ABSTRACT
The effectiveness of holistic neuropsychological rehabilitation for people with acquired brain injury has previously been demonstrated by means of standardized and routinely administered outcome measures. However, the most important outcomes from the perspective of former clients are largely unknown. This study explored the experience of participating in a holistic neuropsychological rehabilitation programme by conducting three focus groups with twelve former clients who had sustained a brain injury. Data were transcribed verbatim and analysed using thematic analysis. “It is an ongoing process” emerged as the overarching theme for the experience of recovery from brain injury. Four subthemes, or phases, were identified. Participants went through (1) a phase of confrontation, after which they (2) trained their skills and strategies, and (3) experimented with these in daily life. In the end, clients reached a phase of (4) coming to terms with their injury. Participants described increased levels of self-esteem, sense of competence, and adaptation as the most important outcomes of the programme, as these factors helped them regain a sense of identity. The results indicate that including these factors in outcome evaluations of complex interventions after brain injury may be important as they appear essential for capturing the client’s perspective on change.
Introduction
Acquired brain injury (ABI) is an umbrella term for all injuries to the brain that occur after birth such as stroke and traumatic brain injury (TBI). ABI is a significant health issue as it leads to long-term consequences in a variety of life domains, for example, physical functioning, cognitive functioning, emotional functioning, fatigue, and societal participation (Albrecht et al., Citation2019; Belmont et al., Citation2006; Draper et al., Citation2007; Rabinowitz & Levin, Citation2014). Problems in these domains can decrease quality of life (Steadman-Pare et al., Citation2001; Sturm et al., Citation2004), revealing a clear need for adequate treatment. Over the years, many types of interventions aimed at rehabilitating or supporting people with ABI have been developed. Given the multitude of consequences contributing to reduced quality of life (Verdugo et al., Citation2019), and the complex interaction between problems within multiple life domains (Gracey et al., Citation2009), evidence points towards the need for a holistic approach to neuropsychological rehabilitation with persons with ABI who experience cognitive, emotional and behavioural consequences, especially in the long term after the injury (Cicerone et al., Citation2019).
Holistic neuropsychological rehabilitation is offered in the post-acute and chronic phase after brain injury, it involves group as well as individual therapy and family counselling, and is offered by a multidisciplinary team of healthcare professionals (Wilson et al., Citation2017). The approach focusses on increasing awareness and acceptance of the consequences of the injury, developing strategies or compensatory skills to reduce cognitive, emotional, and communicative problems, and applying these strategies within functionally relevant settings in the pursuit of personally relevant goals (Wilson et al., Citation2017). The effectiveness of this type of rehabilitation has been established in a number of previous studies which found increases in cognitive and emotional functioning, participation, and life satisfaction, while decreasing caregiver burden (Cicerone et al., Citation2008; Goodwin et al., Citation2016; Holleman et al., Citation2016; Malec, Citation2001). Further, evidence suggests these effects are maintained in the long-term (Shany-Ur et al., Citation2020). However, most of these studies made use of standardized quantitative outcome measures designed by health care practitioners or researchers, which do not always capture the essence of change after the intervention, as they may omit the outcomes that are considered most important to the individuals themselves (Turner-Stokes, Citation2008; Turner-Stokes et al., Citation2005). Healthcare professionals have also expressed dissatisfaction with the process of outcome measurement in rehabilitation, as there seems to be a discrepancy in the outcomes as reported by clients during the programme and results on routine patient-reported questionnaires addressing functional outcome domains (e.g., executive functioning or mood). In 2011, one study qualitatively examined the experiences of holistic group rehabilitation according to people with mild TBI, and found a metatheme of “the process of change.” This theme referred to the accelerated pace at which participants became aware of their deficits and developed compensatory strategies to improve daily life functioning (Nilsson et al., Citation2011). However, the study focused on people with mild injuries, who have a different profile of difficulties and trajectory of recovery than people with moderate-severe injuries, with the latter more commonly associated with impaired self-awareness and identity changes (Hurst et al., Citation2020; Rochat et al., Citation2021).
Overall, previous research has evaluated holistic neuropsychological rehabilitation by means of predominantly quantitative, standardized outcome measures, or by including only a limited target group (e.g., persons with mild ABI). In order to assess clients’ experiences of rehabilitation after brain injury from a more individual perspective, Fish and colleagues conducted a pilot group interview, assessing client reflections on the most effective ingredients of holistic neuropsychological rehabilitation (Fish et al., Citation2018). This study suggested that the outcomes that matter most to clients are on a psychological, rather than a functional level, and are related to the sense of self and ways of relating to others. The main effects of the programme, as reported by former clients, were “a congruent sense of self” and “a new way of joining in” and thus were quite different from the outcomes frequently evaluated in quantitative outcome studies. More evidence is needed to confirm these preliminary findings, which bridge the gap between the scientific, professional, andclientviews on rehabilitation. Therefore, in the current study, we aimed to qualitatively examine former clients’ experiences of participating in a holistic neuropsychological rehabilitation programme, including persons with ABI of different types and a wide range of severity. We focused on former clients’ experiences of the programme in order to understand the course of their recovery, and to gain insight into which outcomes are considered most important to them.
Methods
Design
This study used qualitative methodology operationalized by focus groups. Focus groups were considered the most appropriate method as they are useful for evaluating complex issues that involve internal processes (Agan et al., Citation2008), and make use of social interactions between the clients. Focus groups can reveal various perspectives on the experience of life after brain injury, and uncover new insights into the most important rehabilitation outcome domains (Hennink, Citation2007). The researchers adopted a phenomenological approach in an attempt to capture the lived experiences that underlie a particular phenomenon, in this case, going through holistic neuropsychological rehabilitation after ABI (Langdridge, Citation2008). We report our study in accordance with the consolidated criteria for reporting qualitative research (Tong et al., Citation2007). Written informed consent was obtained from all participants. This study was reviewed and approved by the West Midlands – Solihull Research Ethics Committee (reference number 19/WM/0059).
