Abstract
Purpose
Existing physical activity interventions do not reach a considerable proportion of physically disabled people. This study assessed feasibility and short-term effects of Activity Coach+, a community-based intervention especially targeting this hard-to-reach population.
Methods
Feasibility was determined by reach, dropouts, and compliance with the protocol. Physical activity was measured with the Activ8 accelerometer and the adapted SQUASH questionnaire. Health outcomes were assessed by body composition, blood pressure, hand grip force, 10-metre walk test, 6-minute walk test, and the Berg Balance Scale. The RAND-36, Exercise Self-Efficacy Scale, Fatigue Severity Scale, and IMPACT-S were administered. Measurements were performed at baseline and after 2 and 4 months. Changes over time were analysed by Friedman tests.
Results
Twenty-nine participants enrolled during the first 4 months, of whom two dropped out. Intervention components were employed in 86–100% of the participants. Physical activity did not change after the implementation of Activity Coach+. Body mass index (p = 0.006), diastolic blood pressure (p = 0.032), walking ability (p = 0.002), exercise capacity (p = 0.013), balance (p = 0.014), and vitality (p = 0.049) changed over time.
Conclusions
Activity Coach + is feasible in a community setting. Indications for effectivity of Activity Coach + in hard-to-reach people with a physical disability were found.
Activity Coach + was able to reach physically disabled people living in community, a population that is assumed hard-to-reach.
Activity Coach + was feasible in a population of persons with a physical disability that was heterogeneous with respect to age and (severity of) disability.
The current study provides the first indications for the beneficial health effects of Activity Coach + in hard-to-reach people with a physical disability.
Implications for rehabilitation
Introduction
Physical inactivity has a negative impact on health and is the fourth leading cause of death worldwide [1,Citation2]. The lack of physical activity (PA), defined as any bodily movement produced by skeletal muscles that requires energy expenditure [Citation3], was recently called pandemic in the Lancet [Citation1,Citation2,Citation4]. Being physically active benefits health and functioning, not only in able-bodied people [Citation5], but also in people with a physical disability [Citation6,Citation7]. In people with a physical disability the amount of PA is positively related to bio psychosocial aspects of health-related quality of life [Citation8]. However, people with a physical disability are substantially less physically active than able-bodied people [Citation7,Citation9].
Most existing PA-stimulating interventions designed for people with a physical disability reach their participants via intermediate organisations, such as rehabilitation centres or schools for special education [Citation10]. However, a major part of the physically disabled population cannot be reached through these intermediary organisations, which makes this part of the population hard-to-reach. Several interventions have been found effective and were implemented for improving participation in PA in people with a physical disability [Citation11]. But the limited reach of these effective interventions might explain why PA has not increased in the period of 2001–2011 over the whole population of people with physical disabilities [Citation10,Citation12].
International research on stimulating PA in physically disabled people is experiencing a shift from describing barriers and facilitators regarding PA towards designing interventions that stimulate PA [Citation13]. Although more than 80 exercise interventions aimed at stimulating PA in physically disabled people exist internationally, most interventions are disease-specific and time-restricted. They stimulate participants to perform a specific type of exercise, rather than to participate in PA in general or to adopt an active lifestyle [Citation14–16]. However, to establish long-term behavioural changes in physically disabled people, PA interventions aimed at altering one’s lifestyle are preferred over exercise interventions [Citation16]. The literature describes the need for the design and evaluation of community-based interventions that serve broader populations and stimulate the adoption of an active lifestyle and participation in PA. Notwithstanding the fact that people with different disabilities experience unique barriers, the added value of interventions with a broader scope is that more people with a physical disability in a community can be reached [Citation12,Citation16].
In our previous study, the Intervention Mapping protocol was used for the systematic development of a new intervention that stimulates PA in hard-to-reach people with a physical disability and that can be applied in a community setting [Citation17]. Intervention Mapping is a widely used, systematic six-step method, for developing health promotion interventions based on behavioural change theories [Citation18]. Based on the health problem and context, a set of behavioural change theories can be selected, as for instance, the Theory of Planned Behaviour and the Social Cognitive Theory [Citation19,Citation20]. Intervention Mapping enables both professionals and people with a physical disability to be actively involved in the development of the intervention, ensuring co-creation. Involving these stakeholders results in an intervention that fits the demands of end-users, and has more potential to structurally implement it into existing health systems [Citation21]. Intervention development resulted in the adaptation of an existing Dutch intervention “Activity Coach” (Dutch: Beweegcoach) into the new intervention “Activity Coach+” (Dutch: Beweegcoach+) [Citation17,Citation22]. The current study aims to assess the feasibility and short-term effects of Activity Coach + in hard-to-reach people with a physical disability by determining its effects on PA behaviour and bio psychosocial health outcomes.
