ABSTRACT
The study aimed to determine the respiratory effects of solvents among workers in the Mauritius paint industry. A total of 388 participants were selected using simple random sampling, and were subjected to a questionnaire for data collection. Lung function test was performed using a spirometer. Multiple regression was used to analyze the relationship between hours of exposure to solvents, while adjusting for socio-demographic factors. Independent t-test was also used to identify any difference between the means of lung function tests and the two exposed groups. Male participants were found less likely exposed to solvents compared to females (AOR, 3.39, CI 1.97-5.81). Those with secondary and lower secondary education, and worked for ≤12 hours per week, had an increased likelihood of being exposed to solvents (AOR 2.95, CI 1.20-7.28) (AOR 2.48, CI 1.19-5.16). Participants who were aware of occupational hazards (AOR 0.15, CI (0.05-0.46), and have used PPE (AOR 0.14, CI 0.08-0.25) were less likely to be less exposed to solvents. This study highlights the adverse effects of workplace exposures on respiratory health among paint factory workers.
Introduction
The most important component of paints is solvents. Their main use is to dilute paints to a proper consistency and viscosity for easy handling during manufacturing and application processes (Jafari et al. Citation2009). Solvents enter the bodily respiratory system through inhalation, inadvertent ingestion or through dermal absorption (Joshi and Adhikari Citation2019). Exposure to solvents has been noted to affect auditory system (Nakhooda et al. Citation2019), central nervous system (Beckley and Woodward Citation2013), hepatic system (Caciari et al. Citation2013), renal system (Kataria et al. Citation2015) and respiratory system (Büker et al. Citation2011) among others. The inhalation of uptake concentration is likely to cause respiratory effects, and is a common occupational scenario in many paint-manufacturing industries; hence, this study investigated exposure-related respiratory effects from paint solvents. According to Bahadar et al. (Citation2014), there is a dearth of literature on the effects of solvent exposure on the respiratory system. The authors further noted the inconsistencies and methodological limitations on studies investigating respiratory effects following exposure to solvents. Revathi (Citation2012) also suggested that studies on automobile paint exposure and lung function were inconclusive, and demonstrated no statistical relevance between solvents exposure and lung function tests. In 2018, Simamora et al. found no association between exposure to solvents and the lung function among shoes industry workers. However, an increased risk of pulmonary disease for occupationally exposed participants was noted. Contrary, Świerczyńska-Machura et al. (Citation2014) observed spirometry changes of bronchial obstruction of a mild degree in 17% of the workers who were exposed to paint solvents. Also, Singthong et al. (Citation2014) found an increase in respiratory symptoms among workers exposed to the solvent, trichloroethylene. It is for these previous findings that this study assessed the effects of paint solvents among paint industry workers in Mauritius.
Occupational exposure through inhalation is responsible for the emergence of several airway diseases (Santo Tomas Citation2011). The respiratory effects are even more severe in exposure scenarios where combinations of solvents such as toluene, xylene, ketones, alcohols, esters and glycol ethers, among others, exist (De Oliveira et al. Citation2011). The paint industry on the island, like Mauritius, employed thousands of workers, and the effects of paint solvents of workers’ health remain unknown. Mauritius has been reinforcing its Occupational Safety and Health legislations. However, due to lack of awareness and reporting of the exposure problems in chemical industries, it is thought to be a minor issue compared to its true nature. The National Research Council (National Research Council (US) and Institute of Medicine (US) Committee to Review the NIOSH Respiratory Disease Research Program Citation2008) confirmed that refining the quality of indoor air in workplaces could have significant health and economic benefits. Sobhee (Citation2011) indicated that no health risk assessment has been carried out in Mauritius among workers exposed to paint-manufacturing processes. Moreover, the number of occupational respiratory diseases in Mauritius has been rising in the past 5 years (Ministry of Health and Wellness, Mauritius Citation2020), particularly in the paint-manufacturing industries. To address this knowledge gap, this study seek to describe
the comparison of participants’ socio-demographic factors by week hours exposed to solvents (≤12 hours and >12 hours), and
to examine lung function tests among participants exposed to solvents for ≤12 hours and >12 hours.
