ABSTRACT
The experience sampling method (ESM) is a structured diary method with high ecological validity, in that it accurately captures the everyday context of individuals through repeated measurements in naturalistic environments. Our main objective was to investigate the feasibility of using ESM in individuals with acquired brain injury (ABI). A second goal was to explore the usability of ESM data on a clinical level, by illustrating the interactions between person, environment, and affect. The PsyMate device provided ABI patients (N = 17) with ten signals (beeps) per day during six consecutive days. Each beep was followed by a digital questionnaire assessing mood, location, activities, social context, and physical well-being. Results demonstrated high feasibility with a 71% response rate and a 99% completion rate of the questionnaires. There were no dropouts and the method was experienced as user-friendly. Time-lagged multilevel analysis showed that higher levels of physical activity and fatigue predicted higher levels of negative affect at the same point in time, but not at later time points. This study illustrates the potential of ESM to identify complex person–environment dynamics after ABI, while generating understandable and easy to use graphical feedback.
Introduction
Acquired Brain Injury (ABI) can lead to cognitive impairments in various domains such as attention, recognition, memory, language and speed of information processing. A large part of individuals with ABI also show behavioural problems including impaired self-regulation, reduced social skills, or worsened pre-existing behavioural problems (Ownsworth, McFarland, & Mc Young, Citation2000; Ylvisaker, Turkstra, & Coelho, Citation2005). These problems may persist many years after sustaining brain injury (Milders, Fuchs, & Crawford, Citation2003). Further, ABI has been associated with higher reported levels of fatigue and irritability, as well as a higher risk to develop depressive symptoms (Cumming, Packer, Kramer, & English, Citation2016; Fann, Hart, & Schomer, Citation2009; Mollayeva et al., Citation2014; Robinson & Jorge, Citation2016).).
Emotional and behavioural problems are strongly determined by the interaction between the person experiencing these problems and the context in which they occur (e.g., Kendler, Kuhn, & Prescott, Citation2004). Effective treatment of these problems should therefore take into account the personal and contextual factors that contribute to their occurrence (Ownsworth & Oei, Citation1998; Ylvisaker et al., Citation2005). However, person-environment interactions are often complex and difficult to measure in real life (Cott, Wiles, & Devitt, Citation2007; Moldover, Goldberg, & Prout, Citation2004). Contextual information is therefore often not always available and this may seriously hamper treatment effectiveness (Moldover et al., Citation2004). The use of retrospective questionnaires and clinical interviews may not sufficiently capture these complex real life interactions, and may only reflect state-dependent and potentially biased memory reports. For instance, the presence of cognitive disturbances or high emotional stress may give rise to over- or underreporting of symptoms and problems during the clinical interview (Iverson, Brooks, Ashton, & Lange, Citation2010; Ownsworth et al., Citation2007). As a result, the therapist may lack important information to optimise treatment, while the person being treated might feel misunderstood.
One potential way to address these concerns is the use of “Experience Sampling Methodology” (ESM; Delespaul, Citation1995). ESM is a structured diary method shown to accurately capture the context of individuals in their everyday lives through repeated assessments of affect, current activities, symptomatology, and social context, as well as the subjective appraisal of these situational factors (Myin-Germeys et al., Citation2009). ESM allows to assess daily fluctuations and patterns in mood, thoughts, and symptoms while taking into account person–environment interactions and circumventing recollection bias (Kimhy et al., Citation2006; Myin-Germeys et al., Citation2009). It has been shown to be a valid and feasible method to assess mood, symptomatology, and other variables in various populations such as chronic pain, schizophrenia, ADHD, psychosis and depression (Huijnen et al., Citation2010; Kimhy et al., Citation2006; Kimhy et al., Citation2010; Knouse et al., Citation2007; Kramer et al., Citation2014; Myin-Germeys et al., Citation2003; Thewissen et al., Citation2011; Wichers et al., Citation2011).
Repeated momentary measurements in naturalistic environments are also referred to using different terminology such as “Ecological Momentary Assessment” (EMA). The terms ESM and EMA originate from different disciplinary contexts (Shiffman, Stone, and Hufford, Citation2008), but are currently often employed interchangeably (e.g., Conner & Barret, Citation2012). Shiffman et al. (Citation2008) suggest using EMA as a broader term that refers to a common methodological framework encompassing the measurement of subjective states as well as behaviour and physiological parameters. In contrast, Trull and Ebner-Priemer (Citation2013) propose the term “Ambulatory Assessment” (AA) as an umbrella term to cover the wide range of available assessment methods. Because the current study aimed to sample subjective self-reports of current experiences at different points in time, we believe “experience sampling” best describes our methodology, and we will use the term ESM consistently throughout this report.
