ABSTRACT
The number of older people living with HIV (OPLHIV) is increasing worldwide. However, little is known about the factors that better predict their health-related quality of life (HRQoL). We administered the validated WHOQoL-HIV BREF questionnaire to 247 Spanish OPLHIV (192 men and 55 women). In addition to the six domains of the questionnaire, we constructed a seventh domain as theaverage of punctuations of all domains. Multivariable Poisson regression models with robust estimates by sex were constructed for the seven domains (14 in total). The best-subset selection method together with Mallow's Cp metric was used to select the model factors. The percentage of variability explained by Poisson models ranged from15-38% for men and 29-70% for women. The analysis showed that women were most affected by ageing (four domains), mobility impairments (five domains), and mental disorders (five domains). The factors with the greatest negative influence on men were heterosexuality (six domains), mental disorders (six domains), being single (five domains), and poverty risk (three domains). Physical activity was found to improve HRQoL in both men (six domains) and women (four domains). Future OPLHIV programmes would benefit from considering sex specific HRQoL factors. This could also improve the cost-effectiveness of interventions.
SDG KEYWORDS:
1. Introduction
Modern antiretroviral therapies (ART) have significantly increased the life expectancy of people infected with human immunodeficiency virus (HIV). However, long-term HIV infection is associated with premature ageing of the immune system and the ocurrence of comorbidities and geriatric syndromes at a young age (Guaraldi et al., Citation2011; Pond et al., Citation2021). In 2016, the number of people living with HIV (PLHIV) ≥ 50 years (henceforth referred to as "older people living with HIV (OPLHIV)") in Western Europe and North America was estimated at 880,000, representing 41% of the total number of PLHIV in these regions (Autenrieth et al., Citation2018; Hsieh et al., Citation2022). In Spain, approximately 53% of all PLHIV are OPLHIV (CNE et al., Citation2021). Furthermore, the number of OPLHIV worldwide is expected to increase significantly in the coming decades (Autenrieth et al., Citation2018; Hsieh et al., Citation2022).
Several studies have confirmed that OPLHIV have a lower health-related quality of life (HRQoL) than the general older population and younger people with the infection (Monteiro et al., Citation2016; Morales et al., Citation2022). In addition to clinical factors, the HRQoL of OPLHIV is significantly influenced by social and structural factors that lead to high levels of loneliness, depression, and financial stress (Nobre et al., Citation2017; Vincent et al., Citation2017). Additionally, health systems are generally unprepared to meet the needs of OPLHIV, as they tend to provide fragmented care and fail to integrate age and HIV-related services (Kiplagat et al., Citation2022).
The Spanish Plan for the Prevention and Control of HIV and other Sexually Transmitted Infections 2021–2030 gives high priority to the identification of factors that may influence long-term HIV survival and HRQoL. In Spain, there is currently a lack of studies focusing specifically on OPLHIV (Bruguera et al., Citation2024; Fuster-Ruiz de Apodaca et al., Citation2019; Nuño et al., Citation2024). It is therefore important to understand the factors that can predict the HRQoL of OPLHIV in order to support the development and implementation of future strategies at national, regional, and local levels. This process must also include a perspective that takes sex differences into account. Numerous studies have found significant differences between men and women in terms of HIV progression and HRQoL. Compared to women, men who have sex with men have a lower risk of all-cause mortality, disease progression to acquired immunodeficiency syndrome, and virological failure (Li et al., Citation2020). Similarly, older women living with HIV have poorer physical function and HRQoL despite having better immunological recovery and less cardiovascular disease and risk factors than their male counterparts (Brañas et al., Citation2020). The specific needs, differences, and experiences of men and women living with HIV have, been underrepresented in HIV research to date (Blondeel et al., Citation2016; Loutfy et al., Citation2013). In this study, we examine the demographic, socio-economic, lifestyle, and clinical factors that influence HRQoL in Spanish older men and women living with HIV.
2. Methods
2.1. Participants
A total of 247 OPLHIV living in Spain took part in the study. The mean age of the participants was 56.9 (SD = 5.1) years, 89% (N = 219) were born in Spain, and the average time since HIV diagnosis was 21.2 (SD = 10.5) years. Fifty-seven percent of participants (N = 138) described themselves as homosexual and 41% (N = 101) were partnered. Almost all participants (99%) were receiving ART and 97% reported undetectable viral loads. Self-reported mobility impairments (21%) and mental disorders (20%) were the most common health conditions. A third of participants (36%) were at risk of poverty, and there were notable differences between men and women in terms of sexual orientation, clinical condition, and socio-economic status. A detailed description of participant selection and characteristics is found in Nuño et al. (Citation2024).
2.2. Instruments
We used the validated Spanish version of the standardised WHOQoL-HIV BREF questionnaire (Fuster-Ruiz de Apodaca et al., Citation2019) to assess self-reported HRQoL. The questionnaire includes six domains: physical health (henceforth referred to as “physical”), psychological health (henceforth referred to as “psychological”), level of independence (henceforth referred to as “independence”), social relationships (henceforth referred to as “relationships”), environmental health (henceforth referred to as “environment”), and spirituality/personal beliefs (henceforth referred to as “beliefs”). Additionally, we calculated a seventh domain as the average of punctuation across the original six WHOQoL-HIV BREF questionnaire domains (henceforth referred to as “overall HRQoL” domain). Participants also provided self-reported demographic, socio-economic, lifestyle, and clinical information (e.g., viral load, comorbidities). The full list of comorbidities (reported in the previous year or chronic) included cardiovascular disease, stroke, diabetes mellitus, respiratory diseases (e.g., pulmonary embolism, coronary angioplasty), hypertension, cancer/tumor, sexually transmitted infection, and dementia/Alzheimer. We assessed the risk of poverty of participants following the Europe 2020 guidelines (Eurostat, Citation2018). A detailed description of the instruments and their psychometric properties can be found in Nuño et al. (Nuño et al., Citation2024).
