Abstract
Purpose state: Orthotic wearing time may be an important confounder in efficacy studies of treatment in children with spastic cerebral palsy (SCP). Most studies measure parent-reported wearing time (WTparent) with questionnaires, but it is questionable whether this yields valid results. This study aims to compare WTparent with objectively measured wearing time (WTobj) in children with SCP receiving orthotic treatment.
Method: Eight children with SCP participated in this observational study. For one year, they received knee-ankle-foot orthosis (KAFO) treatment. WTparent was measured using questionnaires. WTobj was measured using temperature sensor-data-loggers that were attached to the KAFOs. The 2.5th and 97.5th percentiles and median of differences between methods (per participant) were used to calculate limits of agreement and systematic differences.
Results: There was no systematic difference between WTparent and WTobj (0.1 h per week), but high inter-individual variation of the difference was found, as reflected by large limits of agreement (lower limit/2.5th percentile: −1.7 h/week; upper limit/97.5th percentile: 11.1 h/week).
Conclusions: Parent-reported wearing time (WTparent) of a KAFO differs largely from objectively measured wearing time (WTobj) using temperature sensors. Therefore, parent-reported wearing time (WTparent) of KAFOs should be interpreted with utmost care.
Low wearing time of orthoses may be a cause of inefficacy of orthotic treatment and incorrect reported wearing time may bias results of efficacy studies.
Results of this study show that parent-reported wearing time is not in agreement with objectively measured wearing time.
Parent-reported wearing time of KAFOs should be interpreted with utmost care.
Objective methods are recommended for measuring orthotic wearing time.
Implications for Rehabilitation
Introduction
According to the International Society for Prosthetics and Orthotics consensus document,[Citation1,Citation2] orthotic treatment is applied in efforts to prevent deformities and muscle shortening in children with spastic cerebral palsy (SCP). Applying a high tensile strain onto muscles by stretching the muscle tendon complex using orthoses is presumed to increase joint range of motion or prevent its loss.[Citation2] Wearing time is an important factor in determining effectiveness, as efficacy of treatment with orthoses is suggested to be dependent on duration that muscles are strained.[Citation3] Two recent studies,[Citation4–6] investigating the efficacy of ankle-foot orthoses (AFO) and knee-ankle-foot orthoses (KAFO) straining the calf muscles, used questionnaires filled in by the participant’s parents to assess wearing time. However, it is questionable whether such parent-reported wearing time (WTparent) is a valid measure.
Research focusing on objective methods to measure wearing time has been reported for patients with scoliosis, wearing spine orthoses. Several objective methods are available, such as data acquisition using temperature sensors [Citation7–10] or using force transducers [Citation9,Citation11] attached to the orthoses. These methods yielded reliable and valid wearing time estimates.[Citation7–11] Temperature sensors have been mentioned as most feasible with good agreement with actual wearing time, with no reported mechanical problems and the sensors being easy to use.[Citation9]
Objective measures have been used for comparison of self-reported wearing time and actual wearing time (further referred to as objectively measured wearing time (WTobj)). Previous studies assessing the reliability and validity of self-reported wearing time measurements in patient with spine orthoses showed that, in general, self-reports by patients or parents led to overestimation.[Citation8,Citation12–16] In particular cases, patient-reported wearing time was twice the WTobj.[Citation14,Citation16] Also children with clubfoot deformities, who were wearing a foot abduction orthosis, patient-reported wearing time (by parents) was overestimated.[Citation17] In efficacy studies, such overestimation may lead to erroneous conclusions if orthoses were not worn long enough to be effective.
To the best of our knowledge, in children with SCP who wear KAFOs or other orthoses to prevent loss of ankle-foot range of motion, WTparent has not been compared to WTobj. As wearing instructions, aim of treatment and design of orthoses are different from patients wearing spine orthoses, validity of WTparent may vary from the above described studies. Therefore, we aim to compare WTparent in children with SCP, collected using questionnaires, and WTobj, measured using temperature sensor-data-loggers attached to the KAFO. It is hypothesised that WTparent differs from objective measurements.
Methods
This observational study is part of a randomized controlled trial that tested the efficacy of KAFO treatment. Approval for this study was obtained from the Medical Ethics Committee of VU University Medical Center.[Citation4,Citation5] All participants (if older than 12 years) and their parents signed an informed consent form.