Methodology
Study area and design
The quantitative, cross-sectional study was conducted in Mauritius, among 388 workers in three paint factories. In Mauritius, there are five paint-manufacturing factories located in Pailles, Coromandel, Baie du Tombeau, La Tour Koenig and Camp Fouquereaux. The study was conducted in the paint factories of Pailles, Coromandel and Baie du Tombeau, respectively. The paint industry employs thousands of people in Mauritius. Considering 20% of workers exposed to solvents in the paint factory, EPI INFO version 7 statistical software Stat-Calc program was used at a confidence interval of 95%, 80% study power and a minimum detectable odds ratio of 2.0 to determine the sample size. A sample with ratio 1:1 contained 173 (≤12 hours) and 173 (>12 hours); 10% non-response rate was added for both exposure hours, and finally a total of 388 study participants (n = 214, ≤12 hours and n = 174, >12 hours) were included in the study.
The paint-manufacturing factories included in this study make use of Xylene, Ethyl benzene, Acetone alcohol, Methanol, N-butyl acetate, Isobutyl acetate, Toluene and Ethyl benzene in their manufacturing processes. This information was derived from the material safety data sheet of the products produced. The main products produced are paints (xylene, Ethyl benzene and Acetone alcohol), lacquers (xylene, Toluene, Acetone and Ethyl benzene), white spirit and thinner (Methanol, N-butyl acetate and Isobutyl acetate).
Sampling
Convenience sampling method was used to select the three factories which lie within a 7-km radius of the capital city, Port Louis. There are 200 workers in the Sofap Ltd. (Taylorsmith Citation2017), 90 employees in Polytol Paints Ltd. (Polytol Citation2019) and 260 staffs in Mauvilac Ltd. (Akzonobel Citation2019). A multi-stage sampling method was used to select the 388 participants from the list provided by the Human Resource Departments. Clusters of workers with previous respiratory symptoms or disease and those without respiratory problems were formed. Out of these clusters, workers were selected through the stratified random sampling method as those in the manufacturing process and in administrative works. Since workers in the manufacturing process are more likely to be exposed to solvents at work compared to those in the administrative department, a simple random method was used to enroll them in order to make up the desired sample, thus having a fair representation of both departments and different exposure rates giving a more precise estimate of the whole population.
Data collection process
A researcher-administered questionnaire was used to screen participants with/without chronic medical conditions and possible exposures. The medical records of workers were accessed through Human Resource department after receiving the participants’ informed consent. This assisted in excluding those with underlying chronic medical conditions. Participants not suffering from any chronic conditions were further assessed by a physical examination. Spirometry test was then carried out when all the conditions for a proper test were met. In case of the contrary, the test was postponed until it was acceptable to be performed.
Study tools
Questionnaire
A researcher-administered questionnaire was filled for each participant after obtaining their consent. Apart from the usual demographic history, workers’ occupations were asked. The health conditions and lifestyle habits were also investigated to assess other risk factors of decreased lung function. The questionnaire was derived from the ECRHS II survey questionnaire after obtaining required permission (European Community Respiratory Health Survey Citation2014). Proper care was taken by the researchers to ensure that questions were asked in a similar manner to guard against recall bias.
Examinations and spirometry
Physical examination and spirometry tests were conducted by a certified medical practitioner. Examination of the respiratory system was carried out for each participant in a private room, to ensure confidentiality. For spirometry tests, FVC and FEV1 were used since they are the best available functional measures and predictors of respiratory health (Griffith et al. Citation2001). FVC was used as an indicator for the maximum amount of air expired after a maximum inspiration and FEV1 as an indicator for the maximum volume of air exhaled in the first second of a forced expiration from a position of full inspiration. The guidelines by the European Respiratory Society were followed to measure the FEV1 and FVC and calculate FEV1/FVC ratio, and three acceptable maneuvers were taken (Moore Citation2012).
Data analysis
The data from the questionnaires was verified for cleanliness, completeness and accuracy, and subsequently coded to facilitate data entry into the Statistical Package for Social Sciences (SPSS) v26.0 for analysis. Data were analyzed to illustrate the frequency of participants based on their socio-demographic characteristics as well as job departments, duration of employment, hazard awareness, the use of personal protective equipment (PPE), smoking habits and secondary exposure to tobacco smoke. Mean and standard deviation of different strata such as age, height, weight and different spirometric readings and ratio were also calculated. The frequency distributions were depicted as bar graphs and pie charts for the categorical data, while continuous data were represented as graphs to outline the central tendency and dispersion of the data. Furthermore, multiple regression analysis was performed to determine the association between hours of exposure and sociodemographic factors, job department, duration of employment, hazard awareness, use of PPE, smoking and secondary exposure to tobacco smoke. 95% Confidence intervals were used to determine the statistical significance. The continuous variables were also compared based on the level of exposure, and the independent t-test (≤.05) was calculated to find any significant association.