Materials and methods
Study design
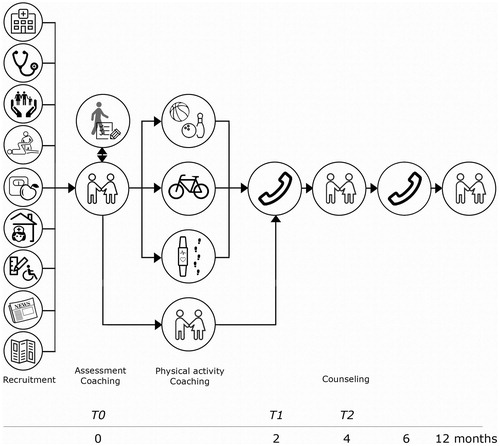
Activity Coach + was pilot tested in three municipalities (Oldambt, Bellingwedde and Vlagtwedde, located in the Province of Groningen, The Netherlands). Feasibility of Activity Coach + was determined by number of participants, recruitment method, number of dropouts, and compliance with the protocol. This study is part of a larger longitudinal study on effectiveness of Activity Coach + until one year after the start of the intervention. The first three measurement points were included in the current study to assess the short-term effects of Activity Coach + on PA behaviour and health outcomes. Measurements were performed at baseline (during the physiotherapeutic intake, which was taken as the starting point of the intervention; T0), after 2 months (T1), and after 4 months (T2) (). Measurements after 2 and 4 months took place at the participants’ homes. According to protocol, no more than 2 weeks’ time was allowed between the actual measurement and the scheduled date according to protocol. A control group was not used since matching a control group (on e.g., age, gender, diagnosis, motivation, and living situation) would be infeasible.
Figure 1. Schematic overview of Activity Coach + including the recruitment of potential participants by different intermediate organisations from health or welfare, a physical assessment by a local physiotherapist, and multiple individual coaching and counselling sessions by a physical activity coach.
Intervention
Activity Coach + aimed to stimulate organised PA (e.g., weekly aqua gym classes), non-organised PA (e.g., going out for a walk with the neighbour), and PA during activities of daily living (e.g., walking to the supermarket instead of going by car). The intervention stimulates all levels of intensity of PA (light, moderate, and vigorous activity). Key behavioural change strategies of the intervention are individual coaching on goal setting and developing action plans, and providing feedback on daily PA behaviour [Citation17].
Participants were recruited via a network of various intermediary organisations from social, medical, and sports backgrounds. In addition, flyers and local newspapers were used for recruiting participants () [Citation17]. Participants first had an intake with a local physiotherapist. The intake included history taking and a physical assessment. In the interviews during the intervention development process, potential participants indicated that a physical assessment including an advice on the safety of PA participation by a health care professional would improve their confidence in PA participation [Citation23]. Moreover, the intake aimed to give the activity coach an idea about the type of activities that are safe to perform and would suit the participant. Physiotherapists provided these recommendations for types of activities based on their own professional training and experience. A standardised form including the Physical Activity Readiness Questionnaire for measuring safety of PA participation was used for this physiotherapeutic intake [Citation24]. Second, barriers regarding PA participation were discussed in a consultation between the participant and the activity coach, using the principles of motivational interviewing.
The activity coach guided the participant towards more active participation in PA in three ways: (1) by informing about local opportunities for organised PA, (2) by matching participants with similar interests to enable participation in non-organised PA, and (3) by distributing a Fitbit Zip activity tracker (Fitbit, San Francisco, CA) for stimulating PA during activities of daily living. The process of coaching was a longer process, in which activities could change over time. In some cases, people were matched after a few months, when another participant with similar interests enrolled. Participants received further counselling from the activity coach after 2 (phone call), 4 (face-to-face contact), 6 (phone call), and 12 months (face-to-face contact), respectively (). During coaching sessions, the following topics were discussed: type of PA, experiences with (non-)organised PA and PA during daily living, setting and adjusting goals, effects of being more physically active, social support of family and friends, and experiences with coaching of the activity coach. In the last coaching session after 12 months, also the topic of PA continuation was discussed. Activity coaches received report forms for each coaching session [Citation17]. Activity coaches were instructed that they may provide additional contacts, in case it was needed for a good coaching process, but to restrict these additional contacts as much as possible, to limit burden on the coaches. Fidelity of the intervention protocol was ensured by providing an instruction manual and regular contact between the researcher and the physiotherapists and activity coaches.
Activity coaches
For this pilot, two different activity coaches were appointed for the three municipalities involved. Activity coaches were professionals with a background in welfare or sports, who worked in the municipality, and had received training in Motivational Interviewing and basic information on the most prevalent physical disabilities. Activity coaches had no previous relationship with the participants.
Participants
Activity Coach + was designed for adults with a physical disability due to a physical impairment (e.g., brain injury, orthopaedic conditions) or a chronic disease that impairs mobility (e.g., cardiopulmonary disease, chronic pain, diabetes). Participants were included if they were 18 years or older, able to visit a primary healthcare physiotherapist, and were at least one year post-rehabilitation or not familiar with rehabilitation in order to prevent overlap with an existing intervention during and directly after inpatient rehabilitation [Citation25]. Participants of Activity Coach + were asked to voluntarily participate in research by the activity coach during the first contact by phone. Participants gave their written informed consent for participation in this study after being informed that the data would be processed anonymously.
