Abstract
Background
Cognitive difficulties are rarely addressed after the treatment of major depressive disorder (MDD). New scalable treatments are needed. To ensure relevance and engagement of novel interventions, there is a need to understand the perspectives of the users.
Aim
Explore former depressed adults needs and perspectives during the planning and development of a novel internet-delivered intervention targeting residual cognitive symptoms after MDD.
Method
The planning phase included exploratory qualitative interviews with former depressed adults (n = 16). In the development phase, a prototype including psychoeducation, attention training and compensatory strategies was tested in think-aloud interviews with former depressed adults (n = 7) and psychologists (n = 4). Data were analysed thematically.
Results
Analysis of exploratory interviews identified four themes. Experiences of residual cognitive symptoms consisted of two sub-themes (Everyday life is more demanding; Concerns about cognitive difficulties). Coping with residual cognitive symptoms had two sub-themes (Compensatory strategies; Acceptance). Needs from an intervention consisted of two-subthemes (Need for information; Therapist support). Barriers for engagement consisted of three sub-themes (Being overwhelmed; Not being motivated; Frequent registration). Analysis of think-aloud interviews was organized into three themes: Positive perceptions of content; Concerns regarding content; Perceptions of Layout, Visuals and Navigation.
Conclusion
The intervention may address concerns and consequences of cognitive difficulties by including psychoeducation, compensatory strategies and elements to increase acceptance and motivation, provided in manageable proportions.
Major depression disorder (MDD) is a leading cause of disease burden (Ferrari et al., Citation2013), and both medical and psychological treatments are effective for MDD (Cuijpers et al., Citation2008). However, evidence shows that many individuals experience residual cognitive symptoms, such as difficulties with memory, attention and executive functions, after no longer meeting core symptoms of MDD; and show impaired performance on neuropsychological tests (Bora et al., Citation2013; Hasselbalch et al., Citation2011; Semkovska et al., Citation2019). A meta-analysis of cognitive impairments after depression showed that those with a history of MDD had large deficits in aspects of long-term memory and small to moderate deficits in most other cognitive domains. More specifically, they underperformed in 73% of the neuropsychological tests when compared to healthy controls (Semkovska et al., Citation2019). There is evidence to support that cognitive difficulties worsen after each consecutive episode of MDD, supporting the hypothesis that neurobiological scarring occurs during states of depression, causing persisting cognitive difficulties after depression (Semkovska et al., Citation2019). However, the underlying mechanisms of cognitive impairment after MDD are not well understood. Nevertheless, consequences of cognitive impairment are significant and involve reduced quality of life (Saragoussi et al., Citation2013) and everyday functioning (Jaeger et al., Citation2006), such as workplace performance (Buist‐Bouwman et al., Citation2008; McIntyre et al., Citation2013). Residual cognitive symptoms after depression are also associated with rumination (Joormann et al., Citation2011) and a tendency to attribute the cognitive impairment to negative aspects of themselves and a sense of being a failure (Ebert et al., Citation2017). Residual cognitive symptoms have also been proposed as a risk factor for new depressive episodes (Schmid & Hammar, Citation2013). This is of significance, as the relapse rates for MDD are high (Mueller et al., Citation1999). Overall, there is a need to develop novel and scalable interventions for adults with residual cognitive symptoms after MDD.
Interventions targeting cognitive difficulties have successfully been conducted for mental health disorders such as schizophrenia where negative symptoms have been reduced after treatment (Wykes et al., Citation2011). These previous findings are relevant, given initiation of activity and motivation are also common symptoms in MDD. However, research regarding interventions for cognitive impairment in MDD is limited (Kim et al., Citation2018). A few studies have tested interventions targeting residual cognitive symptoms in former depressed adults, all with promising results such as improved divided attention, working memory, planning, verbal memories and switching abilities (Hammar et al., Citation2020; Listunova et al., Citation2020; Semkovska & Ahern, Citation2017). Two studies (Hammar et al., Citation2020; Semkovska & Ahern, Citation2017) have used computerized cognitive training with the aim of improving working memory, planning and attention. These interventions did not target cognitive impairment in everyday functioning through psychoeducation and strategy training, suggested as key elements in interventions targeting cognitive difficulties in mood disorders (Douglas et al., Citation2019). The latter elements which were included by Listunova et al. (Citation2020) were the intervention integrated cognitive training, strategy training and psychoeducation to enhance coping, delivered in a face-to-face group format. However, these studies have not addressed worries and rumination associated with cognitive difficulties, which may be a useful approach as rumination is associated with cognitive impairment and depressive relapse (Joormann, Citation2010; Spasojević & Alloy, Citation2001). Moreover, combining elements from cognitive rehabilitation and psychotherapeutic approaches such as cognitive behaviour therapy has successfully been applied for individual with neurological disorders (Gandy et al., Citation2020). Expanding treatment of residual cognitive symptoms to also target rumination may therefore be a promising approach.