Intervention to be reflected upon
The current study was conducted at the Oliver Zangwill Centre for Neuropsychological Rehabilitation, Ely, United Kingdom. All participants were former clients of an 18-week outpatient group-based holistic neuropsychological rehabilitation programme. The ABI specialist interdisciplinary rehabilitation team consists of clinical neuropsychologists, occupational therapists, speech and language therapists, and a clinical manager, supported by an administration team. The programme aims to reduce cognitive, emotional and communicative problems in the pursuit of personally relevant goals through psychoeducation, developing skills and compensation strategies, and increasing awareness and acceptance of the injury. Following referral, clients attend the centre for a two-day interdisciplinary assessment. Following assessment, the findings are drawn together in a psychological case formulation, which entails a description of the client’s needs, strengths, limitations and coping strategies (Wilson et al., Citation2017). Based on the formulation, a proposed treatment plan and initial goals are drawn up which are discussed with the client and family. If the holistic programme is considered appropriate for the person (in some cases an individual, the bespoke programme is considered more suitable), clients typically wait for a period of at least two months for a place within a programme cohort to become available. Each cohort typically consists of four clients. In the initial six-week intensive phase, clients visit the centre four days a week. This phase starts with a week-long induction, including various sessions designed to stimulate the group process and establish a therapeutic milieu. The induction week is followed by five weeks of group and individual sessions. The psychoeducational group sessions are attended each morning and are aimed at providing context and understanding of the brain injury and the associated consequences, and enabling clients to learn strategies to compensate for difficulties with cognition, communication and mood. During the afternoons, clients participate in individual assessment and therapy sessions with each member of the interdisciplinary team in the domains of mood, cognition, communication, and occupational therapy.
In the following community integration phase, which is typically 12 weeks long, clients visit the centre two days per week. During this phase, clients participate chiefly in individual sessions focused on applying strategies to everyday life in order to build confidence, set and work towards goals, and strengthen their sense of identity. Review meetings are scheduled at 3, 6 and 12 months after the end of the programme, to ensure maintenance of gains and further progress towards goals.
Detailed information on the programme can be found in the “brain injury rehabilitation workbook” (Winson et al., Citation2016).
Participants
Participants were former clients of the programme described above and were recruited by mail between January and April 2019. Former clients were eligible if they were 18 years or older and had completed a full rehabilitation programme at the centre. In order to capture long-term perspectives on rehabilitation, only those clients who finished the programme at least one year before participation in the study were included. Furthermore, they needed to be able to communicate sufficiently in order to participate in the focus groups, and be willing and able to travel to the centre. Clients who attended the programme between 2014 and 2018 were invited, as the structure and content of the programme remained stable over this period. Persons who acquired an additional brain injury since participating in the rehabilitation programme were excluded.
Procedures
Focus groups were limited to four participants per group to take into account differences in abilities between the participants. Participant recruitment was performed using a purposive sampling technique. We aimed to include clients from different clinical cohorts within each focus group to ensure a wide range of experiences were included. Therefore, one person from every cohort on the list of former clients who had indicated their interest in research participation was invited for participation in one of the focus groups. As a result, focus groups consisted of members of four different cohorts. An invitation letter, along with the participant information sheet and consent form, was sent by the centre’s secretary and potential participants were invited to respond to this invitation by telephone. Those who had not responded within one week were followed up by telephone. When former clients did not wish to participate, they did not need to provide a reason and were not followed up. When they needed more time to consider the invitation, another follow-up contact was planned. When former clients agreed to participate, they were presented with three potential times. When a sufficient number of participants was reached to set the date for a focus group, the secretary contacted the participants again to confirm this date. Participants brought the signed informed consent form to the appointment, where it was signed by one of the executive researchers. If they did not bring the form, participants and researchers signed a new one on-site. In total, 26 former clients were approached and 12 agreed to participate.
Research suggests that unstratified focus groups with a homogenous study population can reach thematic saturation in three to six iterations (Guest et al., Citation2017). Therefore, three focus groups were initially scheduled between April and June 2019, and subsequent focus groups would have been scheduled until no new themes emerged.
The focus groups were moderated by a facilitator (AD) and observer (DV). The facilitator interacted with participants to ensure they felt comfortable and encouraged to speak up, and asked for clarification when necessary. Further, the facilitator ensured all topics were discussed within the time available. The observer was responsible for the recordings, time keeping, and note-taking to summarize each topic. There were no other non-participants present. To manage the fatiguability associated with ABI, breaks were frequently provided according to the needs of the participants. A semi-structured topic guide was employed, which was piloted (Fish et al., Citation2018) and adjusted accordingly. Subsequently, the adjusted topic guide was proofread and approved by the client consultation committee of the centre. The client committee also recommended providing a layman’s version of the topic guide to the participants to assist their memory and their ability to keep track of the conversation. This lay topic guide was provided at the start of each meeting (Appendix 1) (Paterson & Scott-Findlay, Citation2002). The topic guide featured different types of questions (opening, introductory, transition, key, and ending) to assist the flow of the discussion (Morgan & Krueger, Citation1998). It encouraged participants to reflect on their entireclientjourney from brain injury onset to their current lives, and therefore covered the following subjects: (1) living with a brain injury before starting the rehabilitation programme, (2) experiences with participating in the programme, and (3) the most important outcomes of the programme in the long term.