Data collection
Activity coaches were asked to report the recruitment method of their participants and their contact moments with each participant. The coaches reported whether the physiotherapeutic assessment, face-to-face intake with the activity coach, and phone-based counselling sessions at 2 and 4 months took place; whether the activity tracker was used; and whether any additional contacts took place. At each measuring point, three types of measurements were performed: an objective measurement of PA, a physical assessment, and the administering of questionnaires. Procedures for all types of measurements have been described in detail in a previous study [Citation17]. All measurements were performed by the first author.
Objective measurement of PA
PA during activities of daily living was objectively measured using the Activ8, a tri-axis accelerometer (2M Engineering, Valkenswaard, The Netherlands) [Citation26]. The Activ8 was attached to the ventral side of the thigh (at 10 cm from proximal, in the middle in the frontal plane). Activ8 determines the time spent lying/sitting, standing, walking, running, and cycling based on the orientation (horizontal or vertical) and movement intensity (vector magnitude, expressed in counts) of the thigh. Activity classification was performed at a frequency of 2.56 Hz and output was summed and stored over a 15 s interval (Epoch length).
The Activ8 was worn for seven consecutive days, except when the participants went swimming or bathing. Participants recorded their bed and wake-up times in a measurement diary. The Activ8 output files and digitalised diaries were analysed using Matlab (R2016b, The Mathworks Inc., Natick, MA). Wear time per day was defined as minutes that the device was worn and was retrieved from the diary. Time per activity per day was calculated as absolute time (minutes) and as percentage time (absolute time divided by total wear time × 100%). Daily PA was expressed as percentage of time spent active, intensity of behaviour (counts/min), average number of active bouts, and mean duration of active bouts [Citation26].
Percentage of time spent active was calculated by summing the percentages of time spent walking, running, and cycling. Intensity of behaviour was expressed in counts/min and calculated as the sum of counts divided by total wear time (min). One-minute intervals (sum of four 15 s intervals) were identified as either active (≥80% of time spent on walking, running, or cycling), sedentary (≥90% of time spent on sitting or lying), or neutral (time intervals that were neither active nor sedentary). Active bouts were defined as a sequence of consecutive active time intervals, including neutral intervals of maximum 1 min, provided that at least 70% of the total bout duration consisted of walking, running, or cycling. For each participant, outcomes were averaged over the number of analysed days.
Physical assessment
Body mass index (BMI) and waist circumference were measured as indicators of body composition. Blood pressure was measured using an Omron M3 automatic blood pressure system (Omron Healthcare, Kyoto, Japan). Hand grip force was measured using a dynamometer and E-link software (Biometrics Ltd, Gwent, UK). Contrary to what we described in our previous study [Citation17], hand grip force is reported as the maximum score of the dominant hand to enable comparison with values for clinical relevance found in earlier research [Citation27]. Walking speed was measured using the 10-metre walk test, and walking capacity was measured using the 6-min walk test [Citation28–30]. The 6-min walk test is recommended to estimate functional exercise capacity in cardiac patients [Citation30]. Walking aids were used when needed during both walking tests. Static and dynamic balance were measured using the Berg Balance Scale [Citation31].
Questionnaires
Participants completed a set of questionnaires in the same week as the physical assessment. Health-Related Quality of Life was measured using the RAND-36 [Citation32]. Fatigue was measured using the Fatigue Severity Scale [Citation33]. Self-efficacy regarding PA was measured using the Exercise Self-Efficacy Scale (ESES) [Citation34]. Social participation was measured using the ICF Measure of Participation and ACTivities Screener (IMPACT-S) [Citation35]. Daily PA and sedentary behaviour were measured using the Short Questionnaire to Assess Health-enhancing physical activity (SQUASH) adapted for wheelchair use [Citation36,Citation37]. Previous research has found the above-mentioned tests and questionnaires to be reliable and valid for specific sub-populations of the physically disabled population (Supplementary File 1) [Citation29,Citation30,Citation34–36,Citation38–40].
Data analyses
Data of objective PA monitoring were only used for analyses if the accelerometer had been worn for at least 11 h a day, for at least four out of seven days [Citation41]. Longitudinal progression of the outcome parameters over time was analysed using non-parametric Friedman’s tests. Pairwise comparison using Dunn’s tests with Bonferroni’s correction was performed on the results of the Friedman tests for outcome parameters with significant progression over time (SPSS 20.1, IBM, Armonk, NY). Effect sizes for post hoc testing were calculated as z-value/√total number of observations. Effect sizes of >0.20 were interpreted as small, >0.50 as medium, and >0.80 as large [Citation42]. The selected statistical analyses are an alteration to the initial plan of analysis, but were induced by non-normality of the outcome data [Citation17]. For all tests of significance, α was set at 5%. The Medical Ethical Committee of the University Medical Center Groningen, the Netherlands, confirmed that ethical approval was not required for this study (METc 2016/630). This study was registered in the Dutch Trial Registry (NTR6858).
