Abstract
Purpose
To determine which items regarding prosthesis use were considered most important by adults with major unilateral upper limb absence (ULA) and to develop a patient-reported outcome measure to assess the preferred usage features of upper limb prostheses: PUF-ULP.
Materials and methods
Based on a qualitative meta-synthesis combined with input from patients and clinicians a graphical diagram of 79 items related to prosthesis use was developed. Adults with ULA (N = 358; mean age = 55.4 ± 16.5 years; 52.0% male/40.8% female/7.3% unknown) selected their top-10 of most important items from this diagram. This study is registered in the Netherlands Trial Register: NL7682.
Results
Most selected items were “wearing comfort” (54.0% of cases), “grabbing, picking up, and holding” (34.3%), and “weight” (31.4%). All subpopulations (i.e. age, sex, origin of ULA, level of ULA, and prosthesis type), except multi-grip myoelectric hand prosthesis users (MHP), selected “wearing comfort” most. Nine items were included in the PUF-ULP: “wearing comfort,” “functionality,” “independence,” “work, hobby, and household,” “user-friendly,” “life-like appearance,” “phantom limb pain,” “overuse complaints,” and “reliability.”
Conclusions
All prosthesis users, except MHP-users, considered wearing comfort most important, which might be of interest for future research and industry. The PUF-ULP can be used to reflect the match between users and their prostheses.
All persons with upper limb absence, except multi-grip myoelectric hand prosthesis users, considered “wearing comfort” most important regarding prosthesis use, which highlights that prosthesis wearing comfort deserves more attention in future research to increase the value placed by the user on their upper limb prosthesis.
Regarding prosthesis use, men considered “ease of control” more important compared to the overall population, while women considered “independence,” “household,” “life-like appearance,” “overuse complaints,” and “anonymity” more important.
Persons with a mono- or multi-grip myoelectric upper limb prosthesis rated function-related items as more important compared to the overall population, while persons with a passive/cosmetic prosthesis rated comfort-related and appearance-related items as more important.
The newly developed measurement tool, also called the PUF-ULP, provides a single score that represents the match between the user and their upper limb prosthesis.
IMPLICATIONS FOR REHABILITATION
Introduction
Innovative upper limb prostheses (ULP), like the multi-grip myoelectric hand prosthesis (MHP) with moveable thumb or fingers (e.g., iLimb, Bebionic, or Michelangelo prosthetic hand), are often idealized by the media. The MHPs have advantages, but they are also experienced as less robust, less durable, difficult to control, noisier, relatively large and a cause of stump complaints compared to other prostheses [Citation1]. These disadvantages may affect the value placed by the user on their prosthesis. To consider a prosthesis to be of value for a user, we hypothesize that a match between aspects considered important by an individual and features that the prosthesis can offer is required. Considering the high rejection rates of ULP reported in the literature, it is important to improve the match between the prosthesis and the user [Citation2–6]. A first step to improve this match would be to gain more insights into items related to prosthesis use, which are considered most important by prosthesis users themselves. This information could be used to develop a measurement tool to assess the preferred usage features of ULP users. A second step would be to use this measurement tool to investigate to what extent the features of terminal devices and sockets match the aspects considered most important by the prosthesis users.
A patient-reported outcome measure (PROM) intends to measure any aspect of the health status of a patient directly from the perspective of the patient without any interpretation from anyone else than the patient [Citation7,Citation8]. Multiple studies suggest that capturing the patient’s perspective through PROMs may improve quality of care, patient satisfaction, and communication between patients and health care professionals [Citation9–11]. Nevertheless, only a few PROMs have been developed that evaluate ULP use. The Orthotics and Prosthetics Users’ Survey (OPUS) and the Trinity Amputation and Prosthesis Experience Scales (TAPES) are examples of PROMs that evaluate prosthesis use [Citation12,Citation13]. However, these PROMs were developed with respectively a broader focus (i.e. on orthotics and prosthetics from both the upper and lower limb) or a focus on lower limb amputees [Citation12,Citation13]. Subsequently, adapted versions of the TAPES and OPUS have been developed for people with upper limb amputations [Citation14,Citation15]. Yet an instrument that specifically measures the match between prostheses and the preferred usage features of ULP users, in which the contents are primarily based on what is deemed important by the ULP users themselves, seems to be lacking. Especially, since patient-centered healthcare is becoming increasingly important in clinical practice, it is of utmost importance to embed patient values and preferences into such an instrument [Citation16].