To improve access to treatment for adults with residual cognitive symptoms after depression, there is a need to develop scalable methods of delivering interventions. Internet-delivered treatment is a promising tool, given its potential to reach many individuals without increased costs. To ensure the relevance and engagement for internet-delivered interventions for this target group, there is a need to understand the specific perspectives of formerly depressed adults when engaging with a digital intervention (Yardley et al., Citation2015). The person-based approach provides guidance on how to integrate previous clinical research with the end users’ needs and perspectives in a systematic manner (Yardley et al., Citation2015). This approach has been successfully applied to improve engagement and consequently effects in the development of digital health interventions targeting management of hypertension, asthma and distress (Band et al., Citation2017; Geraghty et al., Citation2016; Morrison et al., Citation2015). There are, however, no studies that have applied a person-based approach for developing digital interventions for residual cognitive symptoms after MDD.
In this study, we utilized a person-based approach that explores former depressed adults’ experiences and needs in order to develop a novel intervention for adults with residual cognitive symptoms after MDD. The research questions are:
What are the experiences with residual cognitive symptoms in former depressed adults?
What are the needs and barriers involved in an internet-delivered intervention targeting residual cognitive symptoms?
How is a viable prototype of the intervention experienced by former depressed adults?
Methods
Design
First, exploratory qualitative interviews with former depressed adults were conducted in the planning phase to investigate experiences, needs and barriers for engagement. Second, in the development phase, a prototype was developed and tested on former depressed adults and therapists through semi-structured qualitative interviews. provides an overview of activities conducted during the planning and development of the intervention.
Table 1. Overview of activities in the planning and development phases.
Exploratory interviews: participants and procedures
Thirty-eight individuals who had previously received either internet-delivered cognitive behavioural therapy for MDD in a secondary health care clinic at Haukeland University Hospital in Bergen (iCBT; Nordgreen et al., Citation2019) or a computerized cognitive training program for former depressed individuals connected to the Neuropsychological Outpatient Clinic at the University of Bergen, Norway (CCT; Hammar et al., Citation2020) received an invitation letter to participate in exploratory interviews. Participants included in the exploratory interviews needed to have a score of <16 on the Montgomery-Åsberg Depression Rating Scale (MADRS-S; Svanborg & Åsberg, Citation1994, Citation2001). Sample sizes of 12 individuals have been found to be sufficient to achieve saturation in qualitative material (Guest et al., Citation2006). Consequently, the inclusion of 12 participants was set as a minimum number of participants.
In total, 16 participants made contact to participate and completed the exploratory interviews. Interviews were conducted between 15 January 2018 to 11 April 2018 and took place face-to-face at Haukeland University Hospital in Bergen or the Faculty of Psychology at the University of Bergen. A therapist, either a clinical psychologist or a student in clinical psychology, led the interviews. The therapist and invitation letter informed participants that the main aim of the study was to explore former depressed adults' experience with cognitive difficulties and internet-delivered treatment with the overall objective of developing an intervention for cognitive difficulties after depression. The interviews were semi-structured and flexible, given the explorative nature of the study. The average length of the interviews was 51 minutes.
Development phase: prototype, participants and procedures
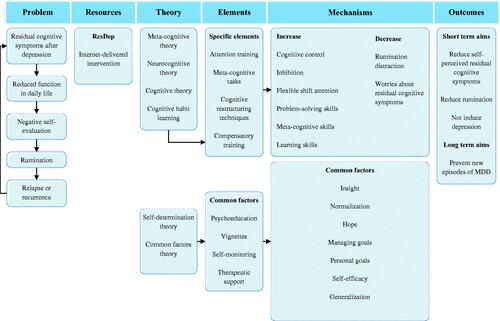
A prototype of the intervention was developed based on the results from the exploratory interviews, theory and evidence from other interventions targeting cognitive difficulties. Construction of prototype content, design, and digital platform were done in collaboration with a team consisting of partners in the research project Introducing Mental Health Through Adaptive Technology (INTROMAT, 259293), an ICT Lighthouse research project funded by the Norwegian Research Council. The team members included clinical psychologists, researchers in human computer interaction (HCI) and an industry partner. Content was based on core principles of Cognitive Enhancement Therapy for Mood Disorders (CET-MD; Douglas et al., Citation2019). More specifically, (1) psychoeducation about residual cognitive symptoms covering attention, memory, executive functions and rumination, (2) cognitive practice employing auditory attention training (Wells, Citation1990) and compensatory strategies, (3) tasks to increase transfer to everyday life. In addition, material was based on cognitive behaviour therapy. Common factor elements were emphasized through vignettes, self-monitoring, therapeutic support, insight and goal-management. A logic model with an overview of the prototype elements, mechanisms of change and outcomes was constructed (see ). The digital platform of the prototype could be delivered on computers, tablets and mobile phones. Example of the prototype front-end is illustrated in .