Upon their arrival at the centre, participants were asked to wait in the common room and were offered a drink. The participants were then invited to the conference room, where they interacted casually with each other as well as the researchers until the focus group officially started. At the commencement of each focus group, the background and aims of the study were introduced and rules and regulations were explained (e.g., breaks were allowed at any point in time, participants were free to speak their mind, and confidentiality was ascertained). Subsequently, as a conversation starter, participants were asked to write one word on a post-it that described their current view on their life with brain injury, which were then placed on a whiteboard and discussed in the group. After this exercise, the topic guide was used to guide participants through a discussion of their experiences recovering from brain injury (1) before holistic neuropsychological rehabilitation, (2) during the programme, and (3) after the programme. After each topic, the observer assisted the facilitator by presenting their summary of the foregoing discussion to review participant agreement (Hennink, Citation2007). When all topics had been covered, participants were given the opportunity to elaborate on anything they still wanted to discuss, and then the meeting was closed. Focus groups were audiotaped as well as video recorded to capture verbal and non-verbal communication and to serve as back-up if either of the two recorded inaudible speech. All groups lasted between 120 and 180 min (frequent breaks included).
Data analysis
All videotapes were transcribed verbatim per focus group by AD, DV, and the secretary of the centre. Audiotapes were used in case the videotape was unintelligible. Non-verbal communications were noted between square brackets (e.g., [laughter]). The transcripts and observations were analysed in light of the research questions. Analyses were performed independently by two researchers (AD and DV) to allow for alternative interpretations. A thematic analysis approach was adopted, in which common themes and categories emerged using inductive reasoning and constant comparison (Braun & Clarke, Citation2006). All transcripts were thoroughly read by AD and DV, after which open codes were identified by the researchers using the qualitative analysis software ATLAS.ti version 7.0 (Muhr, Citation2013). Each focus group was coded individually using a close coding technique and codes referring to the same phenomenon were grouped into categories. The categories of the first focus group gave substance to a coding framework. This coding framework was then expanded with novel categories arising from the second focus group. As the third focus group did not reveal any novel categories, the codes of the third focus group were added to categories that had arisen from the previous focus groups. This final framework was then used to identify higher-order themes. A coding example is displayed in .
Table 1. Simplified coding example of the theme “confrontation”.
Discrepancies in coding and categorizing between AD and DV were discussed to share alternative interpretations. In cases where a consensus could not be reached, a third researcher (JF) was consulted. Quotations describing the categories and themes were selected based on representativeness by AD and checked for relevance by all other authors. AD and DV independently compared the third focus group to the previous two and found no new themes emerged (Krueger, Citation1997a).
Research team reflexivity
The first and third focus groups were moderated by a PhD Candidate with a background in clinical neuropsychology, whose research focuses on outcome measurement and the evaluation of interventions for people with brain injury (author AD, female, four years experience working with people with ABI). The second focus group was moderated by a PhD Candidate with a background in clinical neuropsychology, whose research focuses on long-term psychosocial outcome after brain injury (author DV, male, five years experience working with people with ABI). Both researchers were previously trained in conversation techniques and conducting focus groups. Moreover, both were involved in setting up the research protocol and therefore were aware of the research background and aims. Neither of the focus group moderators knew the participants prior to data collection, nor had they been involved in delivering the rehabilitation treatment. Both researchers introduced themselves and their research interests at the start of each focus group.
Findings
Participants
Three focus groups with four participants each were organized (n = 12). All participants of each focus group originated from separate clinical cohorts. All participants had completed the programme 1–5 years before participating. Demographic characteristics of pseudonymised participants are displayed in .
Table 2. Participant characteristics.
Content analysis
The analysis revealed an overarching topic, or metatheme, of “It is an ongoing process,” reflected by the fact that overcoming a brain injury is an ongoing process which is facilitated by, but not limited to the time spent in rehabilitation. However, the programme was considered vital for bringing about change. When assessing the trajectory of recovery and experience of participating in holistic neuropsychological rehabilitation in greater depth, four subthemes or phases, were distinguished, which characterized the course of rehabilitation: “confrontation” in the assessment and early rehabilitation phase, “training” in the first weeks of the intensive programme, “experimentation” in the integration phase of the programme, and “coming to terms” in the months or years after the programme. A threefold category, characterized as “influential factors,” had an impact on all aspects of rehabilitation: “governmental systems,” “family and friends,” and “community.” In the following paragraphs, the themes and influencing factors are presented in detail.
Confrontation
Before commencing rehabilitation, participants reported they had tried to continue living their lives as they did before their brain injury. In doing so, they were confronted with the impact of the consequences of their brain injury on a daily basis, which led to frustration, insecurity, and isolation. The brain injury disrupted many aspects of the participants’ lives and interfered with their interpersonal relationships. Some reported taking their frustration out on their loved ones.
And after I [was] getting frustrated at the wrong people, like you said (Jack), your family, you take it home with you and you get frustrated […] If it’s someone like your partner or your brother, you can do that, for some reason you find it’s acceptable. Whereas if you did that to someone in the pub they’d probably punch you in the mouth. (Adam)
I think one of the biggest problems I had was I didn’t know how ill I was. So I had three relatively young children, and part of my brain thought I was okay. So I would get up to walk somewhere and end up falling over because I forgot that I couldn’t really walk. (Mary)
I just felt broken somehow – you know, just couldn’t quite understand why but just knew something wasn’t right. I couldn’t explain why, but I just didn’t want to be around people. I had lost my zest for life really, I had no passion, I had no drive. You know, even not wanting to be around my kids and stuff. It was all just too much. I just couldn’t cope really. That’s how it felt. Or just trying to and getting more and more overwhelmed. (Betty)
I used to think there was nothing wrong with me. I refused to acknowledge the strokes. I refused to acknowledge that they were going to have that impact on me. However, when I came here, I realised that – during the day, you come here and you have that big A4 sheet of paper and as well as the A4 sheet of paper on the board? We went through the same kind of process and they tell you what’s wrong with you and all that, do you remember? We got the A4 sheet of paper and it described me. I didn’t recognize the person on there – I thought they were talking about someone else. (James)
And then once you start talking about it and learning what’s happened to you, and you know that more things are wrong with you than you think, that’s when it’s like “no, this isn’t fun anymore”. (Anna)
Cause you go on that journey here. You think “Right, I’m really proud”, then “oh my god, I’m really bad”, then “actually, I’m even worse than I thought I was”. Because that’s what it does to you. And then it suddenly starts building up a little bit. (Eve)
Training
During the training phase, rehabilitation clients are exposed to the different modules of the programme. An important module was “understanding my brain injury,” in which they learned what exactly had happened to them. Participants acknowledged the specialized staff knowledge on the subject which enhanced the feeling of being understood. This factual approach allowed participants to differentiate their identity from the problems they perceived, or, as one participant called it, “co-exist with their brain injury.”
