ABSTRACT
We investigated the clinical effectiveness of Eye-Search, a web-based therapy app designed to improve visual search times, in a large group of patients with either hemianopia, neglect or both hemianopia and neglect. A prospective, interventional cohort design was used. For the main, impairment-based outcome measure (average visual search time), the within-subject control was affected vs. unaffected side. Four hundred and twenty-six participants who fitted the inclusion criteria completed all 4 time points (1200 therapy trials). We found a significant three-way interaction between therapy, side and group. Eye-Search therapy improved search times to the affected visual field of patients with either hemianopia alone or neglect and hemianopia, but not those with neglect alone. Effect sizes were moderate to large and consistent with previous studies. We found a similar significant interaction between therapy and group for the patient-reported outcome measure “finding things” that most closely matched the impairment-based outcome (visual search). Eye-Search therapy improves both impairment-based and patient-reported outcome measures related to visual search in patients with hemianopia alone or hemianopia and neglect.
Introduction
Hemianopia and neglect are the two most common visual disorders complicating posterior brain injury (Corbetta et al., Citation2005; Rowe et al., Citation2019). While neglect is more likely to spontaneously improve over the first year post-injury than hemianopia, both have long-term effects on patients’ activities of daily living (Warren, Citation2009; Wee & Hopman, Citation2008). Several behavioural approaches to treating patients with persistent hemianopia have been successfully trialled. The most consistently effective therapies promote retraining of compensatory eye movements, by practising voluntary guided saccades (e.g., patients have to find a visual target amongst distractors, or find a target that has “jumped” to a new location in their blind field (Jacquin-Courtois et al., Citation2013; Schuett et al., Citation2012)). Eye-movement therapies have also been shown to be effective in treating the symptoms of neglect, although these rely on stimuli that induce smooth-pursuit eye movements (e.g., patients have to focus on targets that move towards their neglected side at a constant velocity (Hopfner et al., Citation2015; Kerkhoff et al., Citation2014)). We have previously reported on the clinical efficiency of Eye-Search (https://www.eyesearch.ucl.ac.uk/), a web-based therapy that improves visual search in patients with hemianopia, but in that study (n = 78) we left out patients with neglect (Ong et al., Citation2015). As hemianopia and neglect can co-occur (Muller-Oehring et al., Citation2003), the aim of this study was to investigate whether Eye-Search therapy works in patients with either neglect alone (“pure neglect” group) or hemianopia and neglect. We also extended the criteria for length of participation in the study from three time points (patients completed 800 therapy trials), to four (1200 therapy trials completed).
Materials and methods
Setting
All subjects' data were collected using the Eye-Search browser-based app. This study was approved by the UCL Research Ethics Committee: 2681/001, and all participants consented to the use of their data. All data were anonymized and held securely on a UCL server. The Eye-Search app has five main data collecting components:
A test to identify hemianopia
A test to identify visual neglect
The therapy: a ramp-step paradigm, embedded in a game, that delivers the trial-by-trial eye-movement practice
An impairment-based outcome measure: a visual search task
A patient-reported outcome measure (PROM): a visual analogue scale for rating difficulty performing six activities of daily life
Subjects re-tested themselves on the two visual tests and two outcome measures before they started therapy (baseline) and then every time that they completed a block of 400 trials (T1 = after 400 trials, T2 after 800 and T3 after 1200).
Study population and selection criteria
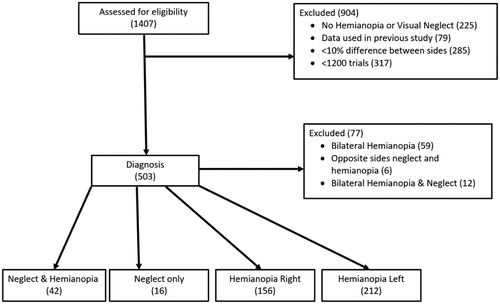
The therapy took place at the discretion of the patient and on their personal computers. Due to the nature and delivery modality of the therapy, the patients are considered to be self-enrolled, rather than traditionally recruited. The data analysed in this study were collected from participants who used the Eye-Search website between July 2012 and February 2019. In this period, 1407 participants took part, out of which 426 fitted the inclusion criteria (see consort diagram ). Of these, 302 (71%) were male. The mean participant age was 60 years [SD 14.6]. Causative diagnosis was self-reported with 6% leaving the section blank. The remaining patients were divided as follows: 84% stroke; 5% head injury; 3% surgery; and, 2% reported other causes such as an abscess, CO poisoning and encephalitis. Time between the cause of their visual impairment and starting therapy was positively skewed, median 85 days [IQR = 44–210 days]. Progress through the therapy was self-paced. The time to get from baseline to T1 and T3 was also positively skewed with subjects taking a median time of 5 days [IQR = 2–12 days] and 20 days [IQR = 9–33 days], respectively.