To test the prototype, former depressed adults participating in the exploratory interviews (n = 7) and therapists with experience delivering treatment digitally (n = 4) accepted the invitation to test the intervention though a face-to-face qualitative interview. Participants from the exploratory interviews were provided with the text of two intervention modules about one week before the interview and were asked to read them before the interview. Overall, 11 single think-aloud interviews were conducted from 23 August 2018 to 29 November 2018 at Haukeland University Hospital or the Faculty of Psychology at the University of Bergen. The interview consisted of two parts. First, a clinical psychologist interviewed the participants about their perceptions of the intervention text. Second, the participants individually tested the intervention prototype on a computer and mobile phone while being observed by a clinical psychologist and in most interviews a researcher in human computer interaction. The main role of HCI researcher was to detect user experience issues and aid the development of the intervention. The average length of interviews was 53 minutes.
Analysis
For coding and organizing the collected material, NVivo 12 was used. Transcripts were analysed inductively applying thematic analysis based on both Braun and Clarke (Citation2006) and Joffe and Yardley’s (Citation2004) approaches. Initially, in order to become familiarized with the data, the first author read and reread all transcripts. Second, in the process of creating the initial coding manual, the first author and a co-author independently coded the first three interviews and integrated these into a coding manual. Furthermore, coding of the interviews was conducted during team meetings where coded transcripts were compared and discussed. The coding manual was iterated upon many times during this process, and new themes were searched. To ensure that no important points of view were neglected, the transcripts were revisited and themes re-evaluated. Themes and codes were later reviewed by other team members. Codes were merged and themes renamed. Final themes were agreed on by all team members. Lastly, a summary of the main findings was written, and a selection of representative quotes was decided on.
Ethics
The study was approved by the Norwegian regional ethics committee (2017/1749). Participants signed a written informed consent including that their data could be used in research. They received a gift card of NOK 400.
Results
For inclusion in the planning phase, a total of 16 participants were found eligible for exploratory interviews. Participants’ characteristics are presented in .
Table 2. Participant characteristics.
Planning phase: exploratory interviews
Themes, sub-themes and sub-theme examples are presented in . Based on the results from the exploratory interviews, guiding principles were formulated (Appendix 3).
Table 3. Summary of qualitative themes identified in exploratory interviews.
Theme 1: experiences of residual cognitive symptoms
Everyday life is more demanding
Overall, many expressed that daily life was more challenging due to the residual cognitive symptoms. Typical situations expressed included not being able to think clearly, focus their attention, remembering messages, becoming easily stressed and overwhelmed. The residual cognitive symptoms often affected participants daily functioning such as vocational performance and social life: “I feel handicapped. I cannot think of a better word. Socially handicapped” (Male, 47 years).
Concerns about cognitive difficulties
Participants reported negative thoughts and worries about the consequences of cognitive impairment and the perceptions of not being able to fulfil their own expectations. They expressed negative thoughts about cognitive difficulties that were related to negative emotional reactions such as frustration, sadness, shame and anger with residual cognitive symptoms: “I became very sad, because I was thinking, it becomes a thing when you have a really bad day, and you go ‘How long is this going to take and will I ever manage to do this again?’” (Female, 32 years).
Theme 2: coping with cognitive impairment
Compensatory strategies
Participants described various ways of coping with residual cognitive symptoms. Generally, compensatory strategies were used for coping with everyday life, such as employing memory techniques and making adjustments to their surroundings: “I make a story and visualize crazy things that do not make any sense, because that’s what sticks to my memory” (Male, 27 years).