Results
Within the first 4 months after implementation of Activity Coach+ (30 March 2017), 29 persons with a physical disability were interested in the intervention and had a physiotherapeutic intake, after which all 29 persons were enrolled in the intervention programme. Twenty-three of these 29 participants participated in this study (six participants declined to participate in research). Two out of 23 participants dropped out within 4 months because of severe progression of arthritis and psychosocial problems, respectively. Characteristics of the 21 included participants, who suffered from various physical disabilities, are presented in . Participants were recruited through local newspapers (n= 5), general practitioners (n= 6), domestic care (n= 6), physiotherapists (n= 2), and social work (n= 2).
Table 1. Characteristics of the participants (n= 21).
All 21 participants underwent a physiotherapeutic assessment and had a face-to-face intake with one of the two activity coaches. Twenty participants received a counselling session at 2 months; six sessions took place by phone, and 14 sessions were face-to-face which was a deviation from the protocol. The counselling session at 2 months of one participant was rescheduled to approximately 3 months. This session was seen as an additional contact, and the counselling session at 2 months was recorded as missing. Nineteen participants received a counselling session at 4 months. Eight of these sessions took place by phone (deviation from the protocol), and 11 were face-to-face. One participant did not participate in the counselling session at 4 months because of personal reasons, and another participant was not able to attend the session but received counselling by means of a text message (deviation from the protocol). Eighteen participants used the activity tracker, whereas three did not. One of these three participants preferred to use her own activity tracker, and the other two felt that use of the activity tracker did not contribute to their behavioural change. Fifteen participants had additional contacts with the coach (1–7 contacts including phone calls). Multiple deviations from the protocol (e.g., face-to-face contacts instead of phone, or additional contacts) took place. According to the activity coaches, these deviations were caused by participants requiring more intensive coaching, and practical reasons (working in area of participants homes).
On average, 13.2% of all measurements were missing. Reasons for missing measurements included participants’ inability to complete the questionnaires due to cognitive decline (2.2%); participants’ physical status (0.8%); holidays (1.6%); incorrect measurements (1.8%); weather conditions (measurements took place at home, whereas walk tests took place outside and could not be performed during heavy rainfall) (0.2%); participants’ inability to wear the Activ8 accelerometer during one week (1.5%); and unknown reasons (5.1%). Participants with complete data did not differ from participants with missing data on gender (Fisher’s exact test: p = 0.133), age (t = 0.751, df = 19; p = 0.462) and diagnosis (Fisher’s exact test: p = 0.857). Given that too many diaries were incomplete, outcomes of objective measurement of PA were reported per 24 h (for which diaries were not needed), instead of per waking time. After excluding periods of non-wear time (as indicated in the diaries, for instance because of swimming/bathing), on average, 1425 min (23 h and 45 min) were analysed per day. Measurements included 6.8 days on average. All measurements fulfilled the criteria of 11 h wear time of the accelerometer per day for at least four days per week and were included for analyses.
PA behaviour did not change significantly over time (). BMI, walking ability, exercise capacity, and balance, were found to significantly increase over time. Diastolic blood pressure significantly decreased over time. No differences over time were found for waist circumference, systolic blood pressure, and hand grip force (). Vitality, a subscale the RAND-36, also significantly increased over time. The other psychosocial constructs measured by the included questionnaires did not change significantly over time (). Results of the post hoc procedures for outcomes showing significant change over time are presented in . shows four illustrative examples of progression of the outcomes over time, presenting large heterogeneity in results between different participants.
Figure 2. Four illustrative examples of progression of the outcomes over time, presenting large heterogeneity in results between different participants.
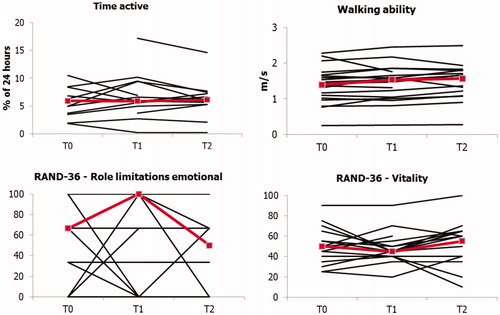
Table 2. Overview of test statistics.
Table 3. Results of post hoc testing.