Results
Distribution of study participants
Most of the participants, 176 (45.4%), were aged between 25 and 34 of years. The lowest number of participants, 15 (3.9%), were of the age range between 55 and 64 years. The study comprised predominantly of males (n = 265, 68.3%) as compared to females (n = 123, 31.7%), and majority of the workers were married (n = 255, 65.7%). The participants were largely educated up to lower secondary level (n = 122, 31.4%) and upper secondary level (n = 108, 27.8%), with a small number (n = 17, 4.4%) having vocational/technical training. More participants reported to have lived in the rural areas (n = 224, 57.7%) as compared to urban area (n = 164, 42.3%). In order to achieve the objectives of the study, the socio-demographic characteristics were distributed between hours of exposure. shows the distribution of participants by socio-demographic characteristics status stratified by hours of exposure.
Table 1. Socio-demographic characteristics status stratified by hours of exposure per work-week.
In this study, there were more male workers with a shift duration of ≤12 hours per week compared to those who worked >12 hours. In addition, the study population comprised more male participants than females. There was an increased probability, by two-fold, of male workers who worked ≤12 hours per week (OR 2.15, CI 1.39–3.32) (AOR 3.39, CI 1.97–5.81) being exposed to solvents compared to female workers (). Participants with the highest level of education, below secondary and lower secondary categories (adjusted for age, gender, marital status and residence) had an increased probability (AOR 2.95, CI 1.20–7.28), nearly three-fold, to be exposed to solvents for ≤12 hours per week.
Table 2. Socio-demographic characteristics with exposure length status.
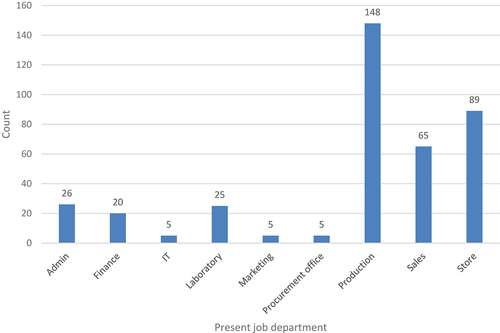
Distribution of participants by occupational history
The contributors were categorized according to the departments in which participants were working. The departments were administration, finance, information technology (IT), laboratory, marketing, procurement office, production, sale and store. shows the distribution of participants by job departments.
The period of employment of the workers was also enquired. The duration was divided as less than 3 years, between 3 and 9 years, between 10 and 16 years and between 17 and 23 years. Most of the participants were employed for less than three years (n = 154, 39.7%) and between three and nine years (n = 171, 44.1%). presents the distribution of employment data.
Table 3. Distribution of study participants by employment data.
Workers in the production section had a decreased likelihood of been exposed to solvents (≤12 hours per week) (OR 0.11, CI 0.06–0.22), while those in the store section had a three-fold exposure probability (OR 3.15, CI 1.39–7.17). Those who were employed for a duration of 3–9 years were also likely to be exposed for ≤12 hours per week (OR 1.58, CI 1.01–2.47) compared to those with a duration of 10–16 years (OR 0.36, CI 0.19–0.70). Participants were also asked whether they were aware of hazards associated with their employment, and majority of them (n = 357, 92.0%) were aware of hazards present in their workplace. Only 245 (63.1%) participants reported to use PPE, and majority of them (n = 298, 76.8%) had local exhaust ventilation present where solvents were used, in their workstations. Furthermore, those who worked for ≤12 hours per week (n = 188, 52.7%) were aware of solvents as hazardous and their effects, and 209 (97.4%) participants were aware of “hazardous” safety sign on solvents containers. presents data for occupational conditions and hazard awareness.
Table 4. Description of study participants’ working conditions.
When adjusted for age, gender, marital status, education and residence, those who were exposed for ≤12 hours per week were not aware of the hazards (AOR 0.15, CI 0.05–0.46) and PPE use (AOR 0.14, CI 0.08–0.25) in their respective work sections. Similarly, those who worked for ≤12 hours per week and were aware of the effects of hazards had decreased probability of being exposed to solvents (AOR 0.35, CI 0.16–0.74). When adjusting for socio-demographics, the presence of local exhaust ventilations at point of solvent use suggested a significantly high probability of exposure to solvents among those who worked for ≤12 hours per week (AOR 14.83, CI 7.11–30.93).