Participants and study design
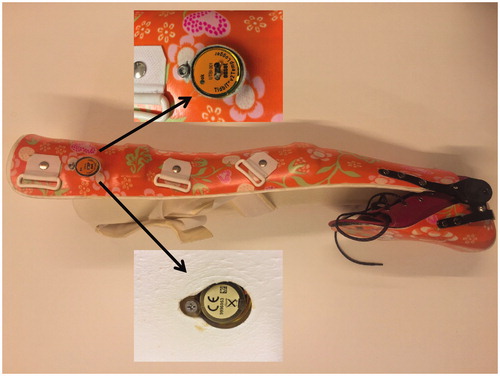
All children participating in this study were also participants in the experimental group of a multi-centre study investigating the efficacy of KAFOs to prevent equinus in children with SCP (Splint study [Citation4,Citation5]). In the Splint study, 30 children were recruited and 17 of them were randomized to the KAFO group. They were recruited between February 2010 and April 2012. The KAFOs of children who were recruited in Amsterdam or Venlo (eight children, allocation was determined by the child’s residence) were equipped with a temperature sensor-data-logger to measure wearing time (). These eight children were included in the present study. Although the sensor-data-logger was visible for the participants, they were not informed about the actual aim of the device. Besides that wearing time was measured objectively, parents of participants were asked to report KAFO wearing time for their child. The participants were aged between 4 and 16 years and were able to walk independently (gross motor function classification system (GMFCS) level of I–II) or with walking aids (GMFCS level III).[Citation18] All participants were instructed to wear KAFOs for at least 6 h every other night.
Figure 1. The temperature sensor-data-logger attached to the KAFO. The KAFO as shown in the figure is configured with a fixed knee angle and a variable ankle angle using a spring that provides variable ankle dorsiflexion. The temperature sensor-data-logger was attached to the KAFO with a nut (upper inset) and bolt (lower inset). The flat side (lower inset) of the sensor-data-logger touched the participants skin while wearing the KAFO.
Measurements
WTparent in hours/week, was collected using questionnaires. For all days of the 4th week of each month during the treatment period, parents of participants were asked to complete online questionnaires. These questionnaires were sent to the parents by email (Netquestionnaire Nederland B.V., Utrecht, The Netherlands). A reminder was sent after two weeks if parents did not respond. The following multiple choice question was asked: “How many hours did your child wear his/her KAFO?”. Answers were given as seven categories, ranging from 0–1 h to 6 h or more.
WTobj in hours/week, was measured with a temperature sensor-data-logger (UTBI-001, Onset Computer Corporation, Bourne, MA) during the treatment period. The sensor-data-logger was embedded in the shelf of the KAFO, touching upper-leg skin of the participant. Temperature was recorded every 15 min. KAFO wearing time was derived from time–temperature data. An increase of at least 3 °C in temperature within 45 min, indicated that the KAFO was put on. As KAFO temperature is not expected to increase over normal body temperature (37 °C), periods with higher temperatures were ignored, because it was assumed that these temperature increases were artefacts caused by external heating (e.g., KAFO exposed to direct sunlight or heater radiation). The KAFO was assumed to be removed if temperature decreased to values similar to previous periods that KAFO was not worn.
Analyses
For each participant, WTparent and WTobj per week were calculated for all weeks that data of both methods were available. A week was only analysed if WTparent and WTobj measurements were available for at least four days. If only 4–6 days of a week were available, wearing time of those days was used to estimate total wearing time of seven days. For WTparent, the centre value of each time category (i.e., 0.5 for 0–1 h, 1.5 for 1–2 h up to 6.5 for 6 h or more) was used to calculate total wearing time of the week.
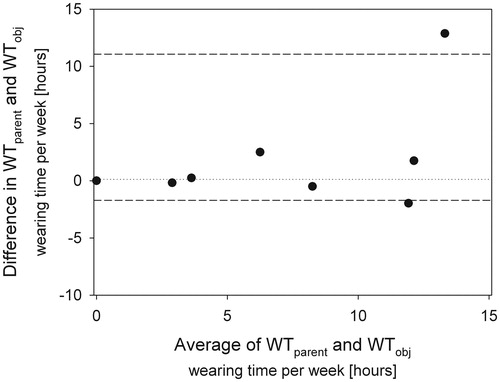
Agreement between the two methods was assessed according to the non-parametric Bland and Altman method.[Citation19] The non-parametric method was used because of violation of normal distribution of data due to some extreme values for differences in wearing time between measurement methods. For each participant, median of the differences between both measurement methods per week was determined. In addition, the group median of differences and 2.5th and 97.5th percentile score were determined, reflecting the systematic difference between methods and limits of agreement, respectively.
