 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
To investigate changes in wheelchair propulsion technique and mechanical efficiency across first five weeks of active inpatient spinal cord injury rehabilitation and to compare the outcomes at discharge with experienced wheelchair users with spinal cord injury.
Methods
Eight individuals with recent spinal cord injury performed six weekly submaximal exercise tests. The first and last measurement additionally contained a wheelchair circuit and peak graded exercise test. Fifteen experienced individuals performed all above-mentioned tests on one occasion.
Results
Mechanical efficiency and propulsion technique did not change during the five weeks of inpatient rehabilitation. Peak power output during peak graded test and performance time on the wheelchair circuit improved between the first and the last week. No difference in propulsion technique, peak power output, and performance time was found between the persons with a recent injury and the experienced group. Mechanical efficiency was higher after the correction for the difference in relative power output in the experienced group.
Conclusion
The group with a recent injury did not improve mechanical efficiency and propulsion technique over the period of active rehabilitation, despite significant improvements on the wheelchair circuit and in work capacity. The only significant difference between the groups was found in mechanical efficiency.
The lack of time-dependent changes in mechanical efficiency and propulsion technique in the group with a recent spinal cord injury, combined with the lack of differences in technique, work capacity and on the wheelchair circuit between the groups, suggest that important adaptations of motor learning may happen even earlier in rehabilitation and emphasize that the group in active rehabilitation was relatively skilled.
Standardized observational analyses of handrim wheelchair propulsion abilities during early spinal cord injury rehabilitation provide detailed understanding of wheelchair technique, skill as well as wheelchair propulsion capacity.
Measurement of external power output is critical to interpretation of gross efficiency, propulsion technique, and capacity.
Wheelchair quality and body weight – next to wheelchair fitness and skill – require careful consideration both in early rehabilitation as well as in the chronic phase of spinal cord injury.
Implications for rehabilitation
Introduction
Proficiency in functional manual wheelchair skill is a key to independence among many individuals with a spinal cord injury (SCI). Low levels of wheelchair skill relate to social isolation and dependence on others [Citation1,Citation2]. In contrast, a high level of skill corresponds to higher independence, self-efficacy, participation, and quality of life [Citation2,Citation3]. Even though the motor learning process of wheelchair skill is considered “highly typical and important” [Citation4], it is seldom studied during early rehabilitation. In this study, we will describe the motor learning process of wheelchair skill across the period of active SCI rehabilitation and beyond.
Motor learning of functional wheelchair skill is a complex and multidimensional phenomenon, emerging from an interplay among various levels and constraints. The most frequently used outcome measures for the motor learning process of wheelchair skill are mechanical efficiency (ratio between energy expenditure and power output) and biomechanical aspects of propulsion technique measured by instrumented wheels [Citation5–7]. A previous study on the motor learning process in wheeled mobility showed that improvements in propulsion technique, such as increasing the contact angle of the hand on the handrim and lowering the push frequency relate to an increase in mechanical efficiency [Citation6]. Although mechanical efficiency has been shown to improve between the beginning of active rehabilitation (moment when the participant can sit in the wheelchair for three consecutive hours) and three months after [Citation8], longitudinal changes in wheelchair propulsion technique during active SCI rehabilitation were not documented so far. Additionally, it is uncertain when the largest changes in efficiency took place as the mentioned study measured only at the beginning of active rehabilitation and 3 months after but not in between these test occasions. Considering that evidence from the able-bodied literature suggests that early motor learning process of handrim wheelchair skill is rapid [Citation6], it is crucial to intensify the frequency of the measurement occasions. Therefore, mechanical efficiency and propulsion technique in the current study will be measured longitudinally, once a week, across 5 weeks, starting at the beginning of active rehabilitation.
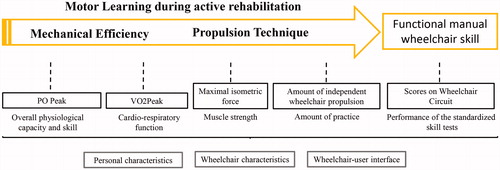
Mechanical efficiency in itself does not pinpoint where the change came from, therefore other factors that may influence the change in efficiency will be measured as well during the first and the last measurement moment (). These factors will include: the cardiorespiratory and muscle function (increase in mechanical efficiency can be caused by an increase in overall physiological capacity) and the amount of independent wheelchair propulsion (amount of wheelchair propulsion practice may contribute to the rate of the learning process) [Citation9]. Moreover, in order to show how the above-mentioned outcome measures relate to a commonly performed clinical measure, which is simple, cheap and easy to administer, the score on the wheelchair skill circuit will also be included [Citation10].
Figure 1. Acquiring functional manual wheelchair skill in the process of motor learning is a goal of rehabilitation. Considering the complexity and multidimensionality of the functional wheelchair skill, a number of factors needs to be taken in account to describe it. Although this study will not look at the association of mechanical efficiency and propulsion technique with other factors, we decided to include them here, to provide a complete picture of the multidimensional changes in physiology and skill during active SCI rehabilitation. Personal and wheelchair factors, as well as the wheelchair-user interface are not the focus of this study but it should be kept in mind that they could potentially influence both the baseline level of motor skill as well as the pace of the motor learning process.
Thus, the goal of this study is to investigate the longitudinal change in wheelchair propulsion technique and mechanical efficiency across five weeks of active in-patient SCI rehabilitation. In order to give an indication about the level of motor skill of the participants with a recent SCI at discharge from active rehabilitation, we will compare their outcomes with a group of experienced community-dwelling wheelchair users with a SCI. Wheelchair propulsion technique and mechanical efficiency in both groups will be presented in a context of related factors: physiological adaptation (peak power output, peak oxygen consumption, bimanual isometric wheelchair-specific force), amount of practice (only in the longitudinal analysis) and level of functional wheelchair skills. We hypothesize that the group with a recent SCI will show improvement on all measured parameters across the duration of active SCI rehabilitation. Moreover, we expect the experienced wheelchair users with SCI to have a better propulsion technique, higher mechanical efficiency, achieve better results during the peak test and show better skills and higher strength than the group with a recent SCI. Quantifying wheelchair performance across and beyond the active SCI rehabilitation can help to point out the factors that may need more attention during active rehabilitation.