With respect to ABI, a small number of studies has used ESM (Jean, Swendsen, Sibon, Fehér, & Husky, Citation2013; Johnson et al., Citation2009; Juengst et al., Citation2015; Lewandowski, Rieger, Smyth, Perry, & Gathje, Citation2009; Mazure, Weinberger, Pittman, Sibon, & Swendsen, Citation2014; Sibon, Lassalle-Lagadec, Renou, & Swendsen, Citation2012); and support the capacity of this method to assess cognitive, physical and affective complaints after brain injury. For instance, Juengst et al. (Citation2015) investigated mood and anxiety symptoms in individuals with traumatic brain injury (TBI) and found initial support for the validity, usability and feasibility of assessing these symptoms using a smartphone “mhealth” application (Juengst et al. Citation2015). Lewandowski et al. (Citation2009) showed that adolescents who had suffered a concussion reported higher levels of irritability and concentration problems than healthy controls. Furthermore, this study revealed temporal patterns in physical complaints with headaches increasing throughout the day and persisting into the night.
Similarly, in ESM studies in stroke survivors, Jean et al. (Citation2013), Johnson et al. (Citation2009), Mazure et al. (Citation2014), and Sibon et al. (Citation2012) offered support for the feasibility of ESM, evidencing compliance rates of up to 84% of measurement moments being answered. Further, they recommended the application of ESM for investigating functional impairments in the natural context and for investigating constructs that cannot easily be assessed by standardised clinical questionnaires, such as identifying precursors of symptom expression (Johnson et al., Citation2009). Specifically, patients’ ESM reports of fatigue, negative affect and anxiety were found to be predictive of the risk of depression three months post-stroke (Sibon et al., Citation2012), and performing sports and working in the acute post-stroke phase was associated with higher depression scores (Jean et al., Citation2013). Finally, Mazure et al. (Citation2014) evidenced greater reactivity to stressful life events in female relative to male stroke survivors.
Although these studies show the potential of ESM in patients with ABI, they come with some limitations. First, the study by Lewandowski et al. (Citation2009) had a very small sample (three individuals with concussion, three healthy controls) consisting of adolescents—for whom the threshold to use ESM applications may be lower relative to older populations. Second, the four studies in stroke survivors are based on the same sample of stroke patients (Johnson et al., Citation2009; Mazure et al., Citation2014; Sibon et al., Citation2012), or a subsample thereof (Jean et al., Citation2013). Thus, they should not be considered as independent replications in terms of feasibility and usability testing. Further, only a limited number of measurements throughout the day were used in this sample, which were also administered at fixed intervals. This not only results in a limited representation of daily life functioning, but may also cause the participants to adapt their behaviour to the assessment moments. This was also the case for Juengst et al. (Citation2015), where questionnaires were administered only once every day during a time frame chosen by participants themselves over a total eight-week period. Although this strategy has its merits in that it allows assessing evolutions in mood and affect over multiple weeks, it has the risk of offering an incomplete view on daily mood and affect variations. Moreover, an ESM protocol consisting of only one daily measurement may have different outcomes in terms of feasibility compared with more intense measurement protocols. In this study, we used an electronic device (PsyMate) that allowed us to collect ESM data at 10 occasions randomly throughout the day. This combination of high measurement intensity and a random sampling schedule provides a more fine-grained depiction of daily life, while simultaneously reducing the risk of participants adapting their behaviour to the methodology.
The main goal of this study was therefore to assess feasibility of ESM with high measurement intensity by using the PsyMate in an ABI population. A second goal was to explore the usability of the ESM data on a clinical level, by illustrating the interactions between person, environment and experienced affect by means of graphs. In addition to clinical applications, ESM offers the opportunity to investigate more complex person–environment dynamics from a purely scientific point of view. As illustration, we will analyze data on the relationship between physical activity, fatigue, and negative affect (NA). Fatigue is a very common complaint after ABI (Cumming et al., Citation2016; Mollayeva et al., Citation2014), and has been shown to be a (prospective) risk factor for increases in negative mood (e.g., Ponsford, Schönberger, & Rajaratnam, Citation2015; Schönberger, Herrberg, & Ponsford, Citation2014). With respect to physical activity, a recent review of ESM studies in clinical and non-clinical populations revealed that exercise may represent a protective factor against negative mood (Pemberton & Fuller Tyszkiewicz, Citation2016). However, another recent review—which also included several ESM studies—found that physical activity was positively related to positive effect, but inconsistently related to NA (Liao, Shonkoff, & Dunton, Citation2015). Moreover, it is unclear whether these general findings are applicable to ABI populations. For instance, Jean et al. (Citation2013) showed that engaging in sports activities in the acute post-stroke phase was associated with higher depressed mood. Therefore, we aimed to use ESM to further explore the relationship between physical activity, fatigue, and NA after ABI.