Results
Temperature sensor data were available for eight participants of the Splint study (mean age: 8.7 ± 1.9 years; gender: six males, two females; GMFCS: level I (n = 2), level II (n = 4), III (n = 2)). The period of KAFO treatment of four participants was shorter than one year because other treatment (e.g., botulinum toxin treatment) was indicated clinically (n = 3) or the KAFO caused too much discomfort (n = 1) and therefore the protocol was not finished. As a consequence, KAFO treatment varied from two months to one year. Individual response to questionnaires ranged from 22 to 100% with a median of 87%. For about 25% of the sent questionnaires, reminders had to be sent. Acceptable time–temperature data that was available per participant ranged from 10 to 100% (median: 66%). Missing time–temperature data was caused by (1) too high air temperature because of weather conditions, leading to a too small increase in temperature if the KAFO was worn (3% of total missing time–temperature data) or (2) technical problems with sensor-data-loggers (due to sensor failure that was not related to KAFO wearing), leading to empty data-files (97% of total missing time–temperature data). The period that data of both WTparent and WTobj were available ranged from 1 to11 weeks per participant, with a median of three weeks.
Individual median, interquartile range, minimum and maximum values of WTparent and WTobj are presented in . Temperature data show that KAFO wearing time was lower than prescribed and in one case, KAFO wearing time was 0 h. In addition, data show that, in some participants, there were large differences between WTparent and WTobj. The median of these differences per week are shown per participant in . This figure shows that there was no systematic difference between both methods (median: 0.13 h per week), but that differences between methods show large variability between participants (ranging from −2.0 to 12.9 h per week), resulting in large limits of agreement (lower limit/2.5th percentile: −1.7 h per week; upper limit/97.5th percentile: 11.1 h per week). This indicates that agreement between methods is low.
Figure 2. Box-and-whisker plots of wearing time per week per participant. Comparison of parent-reported wearing time per week (WTparent) and objectively measured wearing time per week (WTobj) per participant. Numbers of weeks included in analyses are for each participant noted on the x-axis. For participant 107, WTparent and WTobj were reported and measured as 0 h per week. The middle line of each box shows the median wearing time. The outer lines of each box show the 25th and 75th percentile of the wearing times and the end of the whiskers shows the maximum and minimum values.
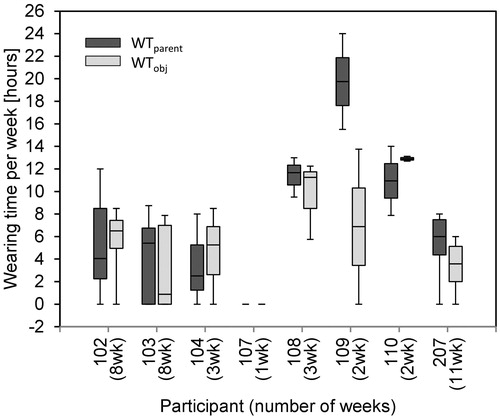
Figure 3. Bland–Altman plot: median differences per participant. Bland–Altman plot of parent-reported wearing time per week (WTparent) and objectively measured wearing time per week (WTobj). Upper and lower dotted lines indicate limits of agreement (2.5th and 97.5th percentile). Dotted line in middle indicates median of the difference between WTparent and WTobj for all participants.
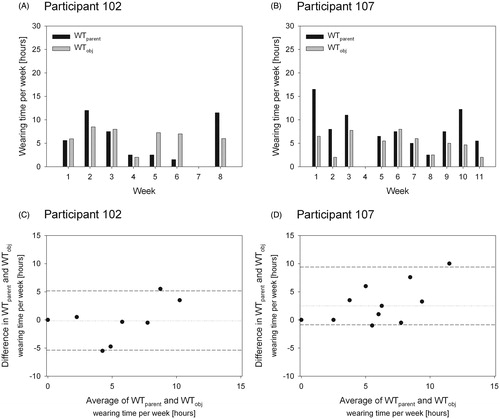
Comparing measurements within participants, a high variability in differences between the two methods was shown as well. Individual data of weekly measurements of two participants is shown in . For participant 102, WTparent ranged from 0 to 12 h per week, while WTobj ranged from 0 to 8.5 h per week (). Differences between WTparent and WTobj ranged from −5.5 to 5.5 h per week with a median of 0 h per week (). For participant 207, WTparent ranged from 0 to 16.5 h per week, while WTobj ranged from 0 to 8.5 h per week (). Differences between WTparent and WTobj ranged from −1 to 10 h per week with a median of 2.5 h per week. The wide range of within participant difference between WTparent and WTobj was also expressed in high individual limits of agreement (see , participant 102: lower limit/2.5th percentile: −5.4 h per week, upper limit/97.5th percentile: 5.2 h per week; participant 207: lower limit/2.5th percentile: –0.9 h per week, upper limit/2.5th percentile: 9.4 h per week).