Methods
Participants and ethics statement
Eight individuals with a recent SCI and 16 experienced wheelchair users with SCI participated voluntarily in this study (). All participants signed an informed consent before the onset of the experiment after receiving detailed written and verbal information about the character of the study and the nature and frequency of the measurements. The protocol of the study was approved by the Medical Ethical Committee, University Medical Center Groningen, The Netherlands (METC 2016/147; ABR: NL57063.042.16).
Table 1. Propulsion technique variables. All variables except cadence were calculated as an average value of all pushes performed during the last minute of each practice block. Equations from Vegter et al [Citation6].
The group with a recent SCI was recruited from the clinical patient pool who were actively following inpatient rehabilitation at the Center for Rehabilitation, University Medical Center Groningen at the time of the study. Experienced participants were recruited from the out-patient population of the same center.
Criteria for inclusion were: having a recent SCI (for the longitudinal group); time since SCI >2 years (for the experienced participants); expected manual wheelchair dependency; age between 18–65 years. Exclusion criteria were: having any cardiovascular contra-indications for testing according to the American College of Sports Medicine guidelines [Citation11], or a resting diastolic blood pressure above 90 mm Hg or a resting systolic blood pressure above 180 mm Hg; insufficient knowledge of the Dutch language to understand the test instructions; progressive disease e.g., cancer or multiple sclerosis; psychiatric problem; pregnancy.
Study design
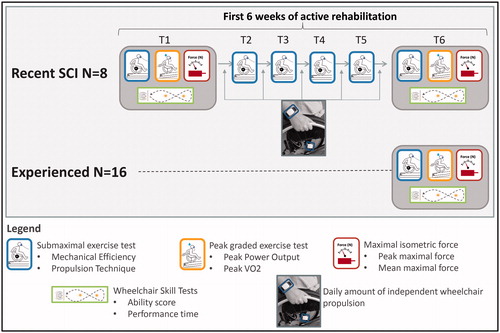
Both groups underwent a medical screening before the first measurement, to make sure they could safely participate in physical exercise testing. Screening was performed by a rehabilitation physician specialized in the post-SCI care. Participants in the group with a recent SCI performed six weekly measurements (). First measurement took place at the start of active rehabilitation which was defined as a moment when participants could sit in a wheelchair for 3 consecutive hours. This is in accordance with previous studies [Citation10] and ensured that participants were able to complete the first and last measurement moments which could take up to 3 h. Experienced participants performed one measurement. The last measurement in the group with a recent SCI was also the discharge measurement and it was used to compare the wheelchair skill between the recent SCI and experienced group. Six out of eight participants in the group with a recent SCI performed the T6 measurement within 2 days from discharge. The remaining two, within 1 and 2 weeks.
Figure 2. Study design. The first and the last measurement in the group with a recent SCI (N = 8) and the measurement in the experienced group (N = 16) contained the full test battery. The second to fifth measurement in the recent group were meant to monitor the motor learning process and consisted only of a submaximal test to determine mechanical efficiency and propulsion technique.
Experimental protocol
Screening
The screening aimed to determine whether any cardiovascular or musculoskeletal contraindications are present. The screening consisted of: lung and heart auscultation, measurement of the blood pressure, measurement of the resting ECG and screening for the cardiovascular contra-indications for testing according to the American College of Sports Medicine guidelines [Citation11]. Additionally the lesion characteristics (level and completeness according to American Spinal Injury Association International Standards for Neurological and Functional Classification of SCI, [Citation12] were established.
Drag test
Participants performed all tests in their own wheelchair which was either provided by the rehabilitation center (recent SCI) or in their personal daily wheelchair (experienced group). All changes to the wheelchair configuration, happening across the duration of the experiment in the group with a recent SCI, were recorded before each measurement occasion. Additionally, the rolling resistance of the wheelchair and user was determined before each measurement during a drag test on the motor-driven treadmill [Citation13,Citation14].
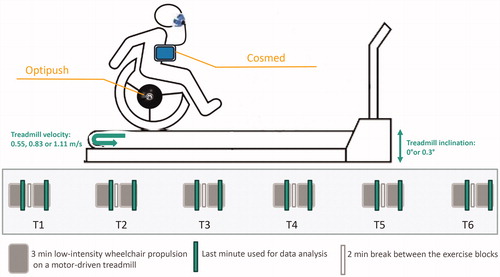
Motor learning outcomes during submaximal exercise test
Propulsion technique and mechanical efficiency were determined during standard submaximal exercise testing on a motor-driven treadmill (2 identical blocks of 3 min, with 2 min rest in between, ) [Citation8]. The last-minute of each submaximal exercise block was analyzed. The mean value of two blocks per measurement occasion was used as input for the statistical test. The velocity for the testing was chosen for each participant and equaled either 0.55, 0.83 or 1.11 m/s (depending on the physical capability of the participant). Same applied to the inclination of the treadmill which equaled either 0 or 0.3°. Testing conditions (treadmill velocity and inclination) chosen for each participant at the first measurement occasion were not altered throughout the duration of the experiment (protocol fixed over time for a participant).
Figure 3. The submaximal exercise test was performed at each measurement occasion in the group with a recent SCI. Treadmill velocity and inclination were chosen for each participant based on their capabilities and were kept unchanged throughout the experiment. The right wheel was exchanged for an instrumented wheel with the same diameter, which continuously recorded the wheelchair propulsion technique. Oxygen consumption was determined breath-by-breath.
Propulsion technique
During each submaximal test, the right wheel of the participant’s wheelchair was exchanged for an instrumented Optipush wheel (MAX Mobility, LLC, Antioch, TN, USA) with the same diameter as participant’s own wheels. The left wheel was exchanged for a dummy wheel with the same mass as the measurement wheel. The 3-dimensional forces and torques applied to the right handrim were continuously measured throughout the duration of each submaximal exercise test. The output registered by the measurement wheels was calculated into specific propulsion technique variables using custom-written Matlab algorithms [Citation6] ().
Mechanical efficiency
Oxygen uptake and respiratory exchange ratio during steady-state wheelchair propulsion were continuously determined breath-by-breath using Quark CPET (experienced group) or Quark K4β2 (group with a recent SCI) (Cosmed, Rome, Italy). Quark CPET or Quark K4β2 were also used to record the heart rate.