2.3. Data collection and analysis
The data was collected between February and October 2022 using the open-source app Kobo Toolbox (KoBo, Inc.), and the statistical analysis was performed using R 3.6 (R Project for statistical computing).
Scores on the WHOQoL-HIV BREF questionnaire range from 4 to 20 points for each domain, with higher scores indicating better HRQoL. Variables with a variance of zero or close to zero and non-response percentages of more than 10% were excluded from the analysis. The continuous variable age was converted into a binary variable, using 55 years as the cut-off value (Catalan et al., Citation2017). In addition, the continuous variable years since HIV diagnosis was converted into a binary variable using the year 1997 (when modern ART became available in Spain) as the cut-off point.
We constructed multivariable Poisson regression models with robust estimates to determine which factors had a greater impact on HRQoL by sex. We first identified potential variables to include in the multivariable Poisson models by running univariable Poisson regressions with robust estimates for each HRQoL domain by sex. Variables with p-values <0.200 were included in the multivariable models. We used the best-subset selection method together with Mallow's Cp metric to select the most appropiate combination of variables that provides a balance between simplicity and accuracy. Unlike other common model selection strategies, such as stepwise regression, the best-subset selection method identifies combinations of variables without eliminating any of them during the process (Chowdhury & Turin, Citation2020).
The Akaike information criterion was used to examine the following interactions in multivariable models: unwanted loneliness and mental disorders (Greene et al., Citation2018), poverty risk and HIV infection pahtways (Pellowski et al., Citation2013), poverty risk and sexual orientation (Pellowski et al., Citation2013), and physical impairments/other comorbidities and years since HIV diagnosis (Guaraldi et al., Citation2011). In addition, multicollinearity was found for variance inflation factors ≥5. Model fits were assessed using the deviance test and Pearson goodness-of-fit test, as well as graphical diagnosis using residuals versus fitted values and Q-Q plots. We estimated the percentage of variability explained by each multivariable model using McFadden's pseudo R2.
3. Results
3.1. Univariable analysis
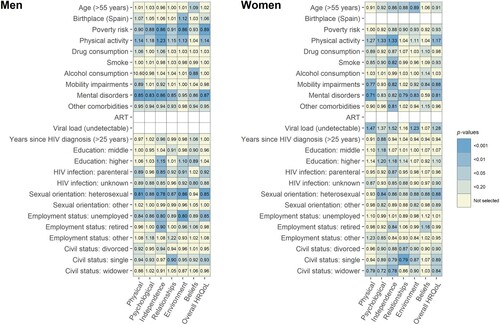
We excluded the variables ART (both men and women), place of birth (women), and viral load (men) from the analysis due to zero or near-zero variance. There were no variables for which the percentage of non-responses exceeded 10%. shows the rate ratios and p-values from the univariable Poisson analysis by sex. The tables with the complete univariable Poisson regressions can be found in supplemental material I.
The univariable analysis yielded marked differences between men and women. In women >55 years of age, a decline in scores was observed in the independence (RR: 0.86; p: 0.020), relationships (RR: 0.88; p: 0.038), and environment (RR: 0.89; p: 0.009) domains. In men, the correlation between age and HRQoL was positive in the beliefs domain (RR: 1.09; p: 0.043). Men born in Spain achieved higher scores in the environment domain (RR: 1.12; p: 0.007). Risk of poverty had a negative effect on men's HRQoL scores in the physical (RR: 0.90; p: 0.011), psychological (RR: 0.88; p: 0.002), independence (RR: 0.86; p: < 0.001), relationships (RR: 0.91; p: 0.025), environment (RR: 0.86; p: < 0.001), and overall HRQoL (RR: 0.89; p: < 0.001) domains. However, this factor was not significant for women in any domain.
Regarding lifestyle characteristics, physical activity was associated with positive HRQoL scores in both men (physical (RR: 1.14; p: 0.009), psychological (RR: 1.18; p: 0.010), independence (RR: 1.23; p: < 0.001), relationships (RR: 1.15; p: 0.011), environment (RR: 1.13; p: 0.002), and overall HRQoL (RR: 1.14; p: 0.002) domains) and women (physical (RR: 1.27; p: 0.022), psychological (RR: 1.33; p: 0.002), independence (RR: 1.33; p: < 0.001), and overall HRQoL (RR: 1.17; p: 0.006) domains). Smoking was negatively associated with independence scores in women (RR: 0.82; p: 0.005) , and alcohol consumption was associated with lower belief scores in men (RR: 0.88; p: 0.008).