Biggest memory for me, I think, was the realisation that the way that I was acting wasn’t my fault. (Jack)
Positive experiences, warmth of staff, relaxed environment helped. (Charles)
But I definitely thought it was helpful, giving you little strategies of “ok if this is the situation and this is the challenge”, then maybe “why don’t you look at it like this”? And even like things that I knew I was going to – events that I thought I was going to – where I was going to be worried about who I was going to talk to and who I was going to know – and it was ok, let’s write down the things that I worried about and how can I deal with this situation if it arises. (Tamara)
Experimenting
The experimental phase was marked by finding out which strategies work and which do not, while reintegrating into society. Participants described this phase as testing and often failing, transitioning from the protective environment of the rehabilitation centre to everyday life.
Yeah, you had stopped being a total hermit, you were making a bit of progress, so you were pushing your own boundaries and you thought you had all these wonderful mechanisms to help you, and then they all fell (laughs). (Mary)
I got to the stage where I had had enough. I needed to stop – I needed to go and try and get back out there. (Eve)
Coming to terms
The last phase represented coming to terms, as the acquired strategies transferred to daily life and improved functioning. Participants described that, in this phase, they automatically made use of what they learned and found a way to work around their problems. However, participants did not regard an improvement in functioning (e.g., as a result of adequate strategy use) the most important outcome of the programme. Instead, they stressed the fact that most (cognitive) problems are still present, but reported an increased feeling of empowerment, consisting of an increased sense of competence and self-esteem, substantiated by a re-established sense of identity and coherent sense of self.
[There now is a lot of] Calm. In some places that are just totally out of control and completely overwhelming, there is – sometimes I just think “OK, I’m feeling like this because of this; I need to get out of this situation – what am I going to do?" You know, whereas before I would have just been like a rabbit in the headlights. […] [The programme] I think shows you – all of the tiny things that they’re giving you are helping you to build up confidence, helping you to see, “all right, this part’s not great” but you have this thing that you can try to use to help you with that. […] One thing that I have really, really learned is I have brain injury but it doesn’t define me. (Eve)
I think that’s the “different” rather than “worse”, it’s not always worse. There are some bits, some things that we learn which are actually better and nicer. So, yeah, I would try to avoid “worse”, and go for “different”. (Mary)
Yes, it’s just having that balance of having enough to do that you can achieve it, rather than having too much and making – not mistakes, but not being able to complete stuff. (Jack)
People have no idea of the other stuff, and the energy and the effort that it takes to maintain that. So, it makes life very different you’ve got to prioritise so much from the minute that you wake up. I am a “complete finisher” by nature, which means that I would work until it is finished. (Mary)
The long-term effect perhaps has yet to manifest itself and maybe it’s still sinking in, maybe the therapy is having an effect which I’m not aware of and perhaps I will realise that later in my life. Perhaps that’s what the programme is meant to do, you know – equip you with strategies and techniques to support you throughout life, and I’m not aware of those yet. (Daniel)
I think part of the recovery process is the acceptance of what has happened to you. You accept what you’ve been told. When people have told you that you have had a stroke and these could be the following problems that could incur, or whatever – but I know when I had my heart attack everyone kept telling me that my memory potentially would be shot and I wouldn’t remember my wife or my children or anything like that but I dismissed everything that I said because I knew in myself that all I had to do was get myself better, get out of here and get back to work. And that’s all, and it was only over time that I realised that it’s that acceptance of what has happened to you, which I didn’t see at first when I was in recovery. (John)
Honestly, I don’t think there was ever a point where I had this big moment and thought, “I’ve cracked this”. I think it’s ongoing and I think it always will be. I think – I mean, this place – like I said, it absolutely saved my life, it absolutely did. I think it’s given me a massive understanding of my brain injury, what I’ve been left with, coping strategies, and self-compassion and that I’m alright and that I can be alright for my kids and my family and that I can move on and what will be, will be. It doesn’t always feel like that but you know, there is hope –definitely. (Eve)
Influential factors
Several environmental factors were said to have an influence on overcoming the consequences of a brain injury in general, and participating in rehabilitation specifically. Firstly, governmental systems such as regulations around employee insurance and general healthcare had an impact on being referred to the centre, and eventually, their financial situation. In regard to general healthcare, participants experienced a lack of recognition and understanding of a brain injury and insufficient interdisciplinary communication.
The corporate health people were just doing things by the book you know. They didn’t realise the consequences of my stroke so they weren’t actually treating it, so [the holistic rehabilitation facility] was more specific to my condition. (Harry)
Next to governmental systems, family and friends played a large role throughout the rehabilitation process. In some occasions, family and friends were the ones to initiate rehabilitation. All participants stressed the importance of the support they received from their family and friends during rehabilitation. Further, they acknowledged that having a brain injury can be a heavy burden to their loved ones and believed that the people around them also benefited from the programme, and that helped to apply the strategies the participants have learned.
Lastly, the community that participants lived in was considered important for their level of functioning and the way they view themselves. Participants often felt misunderstood by people in their surroundings. They feel there is too little public awareness of the chronic consequences of brain injury and some participants experienced similar problems when returning to work. Thus, on the one hand, the fact that the consequences of brain injury are often invisible may lead to a lack of understanding. On the other hand, participants describe being reluctant to inform others of their brain injury because there might be a stigma to it. This may impede successful implementation of the skills and strategies learned.