Mechanical efficiency was calculated over the last minute of each 3-min block. The equation used to calculate mechanical efficiency was: Mechanical efficiency = Power Output × Energy expenditure−1 × 100%, calculated according to the formula proposed by Garby and Astrup [Citation15].
Monitoring the amount of independent wheelchair propulsion
In order to quantify the amount of practice between the weekly submaximal exercise tests, participants in the group with a recent SCI continuously wore a set of two activity monitors between the first and the last measurement moment. Activ8 Professional Activity Monitor (2 M Engineering Ltd., Valkenswaard, The Netherlands) is a triaxial accelerometer. One accelerometer was worn on the dorsal side of the dominant wrist and one on the corresponding rear wheel. Each monitor stored the output on a 5 s epoch base. The vector counts were used to perform the classification. Classification was performed using custom-written Matlab algorithms, which were validated for detecting independent wheelchair propulsion [Citation9]. Each epoch was classified either as independent wheelchair propulsion (propulsion as a result of arm power of the participant) or as other activity (including but not limited to: being pushed in the wheelchair, reaching movements, general upper body motions). A given epoch was classified as independent wheelchair propulsion if the wheel counts were contained between 31 and 310 counts or if they exceeded 310 and at the same time wrist counts exceeded 98 [Citation9]. In all other cases, an activity was classified as “other”. The outcome of the activity monitoring was a number of seconds of independent wheelchair propulsion per day. Only full days were included in the data analysis. Participants were asked to keep a diary where they could indicate if they forgot to put on the wrist accelerometer so that those days were not included in the data analysis. The data of all available days in a week was used to calculate a daily average for each given week, which was then used in the analyses. Additionally, the five-week averages of all weekend days (Saturday and Sunday) and all weekdays (Monday to Thursday) were calculated to indicate whether there was a difference in the amount of practice between the days with scheduled therapy and without it. Fridays were not included in the analysis, as Friday was a test day. Participants were not wearing the activity monitors during the tests to not confound the results (longer testing procedure at T1 and T6 could result in more measured activity). Additionally, the batteries of the activity monitors needed to charge on Friday.
Wheelchair circuit
The Wheelchair Circuit is a test to assess manual wheelchair skill performance. It consisted of 10 different standardized tasks, 8 tasks originally implemented by Kilkens et al. [Citation10] and 2 tasks (holding a wheelie and propelling in a wheelie) proposed by Cowan et al., in order to attenuate floor and ceiling effects [Citation16]. The tasks were performed in a fixed sequence with 2-min breaks between consecutive items. The tasks, in order of performance, were (1) figure-of-8 shape; (2) 0.04-m doorstep crossing; (3) 0.10-m platform ascent; (4) 15.0-m sprint; (5) propelling for 10 s on a treadmill with a 3% inclination; (6) propelling for 10 s on a treadmill with a 6% inclination; (7) holding a wheelie for 10 s; (8) propelling 3 m in a wheelie; (9) making a level transfer; and (10) a 3-min wheeling test on the treadmill. All tests were performed either on a motor-driven treadmill or on an even linoleum floor. The beginning and end point of each test were marked with tape, which was placed on the ground. Participants were instructed to perform the tests as fast as possible. Time score was recorded manually with a stopwatch. Time was recorded from the moment the participant began to drive until the front wheels of the wheelchair passed the finish line. The results of the Wheelchair Circuit consisted of two test scores: ability score and performance time. The ability score is a sum of points awarded per task. Each task is scored either 0 (not able to perform) or 1 (able to perform) point. Three tasks i.e., doorstep crossing, platform ascent and transfer, can be awarded 0.5 point. The ability score ranges from 0 to 10. The performance score is a sum of the performance time of the figure-of-8 and the 15-m sprint.
Work capacity
Bimanual maximal isometric force test
The maximal isometric test is a wheelchair-specific test meant to measure the maximal force that a user can apply to the handrim while the wheelchair remains stationary. The participant, while sitting in the wheelchair, tries to push forward as hard as possible. The wheelchair remains stationary due to a cable, which connects the force transducer with the wheel axle [Citation17]. Each participant performed this test 3 times at a given measurement occasion. The last attempt was used in the data analysis.
Peak graded exercise test
This test consisted of 1-min exercise blocks where the velocity of the treadmill belt was held constant and the workload increased every 60 s by increasing the inclination of the treadmill (1 step each minute) [Citation18]. Velocity equaled the velocity chosen for the submaximal test. The test ended when the participant could no longer maintain his or her position on the belt as a consequence of exhaustion, or when the participant indicated that he/she wanted to stop. Oxygen uptake and heart rate were monitored continuously using Quark K4β2. Highest 30-s mean was calculated to acquire the values of peak oxygen uptake and peak heart rate. The peak power output achieved during the highest inclination maintained for at least 30 s was noted based on the results of the drag test.
Statistical analysis
All statistical analysis was performed using IBM SPSS Statistics version 21.0 (SPSS Inc., Chicago, IL, USA). An inspection of the frequency histogram per variable and the kurtosis and skewness values was performed to determine whether the data were normally distributed.
Longitudinal analysis in the group with a recent SCI
Data in the group with a recent SCI was not normally distributed and, therefore, non-parametric testing was used. If there was one missing data point for a certain participant for a given variable, the mean from the two adjacent data points was used to replace the missing value. This took place two times. If there was more than one missing data point, the participant was excluded from the analysis. The reasons for the missing data were: malfunction of the testing devices, participant being unable to complete a test because of spasms or in case of one participant, unwillingness to perform the peak graded exercise test. Total number of participants per variable is provided in the results section.
To analyze the longitudinal change (6 measurement moments per participant) in mechanical efficiency, propulsion technique variables and the amount of independent wheelchair propulsion, Friedman’s test was used. The difference in the amount of active propulsion during the average of weekend days and weekdays was determined using a Wilcoxon Signed Rank test.
Since the peak graded exercise test, wheelchair circuit and maximal isometric strength test were only performed at the first and the six measurement occasion, the change in the outcomes of those test was compared using Wilcoxon Signed Rank test.