Acceptance
Acceptance and normalization of residual cognitive symptoms were helpful for many participants. Furthermore, several expressed that it was useful not to dwell on the consequences of cognitive impairments: ‘I have become better at accepting situations, that things do not always go as planned. Realizing that not everything can be 100% planned’ (Female, 33 years).
Theme 3: needs from an intervention
Need for information
This theme illustrates the need to get information about residual cognitive symptoms as participants reported to have limited knowledge about residual cognitive symptoms and insights about these could increase hope, control and reduce stress: “Can I have reduced cognitive abilities after depression? That it can last for years. I got tears in my eyes when I read it. Is it possible? Imagine if I can get help, this was a part of me, it was incredibly exhausting, and I felt I could just give up working the way I was working, so this is a real barrier” (Female, 41 years).
Therapist support
Guidance by a therapist was mentioned as a vital component of the intervention. Receiving emotional support and feedback on home assignments were the main argument for having therapist support: “I got very good help from the therapist, it was absolutely necessary, that he could give me that feedback” (Female, 32 years).
Theme 4: barriers for engagement
Being overwhelmed
Participants expressed that they would be overwhelmed if provided with full access to all material at once. Completion of one module before receiving new material was therefore a preference: “I would prefer one module at a time, so you don’t feel it to be massive, because it is something about getting a sense of achievement, that you complete one by one, that you don’t see the entire picture” (Female, 41 years).
Not being motivated
Overall, this theme entails the importance of being willing to work with the program and believe in its potential effect. The participants expressed that motivation was fundamental to their progress and to attain an effect of the digital intervention. Decisions to devote themselves to therapy, and to the assignments given in therapy, had often been taken before the therapy had started. “But you must be prepared to invest personally in it, it is demanding” (Female, 32 years).
Frequent registration
Daily, detailed and irrelevant registration of activities was by many of our participants perceived as a chore more than a meaningful activity: “I felt it was unnecessary for me to write all these plus and minus activities. So, I felt kind of like, this doesn’t fit me” (Female, 41 years).
Development phase: think-aloud interviews
In the development of the intervention, seven participants from the initial sample accepted the invitation to participate in think-aloud interviews. In addition, four clinical psychologists (females = 3, mean age = 36.3 (SD = 10.5)) were included as participants. A summary of qualitative themes is presented in .
Table 4. Summary of qualitative themes identified in think-aloud interviews.
Theme 1: positive perceptions of content
Overall, the participants expressed that the content was relevant and recognizable. The vignettes, based on people experiencing residual cognitive symptoms, were especially appreciated. Generally, participants reported the text as well structured, concrete and easy to read and workload and length of the modules as appropriate. “I could relate to a lot [of the content]. The examples were really on point” (Female, 28 years).
Theme 2: concerns regarding content
The participants articulated some concerns about the intervention content. Several mentioned being were too well-functioning for some tasks. A few participants suggested new content or assignments. Another concern was not understanding examples and tasks: “Then I thought about the concept of ‘cognition’… Is it explained earlier? If I had read this section first, I would not have known what it [cognition] was really” (Female, 30 years).
Theme 3: perceptions of layout, visuals and navigation
The intervention was perceived as easy-to-use by the participants. They also expressed positive perceptions about the layout and visuals of the intervention prototype. Particularly, they reported liking the clean and simple look of the intervention. Participants commented on the design looking professional and pictures with themes from nature were favoured: “I liked this heaven-picture very much. But nature… I like it. The sky and trees and such” (Female, 26 years).
However, some usability and navigation issues were reported while testing the intervention, such as having an overview of pages in each module and a sent button to store answers on tasks. A few participants had negative perceptions of pictures and one participant mentioned photographs of humans as unnatural. Difficulties understanding the meaning of pictures was another issue reported: “I do not think regular photographs capture the intention behind the picture that easily. It can feel a bit messy. I would rather have simplified drawings of some sort” (Female, 28 years).
Optimizing the intervention
As a final step, changes to the content and design were conducted based on the feedback from the think-aloud interviews (Appendix 4). The following criteria were used by the project team to guide iterations: (1) Not in conflict with the evidence on treating cognitive difficulties, (2) In line with guiding principles, (3) Easy to change, (4) Suggested by many participants.
Discussion
In this study, we used a person-based approach to explore former depressed adults’ experiences with residual cognitive symptoms and needs in order to develop a novel intervention for adults with such symptoms after MDD. Think-aloud interviews testing the prototype of the intervention showed that some changes were needed to improve the intervention.