Participants were asked whether they had wheezing or whistling in their chest in the last 12 months, and only a small number of participants (n = 67, 17.3%) confirmed having wheezing or whistling chest in the last 12 months. Most of the participants (n = 351, 90.5%) did not wake up with chest tightness in the past 12 months. However, some workers indicated to have had phlegm in the morning during winter (n = 103, 26.5%). The OR and AOR were calculated for the participants’ health conditions, and none were statistically significant. shows distribution of participants by their health conditions.
Table 5. Distribution of participants by health conditions.
Majority of participants (n = 216, 55.7%) were non-smokers, and only 113 (29.1%) participants suggested to be exposed to tobacco smoke. When comparing smoking habits and exposure hours, most participants were non-smokers (n = 119, 55.1%) and were not exposed to tobacco smoke (n = 162, 58.9%) among those who were exposed to solvents for ≤12 hours per week. When adjusting for age, gender, marital status, education and residence, participants who worked for ≤12 hours per week and were exposed to tobacco smoke were significantly less likely (AOR 0.43, CI 0.25–0.76) to report being exposed to solvents.
Examinations and spirometric tests
The height of the participants was normally distributed with a peak at 1.74 m (mean 1.69 m, SD 0.1) and weight was at a peak of 66 kg (mean 68.38 kg, SD 13.3). The mean age of participants was 32.8 years (SD 9.8). The FVC first reading reached a peak of 3.25 L (mean 2.98 L, SD 0.7), with the FVC second reading at 2.75 L (mean 2.99 L, SD 0.7). The parameters were further compared against the duration of exposure, and independent t-test was also calculated comparing hours of exposure for ≤12 hours and >12 hours per week. The description of these variables is provided in .
Table 6. Descriptive statistics of continuous variables compared by hours of exposure.
Height was found to be statistically significant (p < 0.001) when compared with hours of exposure hours (≤12 and >12 hours). There was also statistical significant differences in FEV1/FVC ratio among those exposed for ≤12 hours (p < 0.001) and those exposed for >12 hours (p < 0.001) for FEV1/FVC readings.
Discussion
This study assessed the effects of solvents, commonly used in the paint-manufacturing industries in Mauritius, on lung function among workers. To the best of our knowledge, this is the first study to assess the effects of solvents on the lung function among the paint industry workers in Mauritius. The results showed that age group 25–34 years had the highest number of workers. However, age was not associated with hours of exposure to solvents. Golbabaei et al. (Citation2018) also noted this finding in a study that investigated occupational exposure to mixed organic solvents in an automotive industry. Majority of the study participants were males, had a lower education level, employed in the production, sales and store departments, and were less likely to be exposed to solvents (≤12 hours per week). This particular observation led to an associative relationship between the lower level of education and less likelihood of exposure to solvents. Participants in the aforementioned departments are employed based on prior experience in similar job tasks, and not necessarily the educational requirements for skilled individuals. Contrary, a study among Italian workers showed that women were more likely to be exposed to carcinogens, which included solvents (Scarselli et al. Citation2018). However, when studying American and Canadian workers and exposure to a particular solvent, it was inferred that women were less likely to be more exposed to solvents (CitationGravel et al. Citation2018), and this accords well with the findings of the current study. Our results on low education and less likelihood of exposure are in inconsistence with the findings of Nielsen et al. (Citation2021) which suggest that lower education level leads to higher occupational exposure to solvents.
The likelihood of exposure to solvents (≤12 and >12 hours per week) was further examined according to participants’ job departments. Participants who worked in the production departments were more likely to be exposed when compared to workers in the store departments. Hassan et al. (Citation2013) made similar findings where workers in the production units had an increased risk of exposure to solvents compared to those assigned to work in the packaging departments. Furthermore, exposure duration and placement of workers in various departments contribute to possible high risks of exposure (Moolla et al. Citation2015). Participants who had a work experience between 3 and 9 years were less likely to be exposed to solvents compared to those with 10 to 16 years of work experience. Ramadhini and Sulistyorini (Citation2021) suggested that there is induced causal effects among those who are exposed to solvents for a longer period. Also, in extended work durations, there is a considerable rise in both potential health hazards and cancer risks (Moolla et al. Citation2015). It was noted that participants who had higher exposure risk to solvents were more conversant with hazard awareness, and acquainted with the use of PPE. These accords well with the suggestion made by Onowhakpor et al. (Citation2017) that the use of PPE is considered significant between hazard awareness and risks prevention.