Comparison between the participants with a recent SCI and experienced wheelchair users
Data used for the between-group comparison was normally distributed. Independent t-test was used to check for initial differences in continuous data between the recent SCI and experienced group. Chi-square was used to check for initial differences in categorical data (gender, lesion completeness, lesion level). Since relative power output during the submaximal test differed significantly between the groups, it was used as a correction factor as it influences both the propulsion technique and the mechanical efficiency [Citation19,Citation20]. Other outcomes i.e., work capacity and wheelchair skills were not corrected for differences in power output because it is not defined whether and how the power output influences all those outcome measures. One-way ANCOVA with a fixed factor (group) and covariate (relative power output) was implemented to compare the propulsion technique and mechanical efficiency between the experienced users and the group with a recent SCI at discharge (T6). To allow the reader an independent interpretation of the results, both analysis: with and without the covariate is presented in the results section. Significance for all above-mentioned tests was set at p < 0.05.
Results
The personal and lesion characteristics for both groups are presented in .
Table 2. Personal and lesion characteristics for the group with a recent SCI (N = 8) and the experienced group (N = 16).
Longitudinal analysis in the group with a recent SCI
Propulsion technique and mechanical efficiency during submaximal exercise test
All participants in the group with a recent SCI (N = 8) completed the testing protocol (). Power output during propulsion at a submaximal intensity did not change significantly throughout the experiment (X2(5) = 1.129, p = 0.952). On the group level, none of the propulsion technique variables or mechanical efficiency changed significantly across time. Individual moment around the wheel axis during the first and the last measurement occasion is presented per participant in .
Figure 4. Individual moment around the wheel axis during the first and the last measurement occasion for each participant in the group with a recent SCI (N = 8).
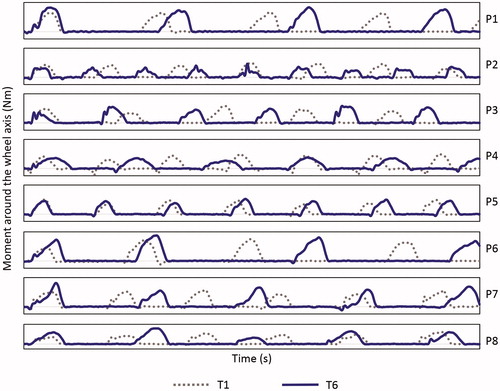
Table 3. Longitudinal course (T1–T6) in mechanical efficiency and propulsion technique in the group with a recent SCI and the course of the amount of independent wheelchair propulsion (bottom two lines).
Amount of independent wheelchair propulsion
The amount of independent wheelchair propulsion did not change significantly throughout the 5 weeks of active SCI rehabilitation (X2(4) = 5.057, p = 0.282) (). Participants were more active during the weekdays (Monday to Thursday) than in the weekend (Median = 6870 s (Range = 3684 s) vs 4999 s (7415 s), Z= −1.960, p = 0.049, 95% CI [30, 3374]).
Wheelchair circuit
Participants showed no significant improvement in the ability score (9 (4.5) → 9.5 (3), Z = 1.841, p = 0.066, 95% CI [0.1]) but exhibited a significant decrease in the performance time of the Figure-of-8 and 15 m sprint (17.6 s (11.2 s) → 16 s (8.6 s), Z= −2.521, p = 0.012, 95% CI [−2.5, −1.1]) ().
Table 4. Results of the wheelchair skill tests, maximal test and maximal force test performed in the group with a recent SCI at the pre- (T1) and the post-test (T6).
Work capacity
Maximal isometric force test
The group with a recent SCI managed to generate higher peak (589 N (467 N) → 621 N (488 N), Z = 2.100, p = 0.036, 95% CI [10, 81]) and mean forces (501 N (457 N) → 579 N (480 N), Z = 2.521, p = 0.012, 95% CI [29,112]) during the maximal isometric force test at the last measurement.
Peak graded exercise test
Participants increased the peak power output between the first (40 W (51 W)) and the last measurement (48 W (56 W); Z = 2.201, p = 0.028, 95% CI [4,10]) (). Peak oxygen consumption and peak heart rate did not change significantly (Z = 0.405, p = 0.686, 95% CI [−5, 29]).
Comparison between the participants with a recent SCI and experienced wheelchair users
Propulsion technique and mechanical efficiency during submaximal exercise test
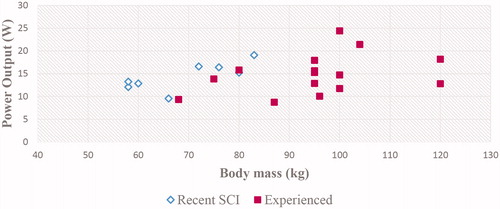
Relative power output in the people with a recent SCI was approximately 33% higher when compared to the experienced group (respectively 0.21 W/kg ± 0.03 W/kg vs 0.16 W/kg ± 0.04 W/kg, p = 0.006, 95% CI [0.02, 0.09]) (). Absolute power output did not differ significantly between the group with a recent SCI and the experienced group (14.4 W ± 3.0 vs 14.9 W ± 4.4 W, 3.086 (21), −0.270(21), p = 0.790, 95% CI [−0.5, 1.7]).
Table 5. Results of the between-group comparison. Effects with and without the relative power output correction.
Both with and without the inclusion of the covariate, there were no significant differences in propulsion technique between the recent SCI and the experienced group. In contrast, the difference in mechanical efficiency approached significance without correction and was higher in the group with a recent SCI (6.1%±0.7% vs 5.1 ± 1.3%, 1.865(20), p = 0.077, 95% CI [−0.1, 2.1]). After correcting for the difference in relative power output, the corrected mean mechanical efficiency was significantly higher in the experienced group (5.2%±0.2% vs 5.5%±0.2%, 36.028(2), p < 0.001, 95% CI [−1.0, 0.4]). Difference in heart rate during submaximal intensity propulsion approached significance (with as well as without the covariate) and was higher in the group with a recent SCI. Energy expenditure was significantly higher in the experienced group independent of whether the covariate was used or not.
Wheelchair circuit
The level of wheelchair skills was similar in both groups. The ability score in the group with a recent SCI (8.9 ± 1.3) did not differ significantly from the one in the experienced group (9.5 ± 1.1, −1.153(22), p = 0.261, 95% CI [−1.7, 0.5]). Both groups needed a similar amount of time to perform the 15 m sprint test and a Figure-of-8 (recent SCI 16.6 s ± 3.3 s vs experienced 15.5 s ± 3.5 s, 0.748(22), p = 0.463, 95% CI [−2.0, 4.2]).