Exploratory interviews indicated that participants experienced the residual cognitive symptoms, such as trouble remembering information and concentrate, to reduce functioning in vocational and social life. Also, participants expressed concerns about cognitive difficulties including worries about having a relapse of depression and whether the cognitive difficulties would ever improve. Adressing these worries therefore appeared relevant. Concerns about residual cognitive symptoms were in the prototype addressed by including elements from cognitive behaviour therapy. This is in line with findings showing that a combination of cognitive interventions and psychological therapy and rehabilitation are more effective than using a single approach (Kukla et al., Citation2018; Wykes et al., Citation2011). Moreover, participants found it valuable to normalize and accept the cognitive difficulties instead of dwelling on or ruminating over their consequences. Associations between cognitive impairment and rumination is reported (Joormann et al., Citation2011) and finding alternative emotion regulation strategies such as acceptance or CBT techniques may be beneficial. Another intervention element identified in the exploratory interviews and included in the prototype was compensatory strategies. Participants had positive experiences using compensatory strategies such as note pads and memory techniques. This is in line with previous studies showing that training in using compensatory strategies is effective for increasing daily functioning in individuals with mental health illnesses (Twamley et al., Citation2012). Moreover, training in automating the use of compensatory strategies is easy to implement and do not rely on advanced technology.
Several needs from the interventions and barriers for engagement were identified in the exploratory interviews. Information about cognitive impairment after depression was suggested as one approach to normalizing experiences. The need to increase knowledge among patients and clinicians about cognitive impairment after depression has previously been reported (McAllister-Williams et al., Citation2017). The prototype therefore included psychoeducation. This is also in line with previous endorsements emphasizing the importance of psychoeducation in treatment of cognitive difficulties in MDD (Douglas et al., Citation2019). However, participants had experienced being easily overwhelmed when receiving too much information at once. Therefore, they wanted the information to be presented in a manageable amount. This may be explained by the residual cognitive symptoms making it difficult to both sustain, switch attention, and retain information. Informed by these findings, we ensured that the interventions had a tunnelled design where only one module is provided at once, had limited tasks to register and a simple design. The participants also expressed a preference for therapist guidance instead of a self-guided intervention. Substantial evidence supports that interventions led by a therapist increase the effects of internet-delivered intervention (Andersson et al., Citation2009). This could be a consequence of therapists promoting motivation and support (Karekla et al., Citation2019), and we therefore developed the intervention to be guided. Finally, the participants emphasized the importance of being motivated to work with the program, which has been found to increase the effect of interventions targeting cognitive difficulties (Choi et al., Citation2010). This was solved by offering self-tailored exercises and tasks, an approach that has been found to make internet-delivered interventions perceived as more helpful and relevant (Yardley et al., Citation2016) and to enhance motivation (Ryan & Deci, Citation2000).
The main findings from the next phase in the think-aloud interviews were that the participants perceived the prototype as relevant and recognizable. Furthermore, participants reported that the intervention was easy to use. However, a key concern was that some assignments underestimated and did not match the participants’ level of cognitive functioning. This may be explained by the fact that some of the elements and tasks were transferred from cognitive rehabilitation for traumatic brain injury and serious mental health disorders, patient groups that often have a more global cognitive impairment and thus poorer functioning. Another feedback from participants was that they did not understand all concept used such as ‘cognition’. This could be a result of participants not receiving all modules at once and difficult concepts being explained in another module. Nevertheless, an effort was made to ensure that abstract concepts were clarified with daily life examples. Some participants also requested other topics or material to be included such as low self-esteem and sleep. These suggestions were assessed by the project team according to their relevance to the intervention.
Implications
The current paper adds to the literature, as it demonstrates a systematic approach to integrating users’ perspectives from the initial stages of intervention planning and in the development stage, optimizing the intervention. Demonstrating this approach could be helpful for others developing novel mental health interventions. Mapping participants needs, barriers for engagement and disliked intervention elements could potentially increase the adherence and effects of the intervention. We have documented the intervention’s preliminary effects and feasibility (Myklebost et al., Citation2021) and an ongoing randomized controlled trial will further investigate its effects (ClinicalTrials.gov: 04864353) Moreover, applying the person-based approach may ease implementation of the intervention into routine care as an effort has been made to make it motivating to use.