Study definitions
Hemianopia
A diagnosis of hemianopia was based on the results of a participants’ visual field test (VFT). This test has been previously reported (Ong et al., Citation2015) and comprises a grid of 16 points (8 in each hemifield, two each at 1, 2.5, 5 and 10 degrees eccentricity). VFT over three time points (baseline, T1 and T2) were assessed to make sure that participants had consistent field loss. If a participant missed 3 or more points in one of the hemifields over 50% (2 times out of 3) of the time, then a diagnosis of hemianopia was made. We had 212 participants with a left-sided hemianopia and 156 with a right-sided one; patients with bilateral loss (n = 59) were excluded.
Neglect
A diagnosis of visual neglect was established using a visual neglect test (VNT) (Gorgoraptis et al., Citation2012). This is a form of cancellation task with targets (circles with an upward facing gap) and distractors (both full circles and circles with a downward facing gap). The test uses a different array each time but always consists of 32 targets and 63 distractors in each hemifield. Subjects have 5 min to click on all the targets. The participants receive transitory feedback, that is, the targets glow green for a second if correctly selected and the distractors red. Unlike traditional pen-and-paper tests, no “mark” is left on any target type. This makes the test harder as the participants have to keep a mental record of where they have been. As in our previous study (Ong et al., Citation2015), we used two ratio criteria for a diagnosis of visual neglect: (1) if subjects consistently missed twice as many targets on one side compared with the other, on two out of three time points (baseline, T1 and T2). (2) A similar lateralized ratio over two out of three time points, but for target revisits; if these were consistently twice as high on one side compared with the other. The results were checked at three time points, baseline and two follow-up therapy time points.
There were 9 participants with left and 7 with right neglect; these were combined to form a single neglect only group. In the neglect & hemianopia group, the two deficits were always on the same side as each other: 37 patients had left-sided deficits and 5 had right-sided ones.
Inclusion criteria
The participants had to have a diagnosis of hemianopia, visual neglect or hemianopia & neglect.
Participants had to have, at baseline, a larger than 10% difference in average visual search time to targets in their affected side compared to their unaffected side. This difference was important because in order to investigate whether a therapy effect has occurred or not, a deficit must first be established.
Data from participants who had taken part in the previously reported Eye-Search study (Ong et al., Citation2015) were excluded.
Only patients who had completed >1200 trials and had reached their third therapy time point (T3) were included.
Therapy
The therapy is a ramp-step pursuit paradigm developed by Jacquin-Courtois et al. (Citation2013), in which participants have to follow a “rolling ball” stimulus that contains a “C” shape and moves in two phases. In the “ramp phase,” the ball starts on one side of the screen and rolls towards the midline. Near this point, the “step phase” occurs with the stimulus appearing instantaneously in a random location beyond the midline. The subjects’ goal is to find the ball’s resting place. They do this by reporting the final orientation of the outcome stimuli with the “C” shape, which is either up or down. The therapy moves through 16 progressively harder levels of 300 trials as static distractor stimuli are added in, and the contrast between the target and background is reduced. Each time that the subjects completed 400 trials, they had to test themselves again on the 2 diagnostic tests and 2 outcomes tests outlined in the settings section above.
Outcomes
Visual search task
This impairment-based outcome is a reaction time based visual search task. Participants search a crowded “virtual desktop” scene for a given object such as a coin or paperclip among multiple other objects. The target item is presented at the beginning of each trial. There are 17 target items, with the first trial a practice run. The remaining 16 target items are presented in an even split (order randomized) with 8 on each side of the scene. An average reaction time (RT) is generated for each side at each time point. The labels for these average scores were recoded for each subject from left/right to affected/unaffected depending on the side of their hemianopia and/or neglect.
