self-reported satisfaction with sex life (with or without a partner) on a 6-point Likert scale (Fugl-Meyer et al., Citation1991).
The Swedish National Quality Assurance Registry InfCareHIV (InfCareHIV) is web-based and follows all people living with HIV from the time of their diagnosis. A validated nine-item health questionnaire was integrated into the registry in 2011 (Marrone et al., Citation2016) to annually assess PROs such as sexual satisfaction. It is not known whether there is an association between sexual satisfaction and HIV-related biomarkers, sociodemographic characteristics, or time-related variables in PLWH in Sweden. Our hypothesis was that lower levels of plasma HIV RNA might be associated with higher levels of self-reported sexual satisfaction. The aim of the study was to investigate self-reported sexual satisfaction in PLWH in Sweden and its association with HIV-related biomarkers and sociodemographic characteristics, and assess changes over time.
Methods
In a retrospective observational cohort study, data from the InfCareHIV registry was analysed and it included all PLWH ≥18 years answering the question about sexual satisfaction in the health questionnaire between 2011 and 2016. The registry includes HIV-related biomarkers, ART prescription and sociodemographic characteristics. The self-reported health questionnaire assesses PROs and patient related experiences on the following items: satisfaction with physical health, satisfaction with psychological well-being, satisfaction with sex life, ART adherence, side effects, involvement in care, and satisfaction with care (Marrone et al., Citation2016; Mellgren et al., Citation2020). The health questionnaire is intended to be offered to patients annually before the routine clinical follow-up visit, either via the internet, electronically, or on paper, and its results form a basis for the patient consultation. It can be completed in English or Swedish, or translated verbally into another language by a professional interpreter. Since it is offered annually, some of the patients answered the questionnaire more than once in this study.
The question about sexual satisfaction was adapted from the self-reported life satisfaction scale: “How satisfied are you with your sex life (regardless of whether you have sex with a partner or on your own)”. The possible answers, reported on a Likert scale, are very unsatisfied, unsatisfied, rather unsatisfied, rather satisfied, satisfied, and very satisfied (Fugl-Meyer et al., Citation1991). Marrone et al. (Citation2016) validated the test-retest reliability of the questionnaire and found good agreement for sexual satisfaction. For this study, the answers were dichotomized into sexual dissatisfaction (corresponding to Likert-scale answers very unsatisfied, unsatisfied, and rather unsatisfied) or sexual satisfaction (corresponding to Likert-scale answers: rather satisfied, satisfied, and very satisfied).
The following sociodemographic characteristics were used: gender (woman or man); mode of HIV transmission (heterosexual contact, homosexual/bisexual contact, intravenous drug use, blood products, mother-to-child transmission, and unknown/other), and country of birth (Sweden or abroad).
The following ART history and biomarkers were used: on ART > 6 months (yes or no); plasma HIV RNA (copies/mL); CD4+ T-cell (CD4) count (cells/µL), and nadir CD4-cell count. In PLWH on ART > 6 months, plasma HIV RNA was defined either as suppressed (HIV RNA < 50 copies/mL) or not suppressed (HIV RNA ≥50 copies/mL). HIV RNA was also analysed as a continuous variable after log10 transformation. HIV RNA was sampled within ± 3 months of questionnaire completion, and CD 4 cells within ± 6 months.
The following time-related variables (in years) were used: age at visit; age at diagnosis; time since diagnosis at visit; calendar year at visit; and time on ART at visit.
Statistical analyses
The Fisher exact test was performed for dichotomous variables, chi-square tests for non-ordered variables, and Mann–Whitney U tests for continuous variables. Associations for sexual satisfaction were tested in univariable models for all study patients and separately for women and men. Multivariable analysis using backward regression was performed for all study patients. Generalized estimation equation models were used to adjust for repeated answers and for within-patient correlations. Log link functions were used to represent relative risks (RR) with 95% confidence intervals (CI) and p-values. All tests were two-tailed and conducted at the 0.05 significance level. All analyses were performed using SAS software version 9.4 (SAS Institute Inc., Citation2017).