The aim of the first part of this study was to determine which items regarding prosthesis use were considered most important by people with major unilateral upper limb absence (ULA). This information will be used in the second part of this study to select a set of items that comprise the preferred usage features of ULP users. The aim of the second part was to develop a PROM to assess the preferred usage features of ULPs: the PUF-ULP.
Materials and methods
This study consists of two parts. In the first part, items that were considered most important regarding prosthesis use were identified following a three-step procedure: (1) a list of all items that could be important regarding prosthesis use was created, (2) the list of selected items was integrated into a survey, in which participants were asked to select and rank their 10 most important items, (3) the reported data was processed and analyzed. In the second part, the PUF-ULP was developed using the collected information from part 1 of the study. This study was carried out in compliance with the Declaration of Helsinki. The local Medical Ethics Review Board of the University Medical Center Groningen (UMCG) judged that formal approval of the study was not needed (METc 2018/582). Participants were asked to sign an informed consent form before filling in the survey.
Part 1: Important items regarding prosthesis use
Selection of items that could be important regarding prosthesis use
To create a list of all items that could be important to people using a prosthesis, we started with all items that were derived from our results of a meta-synthesis of qualitative literature from the users’ perspective and a focus group with patients [Citation1]. In total, 86 candidate items were extracted that were subsequently divided into six main themes: “physical,” “activities and participation,” “mental,” “social,” “rehabilitation, costs, and prosthetist services,” and “prosthesis related factors” [Citation1]. However, not all candidate items seemed suitable to fulfill the aims of the current study. First, our previous study focused on items related to prosthesis choice. In the current study, we aimed to develop a PROM to assess the preferred usage features of ULPs, where we chose to focus on prosthesis use and not on prosthesis choice. Second, while our previous study revealed that “gender” and “origin of limb loss” were influencing items for prosthesis choice, such items are fixed personal characteristics [Citation1]. Therefore, such items were considered unsuitable for a preference-based PROM (see part 2: development of PUF-ULP). In consensus meetings with the research team, all candidate items were discussed for suitability and checked on clarity and completeness. Furthermore, items were added if the research team agreed on them ().
Table 1. Themes that were adapted and items that were added (N = 6) and deleted (N = 13) from the initial candidate set of 86 items [Citation1], creating a final set of seven themes that contained 79 items.
As a final check, 16 national health care professionals (i.e. hand/occupational therapists, prosthetists, and rehabilitation doctors) were invited to check all items on clarity and completeness. Three-hand/occupational therapists and one prosthetist provided feedback, which resulted in the addition of two items (). Last, to improve the structure and clarity, main themes were adapted if the research team deemed this to be appropriate (). The final set of items and themes that could be important regarding prosthesis use consisted of seven themes that contained 79 items.
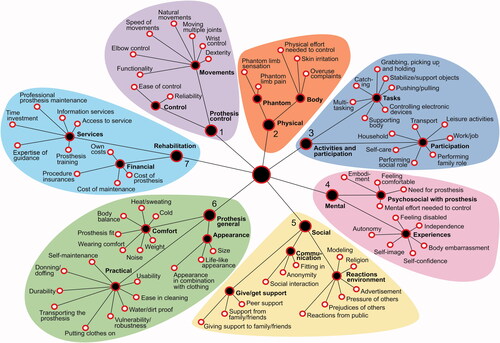
To create a clear and attractive overview, all included items were depicted in a semi-automatically generated software-based graphical diagram: HealthFan () [Citation17–19].