Discussion
The aim of the current study was to assess feasibility and short-term effects of the Activity Coach + intervention programme with regards to PA behaviour and biopsychosocial aspects of health in hard-to-reach people with a physical disability. Within the first 4 months, 29 people with a physical disability were enrolled in Activity Coach+, of which 23 chose to participate in this study. Activity Coach + was able to reach a hard-to-reach physically disabled population. Fifteen of 21 participants were reached through local media or unconventional intermediary organisations (all intermediary organisations in the network except for general practitioners). The study population is suggested to be representative for the target population: people with a physical disability living in a community, in which prevalent diagnoses are brain injuries, orthopaedic injuries, chronic pain, neuromuscular diseases, diabetes, and cardiopulmonary diseases [Citation43]. The programme’s ability to meet the demands of individual participants was witnessed by the fact that different intervention components were applied in 18 (86%) to 21 (100%) of the participants.
More than half of the coaching sessions after 2 and 4 months were face-to-face, rather than by phone, which was not in line with the intervention design. These individual deviations may partly explain the low dropout (n= 2), by better matching the programme to individual preferences. But these deviations from the original protocol, prevented us from determining feasibility of the original protocol. Practical reasons made the coaches deviate from the protocol. It was easy for them to visit participants since they worked in the vicinity of the participants’ homes. Practical reasons for deviating from the protocol (e.g., mode of contacts, and additional contacts) should be taken into account during future intervention planning, as this might induce issues with balancing time investment and intervention effects.
No significant change in PA behaviour was found over time after implementation of Activity Coach+, neither when objectively measured using the Activ8 accelerometer, nor when assessed using the adapted SQUASH questionnaire (). Although not significant, trends were observed for the increase of daily number and duration of active bouts. Earlier research has shown that individually tailored interventions that include motivational interviewing and self-monitoring of behaviour using activity trackers or pedometers, such as Activity Coach+, are more likely to be effective in improving PA behaviour [Citation44–46].
Significant changes in BMI, diastolic blood pressure, walking ability (10-metre walk test), exercise capacity (6-min walk test), balance (Berg Balance Scale), and vitality (one of the items of the RAND-36) were found over time after implementation of Activity Coach+. An unexpected increase in BMI was found from baseline to 4 months after the start of Activity Coach+. Lower BMI indicates better health in this population, which already has a BMI that is too high on average. Trends in the data suggest that the increased BMI might be caused by seasonal influences or by an increase in muscle mass as a result of the intervention [Citation47]. All participants started the intervention between March and August, which means that measurements after 4 months took place between July and January. Future research will study long-term effects of the intervention, allowing for further exploration of seasonal influences. A small to medium decrease of diastolic blood pressure of 5 mmHg was observed (ES=–0.48). Median value for walking ability increased by 0.17 m/s between the start of the intervention and after 4 months, representing a medium effect size (ES = 0.63). An increase of 0.10 (older adults with various physical limitations) to 0.17 m/s (patients after hip fracture) in walking ability was found to be clinically relevant [Citation48,Citation49]. This means that the increase in walking ability found in our study may be a clinically relevant increase. Exercise capacity improved with medium effect size between the start of the intervention and after 2 months (ES = 0.55), and the start of the intervention and after 4 months (ES = 0.55). Median outcome of the 6-min walk test improved by 46 metres, whereas minimum clinically important differences ranged from 23.5 m in chronic obstructive pulmonary disease patients to 82 m in fibromyalgia patients [Citation50,Citation51]. It can be debated whether the increase found in this study is clinically relevant or not, since no values for minimum clinically important differences were available for our heterogeneous target population. Also, values for different diagnoses vary with regard to the differences found in the current study. Median value for balance increased by three points between the start of the intervention and after 4 months, being an increase with a low effect size. Minimum clinically important difference ranged from two points in outpatients with multiple sclerosis [Citation52] to 5.8 points in stroke patients [Citation38]. This means that it is unclear whether the significant increase in balance is clinically relevant. Median value for vitality increased by five points between the start of the intervention and after 4 months. Values for minimum clinically important difference of the SF-36 (almost identical to the RAND-36) were only found for people with a chronic cardiopulmonary disease. For the SF-36 vitality scale minimum clinically important difference was set at 12.5 points, meaning that the increase in vitality in our study was not clinically relevant [Citation53]. Although not significant, a trend was seen within the first 4 months for the increase in hand grip force, which increased by 4.3 kg between the start of the intervention and 4 months later. No values for minimum clinically important difference were found for diagnosis groups included in this study. An increase of 3.4 kg was found relevant in chronic kidney disease patients [Citation27], and an increase of 6.5 kg was found relevant in patients after radius fractures [Citation54]. Compared with these reference values, it is unclear whether the increase found in our study is clinically relevant. The values for minimum clinically relevant differences are based on specific sub-populations of the population of Activity Coach + and are relatively high compared with the baseline level of health outcomes. In this relatively inactive target population, smaller changes may be relevant at an individual level.