But then it makes it difficult on yourself then. Because in some areas, you don’t want to push your brain injury forward, you don’t want people then to judge you for having a brain injury. (Jack)
Discussion
This study explored client experiences of participating in a holistic neuropsychological rehabilitation programme after having acquired a brain injury. A metatheme “it is an ongoing process” was found, reflected by four stages of recovery; confrontation, training, experimenting, and coming to terms. All phases were influenced by interaction with family/friends, community and governmental systems. Participants reported being more in control after attending the programme. Although they feel more able to adapt to life events, they stress that coming to terms with their injury is an everlasting process, in which they increasingly experience their brain injury to be a part of their identity, rather than definingit.
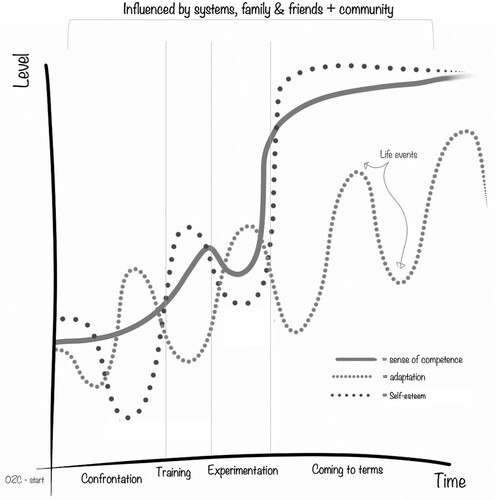
In general, the programme was considered effective for increasing everyday functioning, which is in line with previous effectiveness studies into holistic neuropsychological rehabilitation (Cicerone et al., Citation2008; Goodwin et al., Citation2016; Holleman et al., Citation2016; Malec, Citation2001). Corresponding with the findings of Nilsson et al. (Citation2011), this study emphasizes the process of change over time. This process is characterized by an initial confrontation with the problems in the beginning of the programme, after which participants found that the different components of holistic rehabilitation sparked a change in the way they viewed themselves and their place in the world. An important difference was the subtheme “work” that was found by Nilsson et al., which is likely specific to their mild brain injury sample. The current study included former clients with mixed ABI severity levels, and many were unable to return to work. As a result, they potentially experienced an even larger self-discrepancy, meaning that increased levels of self-esteem, sense of competence, and adaptation were regarded as the main outcomes of the programme. presents a graphic interpretation of the metatheme (ongoing process) including the four stages of recovery, the influential factors (family and friends, community, and government) and the accompanying changes in the three transcendent psychological domains (self-esteem, sense of competence, and adaptation). The figure does not represent empirical data, but rather reflects the course of experiences as reported by the participants.
Figure 1. The model of former clients’ experiences of participating in holistic neuropsychological rehabilitation.
Note: Confrontation (first phase): clients are confronted with their problems and experience consequential decrease in self-esteem, which then increases with learning about (preserved) strengths. Adaptation capacity fluctuates as a result of life-events, but is generally on a low level. Sense of competence slowly increases in anticipation of the training phase. Training (second phase): clients learn to understand their injuries and acquire skills and strategies, leading to an increased sense of competence and self-esteem. Experimentation (third phase): clients apply what they have learned to everyday life. They experience that not all acquired skills are effective in everyday life, leading to a decreased sense of competence, and experience failure, leading to a decreased level of self-esteem. Coming to terms (fourth and final stage): clients learn to cope with their injuries and show a coherent sense of self, consisting of high levels of sense of competence and self-esteem. Adaptation capacity remains under the influence of life-events, but is increased in general. All factors are influenced by environmental factors, which can both be beneficial or detrimental, depending on individual situations.
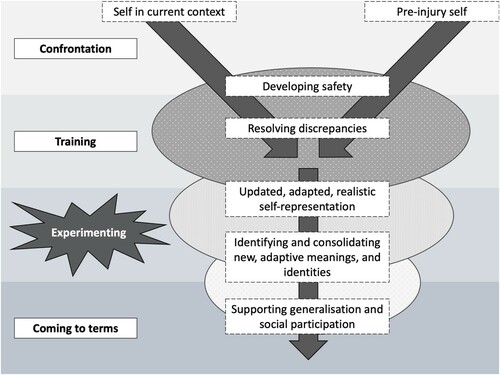
This study’s findings are consistent with the change process underpinning complex rehabilitation interventions, often referred to as the “Y-shaped model” (Gracey et al., Citation2009). The Y-shaped model is based on research into mechanisms behind psychotherapy, as this type of intervention too is multifaceted and therefore difficult to evaluate by means of delimited outcome domains (Whyte & Hart, Citation2003). It describes that persons with ABI first experience a sense of discrepancy between their aspired self and their self in the new context (with a brain injury), as reflected by the “confrontation phase” during which the assessments as part of the programme increased the awareness of these discrepancies. In the next phase of the y-shaped model, the therapeutic milieu ascertains a safe environment in which people can try to resolve these discrepancies through the different components of the programme; the “training phase". Subsequently, the newly set goals and the skills and strategies that people acquire to reach these new goals in a social context consolidate over time and ultimately lead to a re-established sense of identity (Gracey et al., Citation2008). As identity arguably is composed of self-evaluative properties like sense of competence and self-esteem (Stets & Burke, Citation2014), this shift likely is reflected by the “coming to terms phase". The finding that living a meaningful life after a brain injury is an ongoing process has also been described by Woodman et al. (Citation2014). In their review, it is explained that the trajectory towards social participation after stroke is composed of change and disruption, pursuing personal changes, perceived magnitude of individual barriers, building individual confidence and evaluating personal meaning. A schematic overview of the y-shaped model and associated phases are displayed in .