Activities of daily living scale
This patient-reported outcome measure (PROM) is scored on a vertically oriented visual analogue scale (0–100) and consists of six key activities of daily living (ADL) derived from Warren’s study on hemianopic patients (Warren, Citation2009): Shopping, Meal Preparation, Personal Hygiene, Collisions, Getting Lost and Finding Things. The written prompt was, “Do you have difficulty in completing the following activities?” Participants rated each ADL at each time point, but were not able to see their previous ratings.
Visual field and neglect tests
In order to ascertain whether there had been any changes in the severity of participants’ hemianopia or neglect, we analysed data from two time points. Because we used an average of three visual field tests to establish the presence of hemianopia, we compared data from the middle of these (time point T1) to the final measure (T3). For the visual field test, 8 points were tested in each hemifield so we scored the number of missed or partially missed points at each of the two time points (range 0–8). As these data were not continuous, we used a within-subject non-parametric test (Wilcoxon Signed-rank test) to assess the significance of any change. For the neglect test, we used a continuous measure, the average co-ordinate on the x-axis (left–right) of all found targets. As this was a continuous measure, we used a paired t-test to assess the significance of any change. We assessed the effect of any significant change in hemianopia or neglect on visual search by carrying out bivariate (Pearson) correlations.
Statistical analysis
We performed repeated-measures ANOVAs to test our two main hypotheses: Does clinical diagnosis affect the outcome of Eye-Search therapy on (i) visual search and (ii) patient-reported outcome measures? For the visual search task, this was a three-way ANOVA with two within-subject factors (Therapy and Side) and one between-subjects factor (Group). The therapy factor had four levels: baseline, T1, T2 and T3, the side factor had two levels (affected and unaffected), and the group factor had four levels (left-sided hemianopia, right-sided hemianopia, neglect only, and neglect & hemianopia). Post hoc tests were carried out on each group separately to see if there was a significant main effect of therapy or not.
For the PROMs, a repeated-measures ANOVA was carried out on each of the six ADLs in turn. Here there was only one within-subjects factor, Therapy (4 levels, same as above) and one between-subjects factor, Group (4 levels, same as above). The significance level was set at the traditional cut-off of p < .05. Where sphericity assumptions were violated according to Mauchly’s test, we report the effects as adjusted by the Greenhouse–Geisser method.
We also calculated both unstandardized and standardized effect sizes for the visual search task for each of the four diagnostic groups. The unstandardized effect size was calculated as the percentage change (reduction) in average RT into the affected field between baseline (B) and T3 using the formula [(B−T3)/B]*100. The standardized effect size was calculated using a form of Cohen’s d that takes into account the fact that the before and after data are on the same subjects (within-subject) by including a correlation term (Faul et al., Citation2007).
Results
Visual search task
The omnibus ANOVA identified a significant interaction between Therapy × Side × Group, F(7.7, 1088) = 20.2, p = .001. With a significant main effect of Therapy F(2.5, 1038) = 30.9, p = .001. For the post hoc tests, three of the four diagnostic groups showed significant Therapy effects: neglect & hemianopia F(1.8, 77.1) = 10.27, p = .001; right-sided hemianopia F(2.8, 435.8) = 22.7, p = .001; and left-side hemianopia F(2.4, 498) = 36.4, p = .001. The neglect only group, however, demonstrated no significant main Therapy effect, F(1.9, 30) = 0.5, p = .599 (see ). Effect sizes for the three groups that showed a significant effect of therapy are presented in . Calculations are based upon changes to search times on the affected side only.
Figure 2. Mean visual search times (VST) in seconds into the affected (dark grey) and unaffected (light grey) fields for the four patient groups over the four time points (BL = baseline; T1, T2 and T3 = Time points 1, 2 and 3). The three groups where the post hoc tests demonstrated a main effect of Therapy in are shown with a *.