Limitations
The main limitation of the current study is the sample size, and therefore generalization of the results must be done with caution. Overall, the sample had similar characteristics in terms of gender, age, and marital status as users of the iCBT clinic in Nordgreen et al. (Citation2019). One exception is that the current study had a majority of participants with higher education, which could potentially compromise the transferability of the results. Another limitation is that participants had experience with digital interventions and may therefore have a higher level of digital literacy and different perspectives on internet-delivered interventions than those with only experience with face-to-face treatment only. However, participants might have provided a more detailed description of limitations and strengths with this method of receiving treatment because of their experience from digital interventions. Further, internet-delivered treatment might not be suitable for all individuals. Therefore, focusing on the viewpoints of those already willing to receive such treatment might be relevant. Another limitation concerns each participant giving feedback to only two modules, with a test of the full-scale intervention not being included. This might have affected the in-depth understanding of the intervention as a whole. A last limitation is that participants were not consulted to validate the themes emerging from the analyses.
Conclusions
In conclusion, interventions targeting residual cognitive symptoms after MDD should address concerns about cognitive difficulties and their functional consequences by including psychoeducation, compensatory strategies, in addition to psychotherapeutic elements increasing acceptance and useful coping. To addresses barriers of engagement should interventions be motivating to use, which may be achieved by including self-tailoring and providing content in manageable proportions. Testing the intervention prototype identified needs for iterations such as securing that the intervention is relevant for the functioning of former depressed adults and text being written in an easy-to-understand language.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Andersson, G., Carlbring, P., Berger, T., Almlöv, J., & Cuijpers, P. (2009). What makes internet therapy work? Cognitive Behaviour Therapy, 38(Sup1), 55–60. https://doi.org/10.1080/16506070902916400
- Band, R., Bradbury, K., Morton, K., May, C., Michie, S., Mair, F. S., Murray, E., McManus, R. J., Little, P., & Yardley, L. (2017). Intervention planning for a digital intervention for self-management of hypertension: a theory-, evidence-and person-based approach. Implementation Science, 12(1), 25. https://doi.org/10.1186/s13012-017-0553-4
- Bora, E., Harrison, B. J., Yücel, M., & Pantelis, C. (2013). Cognitive impairment in euthymic major depressive disorder: a meta-analysis. Psychological Medicine, 43(10), 2017–2026. https://doi.org/10.1017/S0033291712002085
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Buist‐Bouwman, M., Ormel, J., De Graaf, R., De Jonge, P., Van Sonderen, E., Alonso, J., Bruffaerts, R., Vollebergh, W., & Investigators, E. M. (2008). Mediators of the association between depression and role functioning. Acta Psychiatrica Scandinavica, 118(6), 451–458. https://doi.org/10.1111/j.1600-0447.2008.01285.x
- Choi, J., Mogami, T., & Medalia, A. (2010). Intrinsic motivation inventory: An adapted measure for schizophrenia research. Schizophrenia Bulletin, 36(5), 966–976. https://doi.org/10.1093/schbul/sbp030
- Cuijpers, P., Van Straten, A., Andersson, G., & Van Oppen, P. (2008). Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology, 76(6), 909–922. https://doi.org/10.1037/a0013075
- Douglas, K. M., Peckham, A., Porter, R., & Hammar, A. (2019). Cognitive enhancement therapy for mood disorders: A new paradigm? The Australian and New Zealand Journal of Psychiatry, 53(12), 1148–1150. https://doi.org/10.1177/0004867419873711
- Ebert, B., Miskowiak, K., Kloster, M., Johansen, J., Eckholm, C., Waerner, T., Holme, M., & Bruun, L. M. (2017). An ethnographic study of the effects of cognitive symptoms in patients with major depressive disorder: The IMPACT study. BMC Psychiatry, 17(1), 370.https://doi.org/10.1186/s12888-017-1523-8
- Ferrari, A. J., Charlson, F. J., Norman, R. E., Patten, S. B., Freedman, G., Murray, C. J., Vos, T., & Whiteford, H. A. (2013). Burden of depressive disorders by country, sex, age, and year: Findings from the global burden of disease study 2010. PLoS Medicine, 10(11), e1001547. https://doi.org/10.1371/journal.pmed.1001547
- Gandy, M., Karin, E., McDonald, S., Meares, S., Scott, A. J., Titov, N., & Dear, B. F. (2020). A feasibility trial of an internet-delivered psychological intervention to manage mental health and functional outcomes in neurological disorders. Journal of Psychosomatic Research, 136, 110173. https://doi.org/10.1016/j.jpsychores.2020.110173
- Geraghty, A. W., Muñoz, R. F., Yardley, L., Mc Sharry, J., Little, P., & Moore, M. (2016). Developing an unguided internet-delivered intervention for emotional distress in primary care patients: Applying common factor and person-based approaches. JMIR Mental Health, 3(4), e53. https://doi.org/10.2196/mental.5845
- Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
- Hammar, Å., Semkovska, M., Borgen, I. M. H., Myklebost, S., Ronold, E. H., Sveen, T., Ueland, T., Porter, R., & Johnson, S. L. (2020). A pilot study of cognitive remediation in remitted major depressive disorder patients. Applied Neuropsychology: Adult, 1–11. https://doi.org/10.1080/23279095.2020.1726919
- Hasselbalch, B. J., Knorr, U., & Kessing, L. V. (2011). Cognitive impairment in the remitted state of unipolar depressive disorder: A systematic review. Journal of Affective Disorders, 134(1-3), 20–31. https://doi.org/10.1016/j.jad.2010.11.011
- Jaeger, J., Berns, S., Uzelac, S., & Davis-Conway, S. (2006). Neurocognitive deficits and disability in major depressive disorder. Psychiatry Research, 145(1), 39–48. https://doi.org/10.1016/j.psychres.2005.11.011
- Joffe, H., & Yardley, L. (2004). Research methods for clinical and health psychology. In D. Marks & L. Yardley (Eds.), Content and thematic analysis (pp. 56–68). Sage.