Mobility impairments had a negative effect in four domains for women (physical (RR: 0.77; p: 0.001), independence (RR: 0.82; p: 0.006), beliefs (RR: 0.84; p: 0.018), and overall HRQoL (RR: 0.88; p: 0.006) domains), while for men this factor correlated only with the physical domain (RR: 0.89; p: 0.028). Similarly, self-reported mental disorders affected both men (physical (RR: 0.85; p: < 0.001), psychological (RR: 0.83; p: < 0.001), independence (RR: 0.86; p: < 0.001), relationships (RR: 0.85; p: 0.001), beliefs (RR: 0.86; p: 0.015), and overall HRQoL (RR: 0.87; p: < 0.001) domains) and women (physical (RR: 0.71; p: < 0.001), independence (RR: 0.82; p: 0.035), relationships (RR: 0.79; p: 0.008), environment (RR: 0.83; p: 0.001), and overall HRQoL (RR: 0.81; p: 0.001) domains). However, having other comorbidities only had a negative effect on the independence of women (RR: 0.81; p: 0.001). Undetectable viral loads were positively associated in women with the physical (RR: 1.47; p: 0.001), independence (RR: 1.52; p: 0.026), environment (RR: 1.23; p: 0.003), and overall HRQoL (RR: 1.28: p: 0.010) domains. Likewise, women with an HIV diagnosis after 1997 had lower psychological scores (RR: 0.88; p: 0.042) while this factor was not significant for men.
Compared to women with basic education, both middle-educated (RR: 1.18; p: 0.045) and higher-educated (RR: 1.20; p: 0.021) women scored higher in the psychological domain. In addition, higher-educated women achieved higher scores in the independence domain (RR: 1.18; p: 0.037). In men, the correlation between higher-education and HRQoL was positive in the independence (RR: 1.15; p: 0.001) and environment (RR: 1.10; p: 0.019) domains, and neative in the beliefs domain (RR: 0.89; p: 0.018) compared to men with only basic education.
The route of HIV infection was associated with lower HRQoL scores in men. Men who had acquired HIV through parenteral transmission scored lower in the physical (RR: 0.89; p: 0.010), independence (RR: 0.85; p: 0.001), environment (RR: 0.91; p: 0.015), and overall HRQoL (RR: 0.92; p: 0.034) domains than men who had acquired HIV through sexual intercourse. The lack of knowledge about the route of HIV infection had a negative effect on men's beliefs (RR: 0.80; p: 0.012). Among women, those who had acquired HIV through parenteral transmission performed worse in the independence domain (RR: 0.87; p: 0.047). Heterosexuality was associated with poorer scores in both men (physical (RR: 0.81; p: < 0.001), psychological (RR: 0.88; p: 0.006), independence (RR: 0.78; p: < 0.001), relationships (RR: 0.87; p: 0.003), environment (RR: 0.86; p: < 0.001), and overall HRQoL (RR: 0.85; p: < 0.001) domains) and women (psychological (RR: 0.84; p: 0.007), independence (RR: 0.86; p: 0.037), environment (RR: 0.88; p: 0.026), beliefs (RR: 0.88; p: 0.014), and overall HRQoL (RR: 0.88; p: 0.001) domains).
HRQoL scores were negatively correlated with employment status, especially for men. Unemployed men scored worse than men who ere employed in the physical (RR: 0.84; p: 0.010) psychological (RR: 0.86; p: 0.045), independence (RR: 0.80; p: 0.002), environment (RR: 0.80; p: < 0.001), and overall HRQoL (RR: 0.85; p: 0.006) domains. Retired men scored worse in the independence domain (RR: 0.90; p: 0.004). The scores of retired women were negatively correlated with those of employed women in the independence (RR: 0.84; p: 0.026) and beliefs (RR: 1.16; p: 0.041) domains.
Civil status had an effect in both men and women. Divorced women scored worse than women who were partnered in the relationships domain (RR: 0.87; p: 0.044). The same correlation was observed for single women (independence (RR: 0.79; p: 0.026), relationships (RR: 0.79; p: < 0.001), environment (RR: 0.87; p: 0.034), and overall HRQoL (RR: 0.89; p: 0.019) domains) and widowed women (physical (RR: 0.79; p: 0.037), psychological (RR: 0.72; p: 0.025), independence (RR: 0.78; p: 0.004), and overall HRQoL (RR: 0.84; p: 0.046) domains). Single men also performed worse than partnered men in the relationships (RR: 0.90; p: 0.006) and overall HRQoL (RR: 0.93; p: 0.024) domains.
3.2. Multivariable analysis
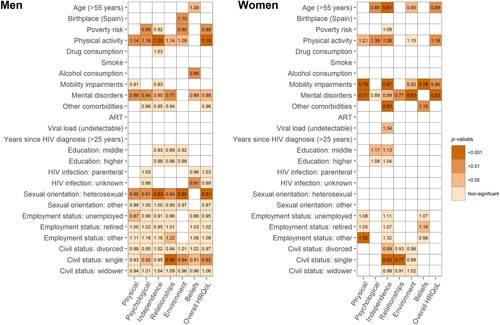
No variables were removed from the multivariable models due to collinearity. For men, we identified interactions between being single and mental disorders (psychological, relationships, and overall HRQoL domains) and between poverty risk and HIV infection pathways (psychological and overall HRQoL domains). No interactions were found between physical impairments/other comorbidities and years since HIV diagnosis or between poverty risk and sexual orientation in either men or women. Multivariable models did not show adjustment problems, and percentages of variability explained ranged from 15-38% for men and 29-70% for women. shows the rate ratios and p-values from the multivariable Poisson models by sex. The tables with the complete multivariable Poisson models and goodness-of-fit tests can be found in supplemental material II.