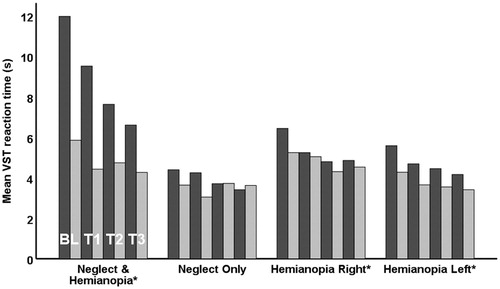
Table 1. The unstandardized (raw percentage change) and standardized (Cohen’s d) effect sizes.
Activities of daily living scale
ADLs where main hypothesis was supported (Therapy × Group interaction)
The “Finding Things” ADL was the only measure where the Therapy × Group interaction was significant and where the main hypothesis was supported F(8.3, 643.1) = 3.3, p = .001. Visual inspection of the data suggested that this was being driven by the same three groups as the visual search task (), so we investigated this formally by carrying out a post hoc analyse looking for therapy-induced changes in each diagnostic group in turn. Three groups showed a main effect of Therapy: left-sided hemianopia F(2.7, 543.4) = 19.9, p = .001; right-sided hemianopia F(2.5, 371.9) = 30.3, p = .001; and, neglect & hemianopia F(2.3, 92.8) = 7.3, p = .001. The neglect only group showed no main effect of Therapy F(2.3, 23.8) = 1.4, p = .254.
ADLs where there was a main effect of therapy
For three of the ADL scores, there was no Therapy by Group interaction but there was a main effect of therapy: “Shopping” F(2.7, 1082) = 8.9, p = .001; “Meal Preparation” F(2.7, 1072.8) = 3.4, p = .022; and, “Collisions” F(2.8, 1102) = 6.5, p = .001.
ADLs where there was no main effect of therapy
The remaining two ADLs, “Hygiene” and “Getting Lost,” showed neither a significant Therapy × Group interaction nor a main effect of Therapy: “Hygiene” F(2.8, 1128.2) = 0.893, p = .439; “Getting Lost” F(2.7, 1100.8) = 1.477, p = .222.
Visual field and neglect tests
We were able to analyse data on 348/368 (95%) of the participants with only hemianopia. The pre-therapy median was 6/8 points missed with a mode of 8, the mean was 5.9. Post-therapy the median and mode remained unchanged but the mean reduced to 5.6 (a 5% proportional reduction). We found a small but significant improvement in the extent of their visual field loss, Z = 3.58, p < .0001, r = .136. Importantly, there was no correlation between the change in visual field score and change in visual search times into the affected hemifield (T3–T1): r(346) = −.008, p = .886.
We were able to analyse data on 53/58 (91%) of the participants with neglect only or hemianopia and neglect. There was a small but non-significant improvement in the mean x-axis co-ordinate of their found targets: 123 pixels (T1) to 110 (T3), t(52) = .824, p = .414.
Discussion
This study has demonstrated the clinical effectiveness of Eye-Search therapy. Patients with hemianopia alone, or with neglect plus hemianopia, can expect their visual search times to improve after 1200 trials by ∼25% and ∼45%, respectively. This is associated with a concomitant improvement in self-reported measures of visual search: “finding things”. The neglect only group showed no significant improvements on either the impairment or self-reported measures of visual search.
For patients with hemianopia alone, the improvements seen in visual search are of a similar magnitude to our previous study that included 78 patients (24% improvement after 800 trials of Eye-Search therapy). The sample reported here is almost five times the size and is likely to be more representative of hemianopic patients in general. The unstandardized effect size is a little larger than that (16%) reported in a recent study of NeuroEyeCoachTM which uses a series of adaptive visual search trials (2400) that 296 patients completed online over a median period of 23 days, very similar to the 20 days for this study (Sahraie et al., Citation2020). In addition to these confirmatory results, we report two clinically novel findings. Firstly, by investigating effects in two different, albeit much small groups, we were able to provide evidence of syndrome specificity, that is, practice with visual search therapy seems to work in patients with co-existing neglect, but not on those with neglect alone. Secondly, and perhaps most importantly, we identified the same group-based interaction in the patients’ self-reported outcome measure (finding things) that most closely matched the impairment-based measure, suggesting that patients have good insight (even when they have neglect) into whether the therapy is working for them. Regarding the five other ADLs these results are largely confirmatory of our previous study. There was a main effect of therapy across the four groups for “Shopping”, “Meal Preparation” and, “Collisions” but no significant effect of therapy on “Hygiene” and “Getting Lost”, indicating that Eye-Search does not have a generalized effect on self-reported visuospatial functions.