Method
Sample
Patients were recruited at Adelante Zorggroep rehabilitation centre in Hoensbroek, The Netherlands, between July 2014 and March 2015. Study inclusion criteria were: (i) participants had to be diagnosed with acquired brain injury, either stroke or traumatic brain injury (TBI), (ii) receiving outpatient care at the time of the study, (iii) were aged between 18 and 65 years. Exclusion criteria for the study were based on clinical judgment by the treating psychologist: (i) severe memory problems compromising participation in the study, e.g., forgetting the purpose and instructions of the study or how to use the PsyMate, (ii) distorted orientation in place and time, and (iii) language impairments compromising reading and understanding written language and verbal instructions.
The study was approved by the Ethics Committee Psychology at the Faculty of Psychology and Neuroscience of Maastricht University, as well as the ethics committee at Adelante Zorggroep.
Device
The PsyMate (smarteHealth GmbH, Luxembourg) is a small electronic device with a user-friendly touch-screen interface, making it accessible for participants with limited technological experience. It was specifically developed to implement ESM in clinical practice. For this study the PsyMate was programmed to emit 10 beeps (signals) throughout the day between 7:30 A.M. and 10:30 P.M., following a semi-random schedule (with the constraint that the interval between two beeps could not be shorter than 15 minutes or longer than 270 minutes; the average interval was 90 minutes). Each beep was a prompt to fill out a brief questionnaire with items assessing current mood (positive/negative affect, e.g., “I feel down”), self-esteem (e.g., “I like myself”) location, activities, social context, physical well-being (e.g., “I am tired”), and whether or not the beep was experienced as disturbing (see Appendix A1). The items measuring positive and negative affect were guided in part by the Positive and Negative Affect Scale (PANAS; Watson, Lee, & Tellegen, Citation1988), and in part by findings of previous ESM studies, selecting items with high negative and positive affect latent factor loadings respectively, good internal consistency, and sufficient within-person variability (e.g., Oorschot et al., Citation2013; Wichers et al., Citation2012). This allowed us to minimise the number of items in our questionnaire, thus limiting participant burden without sacrificing internal consistency and moment-to-moment-variability. Questions with respect to mood, self-esteem, and physical well-being were answered on a 7-point Likert scale (from 1 “not at all” to 7 “very much”). Context and activities related questions were provided in a multiple-choice format (e.g., location: “At home”; “at family’s/friend’s place”; “at work”; “health care setting”; “public space”; “transport”; “somewhere else”). Appraisal of context and activities was assessed with a bipolar scale ranging from -3 (“not pleasant at all”) to + 3 (“very pleasant”), with 0 being neutral.
Psymate evaluation questionnaires
Subjective experiences of PsyMate use were assessed using two debriefing questionnaires, one regarding user friendliness and the second regarding general acceptability of the methodology (e.g., “Did you experience difficulties switching the PsyMate on?,” “Did the PsyMate influence your mood?”). These questionnaires were provided after ESM data acquisition was completed, and a total of 18 items with respect to time burden, interference with daily life, possible difficulties with and acceptability of the method. The items were scored on a 7-point Likert scale ranging from 1 “not at all” to 7 “very much.” A final open-ended item offered the possibility to provide further feedback regarding the PsyMate and its use.
Procedure
After patients were screened on inclusion and exclusion criteria by their treating psychologist, eligible participants received an information letter regarding the specifics of the study. Patients were contacted the week afterwards to check whether they were interested in participation. Upon obtaining informed consent the patient was enrolled in the study procedure. A standardised study protocol was used for every participant including (1) an introduction session, (2) data collection phase, and (3) a debriefing session. An appointment was made for the introduction session; data collection started the day after the introduction session to ensure complete measurement days, and continued for six consecutive days. The debriefing session was planned the day after the final day of data collection.
Introduction session: extensive explanation of the PsyMate device and the questions provided by the PsyMate. Participants were informed about the workings of the device as well as familiarised with the beep signal, question types and format during a 30-minute training. Introductory sessions were given on an individual basis to ensure optimal understanding and effectiveness while working with the PsyMate. Additionally, participants were provided with a leaflet containing a summary about the PsyMate as well as a phone number and email address of the researcher in case any problems or questions would arise during data collection. Every participant was provided with two PsyMate devices, in case of a malfunction.
ESM data collection: Every participant was requested to complete the PsyMate reports after each beep for six consecutive days, including two weekend days. After every beep participants had 15 minutes to respond and fill out the questionnaire. If the participant did not respond within this set time interval the PsyMate turned off again, and the missed questionnaire was skipped altogether. However, patients were instructed to respond immediately after the report was presented to ensure a representative depiction of emotion and activities in the moment.