Women >55 years had lower HRQoL scores in the psychological (RR: 0.85; p: 0.007), independence (RR: 0.81; p: < 0.001), environment (RR: 0.90; p: 0.022), and overall HRQoL (RR: 0.89; p: 0.002) domains. Conversely, ageing was positively associated with men's beliefs (RR: 1.09; p: 0.042). Similar to the univariable analysis, men born in Spain performed better in the environment domain (RR: 1.10; p: 0.008). However, the risk of poverty had a negative impact on men in the psychological (RR: 0.86; p: 0.001), environment (RR: 0.90; p: 0.001), and overall HRQoL (RR: 0.89; p: 0.002) domains. No effect of this factor was observed in women.
Regarding lifestyle characteristics, physical activity was positively associated with HRQoL scores in both men (physical (RR: 1.14; p: 0.009), psychological (RR: 1.16; p: 0.006), independence (RR: 1.20; p: < 0.001), relationships (RR: 1.14; p: 0.016), environment (RR: 1.09; p: 0.010), and overall HRQoL (RR: 1.15; p: < 0.001) domains) and women (physical (RR: 1.21; p: 0.017), psychological (RR: 1.39; p: 0.001), independence (RR: 1.26; p: 0.002), and overall HRQoL (RR: 1.18; p: 0.002) domains). Similar to the univariable analysis, men's alcohol consumption remained negatively correlated with the beliefs domain (RR: 0.88; p: 0.004).
Women with mobility impairments performed worse in the physical (RR: 0.79; p: < 0.001), independence (RR: 0.87; p: < 0.001), environment (RR: 0.92; p: 0.043), beliefs (RR:0.78; p: < 0.001), and overall HRQoL (RR: 0.90; p: 0.003) domains. No effect of this factor was observed in men. Self-reported mental disorders affected both men (physical (RR: 0.88; p: 0.008), psychological (RR: 0.84; p: 0.006); independence (RR: 0.90; p: 0.014), relationships (RR: 0.77; p: 0.001), beliefs (RR: 0.89; p: 0.033), and overall HRQoL (RR: 0.88; p: 0.019) domains) and women (physical (RR: 0.71; p: < 0.001), independence (RR: 0.89; p: 0.012), relationships (RR: 0.77; p: 0.004), environment (RR: 0.83; p: < 0.001), and overall HRQoL (RR: 0.83; p: < 0.001) domains). Women with other comorbidities scored worse on independence (RR: 0.82; p: < 0.001) and better on beliefs (RR: 1.19; p: 0.009). Women with undetectable viral load performed better in the independence domain (RR: 1.34; p: 0.017). Women with an intermediate level of education performed better in the psychological (RR: 1.17; p: 0.019) and independence (RR: 1.13; p: 0.023) domains than women with a basic education. No effect of this factor was observed in men.
Only men were affected by the route of HIV infection and sexual orientation. Lack of knowledge about the route of HIV infection had a negative effect on men's beliefs (RR: 0.81; p: 0.007) compared with men who had acquired HIV through sexual intercourse. Heterosexual men had lower HRQoL scores than homosexual men in the physical (RR: 0.85; p: 0.002), psychological (RR: 0.81; p: 0.002), independence (RR: 0.83; p: < 0.001), relationships (RR: 0.84; p: 0.001), environment (RR: 0.85; p: < 0.001), and overall HRQoL (RR: 0.81; p: < 0.001) domains.
In terms of employment status, unemployed men scored lower in the physical domain (RR: 0.87; p: 0.020) compared to men who were employed. In contrast, the scores of women with other employment situations (e.g., informal jobs) and retired women were positively correlated with those of employed women in the physical (RR: 1.52; p: < 0.001) and beliefs (RR: 1.16; p: 0.043) domains. Civil status mainly affected men. Single men performed worse than partnered men in the psychological (RR: 0.92; p: 0.018), relationships (RR: 0.86; p: < 0.001), environment (RR: 0.94; p: 0.007), beliefs (RR: 0.91; p: 0.046), and overall HRQoL (RR: 0.92; p: 0.006) domains. The scores of single women were negatively correlated with those of partnered women in the independence (RR: 0.82; p: < 0.001) and relationships (RR: 0.77; p: < 0.001) domains. The same correlation was observed between divorced and partnered women in the independence domain (RR: 0.89; p: 0.011).
4. Discussion
Based on data from a cross-sectional study with 247 Spanish older people living with HIV (OPLHIV), we classified health-related quality of life (HRQoL) scores and identified factors influencing HRQoL by sex in seven domains. The results of the multivariable analysis yielded marked differences between men and women, with clinical factors being more important for women, and demographic and socio-economic factors being more significant for men.
Being a woman >55 years and having mobility impairments were negatively correlated with HRQoL in four and five domains respectively, whereas this factor did not affect men. Recent studies describe that the physical function of women living with HIV declines faster with age in comparison with their male counterparts (Brañas et al., Citation2020).