Missing values of variables in the database are presented as “not registered” in the explanation of the study population and are not included in the univariable analysis. In the multivariable analyses, 597 health questionnaires were excluded since at least one variable was missing.
Ethical considerations
All patients in the study had been informed about the InfCareHIV registry and gave their consent to be registered. The Regional Ethical Review Board in Gothenburg, Sweden approved the study (2016, Dnr: 293-16). The study was conducted in accordance with the Declaration of Helsinki (World Medical Association (WMA), Citation2019).
Results
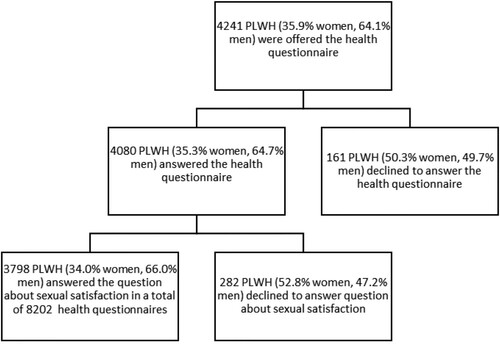
During 2011–2016, 7998 individuals were registered in InfCareHIV. The health questionnaire was offered annually to patients as part of regular patient consultations at the clinics that had implemented the health questionnaire. A total of 4241 patients were offered the health questionnaire of which 161 (3.8%) declined to answer it. Of the 4080 patients answering the questionnaire, 3798 answered the question about sexual satisfaction in a total of 8202 questionnaires (). Each individual patient included had on average responded twice to the questionnaire (range 1–7 times). The study sample included all those who were offered and completed health questionnaires according to the above criteria (n = 3798) and corresponded to 47.5% of the total Swedish InfCareHIV cohort during this period. The study population was representative of the national cohort except for an underrepresentation of women (34.0% vs 41.2%, p < 0.0001) and people born abroad (54.2% vs 70.8%, p < 0.0001). There was also an underrepresentation of patients with heterosexual mode of transmission (Supplementary Table 1).
presents the characteristics of the study population at first visit. The men included were older than the women (48.5 vs 42.1 years). Of all PLWH answering the questionnaire 45.8% were from Sweden, 29.8% from Africa, 11.3% from Asia, 8.1% from the rest of Europe and 5% from other continents. Most of the included women, 79.5%, were born abroad, where 54% originated from Africa. 41.2% of the men were born abroad where Africa was the most common continent (18%).
Table 1. Characteristics of the study population and the distribution of answers regarding self-reported sexual satisfaction at first visit.
Of the total study population, 66.7% reported sexual satisfaction. There was a significant difference between women and men, with 72% of women reporting sexual satisfaction compared to 64% of men (p < 0.0001) ().
Table 2. Univariable analysis of estimated levels of self-reported sexual satisfaction.
Patients with heterosexual contact as mode of HIV transmission were more likely to report sexual satisfaction than those with homosexual/bisexual contact as mode of transmission (RR = 1.10, 95% CI: 1.05–1.15, p < 0.0001). Individuals with intravenous drug use as mode of HIV transmission were less likely to report sexual satisfaction than those with heterosexual contact (RR = 0.83, 95% CI: 0.76–0.92, p = 0.0002). People born abroad were more likely to report sexual satisfaction than people born in Sweden (RR = 1.07, 95% CI: 1.03–1.12, p = 0.0006) (). There were no differences in self-reported sexual satisfaction between individuals who had been on ART > 6 months with HIV RNA < 50 copies/mL and those with HIV RNA ≥ 50 copies/mL ().
Table 3. Univariable analysis of relative risks (RR) of sexual satisfaction.