The height of participants was significantly different when compared to hours of exposure; however, no studies suggested similar results. This could have been to lack of literature on the association between hour of exposure and participants physical characteristics in the paint industries. Only one study (Saraei et al. Citation2019) suggested a statistical non-significant difference among the height of exposed and non-exposed workers in an automobile manufacturing plant. The significant differences between all three FEV1/FVC ratios and those exposed to shorter as well as longer hours were noted. The finding are in agreement with several other studies. Ojo et al. (Citation2017) found a similar decrease in FEV1/FVC ratio among spray painters as compared to controls in Nigeria. The decreased pulmonary function test was also noted among house painters with less than and more than 5 years of exposure in contrast to the control group (Jabbar and Mohammed Citation2021). Similarly, Saraei et al. (Citation2019) found a decrease in the FEV1/FVC ratio among automobile painters compared to their referent group.
The reporting on respiratory health conditions in the last 12 months was further measured against the likelihood of solvents exposure for ≤12 hours or >12 hours shift duration per week. Participants reported respiratory effects such as wheezing (17.3%) and tightness in the chest (9.5%), shortness of breath during the day at rest (2.8%), cough attacks (6.4%), phlegm during winter morning (26.5%), phlegm during the day or night (10.6%) and asthma attacks (5.2%). Majority of the reported respiratory effects were experienced by those who had ≤12 hours shift duration per week, except shortness of breath and cough attacks. Shortness of breath and cough attacks were mainly experienced by those who had >12 hours shift duration per week. No similar study could be found to explain less shift duration and the prevalence of respiratory effects. However, this could be explained by the occurrence of prior exposure to solvents since many participants in the induced exposure sections had prior work experience with solvents. Small number of participants (>12 hours per week) reported to experience cough attacks and shortness of breath. Similar findings were made by Ojo et al. (Citation2020) in Nigeria, where less number of spray painters exposed to organic solvents (5.8%) reported recurrent and prevalent (28%) coughs while 31.7% of the study population reported breathing problems. There is a scarcity of literature on solvents-occupational exposure studies among paint industry workers, making our results comparable to only solvents in spray painting and other painting occupations.
Conclusion
This study highlights adverse effects of workplace exposures on respiratory health and impairment of the pulmonary functions among paint factory workers in Mauritius. The study found a decreased lung functions among the participants exposed >12 hours as compared to those exposed <12 hours to paint solvents. Workers exposed for longer duration of hours to paint solvents are prone to developing health symptoms and pulmonary function impairment. It is noted that exposure to solvents causes several health effects such as dermatitis, renal problems, neuropsychological ill health and cancers, among other; however, this study was only restricted to exposure to paint solvents and lung function. Since there is a scarcity of literature on the around this issue, this study is expected to create foundation for further exploration in the field of inquiry. The results attempt to enable paint industries to plan and implement lung function examinations earlier to detect respiratory effects among workers.
Strengths and limitations
The current study has a very few limitations. Exposure levels of solvents were not quantified and neither biological monitoring was conducted, and only self-administered questionnaire was used to measure the responses on exposure symptoms, and this might have invited recall bias regarding reported symptoms. However, anthropometric measurements and spirometry assessments were conducted to minimize this bias. Majority of study participants were males and this might have skewed the gender-based comparison for exposure to solvents. In the current study, the likelihood of exposure was compared to socio-demographic characteristics, including lung function abilities among paint industry workers. This is one of the relatively few studies in the literature to examine the lung function ability among paint industry workers exposed to solvents.
Author contributions
Conceptualization, M.Y.K.Y. and P.C.R.; methodology, M.Y.K.Y. and P.C.R.; writing – original draft preparation, M.Y.K.Y. and P.C.R.; writing – review and editing, M.Y.K.Y. and P.C.R.; supervision, P.C.R.; All authors have read and agreed to the final version of the manuscript.