We also found that mental disorders adversely affected men and women in six and five HRQoL domains respectively. These findings confirm that there is an urgent need to address the mental health needs of people living with HIV (PLHIV) (McMillan et al., Citation2018; Pond et al., Citation2021; Serrão et al., Citation2019). This issue is also a major concern in Spain. According to a study with 563 PLHIV, 52% of women and 39% of men reported psychological distress. Furthermore, psychological distress was directly associated with non-adherence to and non-use of combined antiretroviral therapy (ART) (Garriga et al., Citation2020). There is also evidence that the Spanish public healthcare system may not be adequately prepared to meet the mental health needs of both PLHIV and OPLHIV. In a recent study, 115 Spanish HIV physicians described that neuropsychiatric comorbidities were underdiagnosed (77%), patients underreported neuropsychiatric comorbidities (54%), and HIV physicians did not receive adequate training on detecting neuropsychiatric comorbidities (64%) (Pérez-Valero et al., Citation2022).
We also found that the HRQoL of men was adversely influenced by their sexual orientation, civil status, and socio-economic situation. Heterosexuality was associated with lower HRQoL scores than homosexuality in six domains, whereas this factor did not affect women. One reason for the stronger impact of sexual orientation on men could be the fact that homosexual men are more likely to develop resilience and acceptance strategies and biuld stronger community bonds (due to common interests and lifestyles) compared to heterosexual men (Liu et al., Citation2022; Skinta et al., Citation2014). Likewise, being men and single had a negative impact on HRQoL scores in five domains, while single women had lower HRQoL scores in only two domains. According to variousstudies, older men living with HIV are more likely han their female counterparts to suffer from symptoms of loneliness associated with fewer relationships and social interactions (Greene et al., Citation2018; Mazonson et al., Citation2021). Negative effects of poverty risk on men wereobserved in three domains, whilethis factor did not affect women.
Physical activity was the most important factor associated with improved HRQoL in both men (five domains) and women (four domains). Although there is evidence that PLHIV are less likely to adhere to physical activity recommendations compared to the general population, higher levels of physical activity are associated with better HRQoL (Martin et al., Citation2019). A recent scoping review found that the mental health and functional status of PLHIV was positively correlated with physical activity (Chetty et al., Citation2021). Likewise, a recent systematic review and meta-analysis also found that physical activity significantly improves walking ability in OPLHIV. However, this review could not confirm that physical activity was associated with significant improvements in HRQoL or depression (Shim & Noh, Citation2022).
Our findings are supported by similar studies in Spain and elsewhere. In Spain, in a sample of men and women living with HIV (no specific information on OPLHIV), Fumaz et al. found that poor physical health was negatively associated with economic worries (men), unemployment (men), insufficient psychological support (both men and women), fewer years since HIV diagnosis (women), low satisfaction with body image (men), and HIV-related stigma (both men and women). In addition, mentalhealth was negatively related to unemployment (men), drug use (men), being single (men), low CD4 cells (women), and low satisfaction with body image (women). Both men and women reported better physical and mental health when they were free of previous opportunistic infections (Fumaz et al., Citation2019). According to another Spanish study involving 1,060 PLHIV, OLPHIV had poorer physical health and similar mental health compared to their young counterparts. In OPLHIV, depressive symptoms and cognitive function correlated negatively with mental and physical health respectively. Conversely, physical health has been found to be improved by satisfaction with social roles. In the United Kingdom, Catalan et al. applied the WHOQoL-HIV BREF questionnaire in a sample of OPLHIV (not stratified by sex) and found that men who have sex with men had higher HRQoL than heterosexual men in one domain. In addition, HRQoL was higher in three domains in participants who were in a relationshipand employment positively influenced HRQoL in one domain (Catalan et al., Citation2017). Finally, in Portugal, Pereira et al. found in a sample of middle-aged PLHIV and OPLHIV that the main factors positively associated with HRQoL were being partnered (one domain), years of education (two domains), being employed (two domains), and ART status (two domains) (Pereira et al., Citation2014).
We identified some limitations in our study. First, due to the design, we were unable to determine how factors influence HRQoL over time. As the sample size was not stratified by age, we were also unable to differentiate how factors influence HRQoL in different age groups. Second, most of the data collected were demographic, socio-economic, and health-related. We believe that this partly explains why the variability explained by the belief domain models was low (15% for men and 29% for women). It is necessary to examine the factors that could explain the HRQoL in this area. HIV-related stigma is a potential factor that may influence OPLHIV beliefs. However, this dimension is not currently captured by the WHOQoL-HIV BREF questionnaire. We considered using an additional validated questionnaire to measure HIV-related stigma in the study, but it was ultimately not implemented due to logistical and time constraints. Future research should investigate the impact of HIV-related stigma on the HRQoL of OPLHIV.
To our knowledge, this is one of the few studies investigating the factors influencing the HRQoL of OPLHIV in Spain. Overall, our study helps to identify important needs of OPLHIV and highlights the need to adapt healthcare models to meet the aging needs of PLHIV. The Spanish healthcare system does not currently address the complexity and care needs of OPLHIV with comorbid conditions. It is, therefore, necessary to develop and implement people-centred strategies in the fight against HIV rthat have been shown to improve health outcomes and the effectiveness of treatment for other chronic diseases (Erlandson & Karris, Citation2019; Lazarus, Cascio, et al., Citation2023; Lazarus, Janamnuaysook, et al., Citation2023).