Figure 1. Seventy-nine items may be important when using a prosthesis depicted in a HealthFan diagram. The white-filled circles represent the items; the black-filled circles represent the seven themes and all subthemes. Themes and subthemes are presented in bold font, themes are marked with numbers 1–7. Each leaf of the diagram represents a theme and was depicted in another color.
Survey development
The created HealthFan was integrated into a digital survey (HealthFan; version 1.0; www.chateau-sante.info). Pilot tests with members of the research team, fellow researchers, acquaintances, and patients without ULA were carried out. Subsequently, the layout of the survey was adapted to improve the clearness and feasibility. In the HealthFan survey, participants were asked to (1) select the 10 most important items regarding prosthesis use from the HealthFan diagram; (2) rank those 10 items from most important to least important; (3) indicate whether they missed certain items in the HealthFan diagram. For some items, explanations appeared when hovering on them. Participants received a link to the HealthFan survey with a single-usable login code on paper.
Due to privacy reasons, questions regarding personal data were administered separately in a paper survey. This included the informed consent form, patient demographics (i.e. age, sex, educational degree, job, side of ULA, the origin of ULA, time since ULA, level of ULA, and type of prosthesis used most, years of experience with prosthesis use) and a question about the satisfaction with their current prosthesis.
Data collection
Between September and December 2019, we approached adults (age ≥18 years) with an acquired amputation or congenital ULA at or proximal of the wrist from two large orthopedic workshops, with several branches all over the country, and nine out of the 10 rehabilitation centers that prescribe ULPs in the Netherlands. Non-prosthesis users were also included because not using a prosthesis is often a conscious consideration as well. Reminders were sent in case no response was received within 2–4 weeks. The reminder included an option to complete the HealthFan survey on paper (e.g., for people with no internet or lack of computer skills). A total of 63 participants, who did only fill out their personal data (partially) but not the assignments of the HealthFan survey, were sent a request to complete the HealthFan survey, and if applicable, complete other missing personal data. This was only applicable to those participants who filled in their address on the returned survey. The first 18 participants with missing answers in their personal data, but without missing data in the HealthFan survey, were also sent a request to answer these unanswered questions. However, since this was very time-consuming and yielded too little result, we decided to discontinue the latter reminder. Participants received an incentive of €10.- after returning the completed survey.
Data analysis
Data were managed using REDCap data capture tools [Citation20,Citation21]. Data from the HealthFan survey were saved on the HealthFan server and subsequently exported to RedCap. Personal data and data from the HealthFan surveys filled out on paper were entered manually into RedCap. Before statistical analysis was carried out the returned surveys were checked for duplicates. This was only possible if participants had provided personal details. Duplicates were expected since participants were approached by both rehabilitation centers and orthopedic workshops. Despite the warning on the title page of the survey, which warned participants that they may receive the survey from multiple paths and should only complete the survey once, a total of 12 duplicates were identified. In these cases, the most complete survey was used for analysis (). If both surveys were equally complete, the first entered survey in the database was used for analysis. Since 23 of the participants checked multiple boxes when they were asked which prosthesis they used most, the variable “prosthesis used most” was regrouped into the categories mono-grip myoelectric, multi-grip myoelectric, body-powered, passive, and no prosthesis. In this way, more data could be used for analyses. Additionally, the variables “highest educational degree” and “level of limb absence” were regrouped to enlarge subgroups. The six participants with bilateral ULA were excluded from analyses since this sample was too small for separate subgroup analysis ().
Statistical analysis
Frequency distributions were generated for all items depicted in the HealthFan. Subgroup analyses were generated for age, sex, the origin of ULA, level of ULA, and type of prosthesis used most. A difference in frequency of at least 5% between subpopulation and overall population was defined as relevant. Furthermore, an explorative multivariate analysis (partial least squares regression: PLS) was performed. PLS is a dimension reduction technique that is a combination of principal component analysis and multiple linear regression [Citation22]. One block of variables is linked with another block of variables. In our case, the background characteristics of the users (predictor variables) were mapped to the set of top-10 prosthesis use items. PLS tries to maximally explain the relative contribution of the background characteristics for each top-10 item [Citation22,Citation23]. As the estimation of the PLS contribution weights is relative, interpretations should be taken cautiously. Therefore, we only interpreted predictors with variable importance in the projection (VIP) higher than 1.5% [Citation23]. Data were analyzed using IBM SPSS Statistics for Windows, version 23 (IBM Corp, Armonk, NY). Graphs were created using R (tidyverse package) [Citation24,Citation25] and CorelDRAW® Graphics Suite 2020 (Corel Corporation, Ottawa, Canada).