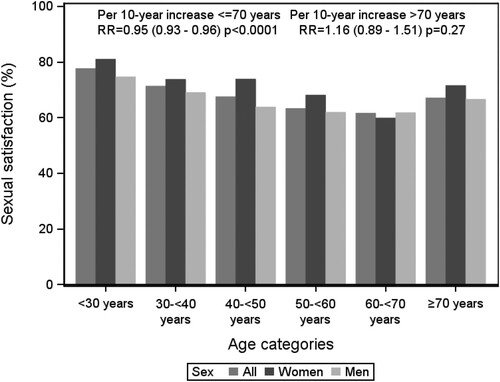
In the univariable analysis, sexual satisfaction was significantly positively associated with being on ART > 6 months compared to not being on ART (RR=1.06, 95% CI: 1.01–1.11, p = 0.032). However, every additional 5 years on ART was significantly negatively associated with sexual satisfaction (RR = 0.97, 95% CI: 0.96–0.99, p = 0.0009). A significant association between self-reported sexual satisfaction and age at visit was found, with 5% less chance of reporting sexual satisfaction for every 10 years’ increase until the age of 70 (RR = 0.95, 95% CI: 0.93–0.96, p < 0.0001.) After age 70 sexual satisfaction increased, but not significantly (p = 0.27) ().
Overall, the probability of reporting sexual satisfaction increased by 4% for every calendar year (RR = 1.04, 95% CI: 1.03–1.05, p < 0.001), (). All variables that were significant for the total population were also significant for women except intravenous drug use versus heterosexual contact as mode of transmission, country of birth, HIV RNA among all individuals (by 1 log10 increase), CD-4 nadir, time since diagnosis, and ART duration (). All variables that were significant for the total population were also significant for men, except heterosexual contact vs homosexual/bisexual contact as mode of transmission, country of birth, on ART > 6 months, CD-4 cell account, and CD-4 nadir ().
Figure 3. Self-reported sexual satisfaction in study group (all), women and men over time in calendar years.
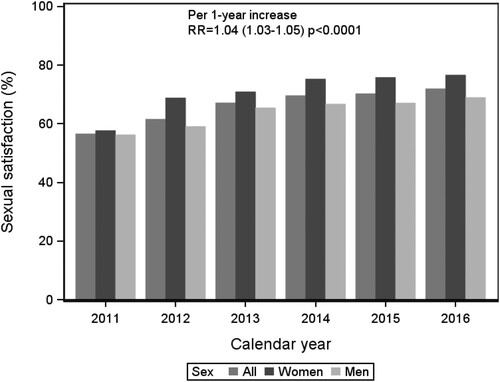
In the multivariable analysis, the difference between women and men in self-reported sexual satisfaction was still significant (women vs men RR = 1.09, 95% CI: 1.05–1.14, p < 0.0001). The negative associations of lower probability of self-reported sexual satisfaction with older age at visit ≤ 70 years (p = 0.0012), and with longer time on ART also remained significant (p = 0.0042). The yearly increase in satisfaction was also still significant (RR = 1.04, 95% CI: 1.03–1.05, p < 0.0001) ().
Table 4. Multivariable analysis of associations between sexual satisfaction and selected variables for all patients.
Discussion
This register-based study of more than 8000 questionnaires answered by almost 4000 PLWH is, to our knowledge, the largest study on self-reported sexual satisfaction in PLWH in Sweden. Two-thirds (67%) of the included patients reported sexual satisfaction, defined as being satisfied or very satisfied with their sexual life. Compared with earlier international studies assessing sexual satisfaction in PLWH, this is one of the highest levels reported (Inoue et al., Citation2004; Peyre et al., Citation2019; Rojas Castro et al., Citation2010) except for a study in PLWH in Romania reporting 68% with sexual satisfaction (Lazăr et al., Citation2014). However, these studies all assessed sexual satisfaction differently and comparisons to our study should be made cautiously. A smaller study (n = 1096) in PLWH in Sweden, showed that 51% reported sexual satisfaction (Schönnesson et al., Citation2018). That study population differed from ours in having a higher ratio of men to women, different HIV transmission routes, higher mean age, and fewer patients born abroad. This might explain the higher levels of sexual satisfaction in our study since we found that sexual satisfaction declined with older age and women were more satisfied than men. Data on sexual satisfaction in the general population in Sweden from 1990s shows that 54% (n = 1461) of the men and 56% (n = 1277) women reported being satisfied or very satisfied with their sexual life (Lewin & Fugl-Meyer, Citation1998). For individuals with a chronic disease, numbers were lower, 48% (n = 293) in women and 52% (n = 283) in men (Lewin & Fugl-Meyer, Citation1998). This study used the same questions about sexual satisfaction and even if the populations differ, it is an indicator that the levels of sexual satisfaction in PLWH in Sweden is high. The difference in sexual satisfaction between women and men in our study (72% vs 64%) was also found in the study of PLWH in Sweden by Schönnesson et al. (Citation2018), in which almost 50% (n = 762) of men and 44% (n = 320) of women reported sexual dissatisfaction. It is known that women and men may assess sexual satisfaction differently (Holmberg & Blair, Citation2009). One factor that might explain the differences in sexual satisfaction between men and women living with HIV is the importance of being in a relationship (Bourne et al., Citation2013; Carter et al., Citation2018). We did not have data on respondents’ relationship status, such as whether they had a stable partner, but a Swedish study of PLWH showed that 62% of the HIV-positive women reported being in a relationship compared with 55% of the men (Schönnesson et al., Citation2018). Further studies investigating factors that are associated with sexual satisfaction such as relationship status or physical and mental health are necessary.