Regarding the causative impairment itself, we found a small but significant improvement in patients’ visual fields between T1 and T3, probably driven by spontaneous recovery. This is unlikely to have driven the gains seen in visual search times as the effect sizes were out of keeping with each other (small for visual field and medium for visual search) and there was no correlation between the changes in patients’ visual fields and search times into their affected field. There was no significant improvement in patients’ neglect severity over the time of the study. The absence of a therapy effect in the neglect only group could be a false negative due to a small n (16), so more evidence is required before concluding that this represents a true lack of clinical effectiveness. However, this is not a big surprise, as eye-movement therapies directed at improving neglect tend to use stimuli that induce smooth-pursuit eye movements. Control therapies in these studies often require subjects to produce self-generated (voluntary) saccades, which do not lead to an improvement in symptoms (Kerkhoff et al., Citation2006, Citation2013, Citation2014). Importantly, the presence of neglect in patients with hemianopia as well does not seem to block the therapeutic effects of visual search training. This is an important finding as these patients are the most impaired in terms of both search times and ADLs and we found the biggest effect sizes in this group
Some limitations of this study deserve highlighting. Firstly, the participants self-selected, and are likely to be biased in some ways from the overall population with hemianopia and neglect. For example, they may not be representative in terms of the spectrum of severity seen in standard clinical populations. Regarding this, on the visual field test, the median field loss was 6/8 points per affected hemifield with the mode at 8/8 suggesting that patients had either a complete or partial hemianopia, consistent with the clinical observations in Zhang’s series of 904 patients (Zhang et al., Citation2006). It is much harder to be sure that this was also the case for the neglect patients as the test we used, while sensitive, is not standardized. Given this, it is possible that patients with milder neglect than seen in clinical settings took part. Secondly, the diagnostic tests were not carried out by qualified professionals on clinical-grade machinery, although the criterion validity of the visual field test is good compared with standard, Humphrey perimetry (Koiava et al., Citation2012) and the neglect test, with vanishing marks, is more sensitive than standard pen-and-paper tests of neglect (Gorgoraptis et al., Citation2012).
This research provides evidence to encourage therapists to recommend this as an effective therapy for patients with symptomatic hemianopia with or without neglect. This study also indicates that this therapy has a real-world improvement on self-reported measures related closely to the impairment-based intervention.
Acknowledgements
This publication presents independent research funded by the National Institute for Health Research (NIHR) and The Stroke Association. The views expressed are those of the author(s) and not necessarily those of The Stroke Association, the NHS, the NIHR or the Department of Health and Social Care.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
An anonymized version of the behavioural data and basic demographic variables (that preserves subject anonymity) are available from the PI, Professor Alex Leff ([email protected]), ORCID id: 0000-0002-0831-3541.