Figure 4. Individual data: examples. A + B: comparison of parent-reported wearing time per week (WTparent) and objectively measured wearing time per week (WTobj) for two participants. If no column is visible, wearing time is 0 h. C + D: Bland–Altman plot of parent-reported wearing time per week (WTparent) and objectively measured wearing time per week (WTobj) for the same participants as in A + B. Upper and lower dotted lines indicate limits of agreement (2.5th and 97.5th percentile). Dotted line in middle indicates median of the difference between WTparent and WTobj for all measurements.
Discussion
The present study shows that WTparent of KAFOs differs from WTobj. The differences in reported wearing time between methods vary considerably per participant: some parents reported higher wearing times than what was measured by temperature sensor-data-loggers while others reported lower wearing times. In literature regarding spine orthoses, mostly overestimation of self reported wearing time/WTparent is reported (differences range from 0 to 150%).[Citation8,Citation12–16] It should be noted that these conclusions are often based on means of all participants. In accordance with the reported range of differences between wearing time measurement methods, the present study found no systematic difference or at most a small overestimation of WTparent. The large range of overestimation reported in literature may indicate a similar trend as found in this study that self reported wearing time/WTparent and WTobj varies considerably between participants. Therefore it may be concluded that WTparent and WTobj are not comparable.
In the present study, high values of limits of agreement between WTparent and WTobj were found. If the WTobj method is considered as a golden standard, the limits of agreement reflect the error of WTparent. In the present study, the limits of agreement indicate that only if parents reported that the KAFO was worn for more than 11 h per week, it can be concluded with certainty that the KAFO was worn for at least a short period. However, participants often did not wear their KAFO for such long period in general (i.e., shows that participant 102 and 207 did wear their KAFO not more than 8.5 h per week). This indicates that parent reported wearing time cannot distinguish whether participants wore their KAFO or not. It should be noted that one outlying value (participant 109, ) affected error of parent-reported outcome considerably. However, sub-analyses excluding this outlier still showed an upper limit of agreement of 2.4 h per week. Taking into account that the median of WTobj of the remaining seven participants was about 5 h per week, agreement between methods is still very low.
The response rate of questionnaires was relatively high (approximately 85%). Additional correlation analysis showed that there was no correlation between response rate and agreement between WTparent and WTobj (Spearman’s rho =0.252, p= 0.5). Another factor possibly affecting agreement was delayed response to questionnaires: it was often necessary to send reminders to parents after two weeks. This may indicate that parents did not complete questionnaires on the day of KAFO wearing and may explain the variability in response. However, uncertainty about delayed responses and therefore variable recall time will always be part of any parent report method. In this study, WTparent could not be influenced by the results of WTobj when WTparent response was delayed because parents and children were not informed about the actual aim and results of the temperature sensor-datalogger. Overestimation in WTparent was larger compared to under estimation: some parents reported KAFO wearing for periods that the temperature-data-logger did not register any higher temperatures. This may be the result of a more general phenomenon that people adjust their answers according to socially desired answers. It is unknown whether other methods of self-reporting may yield more accurate results.
Due to validity problems of parent-reported wearing time, we recommend the use of objective techniques to measure KAFO wearing time. We agree with Hunter et al.,[Citation9] that it is feasible to use temperature sensor-data-loggers to measure KAFO wearing time. However, the high percentage of missing data with the current device indicates that technical failures can occur and need to be solved. In this study, we were able to collect data for each participant after replacing the nonfunctioning sensors. In most datasets, it was straightforward to distinguish KAFO wearing from non-KAFO wearing using criteria described above. However, at high ambient temperatures (about 25 °C), it is more difficult to determine KAFO wearing time because differences in temperature with or without a leg in the KAFO was smaller. Comparison of data from temperature sensors inside the KAFO and additional outside temperature sensors [Citation20] may solve this problem.
Limitations of the study
A limitation of this study is the low number of participants. Non-parametric Bland–Altman plots are less reliable in small sample sizes.[Citation19] However, because of the large intra-individual variation, we believe that research using larger samples will yield similar conclusions.
A second limitation is that WTparent was assessed by only one method and cannot be generalized to other self/parent-reporting wearing time methods. We chose to send online questionnaires during each day. This was only done for every 4th week of the month to decrease burden on participants.
Applications to clinical practice
Measuring parent-reported orthotic wearing time with online daily questionnaires for one week per month does not show to agree with objective measurements using a temperature sensor-data-logger. Outcome of parent-reported questionnaires has to be interpreted with extreme care.