- Joormann, J. (2010). Cognitive inhibition and emotion regulation in depression. Current Directions in Psychological Science, 19(3), 161–166. https://doi.org/10.1177/0963721410370293
- Joormann, J., Levens, S. M., & Gotlib, I. H. (2011). Sticky thoughts: Depression and rumination are associated with difficulties manipulating emotional material in working memory. Psychological Science, 22(8), 979–983. https://doi.org/10.1177/0956797611415539
- Karekla, M., Kasinopoulos, O., Neto, D. D., Ebert, D. D., Van Daele, T., Nordgreen, T., Höfer, S., Oeverland, S., & Jensen, K. L. (2019). Best practices and recommendations for digital interventions to improve engagement and adherence in chronic illness sufferers. European Psychologist, 24(1), 49–67. https://doi.org/10.1027/1016-9040/a000349
- Kim, E. J., Bahk, Y.-C., Oh, H., Lee, W.-H., Lee, J.-S., & Choi, K.-H. (2018). Current status of cognitive remediation for psychiatric disorders: a review. Frontiers in Psychiatry, 9, 461. https://doi.org/10.3389/fpsyt.2018.00461
- Kukla, M., Bell, M. D., & Lysaker, P. H. (2018). A randomized controlled trial examining a cognitive behavioral therapy intervention enhanced with cognitive remediation to improve work and neurocognition outcomes among persons with schizophrenia spectrum disorders. Schizophrenia Research, 197, 400–406.https://doi.org/10.1016/j.jpsychores.2020.110173
- Listunova, L., Kienzle, J., Bartolovic, M., Jaehn, A., Grützner, T. M., Wolf, R. C., Aschenbrenner, S., Weisbrod, M., & Roesch-Ely, D. (2020). Cognitive remediation therapy for partially remitted unipolar depression: A single-blind randomized controlled trial. Journal of Affective Disorders, 276, 316–326. https://doi.org/10.1016/j.jad.2020.07.008
- McAllister-Williams, R. H., Bones, K., Goodwin, G. M., Harrison, J., Katona, C., Rasmussen, J., Strong, S., & Young, A. H. (2017). Analysing UK clinicians' understanding of cognitive symptoms in major depression: A survey of primary care physicians and psychiatrists. Journal of Affective Disorders, 207, 346–352. https://doi.org/10.1016/j.jad.2016.09.036
- McIntyre, R. S., Cha, D. S., Soczynska, J. K., Woldeyohannes, H. O., Gallaugher, L. A., Kudlow, P., Alsuwaidan, M., & Baskaran, A. (2013). Cognitive deficits and functional outcomes in major depressive disorder: Determinants, substrates, and treatment interventions. Depression and Anxiety, 30(6), 515–527. https://doi.org/10.1002/da.22063
- Morrison, D., Mair, F. S., Chaudhuri, R., McGee-Lennon, M., Thomas, M., Thomson, N. C., Yardley, L., & Wyke, S. (2015). Details of development of the resource for adults with asthma in the RAISIN (randomized trial of an asthma internet self-management intervention) study. BMC Medical Informatics and Decision Making, 15(1), 57.https://doi.org/10.1186/s12911-015-0177-z.