Work capacity
Maximal isometric force test
The peak isometric force (recent SCI 552 N ± 202 N vs experienced 623 N ± 171 N, −0.905(22), p = 0.375, 95% CI [−234, 92]) and mean isometric force (recent SCI 510 N ± 188 N vs experienced 539 N ± 146 N, −0.421(22), p = 0.678, 95% CI [−173, 115]) that participants could generate did not differ significantly between the groups.
Peak graded exercise test
There were no significant differences between the recent SCI and experienced group in the peak oxygen consumption (1232 ml/min ± 414 ml/min vs. 1616 ml/min ± 568 ml/min, −1.506(20), p = 0.148, 95% CI [−917, 148]), peak power output (45.1 W ± 20.4 W vs 57.6 W ± 22.7 W, −1.178(20), p = 0.253, 95% CI [−34.6, 9.6]) and the peak heart rate (163 beats/min ± 32 beats/min vs 165 beats/min ± 26 beats/min, −0.112(19), p = 0.912, 95% CI [−27, 30]).
Discussion
The group with a recent SCI did not show significant improvements in the primary outcome measures of this study, the mechanical efficiency and propulsion technique, despite significant improvements on the wheelchair circuit performance score and in physical work capacity over the period of active rehabilitation and 5 weeks after. Moreover, the differences between the group with a recent SCI and experienced participants were less pronounced than hypothesized, with the only significant difference found in mechanical efficiency and no differences in propulsion technique, work capacity and on the wheelchair circuit scores.
Propulsion technique and mechanical efficiency during the submaximal exercise test
Longitudinal analysis in the group with a recent SCI
Contrary to our hypothesis, we found no significant improvements in propulsion technique and mechanical efficiency during 5 weeks of active inpatient rehabilitation in individuals with a recent SCI. This finding was surprising as in the previous studies, mechanical efficiency showed to improve in the first 3 months of active rehabilitation [Citation8,Citation21] and between the beginning and end of active SCI rehabilitation [Citation22]. A possible explanation for the lack of improvement in mechanical efficiency in the current study could be its duration, in total 5 weeks. The previous studies looked at changes after 3 months and then at discharge. This would not be possible here as the whole period of active rehabilitation for our participants was no longer than 10 weeks, since the length of stay in the rehabilitation center has been shortening progressively over the last years, due to policy changes and financial incentives [Citation23]. Future studies should consider extending the measurements beyond the discharge from active rehabilitation. This could help to observe the long-term changes in ME.
In previous literature, propulsion technique and mechanical efficiency showed to be sensitive to change in the early stages (12 min to 7 weeks) of learning in able-bodied participants [Citation5,Citation6,Citation19,Citation20]. This motivated our choice to initiate the measurements at the start of active rehabilitation. It is, however, important to realize, that in contrast to the able-bodied individuals [Citation5,Citation6,Citation19,Citation20], participants in the group with a recent SCI were not totally naïve to the task of wheelchair propulsion at the onset of the study as they received a wheelchair before the inclusion. Since even very short (12 min) and low-intensity practice can elicit significant changes in mechanical efficiency and propulsion technique [Citation6], it cannot be excluded that the rapid short-term changes took place before the onset of the present study. Perhaps starting measuring even earlier, for example from the moment when participants receive a manual wheelchair, would be able to capture the very early improvements in technique and efficiency. It is however arguable whether such study design would be feasible and ethically responsible.
Another explanation for the lack of significant group-level changes in propulsion technique could be the heterogeneity of the group with a recent SCI and resulting inter-individual differences in learning. The presence of individual learning trajectories in wheelchair propulsion was documented before [Citation7]. When comparing the torque signal around the wheel axis (), it is visible that P2 and P3 increased their push frequency and decreased the contact angle between T1 and T6. This direction is opposite to the one observed in the remaining 6 participants. It also contradicts previous literature which found a group-level decrease in push frequency and increase in contact angle of the hand on the handrim in early stages of motor learning process in novice able-bodied wheelchair users [Citation5,Citation6,Citation19]. The heterogeneity of changes in propulsion technique is difficult to interpret, especially considering the small group size in this study. It is however interesting to explore what caused these two individuals, presented with an identical task, to choose various movement strategies. Understanding the inter-individual differences in motor learning is a prerequisite to creating individualized therapies targeting the improvement in wheelchair skill.
Comparison between the participants with a recent SCI and experienced wheelchair users
The differences between the group with a recent SCI and experienced participants were less pronounced than hypothesized, with the only significant difference found in mechanical efficiency. It is quite unexpected that, independent of the relative power output correction, there were no significant differences in the wheelchair propulsion technique between the groups. The mean and standard deviation values for all technique variables were very similar. This finding is very surprising as previous studies found differences in propulsion technique between novice and expert users, both while propelling on the ergometer as during over-ground propulsion [Citation24,Citation25]. It should be considered that these studies included able-bodied persons with no previous wheelchair experience. In contrast, the group with a recent SCI was not totally naïve to the task of wheelchair propulsion.
Propulsion technique did not change significantly across active rehabilitation in the group with a recent SCI and there were no significant differences in technique between the groups with a recent and long-term SCI. Moreover, the overall values of frequency and contact angle in both groups resembled those reported in other studies with experienced wheelchair users with a SCI [Citation24,Citation26–29]. These findings support the earlier discussion point that at least some of the improvement in the propulsion technique in the group with a recent SCI could have taken place before the onset of the study.