Part 2: Development of PUF-ULP
After finishing part 1 of the study, the construct development of the PUF-ULP started. The PUF-ULP is intended to be used as a short and practical measurement tool in clinical practice or research for people with unilateral ULA at or proximal from the wrist. The outcome of the PUF-ULP was the extent to which a prosthesis meets the preferred usage features of a ULP user. Thus the preferred usage features of ULP are dependent on what is deemed important by an individual. Therefore, the results of part 1 of the study, in which participants indicated which items regarding prosthesis use were important for them, were used to select the preferred usage features of ULPs to include in the PUF-ULP. We aimed to develop a preference-based measurement tool to be able to calculate a score that represents the extent to which a prosthesis meets the preferred usage features of ULPs [Citation26]. In preference-based measurement tools, participants typically compare one or more situations with each other and indicate which situation they prefer [Citation26]. Another feature of a preference-based instrument is that all included items have to be assessed simultaneously [Citation26]. As people can only process limited information at one time, the maximum amount of items to be included in the PUF-ULP was set at nine [Citation27,Citation28]. To decide which items should be included in the PUF-ULP two consensus meetings were held with one rehabilitation doctor/professor in hand prosthetics (CS), one hand therapist (PW), one PROM expert (PK), one implementation expert (SvT), one assistant professor from human movement sciences (RB), one research assistant (CB), and two Ph.D. students (XZ and NK). Patients were not invited to these meetings, because we believe that a proper understanding of all analyses of the survey results and a broad and objective view of the needs of the total group of patients were needed to select items for the PUF-ULP. In the consensus meetings, the HealthFan survey results were discussed. These results included thorough analyses from the overall population, subpopulations, and post-hoc ranking of the data (e.g., items selected most in the top-5 and items considered most as number one). Additionally, to determine if multiple items could be covered by one overarching term, conceptual analyses into possible combinations of different items were performed. To clarify those overarching items, a description of their definition was added. Subsequently, the selected items were confirmed and operationalized into questionnaire items with answer categories on an ordinal scale. Special attention was made to the use of lay language.
Results
Part 1: Important items regarding prosthesis use
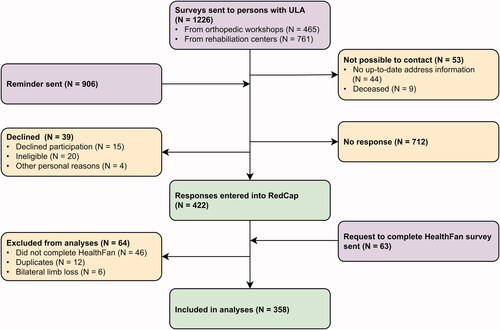
Survey response
Surveys were sent to 1226 participants, of whom 465 were approached by orthopedic workshops and 761 by rehabilitation centers (). Reminders were sent to 906 participants. In the first 88 reminders sent, participants could not assign any missing items of the HealthFan on paper. In the subsequent reminders, this option was added. Eventually, 358 participants were included for analyses. We did not calculate a response rate because of the expected overlap between the populations recruited from the rehabilitation centers and orthopedic workshops.
Population characteristics
Out of the 358 participants, 186 were males (52.0%), 146 were females (40.8%), and from 26 participants the sex was unknown (7.3%) (). The average age was 55.4 years (SD = 16.5; N = 338); 303 were prosthesis users (84.6%), 41 non-users (11.5%), and from 14 participants it was not known whether they used a prosthesis (3.9%). Out of the 41 non-users, 32 participants used a prosthesis in the past (78.0%) and nine participants never used a prosthesis (22.0%). Prosthesis-users started to use their first prosthesis on average 33.1 years (SD = 21.0; N = 295) before completing the survey.