The finding that participants’ PA did not improve, whereas functional outcomes did, may be caused by the curvilinear relationship between the amount of PA and health. In inactive people, a small increase in PA can already lead to substantial health benefits [Citation5]. Moreover, PA was only measured as total PA. Several participants began to take part in activities that were mainly focused on improving balance and muscle strength, for example, exercise groups for the elderly. The finding that total PA did not change despite the participation in new activities might be caused by a decrease in transportation-related PA or household-related PA. Moreover, this study may be underpowered to find a significant improvement in PA, due to the relatively small sample size and the heterogeneity of participants’ baseline PA.
In practice, it is an advantage when community-based interventions can be used in broad populations, considering the relatively low number of people diagnosed with a specific disability or disease in a community. For research purposes, however, a heterogeneous target population has its downside in that it influences the choice of outcome measures. In the current study, the Berg Balance Scale was used because of its discriminative power with regards to people with impaired balance. However, not all participants experienced impaired balance, resulting in ceiling effects. Considering the heterogeneous group of participants, reliability and validity could not be tested for all of the included diagnoses. Therefore, outcome measures were chosen that are reliable and valid for most of the included diagnoses.
The current study design was limited by the lack of a control group. Due to the heterogeneity of the group of participants, several of whom had multiple diagnoses, it was practically infeasible to include a control group that could be matched on diagnoses and age. Practical reasons (lack of time, burden on the participants) also not did allow for a study design that included multiple baseline measures, such as an interrupted time series design, for example. These limitations make it theoretically impossible to attribute changes over time solely to the implementation of the intervention. Median value of the health change outcome (subscale of the RAND-36), however, showed that participants’ perception of health status improved by 25 points after implementation of Activity Coach + compared with the year before. At baseline, the majority of participants rated their health status as somewhat worse or equal to 1 year ago. Four months after the implementation, participants rated their health status as equal or somewhat better than 1 year ago. Although changes experienced in health status are subjective, this improvement is nevertheless important because the Health Change subscale of the RAND-36 is the only measure included that enables comparisons over a longer timeframe before the start of the intervention. Activity Coach + was implemented in a region with a relatively low socioeconomic status [Citation55]. People with lower socioeconomic status are at a higher risk of being physically inactive and of developing chronic diseases, such as diabetes [Citation56,Citation57]. Future research should investigate the generalisability of the results of this study to regions with a higher socioeconomic status.
Monitoring of daily PA behaviour by means of accelerometers was one of the strengths of the current study. This is in line with the research agenda for PA stimulation, which describes a need for objective PA monitoring in physically disabled people [Citation15,Citation16]. Despite the fact that accelerometers might miss important types of PA, such as upper body movements, and the fact that algorithms may not be validated for all diagnoses in a diverse clinical population, PA monitoring using accelerometers is preferred in addition to questionnaires [Citation15]. Moreover, the current study investigated the intervention’s effects on biopsychosocial health outcomes, which is in concordance with the current multidimensional view on health [Citation58]. Finally, the heterogeneity of the study population was one of the strengths of this study; it demonstrated that Activity Coach + was feasible in a heterogeneous group.
Based on the results of this study, the recruitment of people with a physical disability in a community through a network of intermediate organisations and local media is suggested for the development of future interventions. This approach is also recommended by the literature [Citation12]. Targeting people with various physical disabilities and tailoring the coaching to meet the needs of each individual participant was feasible and is suggested for future intervention development. It can be debated whether phone counselling instead of face-to-face counselling should be recommended for future intervention development, given the deviations from the protocol in this study and keeping in mind the lower costs of phone counselling compared with face-to-face counselling.
Future research should focus on the effectiveness of Activity Coach + over a longer period of time in order to determine sustainability of the health effects found in this study. Moreover, experiences with the implementation process of Activity Coach + should be investigated in order to further improve the intervention and enable daily use in a community setting. Based on this feasibility study, no changes to improve the intervention itself are suggested.
In conclusion, the implementation of Activity Coach + in a community setting was feasible. Activity Coach + was able to reach hard-to-reach people with a physical disability, had a very low drop-out rate, and demonstrated high compliance rates with the protocol. The amount of daily PA did not change during the first 4 months after implementation of Activity Coach+. BMI, walking ability, exercise capacity, balance, and vitality increased, whereas diastolic blood pressure decreased during the first 4 months after implementation. The increase in walking ability, balance and hand grip force was clinically relevant; however, clinical relevance of the increase in exercise capacity was questionable. The current study provides the first indications for the beneficial effects on health of Activity Coach + in hard-to-reach people with a physical disability. Future research should address long-term results of Activity Coach+.
Krops2019_FirstResultsActivityCoach_SupplementaryFile.docx
Download MS Word (24.1 KB)Disclosure statement
The authors report no conflicts of interest.
Data availability
Data are available on request, after contacting the first author.
Additional information
Funding
References
- Kohl HW, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380(9838):294–305.
- Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229.
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131.
- Andersen LB, Mota J, Di Pietro L. Update on the global pandemic of physical inactivity. Lancet. 2016;388(10051):1255–1256.
- Warburton DE, Bredin SS. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–556.