Mechanical efficiency, in contrast to propulsion technique, was significantly different between the groups. The interpretation of this difference is, however, difficult as it completely changed direction after the relative power output correction. Without the power output correction, the mechanical efficiency in the group with a recent SCI (6.1%) was not significantly different from the experienced group (5.1%). This finding was unexpected as mechanical efficiency is known to be higher in experts [Citation30]. After the correction for the difference in relative power output between the groups, the direction of difference changed. Model estimated mean mechanical efficiency in the experienced group (5.5%) was significantly higher than in the group with a recent SCI (5.2%). The large difference in relative power output between the groups was rather striking. Since the power output and body mass showed only a moderate correlation, r = 0.36 (), the much higher body mass in the experienced group (93 kg vs 69 kg), did not explain the difference in relative power output between the groups. We did, however, notice that the wheelchairs in the experienced group were all individually fitted (while a group with a recent SCI received wheelchairs from the rehabilitation center without individual fitting) and much better maintained (no frame deformations, fluent rolling of the front wheels, rolling out symmetrically). The fact that a good wheelchair with a proper fitting might be at least partially capable of offsetting the effect of 25 kg of body mass emphasizes the need to provide properly fitted wheelchairs to patients as early as possible, with a goal of improving efficiency but also preventing shoulder overload injuries which are very common in the population with SCI [Citation31–35].
Figure 5. Scatter plot illustrating the relationship between body mass and absolute power output during submaximal exercise test in the group with a recent SCI (N = 8, x̄=14.4 W ± 3.0 W) and the experienced group (N = 16, x̄=14.9 W ± 4.4 W). With the large difference in body mass (24 kg), this leads to a respective relative power for the recent and experienced group of 0.21 W/kg and 0.16 W/kg (p = 0.006).
Amount of independent wheelchair propulsion
The amount of independent wheelchair propulsion across 5 weeks of active rehabilitation in the group with a recent SCI did not increase significantly. This is in contrast to another study which found that the level of dynamical activities increased during inpatient rehabilitation [Citation36]. Measurements in that study were obtained at the start of active rehabilitation, 3 months later and at discharge. The lack of significant difference in our study could be explained as we measured across a much shorter period of time. Also, the absolute amount of activity per day was different in our study. Van den Berg-Emons et al. [Citation36] found a level of dynamic activities at the beginning of active rehabilitation to be 3.4 ± 2.2% of a day (49 min ± 32 min), which is lower than in our study (94 min ± 68 min). The difference could be explained by the fact that the study of Van den Berg-Emons et al. excluded maneuvering from their results [Citation37] which constituted a substantial part of total activity in our study. We included maneuvering as the goal of this study was to quantify the amount of independent wheelchair propulsion practice and maneuvering is a part of that.
Next to the total amount of independent wheelchair propulsion per week we also looked at the difference between the weekend days and weekdays as there is no therapy scheduled during the weekend and participants spent roughly every weekend at home. We found that participants were significantly more active during the weekdays compared to the weekend. It could be that participants are less active during the weekends due to a lack of motivation or possibility to safely perform various activities. It could be that intervention specifically targeting amount of activity during periods when therapy is not provided is crucial for individuals with SCI to prevent a deterioration in overall wheelchair capacity and/or contribute to a greater increase in wheelchair capacity. This suggestion is supported by Berg-Emons et al [Citation36], who reported that the amount of dynamical activities decreased after discharge from rehabilitation.
Wheelchair circuit
The difference between T1 and T6 in scores on the wheelchair circuit showed that the group with a recent SCI significantly improved the performance of functional wheeled-mobility skills. Although the improvement agrees with other studies [Citation10,Citation38], the differences in absolute scores between the studies are remarkable. Median performance time score in the current study was much better, both at T1 (17.6 s) and at T6 (16 s) when compared to the mean scores acquired at the beginning of rehabilitation (28.7 s) and at discharge (19.4 s) in individuals with paraplegia in a previous study [Citation10]. It is interesting to add that the time between T1 and discharge in the previous study was on average 172 days [Citation10] while in the current study the period between T1 and T6, was 5 weeks, so only 35 days. Time since injury at T1 did not differ between the studies.
Contrary to our hypothesis the experienced group did not score significantly better on the wheelchair skill tests than the group with a recent SCI. The mean ability score differed by merely 0.6 point between the groups with both groups scoring high (recent SCI 8.9/10; experienced 9.5/10). Similarly, the mean performance time difference between the groups was 1.1 s. It is, therefore, safe to assume that this difference would have little effect on the functional capacity of the participants. Wheelchair circuit scores were reported previously to exhibit ceiling effect [Citation38]. It is however remarkable that the ceiling effect in the group with a recent SCI was found already at the start of rehabilitation and despite the fact that we added two relatively difficult skills: stationary wheelie and riding in a wheelie. Without the addition of those two tasks, using the scoring range of Kilkens et al. [Citation10] from 0 to 8, the difference between the recent SCI and experienced group would be even smaller (7.6 vs 7.7) Altogether, the results of wheelchair circuit suggest that the group with a recent SCI included in this study was quite skilled, already at the onset of rehabilitation and the chosen 10 skill tests did not allow to discriminate between the groups.
Work capacity
Generally speaking, all work capacity outcomes in both groups do not deviate from values reported for similar populations by other studies [Citation39,Citation40]. Work capacity, operationalized as wheelchair-specific isometric force and outcomes of the peak graded exercise test, improved significantly over the period of 5 weeks in the group with a recent SCI. Increase in both peak and mean isometric force between T1 and T6 is a desired outcome. It shows that participants improved force production and its application to the handrim. Additionally, they significantly improved the peak power output during the peak graded exercise test, which is considered to be an important measure for overall wheelchair capacity and skill. Higher peak power output relates to an increased chance for return to work after suffering a SCI [Citation41] and better quality of life [Citation42].
Surprisingly the difference in work capacity between the recent SCI and experienced group turned out to be smaller than expected. Even though there is a visible trend in all outcome measures favoring the experienced group, none of the differences were significant. This could be related to a heterogeneity within the groups which potentially masked some of the differences but could also be reflecting that the groups were actually quite similar in their work capacity. This again points out the possibility that the group with a recent SCI was quite skilled and relatively fit and therefore may not be entirely representative of all persons with a SCI in early rehabilitation.