Debriefing session: Upon completing the ESM data acquisition phase, patients returned for a debriefing session. During this debriefing session, participants filled out the two evaluation questionnaires.
Statistical analyses
To assess feasibility of the ESM in the ABI population, descriptive analyses of response and completion rates of the reports were conducted. Furthermore, responses to debriefing questionnaires were analysed using descriptive statistics to investigate experiences and possible problems with PsyMate usage.
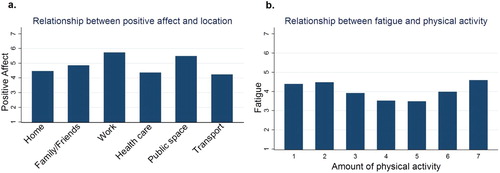
To assess usability of the ESM in this population, the patterns of daily contexts, and—as illustration—the relationships between positive affect and location and between fatigue and physical activity are presented bar graphs and pie charts. Standardised commands were used to generate various bar- and circle graphs regarding physical activity, social company, location, activities, fatigue, and affect. We here present these data on the level of the entire sample, but these graphs can of course also be generated in the clinic at the level of the individual. The variable positive affect was generated from the items “I feel: cheerful, relaxed, enthusiastic, satisfied and confident” (items 1, 2, 3, 4, and 11 in Appendix A1) for every individual. The variable negative affect (NA) was computed following an identical procedure averaging the items “I feel: lonely, anxious, irritable, down, desperate, tensed, hurried, agitated and powerless” (items 6, 7, 8, 9, 10, 12, 13, 14 and 15 in Appendix A1) on an individual level. Factor analyses were performed to confirm that the items loaded on the same factors, and that the PA and NA constructs had sufficient internal validity (Cronbach’s alpha for PA = 0.91, Cronbach’s alpha for NA = 0.95).
Finally, to explore both momentary and temporal relationships between physical activity, fatigue, and NA, a series of multilevel regression and time-lagged multilevel analyses was conducted. To be able to assess these relationships, data were analysed using the xtmixed module in STATA version 12.1 (Stata Corporation, College Station, TX, Texas). Due to the hierarchical nature of the data (multiple observations nested within individuals), multilevel regression is the most suitable statistical method. The matrix of choice was covariance (unstructured) to account for the degree of within-subject co-variance inherent to the ESM data (the beep items filled out by a participant are expected to be more similar to each other than the same items filled out by another participant).
Multilevel regression analyses were used to test whether physical activity and fatigue were significant predictors of experienced NA. To this end, the scores on the items physical activity (“I have been physically active before the beep”) and fatigue (“I am tired”) were entered as the independent variables. The previously generated variable NA was entered as the dependent variable. The next step was to look at the temporal relationships between the variables using time-lagged multilevel regression analyses. To be able to assess the relationship between variables over different time-points, an additional time variable was created, representing the time between beeps. This step made it possible to run time-lagged multilevel regression analyses using time as an independent variable. This time variable was used to generate time lags for each of the variables in the equation making it possible to use the values of the preceding time points (t-1 and t-2) as predictors for current time points (t0). This was done for each of the independent variables creating the variables physical activity t-1 and t-2), NA t-1 and t-2, and fatigue t-1, t-2. To test whether previous physical activity was associated with NA at t0, physical activity at t-1 and t-2 were entered as predictors into separate mixed regression analyses with NA t0 as the outcome variable. Similarly, to test whether previous NA was associated with NA at t0, NA at t-1 and t-2 were entered as predictors into separate analyses, with NA t0 as the outcome variable. The same procedure was applied to investigate whether previous fatigue (at t-1, t-2) was associated with NA at t0. Again, covariance (unstructured was selected for the matrix), and a random intercept and random slope model was used for every analysis. Significance level was set at p = .05 two-tailed.
Results
Feasibility
A total of 17 patients were included in the analyses with a mean age of 44.2 (SD = 14.5), and nine were female (53%). Eight patients sustained TBI and nine suffered a stroke. An average response rate of 71.18% regarding the PsyMate beeps was recorded (726 beeps were answered out of 1020 presented). Additionally, 98.76% of these beep prompted reports were fully completed (see ). There were no dropouts during the ESM data collection. Furthermore, data show that patients thought the questions in the PsyMate to be a good representation of their experiences (M = 4.92, SD = 1.38), whereas the PsyMate was reported to have little influence on their activities (M = 2.15, SD = 1.34) or social contacts (M = 2.00, SD = 1.16). Additionally, participants reported limited to no difficulties when using the PsyMate (M = 1.77, SD = 1.36) and did not experience the PsyMate as burdensome (M = 2.08, SD = 1.19). The complete evaluation regarding general experiences with the PsyMate and user friendliness can be found in and , respectively.