Conclusions
Wearing time of a KAFO assessed by questionnaires is not in agreement with of wearing time assessed by temperature sensor-data-loggers and should therefore be interpreted with utmost care. Using objective measurement methods is preferred. Regarding temperature sensors, we recommend to use a more sophisticated method than used in this study to measure orthotic wearing time with temperature sensor-data-loggers, like the method described by Bus et al.,[Citation20] in order to overcome difficulties in determining orthotic wearing time at high ambient temperatures.
Acknowledgements
We thank all participants and their parents for their participation in this study. We also thank OIM/Noppe orthopedie, Noordwijkerhout, the Netherlands; Kamer orthopedie, Amsterdam, the Netherlands; and Orthopedie Heckert & van Lierop, Venlo, the Netherlands for their cooperation.
Disclosure statement
The authors report no declarations of interest.
Additional information
Funding
References
- Condie DN, Meadows CB. Report of a Consensus Conference on the Lower Limb Orthotic Management of Cerebral Palsy; 1995; Copenhagen, International society of Prosthetics & Orthotics.
- Morris C, Condy D. Recent developments in healthcare for cerebral palsy: implications and opportunities for orthotics. Copenhagen, Denmark: International Society for Prosthetics and Orthotics; 2009.
- Tardieu C, Lespargot A, Tabary C, et al. For how long must the soleus muscle be stretched each day to prevent contractures. Dev Med Child Neurol. 1988;30:3–10.
- Maas J, Dallmeijer A, Huijing P, et al. A randomized controlled trial studying efficacy and tolerance of a knee-ankle-foot orthosis used to prevent equinus in children with spastic cerebral palsy. Clin Rehabil. 2014;28:1025–1038.
- Maas JC, Dallmeijer AJ, Huijing PA, et al. Splint: the efficacy of orthotic management in rest to prevent equinus in children with cerebral palsy, a randomised controlled trial. BMC Pediatr. 2012;12:38.
- Zhao X, Xiao N, Li H, et al. Day vs. day-night use of ankle-foot orthoses in young children with spastic diplegia: a randomized controlled study. Am J Phys Med Rehabil. 2013;92:905–911.
- Benish BM, Smith KJ, Schwartz MH. Validation of a miniature thermochron for monitoring thoracolumbosacral orthosis wear time. Spine (Phila Pa 1976). 2012;37:309–315.
- Helfenstein A, Lankes M, Ohlert K, et al. The objective determination of compliance in treatment of adolescent idiopathic scoliosis with spinal orthoses. Spine (Phila Pa 1976). 2006;31:339–344.
- Hunter LN, Sison-Williamson M, Mendoza MM, et al. The validity of compliance monitors to assess wearing time of thoracic-lumbar-sacral orthoses in children with spinal cord injury. Spine (Phila Pa 1976). 2008;33:1554–1561.
- Rahman T, Borkhuu B, Littleton AG, et al. Electronic monitoring of scoliosis brace wear compliance. J Child Orthop. 2010;4:343–347.
- Havey R, Gavin T, Patwardhan A, et al. A reliable and accurate method for measuring orthosis wearing time. Spine (Phila Pa 1976). 2002;27:211–214.
- Donzelli S, Zaina F, Negrini S. In defense of adolescents: they really do use braces for the hours prescribed, if good help is provided. Results from a prospective everyday clinic cohort using thermobrace. Scoliosis. 2012;7:12.
- Morton A, Riddle R, Buchanan R, et al. Accuracy in the prediction and estimation of adherence to bracewear before and during treatment of adolescent idiopathic scoliosis. J Pediatr Orthop. 2008;28:336–341.
- Nicholson GP, Ferguson-Pell MW, Smith K, et al. The objective measurement of spinal orthosis use for the treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2003;28:2243–2250.
- Takemitsu M, Bowen JR, Rahman T, et al. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29:2070–2074.
- Vandal S, Rivard CH, Bradet R. Measuring the compliance behavior of adolescents wearing orthopedic braces. Issues Compr Pediatr Nurs. 1999;22:59–73.
- Morgenstein A, Davis R, Talwalkar V, et al. A randomized clinical trial comparing reported and measured wear rates in clubfoot bracing using a novel pressure sensor. J Pediatr Orthop. 2015;35:185–191.
- Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–223.
- Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–160.
- Bus SA, Waaijman R, Nollet F. New monitoring technology to objectively assess adherence to prescribed footwear and assistive devices during ambulatory activity. Arch Phys Med Rehabil. 2012;93:2075–2079.