Future recommendation
Apart from the findings that this study reported, there are two aspects that could be addressed in future studies and clinical practice to make sure that patients with SCI receive the best possible and evidence-based care. First of all, this study pointed out how different the current rehabilitation reality is when compared to that approximately 15 years ago. The length of stay in inpatient rehabilitation is progressively shortening which makes the results of studies conducted 10–15 years ago very difficult to use in rehabilitation programs. The same will most likely be true for the current study. The policy changes are galloping and considering the time needed to gather data for a study like the present one from one rehabilitation center (nearly 2 years) we must ask each other whether this kind of studies are justifiable. Perhaps we should consider alternative study designs and methods that would be more efficient but still aim to develop scientific knowledge in order to provide material for evidence-based therapy. One way to do that could include a use of wheelchair-mounted, multisensory activity monitors (such as IMUs, EMG, or a one-dimensional power measurement wheel) that could be used very early in the rehabilitation setting without putting too much burden on the participants. These devices would be able to measure the amount of various activities such as wheelchair propulsion but also transfers or maneuvering, together with the power output during propulsion. This information would be very valuable in terms of activity monitoring, motor learning and overload prevention. Additionally, working towards time-efficient fixed protocols documenting the progress of wheelchair skill throughout rehabilitation and implementation of those in multiple centers, could allow to build much bigger data sets and form ecologically valid results [Citation43].
The second recommendation relates to the large relative power output difference between the two groups. It is worth adding that if we did not standardize the tire pressure to 6 bar, the difference between the groups would be even more striking as the tires in the group with a recent SCI tended to be less inflated than in the experienced group. This suggests that the state of the wheelchair and it is fitting to the participant should probably receive more attention in early rehabilitation.
Limitations
As mentioned previously, the limitation of this study is the small sample size of the group with a recent SCI. The N could ideally have been higher, especially to improve the statistical power of some of the comparisons by offsetting the heterogeneity of the groups or to possibly allow to distinguish subgroups of participants who exhibit various behaviors during rehabilitation. It was, however, not feasible to include more participants from one rehabilitation center during the duration of the current study and given the time-intensive measurements for both the participants and the research team. Another limitation is the inclusion bias which is often an issue in studies which include vulnerable groups. Our results may not be representative of the whole population with SCI, as it is reasonable to think that considering the effort participants needed to put in this study, only the relatively fit persons volunteered to participate. Lastly, it should be kept in mind that this study was performed in a single rehabilitation center in the Netherlands. It may therefore not be fully representative of other rehabilitation centers in the Netherlands and definitely of those around the world.
Conclusion
Despite improvements in the wheelchair circuit and in work capacity, the group with a recent SCI did not show significant improvements in the primary outcome measures of this study, the mechanical efficiency and propulsion technique. It could be that learning curves for mechanical efficiency and propulsion technique are different than those of the other reported parameters. It may be that the most rapid changes in both parameters took place before the onset of the study. Additionally, our study may have not been long enough to capture further optimization.
The differences between the group with a recent SCI and experienced participants were less pronounced than hypothesized, with the only significant difference found in mechanical efficiency and no significant difference in propulsion technique, work capacity and on the wheelchair circuit scores. Propulsion technique was so similar between the groups that based on our results, there is no ground to think that the findings would be different with a larger sample size. Contrary to that, differences in work capacity and on the wheelchair circuit were not significant, but showed a trend favoring the experienced group. Nevertheless, the lack of significant differences between the groups suggests that the group with a recent SCI was relatively skilled, even already at the onset of the study. This could also explain why they did not significantly improve their propulsion technique and mechanical efficiency between the first measurement and discharge.
Acknowledgement
Firstly, we would like to thank all the participants for their effort in performing the measurements. Secondly, we would like to acknowledge that this study would not be possible without the assistance of many undergraduate students and technical support staff from the Center for Human Movement Sciences. Lastly, we would like to thank the physiotherapists from the UMCG Center for Rehabilitation, for their assistance in identifying several patients eligible for inclusion in the study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Hosseini SM, Oyster ML, Kirby RL, et al. Manual wheelchair skills capacity predicts quality of life and community integration in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93(12):2237–2243.
- Smith EM, Sakakibara BM, Miller WC. A review of factors influencing participation in social and community activities for wheelchair users. Disabil Rehabil Assist Technol. 2016;11(5):361–374.
- Kilkens OJ, Post MW, Dallmeijer AJ, et al. Relationship between manual wheelchair skill performance and participation of persons with spinal cord injuries 1 year after discharge from inpatient rehabilitation. J Rehabil Res Dev. 2004;42(3sup1):65–73.
- van dW, de Groot S, van Drongelen S, et al. Evaluation of manual wheelchair performance in everyday life. Topics Spinal Cord Injury Rehabil. 2009;15(2):1–15.
- de Groot S, de Bruin M, Noomen SP, et al. Mechanical efficiency and propulsion technique after 7 weeks of low-intensity wheelchair training. Clin Biomech (Bristol, Avon). 2008;23(4):434–441.
- Vegter RJ, de Groot S, Lamoth CJ, et al. Initial skill acquisition of handrim wheelchair propulsion: a new perspective. IEEE Trans Neural Syst Rehabil Eng. 2014;22(1):104–113.
- Vegter RJ, Lamoth CJ, de Groot S, et al. Inter-individual differences in the initial 80 minutes of motor learning of handrim wheelchair propulsion. PLoS One. 2014;9(2):e89729.
- de Groot S, Dallmeijer AJ, Kilkens OJ, et al. Course of gross mechanical efficiency in handrim wheelchair propulsion during rehabilitation of people with spinal cord injury: a prospective cohort study. Arch Phys Med Rehabil. 2005;86(7):1452–1460.
- Leving MT, Horemans HLD, Vegter RJK, et al. Validity of consumer-grade activity monitor to identify manual wheelchair propulsion in standardized activities of daily living. PLoS One. 2018;13(4):e0194864.
- Kilkens OJ, Dallmeijer AJ, De Witte LP, et al. The wheelchair circuit: construct validity and responsiveness of a test to assess manual wheelchair mobility in persons with spinal cord injury. Arch Phys Med Rehabil. 2004;85(3):424–431.
- American college of sports medicine position stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30(6):975–991.
- Kirshblum SC, Waring W, Biering-Sorensen F, et al. Reference for the 2011 revision of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2011;34(6):547–554.
- de Groot S, Zuidgeest M, van der Woude LH. Standardization of measuring power output during wheelchair propulsion on a treadmill pitfalls in a multi-center study. Med Eng Phys. 2006;28(6):604–612.