Table 2. Characteristics of the 358 participants.
HealthFan survey
A total of 257 participants completed the digital HealthFan survey and 101 the paper version. Due to the option to fill out the HealthFan survey also on paper, participants could write more or less than the 10 requested items or could skip the ranking task, which was not possible in the digital HealthFan survey. If participants selected and ranked more than 10 items, the first 10 were entered into RedCap. Items were assigned as missing if <10 items were selected (N = 12), items were unclear (N = 5), more than 10 items were selected and not ranked (N = 3), and if the HealthFan survey was not filled out the way it was meant (N = 5). From eight out of the 358 included participants all items were assigned as missing. Therefore, the item analysis was ultimately based on 350 responses.
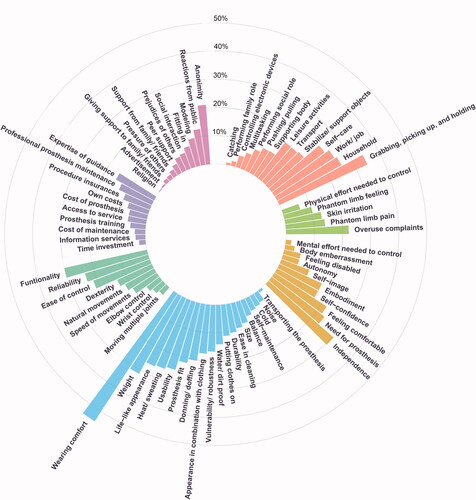
The frequency of how often each HealhFan item was selected in the top-10 from the participants was calculated (). Most selected items in consecutive order were: “wearing comfort” (54.0%); “grabbing, picking up, and holding” (34.3%); “weight” (31.4%); “independence” (30.6%); “functionality” (30.0%); “life-like appearance” (26.6%); “heat/sweating” (26.0%) and “household” (26.0%); “usability” (25.1%) and “work/job” (25.1%).
Figure 3. Circular barplot presenting how often participants (N = 350) selected each HealthFan item in their top-10. The lengths of the bars represent the percentage of participants who selected the particular item. The different colors represent the seven themes (clockwise): salmon = activities and participation; green = physical; yellow = mental; blue = prosthesis general; aquamarine = prosthesis control; purple = rehabilitation; violet = social.
Subgroup analyses
Only relevant differences from items selected by more than 25% of the subpopulations will be discussed below (Supplementary Material 1). See Supplementary Material 2 for the top-20 selected items from all subpopulations.
Age. People aged between 18 and 40 years selected “weight,” “work/job,” “ease of control,” “usability,” and “anonymity” more compared to the overall population. Although “wearing comfort” was selected less frequently by this group compared to the overall population, this item was still the most selected item by people aged 18–40 years. No substantial differences were found between people aged 41–65 years and the overall population. People aged 66 years and older selected “need for prosthesis” more often.
Sex. Women selected “independence,” “household,” “life-like appearance,” “overuse complaints,” and “anonymity” more often compared to the overall population, while “grabbing, picking up, and holding” and “functionality” were selected less frequently. Men selected “ease of control” more often.
Origin of limb absence. People with congenital ULA selected the items “weight,” “life-like appearance,” “household,” “work/job,” and “anonymity” more often compared to the overall population. No substantial differences were found between people with an acquired amputation and the overall population.
Level of limb absence. People with ULA at or proximal from the elbow selected “donning/doffing” more often compared to the overall population, and “grabbing, picking up, and holding” less. People with ULA distal from the elbow selected “household” and “self-care” more often.