- Mueller, T. I., Leon, A. C., Keller, M. B., Solomon, D. A., Endicott, J., Coryell, W., Warshaw, M., & Maser, J. D. (1999). Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. American Journal of Psychiatry, 156(7), 1000–1006. https://doi.org/10.1176/ajp.156.7.1000
- Myklebost, S. B., Nordgreen, T., & Hammar, Å. (2021). An open pilot study of an internet-delivered intervention targeting self-perceived residual cognitive symptoms after major depressive disorder. Applied Neuropsychology: Adult, 1–10. https://doi.org/10.1080/23279095.2021.1901706
- Nordgreen, T., Blom, K., Andersson, G., Carlbring, P., & Havik, O. E. (2019). Effectiveness of guided Internet-delivered treatment for major depression in routine mental healthcare – An open study. Internet Interventions, 18, 100274. https://doi.org/10.1016/j.invent.2019.100274
- Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68–78. https://doi.org/10.1037/0003-066X.55.1.68
- Saragoussi, D., Haro, J.-M., Boulenger, J.-P., Jönsson, B., Knapp, M., Caillou, H., Chalem, Y., Milea, D., & François, C. (2013). Patient-reported cognitive dysfunction negatively impacts functioning in patients with major depressive disorder – Preliminary findings from the PERFORM study. Value in Health, 16(7), A543–A544. https://doi.org/10.1016/j.jval.2013.08.1383
- Schmid, M., & Hammar, Å. (2013). Cognitive function in first episode major depressive disorder: Poor inhibition and semantic fluency performance. Cognitive Neuropsychiatry, 18(6), 515–530. https://doi.org/10.1080/13546805.2012.754748
- Semkovska, M., & Ahern, E. (2017). Online neurocognitive remediation therapy to improve cognition in community-living individuals with a history of depression: A pilot study. Internet Interventions, 9, 7–14. https://doi.org/10.1016/j.invent.2017.04.003
- Semkovska, M., Quinlivan, L., O'Grady, T., Johnson, R., Collins, A., O'Connor, J., Knittle, H., Ahern, E., & Gload, T. (2019). Cognitive function following a major depressive episode: A systematic review and meta-analysis. The Lancet Psychiatry, 6(10), 851–861. https://doi.org/10.1016/S2215-0366(19)30291-3
- Spasojević, J., & Alloy, L. B. (2001). Rumination as a common mechanism relating depressive risk factors to depression. Emotion (Washington, D.C.), 1(1), 25–37. https://doi.org/10.1037/1528-3542.1.1.25
- Svanborg, P., & Åsberg, M. (1994). A new self-rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale . Acta Psychiatrica Scandinavica, 89(1), 21–28. https://doi.org/10.1111/j.1600-0447.1994.tb01480.x
- Svanborg, P., & Åsberg, M. (2001). A comparison between the Beck Depression Inventory (BDI) and the self-rating version of the Montgomery Åsberg Depression Rating Scale (MADRS). Journal of Affective Disorders, 64(2-3), 203–216. https://doi.org/10.1016/S0165-0327(00)00242-1
- Twamley, E. W., Vella, L., Burton, C. Z., Heaton, R. K., & Jeste, D. V. (2012). Compensatory cognitive training for psychosis: Effects in a randomized controlled trial. The Journal of Clinical Psychiatry, 73(9), 1212–1219. https://doi.org/10.4088/JCP.12m07686
- Wells, A. (1990). Panic disorder in association with relaxation induced anxiety: An attentional training approach to treatment. Behavior Therapy, 21(3), 273–280. https://doi.org/10.1016/S0005-7894(05)80330-2
- Wykes, T., Huddy, V., Cellard, C., McGurk, S. R., & Czobor, P. (2011). A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. The American Journal of Psychiatry, 168(5), 472–485. https://doi.org/10.1176/appi.ajp.2010.10060855
- Yardley, L., Morrison, L., Bradbury, K., & Muller, I. (2015). The person-based approach to intervention development: Application to digital health-related behavior change interventions. Journal of Medical Internet Research, 17(1), e30. https://doi.org/10.2196/jmir.4055
- Yardley, L., Spring, B. J., Riper, H., Morrison, L. G., Crane, D. H., Curtis, K., Merchant, G. C., Naughton, F., & Blandford, A. (2016). Understanding and promoting effective engagement with digital behavior change interventions. American Journal of Preventive Medicine, 51(5), 833–842. https://doi.org/10.1016/j.amepre.2016.06.015