Furthermore, these approaches must recognise and prioritise biological, cultural, social and sex differences. This includes, for example, promoting equal participation of men and women living with HIV in clinical trials to ensure the efficacyand safety of medical treatments for both sexes or developing mental health strategies tailored to the specific needs of women living with HIV, as they generally have a high prevalence of physical and sexual abuse, caregiver stress, and increased internalised stigma (Waldron et al., Citation2021). All these changes should also have a structural background, including specific and continuous training of health professionals and the development of coordination protocols between primary and hospital care for the treatment and follow-up of the disease (De la Torre-Lima et al., Citation2023). Consequently, the development and implementation of people-centered strategies that take sex differences into account can help to comprehensively improve the HRQoL and well-being of Spanish OPLHIV.
5. Conclusion
Using the validated WHOQoL-HIV BREF questionnaire, we assessed demographic, socio-economic, lifestyle and clinical factors influencing the health-related quality of life (HRQoL) in 247 Spanish men and women ≥50 years living with HIV (192 men and 55 women). Women's HRQoL was more strongly affected by age, mobility impairments, and mental health disorders, while men's HRQoL was negatively affected by sexual orientation, civil status, poverty risk, and mental health disorders. Physical activity was the most important factor associated with improved HRQoL in both men and women. National, regional, and local HIV prevention and treatment organisations could benefit from considering these factors in future interventions. Indentifying specific factors that influence HRQoL by sex may contribute to the cost-effectiveness of interventions.
Ethics approval and consent to participate
Participation in this study was voluntary. Netither the researchers nor the participants received any compensation for their participation in the study. No personal data were collected in either the questionnaires or the consent forms, as some PLHIV in Spain refuse to publicly disclose their HIV serological status due to HIV-related stigma (Fuster-Ruiz de Apodaca et al., 2013). The ethics committee of La Princesa Hospital (Madrid) exempted the study from review. The study was conducted in accordance with the Declaration of Helsinki. All participants signed an informed consent form before completing the questionnaire.
Author contributions
NN and RP designed the study; NN and JSH collected data; NN, RP, and JSH were in charge of implementing the study; NN and AM provided with essential statistical advice. NN, AM, RP, and MC analysed and interpreted the data; NN wrote the first draft manuscript; RP, AM, SM, MC, and JSH interpreted the data, performed critical revisions of the manuscript and contributed to the writing; RP and SM provided administrative, technical and material support; NN and RP coordinated and supervised the study. All authors read and approved the final manuscript.
caic-2024-01-0011-File005
Download PDF (1.9 MB)caic-2024-01-0011-File004
Download PDF (357.4 KB)Acknowledgements
We would like to thank all participants for their contribution in the questionnaire. In addition, we also acknowledge gTt-VIH for their assistance in the implementation of the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The Spanish Ministry of Health legally owns the data of this study. Access to the database can be requested through the email address [email protected].
Additional information
Funding
References
- Autenrieth, C. S., Beck, E. J., Stelzle, D., Mallouris, C., Mahy, M., & Ghys, P. (2018). Global and regional trends of people living with HIV aged 50 and over: Estimates and projections for 2000–2020. PLoS One, 13(11), e0207005. https://doi.org/10.1371/journal.pone.0207005
- Blondeel, K., Say, L., Chou, D., Toskin, I., Khosla, R., Scolaro, E., & Temmerman, M. (2016, January 22). Evidence and knowledge gaps on the disease burden in sexual and gender minorities: A review of systematic reviews. International Journal for Equity in Health, 15, 16. https://doi.org/10.1186/s12939-016-0304-1
- Brañas, F., Sánchez-Conde, M., Carli, F., Menozzi, M., Raimondi, A., Milic, J., Franconi, J., Cuomo, G., Mussini, C., Moreno, S., & Guaraldi, G. (2020, March 1). Sex differences in people aging with HIV. Journal of Acquired Immune Deficiency Syndromes, 83(3), 284–291. https://doi.org/10.1097/QAI.0000000000002259
- Bruguera, A., Egea-Cortés, L., Mesías-Gazmuri, J., Palacio -Vieira, J., Forero, C. G., Miranda, C., Saumoy, M., Fernández, E., Navarro, G., Orti, A., Miró, J. M., Casabona, J., Reyes-Urueña, J., & Group, P. S. (2024, April 01). Predictors of poor health-related quality of life among people living with HIV aged ≥60 years in the PISCIS cohort: Findings from the Vive+ project. HIV Medicine, 25(4), 424–439. https://doi.org/10.1111/hiv.13590