Table 1. Frequencies of questionnaires answered and completed.
Table 2. General evaluation questionnaire PsyMate.
Table 3. Evaluation of PsyMate user friendliness.
Usability
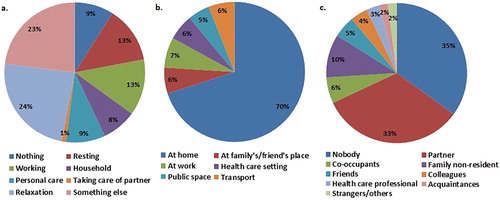
ESM data on a group level show that patients spent most of their time on relaxation (24%) and other not further specified activities (23%) (a). The least time is spent on doing household related activities (8%), and taking care for their partner (1%). Moreover, patients spent most of their time at home (70%) or at work (7%) (b). With respect to social environment, patients spent most of their time alone (35%), or in the company of their partner (33%) (c).
Figure 1. Reported activities (a), environment (b) and social context (c) on the level of the entire sample.
When looking at positive affect (PA) and daily context of the patients, (panel a) indicates that most positive affect is experienced at work or in public spaces, whereas being at a healthcare institution results in the lowest levels of PA, followed by transport or being at home. This may be surprising as participants spend 70% of their time at home. Finally, (panel b) depicts levels of fatigue as a function of physical activity, and suggests that there is an optimum around average levels of activity, resulting in the lowest levels of experienced fatigue (b). Both very low and very high levels of activity appear to be associated with relatively higher levels of fatigue. It should be noted that these figures are provided to demonstrate the clinical usability of ESM data by generating graphs that are easy to interpret, and that not all of these graphs are complemented with statistical analyses. In the following section, we provide statistical analyses on the relationship between physical activity, fatigue, and NA.
Strength of associations between physical activity, fatigue, and negative affect
Multilevel regression analyses showed higher physical activity (B = 0.11, SE = 0.02, p < .01) and fatigue (B = 0.17, SE = 0.03, p < .01) to be significant predictors of increased NA when measured at the same moment in time. However, time-lagged analyses revealed that previous physical activity at t-1 (B = 0.00, SE = 0.01, p = .77) and t-2 (B = 0.00, SE = 0.02, p = .71) was not significantly associated with NA at t0. NA at time point t0 was significantly predicted by increased NA at t-1 (B = 0.35, SE = 0.03, p = .01) and t-2 (B = 0.07, SE = 0.03, p = .05). Additionally, when controlling for levels of fatigue at t-1 and t-2, physical activity remained non-significant B = 0.00, SE = 0.01, p = .86 and B = 0.00, SE = 0.01, p = .75. Fatigue also had no significant effect on experienced NA at later moments in time, B = −0.03, SE = 0.02, p = .15 (t-1) and B = −0.01, SE = 0.02, p = .5 (t-2). In contrast, the predictive value of NA on experienced NA later in time remained significant at both time points, B = 0.36, SE = 0.03, p < .001 (t-1) and B = 0.07, SE = 0.03, p = .041 (t-2), indicating that higher levels of NA were predicted by higher NA scores measured up to three hours earlier in time.
Discussion
The first goal of this study was to assess the feasibility of ESM and the PsyMate device within an ABI population. Our results showed an average response rate of 71%, which is more than twice the minimum requirement of 33% for the method to be valid (Delespaul, Citation1995). Although our intensity of measurements was twice as high relative to previous ESM studies that included stroke survivors, our overall response rate was only 13% lower in comparison to their very high response rate of 84% (Jean et al., Citation2013; Johnson et al., Citation2009; Mazure et al., Citation2014). This shows that high measurement intensity is feasible in an ABI population.
Besides the high response rate, 99% of beeps responded to were fully completed by participants. This high completion percentage shows that 45–50 questions per report are not too burdensome for patients. This can be explained by the observation that participants familiarise with the questions over time, reducing the time and energy needed to answer them. These findings further underline the effectiveness of the PsyMate as a means to obtain ESM data.
Further support for the application of ESM and PsyMate comes from the fact that participants reported the PsyMate to have little effect on their mood, activities and social contacts throughout the data acquisition week. Not only does this imply high tolerability of the device, it also suggests that patients do not actively adapt their activities of daily life to working with the PsyMate, ensuring high ecological validity of obtained data. Nevertheless, it remains possible that the PsyMate exerted subtle influences on behaviour beyond conscious awareness, which obviously precludes detecting these effects by means of self-reports.