Informed consent statement
Informed consent was obtained from all subjects involved in the study prior commencement.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and has been approved by the Ethics Committee of the Faculty of Health Sciences at the University of Johannesburg. Ethics clearance number: REC-919-2021.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Akzonobel. 2019. AkzoNobel to strengthen position in Sub-Saharan African paints market with acquisition of Mauvilac. https://www.akzonobel.com/en/for-media/media-releases-and-features/akzonobel-strengthen-position-sub-saharan-african-paints.
- Bahadar H, Mostafalou S, Abdollahi M. 2014. Current understandings and perspectives on non-cancer health effects of Benzene: a global concern. Toxicol Appl Pharmacol. 276(2):83–94. doi:10.1016/j.taap.2014.02.01.
- Beckley JT, Woodward JJ. 2013. Volatile solvents as drugs of abuse: focus on the cortico-mesolimbic circuitry. Neuropsychopharmacology. 38(13):2555–2567. doi:10.1038/npp.2013.206.
- Büker HS, Demir E, Yüncü Z, Gülen F, Midyat L, Tanaç R. 2011. Effects of volatile substance abuse on the respiratory system in adolescents. Multidiscip Respir Med. 6(3):161–168. doi:10.1186/2049-6958-6-3-161.
- Caciari T, Casale T, Pimpinella B, Montuori L, Trovè L, Tomei G, Capozzella A, Schifano MP, Fiaschetti M, Scala B et al. 2013. Exposure to solvents in health care workers: assessment of the hepatic effects. Annali di Igiene: medicina preventiva e di comunita. 25(2):125–136. doi:10.7416/ai.2013.1914.
- De Oliveira HM, Dagostim GP, da Silva AM, Tavares P, da Rosa LA, de Andrade VM. 2011. Occupational risk assessment of paint industry workers. Indian J Occup Environ Med. 15(2):52–58. doi:10.4103/0019-5278.90374.
- European Community Respiratory Health Survey. 2014. Questionnaires, protocols and instructions. http://www.ecrhs.org/Quests.htm.
- Golbabaei F, Dehghani F, Saatchi M, Zakerian SA. 2018. Evaluation of occupational exposure to different levels of mixed organic solvents and cognitive function in the painting unit of an automotive industry. Health Promot Perspect. 8(4):296–302. doi:10.15171/hpp.2018.42.
- Gravel S, Lavoué J, Labrèche F. 2018. Exposure to polybrominated diphenyl ethers (PBDEs) in American and Canadian workers: biomonitoring data from two national surveys. Sci Total Environ. 631-632:1465–1471. doi:10.1016/j.scitotenv.2018.03.025.
- Griffith KA, Sherrill DL, Siegel EM, Manolio TA, Bonekat HW, Enright PL. 2001. Predictors of loss of lung function in the elderly: the Cardiovascular Health Study. Am J Respir Crit Care Med. 163(1):61–68. doi:10.1164/ajrccm.163.1.9906089.
- Hassan AAEH, El-Nagar SAEM, Tayeb IME, Bolbol SAEH. 2013. Health hazards of solvents exposure among workers in paint industry. Open J Saf Sci Technol. 3(4):87–95. doi:10.4236/ojsst.2013.34011.
- Jabbar AS, Mohammed RN. 2021. Impact of paints exposure on pulmonary function tests of male workers in Basrah City, South of Iraq. Int J Pharm Res. 12. doi:10.31838/ijpr/2020.SP2.127.
- Jafari MJ, Karimi A, Azari M. 2009. The challenges of controlling organic solvents in a paint factory due to solvent impurity. Ind Health. 47(3):326–332. doi:10.2486/indhealth.47.326.
- Joshi D, Adhikari N. 2019. An overview on common organic solvents and their toxicity. J Pharm Res Int. 28(3):1–18. doi:10.9734/jpri/2019/v28i330203.
- Kataria A, Trasande L, Trachtman H. 2015. The effects of environmental chemicals on renal function. Nat Rev Nephrol. 11(10):610–625. doi:10.1038/nrneph.2015.94.
- Ministry of Health and Wellness, Mauritius. 2020. Health statistics reports. http://health.govmu.org/English/Statistics/Health/Mauritius/Pages/default.aspx.
- Moolla G, FitzGerald JM, Rousseau R, Chen W, Sadatsafavi M. 2015. Interaction effect of psychological distress and asthma control on productivity loss? Eur Respir J. 45(6):1557–1565. doi:10.1183/09031936.00141614.