- Catalan, J., Tuffrey, V., Ridge, D., Rosenfeld, D., & Team, H. (2017, April 11). What influences quality of life in older people living with HIV? AIDS Research and Therapy, 14(1), 22. https://doi.org/10.1186/s12981-017-0148-9
- Chetty, L., Cobbing, S., & Chetty, V. (2021). Physical activity and exercise for older people living with HIV: A scoping review. HIV/AIDS - Research and Palliative Care, 13, 1079–1090. https://doi.org/10.2147/HIV.S336886
- Chowdhury, M. Z. I., & Turin, T. C. (2020). Variable selection strategies and its importance in clinical prediction modelling. Family Medicine and Community Health, 8, e000262. https://doi.org/10.1136/fmch-2019-000262
- CNE, ISCII, & PNS. (2021). Encuesta Hospitalaria de pacientes con infección por el VIH. Resultados 2021. Análisis de la evolución 2006-2021. PNS. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/VIH/informes%20encuesta%20hospitalaria%20anteriores/Informe%20Encuesta%20hospitalaria_2006_2021_def.pdf
- De la Torre-Lima, J., Oteo, J. A., Pinilla, J., Mansilla, R., Zamora, C., Ayala Vargas, V., Morillo-Verdugo, R., Moreno, S., Fuster-Ruiz de Apodaca, M. J., Pérez-Molina, J. A., & Colom, J. (2023, December). Study on the approach to HIV: Health management and the healthcare process in Spain. Enfermedades Infecciosas y Microbiología Clínica, 41(10), 604–611. https://doi.org/10.1016/j.eimce.2022.12.008
- Erlandson, K. M., & Karris, M. Y. (2019, September 01). Hiv and aging: Reconsidering the approach to management of comorbidities. Infectious Disease Clinics of North America, 33(3), 769–786. https://doi.org/10.1016/j.idc.2019.04.005
- Eurostat. (2018). Glossary: EU 2020 Strategy. Retrieved May 21, from https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Glossary:EU_2020_Strategy
- Fumaz, C. R., Larrañaga-Eguilegor, M., Mayordomo-López, S., Gómez-Martínez, S., González-García, M., Ornellas, A., Fuster Ruiz de Apodaca, M. J., Remor, E., & Ballester-Arnal, R. (2019, December). Health-related quality of life of people living with HIV infection in Spain: A gender perspective. AIDS Care, 31(12), 1509–1517. https://doi.org/10.1080/09540121.2019.1597959
- Fuster-Ruiz de Apodaca, M. J., Laguía, A., Safreed-Harmon, K., Lazarus, J. V., Cenoz, S., & Del Amo, J. (2019, August 19). Assessing quality of life in people with HIV in Spain: Psychometric testing of the Spanish version of WHOQOL-HIV-BREF. Health Quality Life Outcomes, 17(1), 144. https://doi.org/10.1186/s12955-019-1208-8
- Fuster-Ruiz de Apodaca, M. J., Molero, F., de Montes, L. G., Agirrezabal, A., & Vitoria, A. (2013). HIV- and AIDS-related stigma: Psychosocial aspects in a representative Spanish sample. Spanish Journal of Psychology, 16, E30. https://doi.org/10.1017/sjp.2013.52
- Garriga, C., Gutierrez, L. T., Romero, J., Montero, M., Pérez-Elías, M. J., Lévano, D. C., Gutierrez, F., Gómez-Sirvent, J. L., Peña-Monje, A., Blanco, J. R., & Rodríguez-Arenas, M. A. (2020). Psychological distress in women and men living with HIV in Spain: A cross-sectional telephone survey. Evidence Based Mental Health, 23(3), 91. https://doi.org/10.1136/ebmental-2019-300138
- Greene, M., Hessol, N. A., Perissinotto, C., Zepf, R., Hutton Parrott, A., Foreman, C., Whirry, R., Gandhi, M., & John, M. (2018, May). Loneliness in older adults living with HIV. AIDS Behavior, 22(5), 1475–1484. https://doi.org/10.1007/s10461-017-1985-1
- Guaraldi, G., Orlando, G., Zona, S., Menozzi, M., Carli, F., Garlassi, E., Berti, A., Rossi, E., Roverato, A., & Palella, F. (2011, December). Premature age-related comorbidities among HIV-infected persons compared with the general population. Clinical Infectious Diseases, 53(11), 1120–1126. https://doi.org/10.1093/cid/cir627
- Hsieh, E., Polo, R., Qian, H., Fuster-Ruiz de Apocada, M. J., & del Amo, J. (2022). Intersectionality of stigmas and health-related quality of life in people ageing with HIV in China, Europe, and Latin America. The Lancet Healthy Longevity, 3(3), e206–e215. https://doi.org/10.1016/S2666-7568(22)00003-4
- Kiplagat, J., Tran, D. N., Barber, T., Njuguna, B., Vedanthan, R., Triant, V. A., & Pastakia, S. D. (2022, April, 01). How health systems can adapt to a population ageing with HIV and comorbid disease. The Lancet HIV, 9(4), e281–e292. https://doi.org/10.1016/S2352-3018(22)00009-1
- Lazarus, J. V., Cascio, M., Anderson, J., Pasanen, S., & Harding, R. (2023). A person-centred approach to enhance the long-term health and wellbeing of people living with HIV in Europe. Journal of The International Aids Society, 26(S1), e26117. https://doi.org/10.1002/jia2.26117
- Lazarus, J. V., Janamnuaysook, R., & Caswell, G. (2023, July). A people-centred health system must be the foundation for person-centred care in the HIV response. Journal of The International Aids Society, 26(Suppl 1), e26125. https://doi.org/10.1002/jia2.26125
- Li, L., Yuan, T., Wang, J., Fitzpatrick, T., Li, Q., Li, P., Tang, X., Xu, G., Chen, D., Liang, B., Cai, W., & Zou, H. (2020, May). Sex differences in HIV treatment outcomes and adherence by exposure groups among adults in guangdong, China: A retrospective observational cohort study. EClinicalMedicine, 22, 100351. https://doi.org/10.1016/j.eclinm.2020.100351