Additional information
Funding
References
- Corbetta, M., Kincade, M. J., Lewis, C., Snyder, A. Z., & Sapir, A. (2005). Neural basis and recovery of spatial attention deficits in spatial neglect. Nature Neuroscience, 8(11), 1603–1610. https://doi.org/10.1038/nn1574
- Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
- Gorgoraptis, N., Mah, Y. H., Machner, B., Singh-Curry, V., Malhotra, P., Hadji-Michael, M., Cohen, D., Simister, R., Nair, A., Kulinskaya, E., Ward, N., Greenwood, R., & Husain, M. (2012). The effects of the dopamine agonist rotigotine on hemispatial neglect following stroke. Brain, 135(8), 2478–2491. https://doi.org/10.1093/brain/aws154
- Hopfner, S., Cazzoli, D., Muri, R. M., Nef, T., Mosimann, U. P., Bohlhalter, S., Vanbellingen, T., & Nyffeler, T. (2015). Enhancing treatment effects by combining continuous theta burst stimulation with smooth pursuit training. Neuropsychologia, 74, 145–151. https://doi.org/10.1016/j.neuropsychologia.2014.10.018
- Jacquin-Courtois, S., Bays, P. M., Salemme, R., Leff, A. P., & Husain, M. (2013). Rapid compensation of visual search strategy in patients with chronic visual field defects. Cortex, 49(4), 994–1000. https://doi.org/10.1016/j.cortex.2012.03.025
- Kerkhoff, G., Bucher, L., Brasse, M., Leonhart, E., Holzgraefe, M., Volzke, V., … Reinhart, S. (2014). Smooth pursuit “bedside” training Reduces Disability and Unawareness During the activities of daily living in neglect: A randomized Controlled trial. Neurorehabilitation and Neural Repair, 28(6), 554–563. https://doi.org/10.1177/1545968313517757
- Kerkhoff, G., Keller, I., Ritter, V., & Marquardt, C. (2006). Repetitive optokinetic stimulation induces lasting recovery from visual neglect. Restorative Neurology and Neuroscience, 24(4-6), 357–369.
- Kerkhoff, G., Reinhart, S., Ziegler, W., Artinger, F., Marquardt, C., & Keller, I. (2013). Smooth pursuit Eye movement training Promotes recovery from Auditory and visual neglect: A randomized Controlled study. Neurorehabilitation and Neural Repair, 27(9), 789–798. https://doi.org/10.1177/1545968313491012
- Koiava, N., Ong, Y. H., Brown, M. M., Acheson, J., Plant, G. T., & Leff, A. P. (2012). A ‘web app’ for diagnosing hemianopia. Journal of Neurology, Neurosurgery & Psychiatry, 83(12), 1222–1224. https://doi.org/10.1136/jnnp-2012-302270
- Muller-Oehring, E. M., Kasten, E., Poggel, D. A., Schulte, T., Strasburger, H., & Sabel, B. A. (2003). Neglect and hemianopia superimposed. Journal of Clinical and Experimental Neuropsychology, 25(8), 1154–1168. https://doi.org/10.1076/jcen.25.8.1154.16727
- Ong, Y. H., Jacquin-Courtois, S., Gorgoraptis, N., Bays, P. M., Husain, M., & Leff, A. P. (2015). Eye-Search: A web-based therapy that improves visual search in hemianopia. Annals of Clinical and Translational Neurology, 2(1), 74–78. https://doi.org/10.1002/acn3.154
- Rowe, F. J., Hepworth, L. R., Howard, C., Hanna, K. L., Cheyne, C. P., & Currie, J. (2019). High incidence and prevalence of visual problems after acute stroke: An epidemiology study with implications for service delivery. PLoS One, 14(3), e0213035. https://doi.org/10.1371/journal.pone.0213035
- Sahraie, A., Cederblad, A. M. H., Kenkel, S., & Romano, J. G. (2020). Efficacy and predictors of recovery of function after eye movement training in 296 hemianopic patients. Cortex, 125, 149–160. https://doi.org/10.1016/j.cortex.2019.12.005
- Schuett, S., Heywood, C. A., Kentridge, R. W., Dauner, R., & Zihl, J. (2012). Rehabilitation of reading and visual exploration in visual field disorders: Transfer or specificity? Brain, 135(Pt 3), 912–921. https://doi.org/10.1093/brain/awr356
- Warren, M. (2009). Pilot study on activities of daily living limitations in adults with hemianopsia. American Journal of Occupational Therapy, 63(5), 626–633. https://doi.org/10.5014/ajot.63.5.626
- Wee, J. Y., & Hopman, W. M. (2008). Comparing consequences of right and left unilateral neglect in a stroke rehabilitation population. American Journal of Physical Medicine & Rehabilitation, 87(11), 910–920. https://doi.org/10.1097/PHM.0b013e31818a58bd
- Zhang, X., Kedar, S., Lynn, M. J., Newman, N. J., & Biousse, V. (2006). Homonymous hemianopias: Clinical-anatomic correlations in 904 cases. Neurology, 66(6), 906–910. https://doi.org/10.1212/01.wnl.0000203913.12088.93