- van der Woude LH, de Groot G, Hollander AP, et al. Wheelchair ergonomics and physiological testing of prototypes. Ergonomics. 1986;29(12):1561–1573. Dec
- Garby L, Astrup A. The relationship between the respiratory quotient and the energy equivalent of oxygen during simultaneous glucose and lipid oxidation and lipogenesis. Acta Physiol Scand. 1987;129(3):443–444.
- Cowan RE, Nash MS, de Groot S, et al. Adapted manual wheelchair circuit: test-retest reliability and discriminative validity in persons with spinal cord injury. Arch Phys Med Rehabil. 2011;92(8):1270–1280.
- van der Scheer JW, de Groot S, Postema K, et al. Design of a randomized-controlled trial on low-intensity aerobic wheelchair exercise for inactive persons with chronic spinal cord injury. Disabil Rehabil. 2013;35(13):1119–1126.
- Dallmeijer AJ, Kilkens OJ, Post MW, et al. Hand-rim wheelchair propulsion capacity during rehabilitation of persons with spinal cord injury. J Rehabil Res Dev. 2004;42(3sup1):55–63.
- Leving MT, Vegter RJ, Hartog J, et al. Effects of visual feedback-induced variability on motor learning of handrim wheelchair propulsion. PLoS ONE. 2015;10(5):e0127311.
- Leving MT, Vegter RJ, de Groot S, et al. Effects of variable practice on the motor learning outcomes in manual wheelchair propulsion. J Neuroeng Rehab. 2016;13(1):100,016–0209-7.
- de Groot S, Dallmeijer AJ, van Asbeck FW, et al. Mechanical efficiency and wheelchair performance during and after spinal cord injury rehabilitation. Int J Sports Med. 2007;28(10):880–886.
- Dallmeijer AJ, van der Woude LH, Hollander AP, et al. Physical performance during rehabilitation in persons with spinal cord injuries. Med Sci Sports Exerc. 1999;31(9):1330–1335.
- Burns AS, Santos A, Cheng CL, et al. Understanding length of stay after spinal cord injury: insights and limitations from the access to care and timing project. J Neurotrauma. 2017;34(20):2910–2916.
- Symonds A, Holloway C, Suzuki T, et al. Identifying key experience-related differences in over-ground manual wheelchair propulsion biomechanics. J Rehabil Assist Technol Eng. 2016;3:205566831667836.
- Rodgers MM, McQuade KJ, Rasch EK, et al. Upper-limb fatigue-related joint power shifts in experienced wheelchair users and nonwheelchair users. J Rehabil Res Dev. 2003;40(1):27–37.
- Chenier F, Champagne A, Desroches G, et al. Unmatched speed perceptions between overground and treadmill manual wheelchair propulsion in long-term manual wheelchair users. Gait Posture. 2018;61:398–402.
- Morgan KA, Tucker SM, Klaesner JW, et al. A motor learning approach to training wheelchair propulsion biomechanics for new manual wheelchair users: a pilot study. J Spinal Cord Med. 2017;40(3):304–315.
- Requejo PS, Mulroy SJ, Ruparel P, et al. Relationship between hand contact angle and shoulder loading during manual wheelchair propulsion by individuals with paraplegia. Top Spinal Cord Inj Rehabil. 2015;21(4):313–324.
- van der Scheer JW, de Groot S, Vegter RJ, et al. Low-intensity wheelchair training in inactive people with long-term spinal cord injury: a randomized controlled trial on propulsion technique. Am J Phys Med Rehabil. 2015;94(11):975–986.
- Lenton JP, Fowler NE, van der Woude L, et al. Wheelchair propulsion: effects of experience and push strategy on efficiency and perceived exertion. Appl Physiol Nutr Metab. 2008;33(5):870–879.
- Curtis KA, Drysdale GA, Lanza RD, et al. Shoulder pain in wheelchair users with tetraplegia and paraplegia. Arch Phys Med Rehabil. 1999;80(4):453–457.
- Gironda RJ, Clark ME, Neugaard B, et al. Upper limb pain in a national sample of veterans with paraplegia. J Spinal Cord Med. 2004;27(2):120–127.
- Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord. 1999;37(3):191–195.
- Nichols PJ, Norman PA, Ennis JR. Wheelchair user's shoulder? Shoulder pain in patients with spinal cord lesions. Scand J Rehabil Med. 1979;11(1):29–32.
- Eriks-Hoogland IE, Hoekstra T, de Groot S, et al. Trajectories of musculoskeletal shoulder pain after spinal cord injury: identification and predictors. J Spinal Cord Med. 2014;37(3):288–298.
- van den Berg-Emons RJ, Bussmann JB, Haisma JA, et al. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil. 2008;89(11):2094–2101.
- Postma K, van den Berg-Emons HJ, Bussmann JB, et al. Validity of the detection of wheelchair propulsion as measured with an activity monitor in patients with spinal cord injury. Spinal Cord. 2005;43(9):550–557.
- Fliess-Douer O, Vanlandewijck YC, Post MW, et al. Wheelchair skills performance between discharge and one year after inpatient rehabilitation in hand-rim wheelchair users with spinal cord injury. J Rehabil Med. 2013;45(6):553–559.
- Eerden S, Dekker R, Hettinga FJ. Maximal and submaximal aerobic tests for wheelchair-dependent persons with spinal cord injury: a systematic review to summarize and identify useful applications for clinical rehabilitation. Disabil Rehabil. 2018;40(5):497–521.
- Scheer J, Groot S, Tepper M, et al. Low-intensity wheelchair training in inactive people with long-term spinal cord injury: a randomized controlled trial on fitness, wheelchair skill performance and physical activity levels. J Rehabil Med. 2016;48(1):33–42.
- van Velzen JM, de Groot S, Post MW, et al. Return to work after spinal cord injury: is it related to wheelchair capacity at discharge from clinical rehabilitation? Am J Phys Med Rehabil. 2009;88(1):47–56.
- van Koppenhagen CF, Post M, de Groot S, et al. Longitudinal relationship between wheelchair exercise capacity and life satisfaction in patients with spinal cord injury: a cohort study in the netherlands. J Spinal Cord Med. 2014;37(3):328–337.
- de Groot S, Vegter R, Vuijk C, et al. WHEEL-I: development of a wheelchair propulsion laboratory for rehabilitation. J Rehabil Med. 2014;46(6):493–503.