A second goal of the study was to investigate the usability of ESM data. When exploring the usability of descriptive data on a population level, much information can be obtained using ESM that is otherwise not available via retrospective questionnaires and clinical interviews. For example, visual inspection of the presented figures suggests that positive affect is associated with, and influenced by, context. Although participants spend most of their time at home (70%), (panel a) suggests that being home is not associated with high positive affect. Furthermore, data on fatigue and physical activity show an inverted U-shape pattern with an optimal level of PA at an average level of physical activity. Although differences are small on the level of the entire sample, as depicted in (panel b), they might be clinically relevant on the level of an individual patient. These findings illustrate how graphical representation of the data can be used as a tool in the clinic to discuss problems experienced by patients, or even as guidance for intervention.
An application of ESM that nicely illustrates the clinical possibilities of ESM research is the Kramer et al. (Citation2014) study. The authors show the value of ESM as a therapeutic tool in addition to standardised medical treatment for depression. By providing structured feedback based on the patients ESM data, a linear decrease in depressive symptoms was observed which persisted up to six months. Combining regular feedback regarding daily life activities and medical treatment results in clinically relevant differences in experienced depressive symptoms compared with receiving medical treatment without feedback.
Besides using ESM data to create more insight for both patient and clinician on a descriptive level, ESM data provide the possibility to investigate the dynamics between the environment, behaviour, and emotion. We explored the relationship between physical activity, fatigue, and NA. Interestingly, we found that higher levels of physical activity and fatigue were associated with higher NA when measured at the same moment in time. However, these effects disappeared when a time component was introduced; neither physical activity nor fatigue had predictive value for NA at later time points. Only higher levels of NA proved to be a predictor of higher NA at a later point in time. An initial negative mood state predicted NA for up to three hours later.
These findings nicely illustrate how ESM can provide more fine-grained and time stamped data acquisition. This in turn offers the possibility to identify more complex and subtle relationships between various variables that might otherwise be lost due to the coarse nature of retrospective questionnaires and clinical interviews. Present findings clearly illustrate the complexity of such relationships as the role of the various predictors changes over the course of time.
To summarise, these results provide support for the feasibility and usability of ESM in ABI populations. The methodology is generally well accepted and is reported by participants to exert little interference with daily life activities. Limitations of this study include the limited sample size. Even though we demonstrate the potential of ESM in an ABI sample, further studies with larger samples are necessary to confirm initial results. Further, our sample consisted of individuals with ABI who were still receiving outpatient care. It may be safe to assume that our feasibility findings might be different in a sample of individuals who finished therapy or who had perhaps rejected therapy. Another limitation concerns the questions about physical well-being, which were all framed negatively (i.e., “I am tired”; “I do not feel well”; “I am in pain”). This negative framing may have induced a certain response bias. Further, as for most if not all ESM research, it is possible that participants completed fewer questionnaires when they were engaging in, for instance, physical activity or work, relative to doing nothing or relaxing. This may have resulted in an underestimation of participants’ activity levels.
In conclusion, the high level of compliance and acceptance of the methodology by patients suggests good feasibility and a promising new direction in both ABI research and clinical practice. Besides proving the feasibility of the methodology, this shows the strengths and potential of ESM research in the context of ABI. Not only does it offer the possibility to uncover complex environmental dynamics, it also provides the opportunity to generate constructive and ecologically valid feedback about these dynamics for both patients and healthcare professionals, paving the way towards personalised intervention techniques.
Supplementary Material
Download PDF (117 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Conner, T. S., & Barrett, L. F. (2012). Trends in ambulatory self-report: The role of momentary experience in psychosomatic medicine. Psychosomatic Medicine, 74, 327–337.
- Cott, C. A., Wiles, R., & Devitt, R. (2007). Continuity, transition and participation: Preparing clients for life in the community post-stroke. Disability and Rehabilitation, 29, 1566–1574. doi: 10.1080/09638280701618588
- Cumming, T. B., Packer, M., Kramer, S. F., & English, C. (2016). The prevalence of fatigue after stroke: A systematic review and meta-analysis. International Journal of Stroke, 11, 968–977. doi: 10.1177/1747493016669861
- Delespaul, P. A. E. G. (1995). Assessing schizophrenia in daily life. Maastricht, the Netherlands.