We found no differences in reports of sexual satisfaction between PLWH who had been on ART > 6 months and were virally suppressed compared to those with HIV RNA ≥ 50 copies/mL. Our hypothesis that suppressed plasma HIV RNA (making it impossible to transmit HIV sexually) would be associated with more self-reported sexual satisfaction was based on the results of a qualitative study of women living with HIV in Sweden that described how fear of transmitting HIV negatively affected their sex lives (Carlsson-Lalloo et al., Citation2018). However, sexual satisfaction in PLWH seems to be more complex. Having a suppressed viral load seems to be an insufficient predictor of sexual satisfaction (Bucciardini et al., Citation2014). We observed in our study that a longer time on ART and a higher age when responding to the questionnaire were associated with lower levels of sexual satisfaction. This association between sexual satisfaction and age in PLWH has been previously reported (Bucciardini et al., Citation2014; Rojas Castro et al., Citation2010). It is therefore important for health care providers to discuss sexuality with PLWH regardless of their age.
Our national cohort study shows that the participants’ self-reported sexual satisfaction increased yearly from 2011 to 2016. There are several factors that may have positively affected the sexual life of PLWH during this period. As in most countries, initiating ART in all eligible patients regardless of CD4+ (Eriksen et al., Citation2017;) was recommended in accordance with research results (Lundgren et al., Citation2015). During this time the Swedish requirement that HIV status to be disclosed to sexual partners was also revised due to new evidence that there is negligible risk of sexual HIV transmission in patients with an undetectable viral load (plasma HIV RNA < 20 copies/mL) (Albert et al., Citation2014). This change eased legal restraints by removing the duty to inform sexual partners from individuals who fulfilled the treatment requirements for viral suppression and also signalled an important shift away from considering HIV transmission a criminal act. The evidence of no possible risk of sexual HIV transmission from persons with a suppressed viral load while on ART is now solid (Rodger et al., Citation2019), and it is important to continue to spread the message that U = U (undetectable = untransmittable) to people living with HIV and to the public.
It seems to be difficult for health professionals to talk about issues related to sexuality (Saunamäki & Engström, Citation2014). A standardized instrument that includes sexual satisfaction may facilitate conversations about sexuality, and PROs can be used to initiate and support interventions to ensure optimal HIV care and promote well-being and health. The yearly increase in sexual satisfaction seen in our study could thus be attributed to the use of the health questionnaire and the interventions that followed. In the same health questionnaire, there are also others PROs such as self-reported physical satisfaction and psychological well-being. The impact of these PRO must also be examined in future studies to better explain the quality of life for PLWH and the association to sexual satisfaction.
Methodological limitations
People can assess sexual satisfaction differently, and sexual satisfaction seems to be complex as it can be influenced by psychological health, physical health, and other factors (Bova & Durante, Citation2003; Luzi et al., Citation2009). This study covers only a limited number of sociodemographic and psychosocial variables that may affect sexuality. The registry also only records individuals as women or men and allows no other gender identities. In Sweden more than 1% of PLWH identify as neither women nor men (Public Health Agency of Sweden, Citation2015). People who make use of health care services and agree to answer a health questionnaire might also be those who are most satisfied with their general well-being, and consequently also with their sexual life.