Figure 2. Schematic overview of the y-shaped model and the associated phases of holistic neuropsychological rehabilitation. Adapted from Gracey et al. Citation2009. (Gracey et al., Citation2009).
The decrease in self-esteem and sense of competence experienced during the "experimentation phase" is not emphasized within the y-shaped model; however, difficulty returning home after rehabilitation is a well-known phenomenon which has previously been documented (Beunder et al., Citation2015; Gustafsson & Bootle, Citation2013; Hodson et al., Citation2016). It is often referred to informally among the healthcare professionals involved in holistic rehabilitation as the “u-bend,” symbolizing a sudden dip in self-appreciation when the reintegration phase of rehabilitation commences and clients worry about what would happen when the supports associated with the programme were taken away. This u-bend has important implications for outcome measurement, as participants mention that the material “needs to sink in.” As the duration of this phase may differ from one client to the other, the optimal moment to measure post-programme change may be difficult to pinpoint in time. This might mask potential treatment effects in cases where the follow-up period is relatively brief, or where statistical methods based on group means are used, as these are relatively insensitive to individual trajectories of recovery (Bonanno et al., Citation2011).
The impact of personal factors such as personality and coping styles on the outcome of ABI has previously been examined (Sela-Kaufman et al., Citation2013; Van Mierlo et al., Citation2015; Wardlaw et al., Citation2018), with factors such as psychological resilience, coping style, and perseverance being determinants of (functional) outcome. In addition, the finding that governmental systems, family and friends, and community are important for overcoming a brain injury was consistent with a previous study into the healthcare needs of people with brain injury (Stiekema et al., Citation2020). The authors suggest that appointing a case manager to persons with brain injury could support them and their significant others and guide them through the healthcare system and community. This recommendation is endorsed by our findings.
Strengths and limitations
The current study was conducted among a heterogeneous sample of former clients of a holistic neuropsychological rehabilitation programme and spanned the entireclientjourney over a minimum of two years. Using purposive sampling, we established focus groups with participants from different cohorts, capturing different phases in the recovery process. As we managed to include a large proportion of the eligible participants, we have reflected the diverse experiences of participants who attended and completed the holistic rehabilitation programme during this time frame. The researchers were independent of the rehabilitation programme, minimizing moderator bias (Krueger, Citation1997b). The fact that this study is composed of client perspectives that were collected by means of systematic qualitative research methods allows for a deepened analysis of the effects of the programme as compared to conclusions drawn on the basis of questionnaire, test, or goal-based data.
This study also has limitations. Due to the purposive sampling method, the inclusion criteria, and the need to travel to the centre to participate, there might have been a sampling bias towards clients with a higher level of functioning, and clients who felt motivated to express their appreciation for the programme. In addition, as a result of the study location, local clients whose rehabilitation was funded by NHS commissioners were more likely to participate than privately-funded clients, who typically reside further from the centre. Further, as mostclientss experience cognitive problems, there might have been a recollection bias to their reports. As a result of the research design, the changes reported by the participants cannot be attributed to the programme specifically and could be a result of mere time, although this is unlikely given there is evidence from controlled trials that the programme is effective.
Future directions
The current findings have implications for clinical practice. They indicate that rehabilitation clients need to be prepared for the phases that lie ahead, and to recognize that brain injury is a chronic condition characterized by ongoing and changing experiences. Further, the incorporation of more follow-up visits could allow clinicians to check on the “ongoing process” in order to signal problems, or reinforce further growth. This study also has important implications for outcome measurement of neuropsychological rehabilitation. Traditionally, outcome measurement has been centred around measuring functional outcome (Ownsworth & Haslam, Citation2016; van Heugten et al., Citation2019). However, when interventions become more complex, as is the case for holistic neuropsychological rehabilitation, these outcome domains might not be considered the most important by clients. Consequently, this leads to a discrepancy between the perceived and objective effect of a treatment, and an apparent difficulty in demonstrating the effectiveness of these interventions to service providers and commissioners (Wade, Citation2020). Although qualitative assessment methods presumably are best suited to understand all aspects of a treatment effect, such methods would be too time-consuming to use in routine care (Gracey et al., Citation2008). One could argue that the extent to which someone reintegrates into society, or, the level of social participation, is the ultimate outcome of rehabilitation (Wade, Citation2020). However, participation is a complex construct (Woodman et al., Citation2014) and measuring it may be subject to many factors other than the impact of the injury. Therefore, participation might be too “distant” from actual effectiveness to be used as an outcome measure for rehabilitation (Domensino & Heugten, Citation2020). Similarly, using quality of life as treatment outcome can be problematic, as it might be obscured by factors other than those that can be addressed by rehabilitation interventions. We, therefore, recommend measurement of concepts valued by former clients, which are self-esteem, sense of competence, and adaptation. Increases in these concepts as a result of treatment, alongside functional improvement, should be recognized as an important effect of these complex interventions.
Conclusion
Holistic neuropsychological rehabilitation is considered effective by former clients. Overcoming a brain injury is considered an ongoing process, which is facilitated by, but not limited to the time spent in rehabilitation. Participants of the programme go through a phase of confrontation, after which they train their skills and strategies, and experiment with these in daily life. In the end, clients reach a phase of coming to terms, in which levels of self-esteem, sense of competence, and capacity for adaptationhaveincreased, and a sense of identity is regained. Future research should reconsider the most important outcome domains for evaluation of complex interventions, as the essence of change may be in transcending psychological factors, rather than functional outcome.
Author contributions
AB, BW, JF, JW, RP and CvH designed the study. AB and LP guided practical execution on site. AD and DV acquired and analysed the data, and all authors interpreted the data after processing.
Acknowledgements
The authors would like to thank all former clients who took the time and effort to participate in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Agan, J., Koch, L. C., & Rumrill, P. D. Jr. (2008). The use of focus groups in rehabilitation research. Work, 31(2), 259–269.