- Heath GW, Fentem PH. Physical activity among persons with disabilities—a public health perspective. Exerc Sport Sci Rev. 1997;25:195–234.
- Carroll DD, Courtney-Long EA, Stevens AC, et al. Vital signs: disability and physical activity – United States, 2009–2012. MMWR Morb Mortal Wkly Rep. 2014;63(18):407–413.
- Krops LA, Jaarsma EA, Dijkstra PU, et al. Health related quality of life in a Dutch Rehabilitation Population: reference values and the effect of physical activity. PLoS One. 2017;12(1):e0169169.
- Van Den Berg-Emons RJ, Bussmann JB, Stam HJ. Accelerometry-based activity spectrum in persons with chronic physical conditions. Arch Phys Med Rehabil. 2010;91(12):1856–1861.
- von Heijden A, van den Dool R, van Lindert C, et al. Monitor sport- en beweegdeelname van mensen met een handicap [(Un)limited exercise 2013. Monitoring sport- and exercise participation in handicapped people]. Utrecht (The Netherlands): Mulier Instituut/Arko Sports Media; 2013.
- Ma JK, Martin Ginis KA. A meta-analysis of physical activity interventions in people with physical disabilities: content, characteristics, and effects on behaviour. Psychol Sport Exerc. 2018;34:262–273.
- Mendoza-Vasconez AS, Linke S, Munoz M, et al. Promoting physical activity among underserved populations. Curr Sports Med Rep. 2016;15(4):290–297.
- Martin Ginis KA, Ma JK, Latimer-Cheung AE, et al. Systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol Rev. 2016;7199:1–31.
- Rimmer JH, Chen MD, McCubbin JA, et al. Exercise intervention research on persons with disabilities: what we know and where we need to go. Am J Phys Med Rehabil. 2010;89(3):249–263.
- Cervantes CM, Taylor WC. Physical activity interventions in adult populations with disabilities: a review. Quest. 2011;63(4):385–410.
- Rosenberg DE, Bombardier CH, Hoffman JM, et al. Physical activity among persons aging with mobility disabilities: shaping a research agenda. J Aging Res. 2011;2011:1–16.
- Krops LA, Dekker R, Geertzen JHB, et al. Development of an intervention to stimulate physical activity in hard-to-reach physically disabled people and design of a pilot-implementation: an Intervention Mapping approach. BMJ Open. 2018;8(3):e020934.
- Bartholomew LK, Parcel GS, Kok G, et al. Planning health promotion programs; an intervention mapping approach. San Francisco: Jossey-Bass; 2011.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
- Bandura A. Social foundations of thought and action: a social cognitive theory. New Jersey: Prentice Hall; 1986.
- Jull J, Giles A, Graham ID. Community-based participatory research and integrated knowledge translation: advancing the co-creation of knowledge. Implement Sci. 2017;12(1):150.
- Kenniscentrum Sport. Netwerk in Beweging [Knowledge Center Sports. Network in movement]; 2017 [cited 2017 Jul 7]. Available from: https://www.netwerkinbeweging.nl/interventies/overzicht/22530?mode=Mode-all&trefwoorden=beweegcoach&leeftijdscategorie=&beoordeling=&thema=&doelgroep=&setting=&sport=. Dutch
- Krops LA, Folkertsma N, Hols DH, et al. Target population’s requirements on a community-based intervention for stimulating physical activity in hard-to-reach physically disabled people: an interview study. Disabil Rehabil. 2019;41:2272–2279.
- Goodman JM, Thomas SG, Burr J. Evidence-based risk assessment and recommendations for exercise testing and physical activity clearance in apparently healthy individuals. Appl Physiol Nutr Metab. 2011;36:S12–S32.
- Hoekstra F, Hettinga FJ, Alingh RA, et al. The current implementation status of the integration of sports and physical activity into Dutch rehabilitation care. Disabil Rehabil. 2017;39(2):181–186.
- Fanchamps MHJ, Horemans HLD, Ribbers GM, et al. The accuracy of the detection of body postures and movements using a physical activity monitor in people after a stroke. Sensors (Switzerland). 2018;18(7):2167.
- Segura-Ortí E, Martínez-Olmos FJ. Test–retest reliability and minimal detectable change scores for sit-to-stand-to-sit tests, the six-minute walk test, the one-leg heel-rise test, and handgrip strength in people undergoing hemodialysis. Phys Ther. 2011;91(8):1244–1252.
- Collen F, Wade D, Bradshaw C. Mobility after stroke: reliability of measures of impairment and disability. Disabil Rehabil. 1990;12:6–9.
- Tyson S, Connell L. The psychometric properties and clinical utility of measures of walking and mobility in neurological conditions: a systematic review. Clin Rehabil. 2009;23(11):1018–1033.
- Bellet RN, Adams L, Morris NR. The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness—a systematic review. Physiother (United Kingdom). 2012;98:277–287.