- Fann, J. R., Hart, T., & Schomer, K. G. (2009). Treatment for depression after traumatic brain injury: A systematic review. Journal of Neurotrauma, 26, 2383–2402. doi: 10.1089/neu.2009.1091
- Huijnen, I. P., Verbunt, J. A., Peters, M. L., Delespaul, P., Kindermans, H. P., Roelofs, J., … Seelen, H. A. (2010). Do depression and pain intensity interfere with physical activity in daily life in patients with chronic low back pain? Pain, 150, 161–166. doi: 10.1016/j.pain.2010.04.021
- Iverson, G. L., Brooks, B. L., Ashton, V. L., & Lange, R. T. (2010). Interview versus questionnaire symptom reporting in people with the postconcussion syndrome. Journal of Head Trauma Rehabilitation, 25, 23–30. doi: 10.1097/HTR.0b013e3181b4b6ab
- Jean, F. A., Swendsen, J. D., Sibon, I., Fehér, K., & Husky, M. (2013). Daily life behaviors and depression risk following stroke: A preliminary study using ecological momentary assessment. Journal of Geriatric Psychiatry and Neurology, 26, 138–143. doi: 10.1177/0891988713484193
- Johnson, E. I., Sibon, I., Renou, P., Rouanet, F., Allard, M., & Swendsen, J. (2009). Feasibility and validity of computerized ambulatory monitoring in stroke patients. Neurology, 73, 1579–1583. doi: 10.1212/WNL.0b013e3181c0d466
- Juengst, S. B., Graham, K. M., Wayan Pulantara, I., McCue, M., Whyte, E. M., Dicianno, B. E., … Wagner, A. K. (2015). Pilot feasibility of an mHealth system for conducting ecological momentary assessment of mood-related symptoms following traumatic brain injury. Brain Injury, 29, 1351–1361.
- Kendler, K. S., Kuhn, J., & Prescott, C. A. (2004). The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. American Journal of Psychiatry, 161, 631–636. doi: 10.1176/appi.ajp.161.4.631
- Kimhy, D., Delespaul, P., Ahn, H., Cai, S., Shikhman, M., Lieberman, J. A., … Sloan, R. P. (2010). Concurrent measurement of “real-world” stress and arousal in individuals with psychosis: Assessing the feasibility and validity of a novel methodology. Schizophrenia Bulletin, 36, 1131–1139. doi: 10.1093/schbul/sbp028
- Kimhy, D., Delespaul, P., Corcoran, C., Ahn, H., Yale, S., &Malaspina, D. (2006). Computerized experience sampling method (ESMc): Assessing feasibility and validity among individuals with schizophrenia. Journal of Psychiatric Research, 40, 221–230. doi: 10.1016/j.jpsychires.2005.09.007
- Knouse, L. E., Mitchell, J. T., Brown, L. H., Silvia, P. J., Kane, M. J., Myin-Germeys, I., & Kwapil, T. R. (2007). The expression of adult ADHD symptoms in daily life: An application of experience sampling methodology. Journal of Attention Disorders, 11, 652–663. doi: 10.1177/1087054707299411
- Kramer, I., Simons, C. J., Hartmann, J. A., Menne-Lothmann, C., Viechtbauer, W., Peeters, F., … Wichers, M. (2014). A therapeutic application of the experience sampling method in the treatment of depression: A randomized controlled trial. World Psychiatry, 13, 68–77. doi: 10.1002/wps.20090
- Lewandowski, L., Rieger, B., Smyth, J., Perry, L., & Gathje, R. (2009). Measuring post-concussion symptoms in adolescents: Feasibility of ecological momentary assessment. Archives of Clinical Neuropsychology, 24(8), 791–796. doi: 10.1093/arclin/acp087
- Liao, Y., Shonkoff, E. T., & Dunton, G. F. (2015). The acute relationships between affect, physical feeling states, and physical activity in daily life: A review of current evidence. Frontiers in Psychology, 6, 1–7. doi: 10.3389/fpsyg.2015.01975
- Mazure, C. M., Weinberger, H., Pittman, B., Sibon, I., Swendsen, J. (2014). Gender and stress in predicting depressive symptoms following stroke. Cerebrovascular Diseases, 38, 240–246. doi: 10.1159/000365838
- Milders, M., Fuchs, S., & Crawford, J. R. (2003). Neuropsychological impairments and changes in emotional and social behaviour following severe traumatic brain injury. Journal of Clinical and Experimental Neuropsychology (Neuropsychology, Development and Cognition: Section A), 25, 157–172. doi: 10.1076/jcen.25.2.157.13642
- Moldover, J. E., Goldberg, K. B., & Prout, M. F. (2004). Depression after traumatic brain injury: A review of evidence for clinical heterogeneity. Neuropsychology Review, 14, 143–154. doi: 10.1023/B:NERV.0000048181.46159.61