- Albrecht, J. S., Barbour, L., Abariga, S. A., Rao, V., & Perfetto, E. M. (2019). Risk of depression after traumatic brain injury in a large national sample. Journal of Neurotrauma, 36(2), 300–307. https://doi.org/10.1089/neu.2017.5608
- Belmont, A., Agar,N., Hugeron,C., Gallais,B., & Azouvi, P. (2006). Fatigue and traumatic brain injury. In Annales de réadaptation et de médecine physique. Elsevier.
- Beunder, C., Dekker, J. H., Brasser, J. A., & Depla, M. F. (2015). Thuis na een CVA:‘Dan begint het pas’. Een kwalitatief onderzoek naar de behoefte aan nazorg van CVA-patiënten na terugkeer naar huis. Tijdschrift voor Gerontologie en Geriatrie, 46(4), 196–203. https://doi.org/10.1007/s12439-015-0139-z
- Bonanno, G. A., Westphal, M., & Mancini, A. D. (2011). Resilience to loss and potential trauma. Annual Review of Clinical Psychology, 7(1), 511–535. https://doi.org/10.1146/annurev-clinpsy-032210-104526
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Cicerone, K. D., Goldin, Y., Ganci, K., Rosenbaum, A., Wethe, J. V., Langenbahn, D. M., … Harley, J. P. (2008). A randomized controlled trial of holistic neuropsychologic rehabilitation after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 89(12), 2239–2249. https://doi.org/10.1016/j.apmr.2008.06.017
- Cicerone, K. D., Mott, T., Azulay, J., Sharlow-Galella, M. A., Ellmo, W. J., Paradise, S., & Friel, J. C. (2019). Evidence-Based cognitive rehabilitation: Systematic review of the literature from 2009 through 2014. Archives of Physical Medicine and Rehabilitation, 100(8), 1515–1533. https://doi.org/10.1016/j.apmr.2019.02.011
- Domensino, A. F., Heugten, C. v., & De expertgroep. (2020). Van de 15-woordentest naar ‘Heb ik nu wel alle boodschappen gedaan?’: Het meten van cognitief functioneren op het continuüm van de kunstmatige testsituatie tot het dagelijks leven. Tijdschrift voor neuropsychologie.
- Draper, K., Ponsford, J., & Schönberger, M. (2007). Psychosocial and emotional outcomes 10 years following traumatic brain injury. Journal of Head Trauma Rehabilitation, 22(5), 278–287. https://doi.org/10.1097/01.HTR.0000290972.63753.a7
- Fish, J., Prince, L., & Winegardner, J. (2018). “Finding the confidence to crack on with things”: A qualitative study of client reflections on holistic neuropsychological rehabilitation several years post-programme. In 15th Neuropsychological Rehabilitation Special Interest Group of the WFNR, Prague.
- Goodwin, R. A., Lincoln, N. B., & Bateman, A. (2016). Dysexecutive symptoms and carer strain following acquired brain injury: Changes measured before and after holistic neuropsychological rehabilitation. NeuroRehabilitation, 39(1), 53–64. https://doi.org/10.3233/NRE-161338
- Gracey, F., Evans, J. J., & Malley, D. (2008). “Feeling part of things”: personal construction of self after brain injury. Neuropsychological Rehabilitation, 18(5-6), 627–650. https://doi.org/10.1080/09602010802041238
- Gracey, F., Evans, J. J., & Malley, D. (2009). Capturing process and outcome in complex rehabilitation interventions: A “Y-shaped” model. Neuropsychological Rehabilitation, 19(6), 867–890. https://doi.org/10.1080/09602010903027763
- Guest, G., Namey, E., & McKenna, K. (2017). How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods, 29(1), 3–22. https://doi.org/10.1177/1525822X16639015
- Gustafsson, L., & Bootle, K. (2013). Client and carer experience of transition home from inpatient stroke rehabilitation. Disability and Rehabilitation, 35(16), 1380–1386. https://doi.org/10.3109/09638288.2012.740134
- Hennink, M. M. (2007). International focus group research: A handbook for the health and social sciences. Cambridge University Press.
- Hodson, T., Aplin, T., & Gustafsson, L. (2016). Understanding the dimensions of home for people returning home post stroke rehabilitation. British Journal of Occupational Therapy, 79(7), 427–433. https://doi.org/10.1177/0308022615619420
- Holleman, M., Vink, M., Nijland, R., & Schmand, B. (2016). Effects of intensive neuropsychological rehabilitation for acquired brain injury. Neuropsychological Rehabilitation, 1–14. https://doi.org/10.1080/09602011.2016.1210013
- Hurst, F. G., Ownsworth, T., Beadle, E., Shum, D. H., & Fleming, J. (2020). Domain-specific deficits in self-awareness and relationship to psychosocial outcomes after severe traumatic brain injury. Disability and Rehabilitation, 42(5), 651–659. https://doi.org/10.1080/09638288.2018.1504993
- Krueger, R. A. (1997a). Analyzing and reporting focus group results (Vol. 6) Sage Publications.
- Krueger, R. A. (1997b). Moderating focus groups (Vol. 4). Sage Publications.
- Langdridge, D. (2008). Phenomenology and critical social psychology: Directions and debates in theory and research. Social and Personality Psychology Compass, 2(3), 1126–1142. https://doi.org/10.1111/j.1751-9004.2008.00114.x
- Malec, J. F. (2001). Impact of comprehensive day treatment on societal participation for persons with acquired brain injury. Archives of Physical Medicine and Rehabilitation, 82(7), 885–895. https://doi.org/10.1053/apmr.2001.23895
- Morgan, D. L., & Krueger, R. A. (1998). Developing questions for focus groups. Sage.
- Muhr, T. (2013). ATLAS. ti (Version 7.0. 89) [Computer software]. Atlas. ti GmbH.