- Berg K, Wood-Dauphinee S, Williams JI, et al. Measuring balance in the elderly: preliminary development of an instrument. Physiother Canada. 1989;41(6):304–311.
- Van der Zee KI, Sanderman R. Het meten van de algemene gezondheidstoestand met de RAND-36. een handleiding [Measuring general health status with the RAND-36. Users manual]. 2nd ed. Groningen (The Netherlands): Research Institute SHARE; 2012. Available from: https://www.umcg.nl/SiteCollectionDocuments/research/institutes/SHARE/assessment tools/handleiding_rand36_2e_druk.pdf. Dutch
- Elbers RG, Rietberg MB, Van Wegen EEH, et al. Self-report fatigue questionnaires in multiple sclerosis, Parkinson’s disease and stroke: a systematic review of measurement properties. Qual Life Res. 2012;21(6):925–944.
- Nooijen CFJ, Post MWM, Spijkerman DCM, et al. Exercise self-efficacy in persons with spinal cord injury: psychometric properties of the Dutch translation of the Exercise Self-Efficacy Scale. J Rehabil Med. 2013;45(4):347–350.
- Post MWM, de Witte LP, Reichrath E, et al. Development and validation of impact-s, an ICF-based questionnaire to measure activities and participation. J Rehabil Med. 2008;40(8):620–627.
- Alingh RA, Hoekstra F, van der Schans CP, et al. Protocol of a longitudinal cohort study on phyiscal activity behaviour in physically disabled patients participating in a rehabilitation counselling programme: ReSpAct. BMJ Open. 2015;5(1):e007591.
- Wendel-Vos GCW, Schuit AJ, Saris WHM, et al. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol. 2003;56(12):1163–1169.
- Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008;88(5):559–566.
- Krops LA, Wolthuizen L, Dijkstra PU, et al. Reliability of translation of the RAND 36-item health survey in a post-rehabilitation population. Int J Rehabil Res. 2018;41(2):128–137.
- Rosti-Otajärvi E, Hämäläinen P, Wiksten A, et al. Validity and reliability of the Fatigue Severity Scale in Finnish multiple sclerosis patients. Brain Behav. 2017;7(7):e00743.
- Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47:1821–1845.
- Cohen J. Statistical power for the social sciences. Hillsdale (NJ): Laurence Erlbaum Assoc.; 1988.
- James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858.
- Greaves CJ, Sheppard KE, Abraham C, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11(1):119.
- Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Heal Psychol. 2009;28(6):690–701.
- Avery L, Flynn D, Van Wersch A, et al. Changing physical activity behavior in type 2 diabetes: a systematic review and meta-analysis of behavioral interventions. Diabetes Care. 2012;35(12):2681–2689.
- Visscher TLS, Seidell JC. Time trends (1993–1997) and seasonal variation in body mass index and waist circumference in the Netherlands. Int J Obes. 2004;28(10):1309–1316.
- Latham NK, Mehta V, Nguyen AM, et al. Performance-based or self-report measures of physical function: which should be used in clinical trials of hip fracture patients? Arch Phys Med Rehabil. 2008;89(11):2146–2155.
- Perera S, Mody SH, Woodman RC, et al. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749.
- Holland AE, Hill CJ, Rasekaba T, et al. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(2):221–225.
- Steffen T, Seney M. Test–retest reliability and minimal detectable change on balance and ambulation tests, the 36-item short-form health survey, and the unified Parkinson disease rating scale in people with parkinsonism. Phys Ther. 2008;88(6):733–746.
- Gervasoni E, Jonsdottir J, Montesano A, et al. Minimal clinically important difference of berg balance scale in people with multiple sclerosis. Arch Phys Med Rehabil. 2017;98(2):337–340.e2.
- Wyrwich KW, Tierney WM, Babu AN, et al. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Heal Serv Res. 2005;40(2):577–591.
- Kim JK, Park MG, Shin SJ. What is the minimum clinically important difference in grip strength? Clin Orthop Relat Res. 2014;472(8):2536–2541.
- Centraal Bureau voor de Statistiek. Laag en langdurig laag inkomen; huishoudenskenmerken en regio [Statistics Netherlands. Low- and long term low incomes; household- and region characteristics]; 2017 [cited 2018 Jan 23]. Available from: https://www.volksgezondheidenzorg.info/onderwerp/sociaaleconomische-status/regionaal-internationaal/regionaal#node-huishoudens-met-laag-inkomen-gemeente
- Van Zon SKR, Snieder H, Bültmann U, et al. The interaction of socioeconomic position and type 2 diabetes mellitus family history: a cross-sectional analysis of the Lifelines Cohort and Biobank Study. BMJ Open. 2017;7(4):e015275.
- Giles-Corti B, Donovan RJ. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Prev Med (Baltim). 2002;35(6):601–611.
- Adler RH. Engel’s biopsychosocial model is still relevant today. J Psychosom Res. 2009;67(6):607–611.