- Mollayeva, T., Kendzerska, T., Mollayeva, S., Shapiro, C. M., Colantonio, A., & Cassidy, J. D. (2014). A systematic review of fatigue in patients with traumatic brain injury: The course, predictors and consequences. Neuroscience and Biobehavioral Reviews, 47, 684–716. doi: 10.1016/j.neubiorev.2014.10.024
- Myin-Germeys, I., Oorschot, M., Collip, D., Lataster, J., Delespaul, P., & van Os, J. (2009). Experience sampling research in psychopathology: Opening the black box of daily life. Psychological Medicine, 39, 1533–1547. doi: 10.1017/S0033291708004947
- Myin-Germeys, I., Peeters, F. P. M. L., Havermans, R., Nicolson, N. A., DeVries, M. W., Delespaul, P. A. E. G., & Van Os, J. (2003). Emotional reactivity to daily life stress in psychosis and affective disorder: An experience sampling study. Acta Psychiatrica Scandinavica, 107, 124–131. doi: 10.1034/j.1600-0447.2003.02025.x
- Oorschot, M., Lataster, T., Thewissen, V., Lardinois, M., Wichers, M., van Os, J., … Myin-germeys, I. (2013). Emotional experience in negative symptoms of schizophrenia - No evidence for a generalized hedonic deficit. Schizophrenia Bulletin, 39, 217–225. doi: 10.1093/schbul/sbr137
- Ownsworth, T., Fleming, J., Strong, J., Radel, M., Chan, W., & Clare, L. (2007). Awareness typologies, long-term emotional adjustment and psychosocial outcomes following acquired brain injury. Neuropsychological Rehabilitation, 17, 129–150. doi: 10.1080/09602010600615506
- Ownsworth, T. L., McFarland, K., & Mc Young, R. (2000). Self-awareness and psychosocial functioning following acquired brain injury: An evaluation of a group support programme. Neuropsychological Rehabilitation, 10, 465–484. doi: 10.1080/09602010050143559
- Ownsworth, T. L., & Oei, T. P. (1998). Depression after traumatic brain injury: Conceptualization and treatment considerations. Brain Injury, 12, 735–751. doi: 10.1080/026990598122133
- Pemberton, R., & Fuller Tyszkiewicz, M. D. (2016). Factors contributing to depressive mood states in everyday life: A systematic review. Journal of Affective Disorders, 200, 103–110.
- Ponsford, J., Schönberger, M., & Rajaratnam, S. M. W. (2015). A model of fatigue following traumatic brain injury. Journal of Head Trauma Rehabilitation, 30, 277–282. doi: 10.1097/HTR.0000000000000049
- Robinson, R. G., & Jorge, R. E. (2016). Post-stroke depression: A review. American Journal of Psychiatry, 173, 221–231. doi: 10.1176/appi.ajp.2015.15030363
- Schönberger, M., Herrberg, M., & Ponsford, J. (2014). Fatigue as a cause, not a consequence of depression and daytime sleepiness: A cross-lagged analysis. Journal of Head Trauma Rehabilitation, 29, 427–431. doi: 10.1097/HTR.0b013e31829ddd08
- Shiffman, S., Stone, A. A., & Hufford, M. R. (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32.
- Sibon, I., Lassalle-Lagadec, S., Renou, P., & Swendsen, J. (2012). Evolution of depression symptoms following stroke: A prospective study using computerized ambulatory monitoring. Cerebrovascular Diseases, 33, 280–285. doi: 10.1159/000334663
- Thewissen, V., Bentall, R. P., Oorschot, M., van Lierop, T., van Os, J., & Myin-Germeys, I. (2011). Emotions, self-esteem, and paranoid episodes: An experience sampling study. British Journal of Clinical Psychology, 50, 178–195. doi: 10.1348/014466510X508677
- Trull, T. J., & Ebner-Priemer, U. (2013). Ambulatory assessment. Annual Review of Clinical Psychology, 9, 151–176.
- Watson, D., Lee, C., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070.
- Wichers, M., Peeters, F., Rutten, B. P. F., Jacobs, N., Derom, C., Delespaul, P., … Delespaul, P. (2012). A time-lagged momentary assessment atudy on daily life physical activity and affect: A time-lagged momentary assessment study on daily life physical activity and affect. Health Psychology, 31, 135–144. doi: 10.1037/a0025688
- Wichers, M., Simons, C. J. P., Kramer, I. M. A., Hartmann, J. A., Lothmann, C., Myin-Germeys, I., … van Os, J. (2011). Momentary assessment technology as a tool to help patients with depression help themselves. Acta Psychiatrica Scandinavica, 124, 262–272. doi: 10.1111/j.1600-0447.2011.01749.x
- Ylvisaker, M., Turkstra, L. S., & Coelho, C. (2005, November). Behavioral and social interventions for individuals with traumatic brain injury: A summary of the research with clinical implications. Seminars in Speech and Language, 26, 256–267. doi: 10.1055/s-2005-922104