- Nilsson, C., Bartfai, A., & Löfgren, M. (2011). Holistic group rehabilitation–a short cut to adaptation to the new life after mild acquired brain injury. Disability and Rehabilitation, 33(12), 969–978. https://doi.org/10.3109/09638288.2010.528141
- Ownsworth, T., & Haslam, C. (2016). Impact of rehabilitation on self-concept following traumatic brain injury: An exploratory systematic review of intervention methodology and efficacy. Neuropsychological Rehabilitation, 26(1), 1–35. https://doi.org/10.1080/09602011.2014.977924
- Paterson, B., & Scott-Findlay, S. (2002). Critical issues in interviewing people with traumatic brain injury. Qualitative Health Research, 12(3), 399–409. https://doi.org/10.1177/104973202129119973
- Rabinowitz, A. R., & Levin, H. S. (2014). Cognitive sequelae of traumatic brain injury. Psychiatric Clinics of North America, 37(1), 1–11. https://doi.org/10.1016/j.psc.2013.11.004
- Rochat, L., Renaud, O., Arnould, A., Lardi Robyn, C., Barbot, F., Azouvi, P., & Van der Linden, M. (2021). Self-defining memories after severe traumatic brain injury: A preliminary study. Journal of Neuropsychology, 15(1), 112–128. https://doi.org/10.1111/jnp.12212
- Sela-Kaufman, M., Rassovsky, Y., Agranov, E., Levi, Y., & Vakil, E. (2013). Premorbid personality characteristics and attachment style moderate the effect of injury severity on occupational outcome in traumatic brain injury: Another aspect of reserve. Journal of Clinical and Experimental Neuropsychology, 35(6), 584–595. https://doi.org/10.1080/13803395.2013.799123
- Shany-Ur, T., Bloch, A., Salomon-Shushan, T., Bar-Lev, N., Sharoni, L., & Hoofien, D. (2020). Efficacy of postacute neuropsychological rehabilitation for patients with acquired brain injuries is maintained in the long-term. Journal of the International Neuropsychological Society, 26(1), 130–141. https://doi.org/10.1017/S1355617719001024
- Steadman-Pare, D., Colantonio, A., Ratcliff, G., Chase, S., & Vernich, L. (2001). Factors associated with perceived quality of life many years after traumatic brain injury. Journal of Head Trauma Rehabilitation, 16(4), 330–342. https://doi.org/10.1097/00001199-200108000-00004
- Stets, J. E., & Burke, P. J. (2014). Self-esteem and identities. Sociological Perspectives, 57(4), 409–433. https://doi.org/10.1177/0731121414536141
- Stiekema, A. P. M., Winkens, I., Ponds, R., De Vugt, M. E., & Van Heugten, C. M. (2020). Finding a new balance in life: A qualitative study on perceived long-term needs of people with acquired brain injury and partners. Brain Injury, 34(3), 421–429. doi:10.1080/02699052.2020.1725125
- Sturm, J. W., Donnan, G. A., Dewey, H. M., Macdonell, R. A., Gilligan, A. K., Srikanth, V., & Thrift, A. G. (2004). Quality of life after stroke: The North East Melbourne stroke incidence study (NEMESIS). Stroke, 35(10), 2340–2345. https://doi.org/10.1161/01.STR.0000141977.18520.3b
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042
- Turner-Stokes, L., Nair, A., Sedki, I., Disler, P. B., & Wade, D. T. (2005). Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database of Systematic Reviews, (12). doi:10.1002/14651858.CD004170
- Turner-Stokes, L. (2008). Evidence for the effectiveness of multi-disciplinary rehabilitation following acquired brain injury: A synthesis of two systematic approaches. Journal of Rehabilitation Medicine, 40(9), 691–701. https://doi.org/10.2340/16501977-0265
- van Heugten, C., Caldenhove, S., Crutsen, J., & Winkens, I. (2019). An overview of outcome measures used in neuropsychological rehabilitation research on adults with acquired brain injury. Neuropsychological Rehabilitation, 30(8), 1598–1623. doi:10.1080/09602011.2019.1589533
- Van Mierlo, M. L., Van Heugten, C. M., Post, M. W., De Kort, P. L., & Visser-Meily, J. M. (2015). Psychological factors determine depressive symptomatology after stroke. Archives of Physical Medicine and Rehabilitation, 96(6), 1064–1070. https://doi.org/10.1016/j.apmr.2015.01.022
- Verdugo, M. A., Fernández, M., Gómez, L. E., Amor, A. M., & Aza, A. (2019). Predictive factors of quality of life in acquired brain injury. International Journal of Clinical and Health Psychology, 19(3), 189–197. https://doi.org/10.1016/j.ijchp.2019.06.004
- Wade, D. T. (2020). What is rehabilitation? An empirical investigation leading to an evidence-based description. SAGE Publications.
- Wardlaw, C., Hicks, A. J., Sherer, M., & Ponsford, J. L. (2018). Psychological resilience is associated with participation outcomes following mild to severe traumatic brain injury. Frontiers in Neurology, 9, 563. https://doi.org/10.3389/fneur.2018.00563
- Whyte, J., & Hart, T. (2003). It’s more than a black box; it’sa Russian doll: Defining rehabilitation treatments. American Journal of Physical Medicine & Rehabilitation, 82(8), 639–652.
- Wilson, B. A., Winegardner, J., van Heugten, C. M., & Ownsworth, T. (2017). Neuropsychological rehabilitation: The international handbook. Psychology Press.
- Winson, R., Wilson, B. A., & Bateman, A. (2016). The brain injury rehabilitation workbook. Guilford Publications.
- Woodman, P., Riazi, A., Pereira, C., & Jones, F. (2014). Social participation post stroke: A meta-ethnographic review of the experiences and views of community-dwelling stroke survivors. Disability and Rehabilitation, 36(24), 2031–2043. https://doi.org/10.3109/09638288.2014.887796
Appendix 1. Lay topic guide.
![]()