Type of prosthesis used most. People who used a mono-grip myoelectric prosthesis most selected “grabbing, picking up, and holding,” “reliability,” “independence,” “need for prosthesis,” “ease of control,” and “work/job” more frequently. MHP-users selected “household,” “grabbing, picking up, and holding,” “weight,” “reliability,” “independence,” “work/job,” “speed of movements,” “heat/sweating,” “dexterity,” and “overuse complaints” more. MHP-users selected “wearing comfort” less. Cosmetic/passive prosthesis users selected “wearing comfort,” “life-like appearance,” “prosthesis fit,” “anonymity,” “donning/doffing,” and “appearance in combination with clothing” more often, and they selected “independence” less often. People with a body-powered prosthesis selected “wearing comfort,” “grabbing, picking up, and holding,” “usability,” “need for prosthesis,” and “feeling comfortable” more frequently compared to the overall population. Non-users selected “weight,” “functionality,” “ease of control,” and “phantom limb pain” more often as the most important factors too, in these cases, not to use a prosthesis.
Items missing in the HealthFan
A total of 62 participants indicated that they missed one or more items in the HealthFan diagram. Out of the 69 suggested items, 60 were already included in the HealthFan diagram. The following new items were identified by the participants: “acceptance” (1×), “stump pain” (1×), “sensation” (1×) and “involvement of a health care professional” (2×). Additionally, three items that did not suit the aims of this study were suggested: the fixed item “stump length” (1×) and the items “accessories/tools for prosthesis” (1×) and “option to determine the looks of a prosthesis yourself” (1×), which were consciously not included in the HealthFan diagram. Last, the item “shared decision making” was suggested (1×), which may be applicable for prosthesis choice, but less for prosthesis use, the focus of this study.
Partial least squares regression
The first and overall latent variable explained 13.5% of the variance in the choice of the top-10 selected items. The most relevant predictors for the choice of the top-10 selected items were older age (VIP = 1.99%) and not having a job (VIP = 1.59%), meaning that the PLS model can predict the top-10 selected items best for older people and people with no job. The contribution of sex and education was low.
Part 2: Development of the PUF-ULP
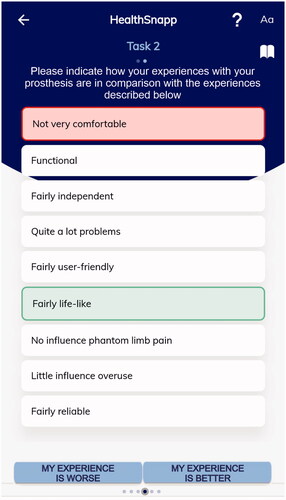
The following nine items were selected for inclusion in the PUF-ULP: “wearing comfort,” “functionality,” “independence,” “work, hobby and household,” “user-friendly,” “life-like appearance,” “phantom limb pain,” “overuse complaints,” and “reliability.” In Supplementary Material 3 the rationale to include these nine items and their definitions are given. All selected items were integrated into the data collection technology HealthSnApp 4.0 (www.chateau-sante.info) [Citation27]. The HealthSnApp technology is based on a simple (i.e. comparing own condition with a few hypothetical conditions) but robust measurement model that has a connection with the Rasch model [Citation29,Citation30]. The PUF-ULP exists of two tasks. In the first task, participants are asked to describe their present experiences with their prosthesis by ranking the nine included items (). As in the studies of Krabbe et al. and Shahabeddin Parizi et al., in which the same methodology and software were used to develop a PROM, each item had four answer categories (Supplementary Material 3) [Citation19,Citation27]. By clicking on the information sign (i) in the software, the definition of the item is shown. In the second task, participants are asked to compare their own described experiences with slightly different experiences and to indicate whether they think their situation is better or worse than the shown experiences (). An advantage of this new measurement model is the ability to calculate a single score, which in this case represents the extent to which a prosthesis meets the preferred usage features of ULPs [Citation29,Citation30].
Figure 4. The first task of the developed mobile measurement tool is to assess the preferred usage features of upper limb prostheses (PUF-ULP). The nine included items are depicted on screen A. When clicking on the items on screen A, the answer options will change (screen B). Each item has four answer options (C). The colors of the answers on screen B correspond with the answers in C. By clicking on the information sign (i) on-screen A or B, the definition of the item will appear.