- Moore VC. 2012. Spirometry: step by step. Breathe. 8(3):232–240. doi:10.1183/20734735.0021711.
- Nakhooda F, Sartorius B, Govender SM. 2019. The effects of combined exposure of solvents and noise on auditory function - a systematic review and meta-analysis. The South African Journal of Communication Disorders = Die Suid-Afrikaanse Tydskrif Vir Kommunikasieafwykings. 66(1):e1–11. doi:10.4102/sajcd.v66i1.568.
- National Research Council (US) and Institute of Medicine (US) Committee to Review the NIOSH Respiratory Disease Research Program. 2008. Respiratory Diseases Research at NIOSH: reviews of Research Programs of the National Institute for Occupational Safety and Health. 2, Evaluation of the Respiratory Diseases Research Program. Washington (DC): National Academies Press (US).
- Nielsen SS, Warden MN, Sallmén M, Sainio M, Uuksulainen S, Checkoway H, Hublin C, Racette BA. 2021. Solvent exposed occupations and risk of Parkinson disease in Finland. Clin Parkinsonism Relat Disord. 4:100092. doi:10.1016/j.prdoa.2021.100092.
- Ojo TO, Onayade AA, Afolabi OT, Ijadunola MY, Esan OT, Akinyemi PA, Awe OO. 2020. Work practices and health problems of spray painters exposed to organic solvents in Ile-Ife, Nigeria. J Health Pollut. 10(28). doi:10.5696/2156-9614-10.28.201208.
- Ojo TO, Onayade AA, Akinyemi PA, Adesanmi AJ. 2017. Environmental working conditions, lung function and total serum bile acids of spray painters exposed to organic solvents in Ile-Ife, Nigeria. J Health Pollut. 7(13):2–10. doi:10.5696/2156-9614-7-13.2.
- Onowhakpor A, Abusu G, Adebayo B, Esene H, Okojie O. 2017. Determinants of occupational health and safety: knowledge, attitude, and safety practices toward occupational hazards of sawmill workers in Egor Local Government Area, Edo State. Afr J Med Health Sci. 16(1):58. doi:10.4103/2384-5589.209487.
- Polytol. 2019. About polytol paints. https://www.polytolpaints.com/about
- Ramadhini B, Sulistyorini L. 2021. Correlation between workers’ characteristics and health complaints due to exposure to organic solvents in the Sidoarjo offset printing. Indonesian J Occup Saf Health. 10(2):199. doi:10.199.10.20473/ijosh.v10i2.2021.199-207.
- Revathi M. 2012. Effects of pulmonary function in short duration exposed automobile spray painters. IOSR J Dent Med Sci. 2(2):48–51. doi:10.9790/0853-0224851.
- Santo Tomas LH. 2011. Emphysema and chronic obstructive pulmonary disease in coal miners. Curr Opin Pulm Med. 17(2):123–125. doi:10.1097/MCP.0b013e3283431674.
- Saraei M, Pouryaghoub G, Eftekhari S. 2019. Effects of car painting vapors on spirometric parameters in automobile painting workers. Tanaffos. 18(4):346–350. PMID: 32607116.
- Scarselli A, Corfiati M, Di Marzio D, Marinaccio A, Iavicoli S. 2018. Gender differences in occupational exposure to carcinogens among Italian workers. BMC Public Health. 18(1):413. doi:10.1186/s12889-018-5332-x.
- Singthong S, Pakkong P, Choosang K, Wongsanit S. 2014. Occupational health risks among trichloroethylene-exposed workers in a clock manufacturing factory. Glob J Health Sci. 7(1):161–172. doi:10.5539/gjhs.v7n1p161.
- Sobhee SK. 2011. Occupational hazards and health and safety risks pertaining to persistent organic pollutants (Pops) in a small island developing state – Mauritius. Int J Environ Sci Ecotechnol. 1(2):114–125.
- Świerczyńska-Machura D, Brzeźnicki S, Nowakowska-Świrta E, Walusiak-Skorupa J, Wittczak T, Dudek W, Bonczarowska M, Wesolowski W, Czerczak S, Pałczyński C. 2014. Occupational exposure to diisocyanates in polyurethane foam factory workers. Int J Occup Med Environ Health. 28(6):985–998. doi:10.13075/ijomeh.1896.00284.
- Taylorsmith. 2017. Sofap. https://www.taylorsmith.com/en/manufacturing/sofap.