- Liu, K., Cheng, F., Dong, H., Dong, X., & Xu, J. (2022, January). Sexual orientation and quality of life of people living with HIV/AIDS in China: Evidence from an institutional-based cross-sectional study. Quality of Life Research, 31(1), 125–134. https://doi.org/10.1007/s11136-021-02877-3
- Loutfy, M. R., Sherr, L., Sonnenberg-Schwan, U., Walmsley, S. L., Johnson, M., d'Arminio Monforte, A., & Action, W. f. P. (2013). Caring for women living with HIV: Gaps in the evidence. Journal of The International Aids Society, 16(1), 18509. https://doi.org/10.7448/IAS.16.1.18509
- Martin, K., Naclerio, F., Karsten, B., & Vera, J. H. (2019, May). Physical activity and quality of life in people living with HIV. AIDS Care, 31(5), 589–598. https://doi.org/10.1080/09540121.2019.1576848
- Mazonson, P., Berko, J., Loo, T., Kane, M., Zolopa, A., Spinelli, F., Karris, M., & Shalit, P. (2021, March). Loneliness among older adults living with HIV: The “older old” may be less lonely than the “younger old”. AIDS Care, 33(3), 375–382. https://doi.org/10.1080/09540121.2020.1722311
- McMillan, J. M., Krentz, H., Gill, M. J., & Hogan, D. B. (2018, October 22). Managing HIV infection in patients older than 50 years. Canadian Medical Association Journal, 190(42), E1253–e1258. https://doi.org/10.1503/cmaj.171409
- Monteiro, F., Canavarro, M. C., & Pereira, M. (2016). Factors associated with quality of life in middle-aged and older patients living with HIV. AIDS Care, 28(sup1), 92–98. https://doi.org/10.1080/09540121.2016.1146209
- Morales, D. R., Moreno-Martos, D., Matin, N., & McGettigan, P. (2022, May). Health conditions in adults with HIV compared with the general population: A population-based cross-sectional analysis. EClinicalMedicine, 47, 101392. https://doi.org/10.1016/j.eclinm.2022.101392
- Nobre, N., Pereira, M., Roine, R. P., Sintonen, H., & Sutinen, J. (2017, August). Factors associated with the quality of life of people living with HIV in Finland. AIDS Care, 29(8), 1074–1078. https://doi.org/10.1080/09540121.2017.1281879
- Nuño, N., Martínez, A., Martínez, S., Cobos, M., Hernández, J. S., & Polo, R. (2024). Sex differences in health-related quality of life and poverty risk among older people living with HIV in Spain: A cross-sectional study. PLoS One, 19(5), e0301335. https://doi.org/10.1371/journal.pone.0301335
- Pellowski, J. A., Kalichman, S. C., Matthews, K. A., & Adler, N. (2013, May-June). A pandemic of the poor: Social disadvantage and the U.S. HIV epidemic. American Psychologist, 68(4), 197–209. https://doi.org/10.1037/a0032694
- Pereira, M., Martins, A., Alves, S., & Canavarro, M. C. (2014, November). Assessing quality of life in middle-aged and older adults with HIV: Psychometric testing of the WHOQOL-HIV-bref. Quality of Life Research, 23(9), 2473–2479. https://doi.org/10.1007/s11136-014-0707-7
- Pérez-Valero, I., Blanch, J., & Martínez, E. (2022, October). Perception of HIV physicians in Spain towards diagnosis and management of neuropsychiatric comorbidities in people with HIV. HIV Medicine, 23(9), 969–977. https://doi.org/10.1111/hiv.13296
- Pond, R. A., Collins, L. F., & Lahiri, C. D. (2021). Sex differences in non-AIDS comorbidities among people With human immunodeficiency virus. Open Forum Infectious Diseases, 8(12), ofab558. https://doi.org/10.1093/ofid/ofab558
- Serrão, R., Piñero, C., Velez, J., Coutinho, D., Maltez, F., Lino, S., Sarmento, E. C. R., Tavares, A. P., Pacheco, P., Lopes, M. J., Mansinho, K., Miranda, A. C., Neves, I., Correia de Abreu, R., Almeida, J., & Pássaro, L. (2019, February). Non-AIDS-related comorbidities in people living with HIV-1 aged 50 years and older: The AGING POSITIVE study. International Journal of Infectious Diseases, 79, 94–100. https://doi.org/10.1016/j.ijid.2018.10.011
- Shim, M. S., & Noh, D. (2022, July 11). Effects of physical activity interventions on health outcomes among older adults living with HIV: A systematic review and meta-analysis. International Journal of Environment Research and Public Health, 19(14), https://doi.org/10.3390/ijerph19148439
- Skinta, M. D., Brandrett, B. D., Schenk, W. C., Wells, G., & Dilley, J. W. (2014). Shame, self-acceptance and disclosure in the lives of gay men living with HIV: An interpretative phenomenological analysis approach. Psychology & Health, 29(5), 583–597. https://doi.org/10.1080/08870446.2013.871283
- Vincent, W., Fang, X., Calabrese, S. K., Heckman, T. G., Sikkema, K. J., & Hansen, N. B. (2017). HIV-related shame and health-related quality of life among older, HIV-positive adults. Journal of Behavioral Medicine, 40(3), 434–444. https://doi.org/10.1007/s10865-016-9812-0
- Waldron, E. M., Burnett-Zeigler, I., Wee, V., Ng, Y. W., Koenig, L. J., Pederson, A. B., Tomaszewski, E., & Miller, E. S. (2021, January-December). Mental health in women living With HIV: The unique and unmet needs. Journal of the International Association of Providers of AIDS Care, 20, 2325958220985665. https://doi.org/10.1177/2325958220985665