Another limitation is that not all clinics have implemented the health questionnaire in routine care. However, the few clinics that have not done so care for less than 10% of all people living with HIV in Sweden and the questionnaire reached almost 50% of the total population of PLWH in Sweden during this period, and very few of those who were offered the questionnaire declined to complete it (3.8%).
Conclusions
This large cohort study on sexuality as a PRO demonstrates high levels of self-reported sexual satisfaction among PLWH in Sweden, with the positive trend of a yearly increase in satisfaction. This increase may be a result of greater knowledge about HIV transmission risks and the concomitant revision of legal restrictions concerning the obligation in Sweden to inform a sexual partner about an HIV diagnosis. It may also be attributable to interventions prompted by using the health questionnaire. Being or not being virally suppressed on ART was not a predictor of sexual satisfaction. Instead, younger age had a positive influence on sexual satisfaction, and longer time on ART was negatively associated with sexual satisfaction.
The finding that women were more satisfied with their sex life than men needs further study, for example, concerning the importance of relationship status. We suggest the use of PROs such as a health questionnaire or other instruments to facilitate conversations with patients about sexual satisfaction and HIV transmission risks. The use of PROs on subjects such as sexual satisfaction can also initiate interventions to support health and well-being for PLWH.
Supplemental Material
Download MS Word (15 KB)Acknowledgements
We thank Aldina Pivodic at Statistiska Konsultgruppen in Gothenburg for performing the statistical analysis.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Albert, J., Berglund, T., Gisslén, M., Gröön, P., Sönnerborg, A., Tegnell, A., Alexandersson, A., Berggren, I., Blaxhult, A., Brytting, M., Carlander, C., Carlson, J., Flamholc, L., Follin, P., Haggar, A., Hansdotter, F., Josephson, F., Karlström, O., Liljeros, F., Navér, L., … Widgren, K. (2014). Risk of HIV transmission from patients on antiretroviral therapy: A position statement from the Public Health Agency of Sweden and the Swedish Reference Group for Antiviral Therapy. Scandinavian Journal of Infectious Diseases, 46(10), 673–677. https://doi.org/https://doi.org/10.3109/00365548.2014.926565
- Bourne, A., Hammond, G., Hickson, F., Reid, D., Schmidt, A. J., & Weatherburn, P. (2013). What constitutes the best sex life for gay and bisexual men? Implications for HIV prevention. BMC Public Health, 13(1), 1083–1083. https://doi.org/https://doi.org/10.1186/1471-2458-13-1083
- Bova, C., & Durante, A. (2003). Sexual functioning among HIV-infected women. AIDS Patient Care and STDs, 17(2), 75–83. https://doi.org/https://doi.org/10.1089/108729103321150809
- Bucciardini, R., Pugliese, K., Weimer, L., Digregorio, M., Fragola, V., Mancini, M., Maroccia, Z., Ladisa, N., Francisci, D., Bellagamba, R., Degli Antoni, A., Guaraldi, G., Cirioni, O., Ortu, F., Parruti, G., Mannazzu, M., Libertone, R., Donnini, S., & Floridia, M. (2014). Relationship between health-related quality of life measures and high HIV viral load in HIV-infected triple-class-experienced patients. HIV Clinical Trials, 15(4), 176–183. https://doi.org/https://doi.org/10.1310/hct1504-176
- Carlsson-Lalloo, E., Berg, M., Mellgren, A., & Rusner, M. (2018). Sexuality and childbearing as it is experienced by women living with HIV in Sweden: A lifeworld phenomenological study. International Journal of Qualitative Studies on Health and Well-Being, 13(1), 1. https://doi.org/https://doi.org/10.1080/17482631.2018.1487760
- Carter, A., Greene, S., Money, D., Sanchez, M., Webster, K., Nicholson, V., Brotto, L. A., Hankins, C., Kestler, M., Pick, N., Salters, K., Proulx-Boucher, K., O’Brien, N., Patterson, S., de Pokomandy, A., Loutfy, M., Kaida, A., & Kaida, A. (2018). Supporting the sexual rights of women living with HIV: A critical analysis of sexual satisfaction and pleasure across five relationship types. The Journal of Sex Research, 55(9), 1134–1154. https://doi.org/https://doi.org/10.1080/00224499.2018.1440370
- Eriksen, J., Albert, J., Blaxhult, A., Carlander, C., Flamholc, L., Gisslén, M., Josephson, F., Karlström, O., Navér, L., Svedhem, V., Yilmaz, A., & Sonnerborg, A. (2017). Antiretroviral treatment for HIV infection: Swedish recommendations 2016. Infectious Diseases, 49(1), 1–34. https://doi.org/https://doi.org/10.1080/23744235.2016.1247495
- Fugl-Meyer, A. R., Bränholm, I.-B., & Fugl-Meyer, K. S. (1991). Happiness and domain: Specific life satisfaction in adult northern Swedes. Clinical Rehabilitation, 5(1), 25–33. https://doi.org/https://doi.org/10.1177/026921559100500105
- Holmberg, D., & Blair, K. L. (2009). Sexual desire, communication, satisfaction, and preferences of men and women in same-sex versus mixed-sex relationships. Journal of Sex Research, 46(1), 57–66. https://doi.org/https://doi.org/10.1080/00224490802645294
- Inoue, Y., Yamazaki, Y., Seki, Y., Wakabayashi, C., & Kihara, M. (2004). Sexual activities and social relationships of people with HIV in Japan. AIDS Care, 16(3), 349–362. https://doi.org/https://doi.org/10.1080/09540120410001665358
- Kall, M., Marcellin, F., Harding, R., Lazarus, JV., & Carrieri, P. (2020). Patient-reported outcomes to enhance person-centred HIV care. The Lancet HIV, 7(1), e59–e68. https://doi.org/https://doi.org/10.1016/S2352-3018(19)30345-5
- Lawrance, K., & Byers, E. S. (1995). Sexual satisfaction in long-term heterosexual relationships: The interpersonal exchange model of sexual satisfaction. Personal Relationships, 2(4), 267–285. https://doi.org/https://doi.org/10.1111/j.1475-6811.1995.tb00092.x
- Lazăr, F., Verdeş, L., Henry, E., Fugon, L., Bernier, A., Otis, J., & Préau, M. (2014). Satisfaction with sexual life in people living with HIV in Romania, together with associated individual and social factors. AIDS Care, 26(Supp 1), S65–S69. https://doi.org/https://doi.org/10.1080/09540121.2014.906550
- Lazarus, J. V., Safreed-Harmon, K., Barton, S. E., Costagliola, D., Dedes, N., del Amo Valero, J., Gatell, J. M., Baptista-Leite, R., Mendão, L., Porter, K., Vella, S., & Rockstroh, J. K. (2016). Beyond viral suppression of HIV: The new quality of life frontier. BMC Medicine, 14(1), 94. https://doi.org/https://doi.org/10.1186/s12916-016-0640-4
- Lewin, B., & Fugl-Meyer, K. (1998). Sex i Sverige: om sexuallivet i Sverige 1996 [Sex in Sweden: About sexual life in Sweden 1996] (3rd ed.). Folkhälsoinstitutet.
- Lundgren, J., Babiker, A., Gordin, F., Emery, S., Grund, B., Sharma, S., Avihingsanon, A., Cooper, D., Fätkenheuer, G., Llibre, J., Molina, J.-M., Munderi, P., Schechter, M., Wood, R., Klingman, K., Collins, S., Lane, C., Phillips, A., & Neaton, J. (2015). Initiation of antiretroviral therapy in early asymptomatic HIV infection. New England Journal of Medicine, 373(9), 795–807. https://doi.org/https://doi.org/10.1056/NEJMoa1506816
- Luzi, K., Guaraldi, G., Murri, R., De Paola, M., Orlando, G., Squillace, N., & Martinez, E. (2009). Body image is a major determinant of sexual dysfunction in stable HIV-infected women. Antiviral Therapy, 14(1), 85–92.
- Mark, K. P., Herbenick, D., Fortenberry, J. D., Sanders, S., & Reece, M. (2013). A psychometric comparison of three scales and a single-item measure to assess sexual satisfaction. Journal of Sex Research, 51(2), 1–11. https://doi-org.ezproxy.ub.gu.se/https://doi.org/10.1080/00224499.2013.816261
- Marrone, G., Mellgren, Å, Eriksson, L. E., Svedhem, V., & De Socio, G. V. (2016). High concordance between self-reported adherence, treatment outcome and satisfaction with care using a nine-item health questionnaire in InfCareHIV. PLoS ONE, 11(6). https://doi.org/https://doi.org/10.1371/journal.pone.0156916
- Mellgren, Å, Eriksson, L. E., Reinius, M., Marrone, G., & Svedhem, V. (2020). Longitudinal trends and determinants of patient-reported side effects on ART–A Swedish national registry study. PLoS ONE, 15(12), Article e0242710. https://doi.org/https://doi.org/10.1371/journal.pone.0242710
- Nakagawa, F., Lodwick, R. K., Smith, C. J., Smith, R., Cambiano, V., Lundgren, J. D., Delpech, V., & Phillips, A. N. (2012). Projected life expectancy of people with HIV according to timing of diagnosis. AIDS, 26(3), 335–343. https://doi.org/https://doi.org/10.1097/QAD.0b013e32834dcec9
- Peyre, M., Gauchet, A., Bissuel, F., Blanc, M., Boibieux, A., Cotte, L., Forestier E., Janssen C., Legout L., & Epaulard, O. (2019). Satisfaction with sexual life in people living with HIV/AIDS: The persistent weight of the fear of transmission. AIDS Care, 31(6), 681–686. https://doi.org/https://doi.org/10.1080/09540121.2018.1537465
- Public Health Agency of Sweden. (2015). Att leva med hiv i Sverige- En studie om livskvalitet hos personer som lever med hiv [Living with HIV in Sweden: A study on quality of life for people living with HIV]. Folkhälsomyndigheten.
- Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., Degen, O., … Janeiro, N. (2019). Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. The Lancet, 393(10189), 2428–2438. https://doi.org/https://doi.org/10.1016/S0140-6736(19)30418-0
- Rojas Castro, D., Le Gall, J. M., Andreo, C., & Spire, B. (2010). Stigma, discrimination, and sexual (dis)satisfaction among people living with HIV: Results from the “AIDES et toi” survey. AIDS Care, 9th International Conference Special Issue Gaborone, Botswana, 22(8), 961–969. https://doi.org/https://doi.org/10.1080/09540121003758614
- SAS Institute Inc. (2017). Retrieved September 1, 2019, from https://www.sas.com/en_us/home.html
- Saunamäki, N., & Engström, M. (2014). Registered nurses’ reflections on discussing sexuality with patients: Responsibilities, doubts and fears. Journal of Clinical Nursing, 23(3–4), 531–540. https://doi.org/https://doi.org/10.1111/jocn.12155
- Schönnesson, L., Zeluf, G., Garcia-Huidobro, D., Ross, M., Eriksson, L., & Ekström, A. (2018). Sexual (dis)satisfaction and its contributors among people living with HIV infection in Sweden. Archives of Sexual Behavior, 47(7), 2007–2026. https://doi.org/https://doi.org/10.1007/s10508-017-1106-2
- Vernazza, P., Hirschel, B., Bernasconi, E., & Flepp, M. (2008). HIV-infizierte Menschen ohne andere STD sind unter wirksamer antiretroviraler Therapie sexuell nicht infektiös [HIV-infected people free of other STDs are sexually not infectious on effective antiretroviral therapy]. Schweizerische Ärztezeitung, 89(05), 165–169. https://doi.org/https://doi.org/10.4414/saez.2008.13252
- World Medical Association (WMA). (2019). Declaration of Helsinki. Retrieved September 1, 2019, from https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- Zeluf-Andersson, G., Eriksson, L. E., Schönnesson, L. N., Höijer, J., Månehall, P., & Ekström, A. M. (2019). Beyond viral suppression: The quality of life of people living with HIV in Sweden. AIDS Care, 31(4), 403–412. https://doi.org/https://doi.org/10.1080/09540121.2018.1545990