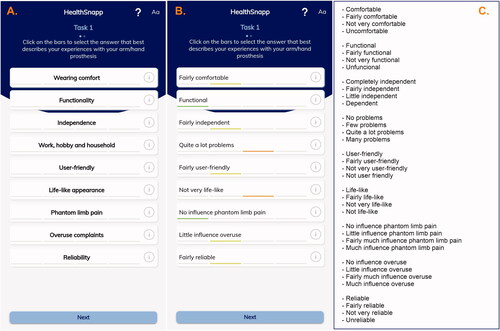
Figure 5. The second task of the developed mobile measurement tool is to assess the preferred usage features of upper limb prostheses (PUF-ULP). Participants were asked to compare their own experiences with their upper limb prosthesis as rated in task 1 with the shown experiences. In the shown experiences, one item will get better compared to the participant's experiences (green accent) and one will get worse (red accent). When clicking on the “book” sign in the upper right corner, the answers given in task 1 will appear.
Discussion
In this survey study, 358 participants with ULA selected their top-10 most important items regarding prosthesis use from an extensive overview, also called the HealthFan (). “Wearing comfort” was selected most frequently by the overall population, as well as by most subpopulations except MHP-users. Furthermore, other comfort-related (e.g., “weight,” “heat/sweating”) and function-related items (e.g., “grabbing, picking up, and holding,” “functionality,” and “usability”) were considered important. With regard to the subpopulations, men rated “ease of control” as more important compared to the overall population, while women considered “independence,” “household,” “life-like appearance,” “overuse complaints,” and “anonymity” more important. Furthermore, people with a mono- or multi-grip prosthesis rated function-related items as more important compared to the overall population, while people with a passive/cosmetic prosthesis rated comfort-related and appearance-related items as more important. Based on the results of the HealthFan survey, nine items were selected to include in the PUF-ULP.
Our results indicate that people with ULA consider comfort and function most important when using a ULP, which is in line with the literature, in which dissatisfaction with function or comfort were mentioned frequently as reasons for prosthesis abandonment [Citation2,Citation6,Citation31–33]. Most research in the field of hand prosthetics focuses on the improvement of function or control techniques, like pattern recognition control or restoring sensation [Citation34–37]. Remarkably, there seems to be far less research focusing on improving the wearing comfort of prostheses, while multiple studies underline the importance of comfort [Citation31,Citation38]. Central to the issue of discomfort seems to be the socket design. A promising and recently upcoming technique to overcome the limitations of conventional socket design is osseointegration (i.e. bone-anchored prostheses) [Citation34,Citation39,Citation40]. However, this technique is only available for a limited number of people. Another potential solution for prosthesis discomfort, that still has to be explored, is the customized 3D printed prosthetic sockets [Citation41,Citation42]. We would encourage new studies and the industry to heed the needs of people with ULA and further investigate solutions that may improve the comfort of ULPs.
In the review of Smail et al., it was stated that only a few studies addressed the use of contemporary devices like MHPs [Citation31]. In our study, MHP-users were analyzed as a separate subgroup. The main difference between an MHP and other prostheses is the number of grips that can be performed. Our results confirmed that function-related items (e.g., “grabbing, picking up, and holding,” “dexterity,” “reliability,” and “speed of movements”) were more important for MHP-users compared to the overall population. The finding that “reliability” was considered more important by MHP-users, may be explained by the more complex control and lower durability of these devices [Citation1]. Furthermore, it was interesting that “household” was considered important by MHP-users, while MHPs are often experienced as less durable [Citation1]. This may be explained by the more convenient grips to hold objects and tools used during household activities. Another remarkable result is that MHP-users were the only subpopulation that did not consider “wearing comfort” as the most important item regarding prosthesis use. Since the socket of the MHP is comparable with the socket of the SHP, this may be explained by a higher priority for prosthesis function within this subpopulation, which might also be the reason that they pursued an MHP. Although our study included only 30 MHP-users, this is a considerable number in comparison with previously published papers [Citation43,Citation44]. Additional studies that include more MHP-users are needed to confirm the results of this study.
Our study suggests that the items considered important by people using different types of prostheses are generally consistent with the purpose of these prostheses: people with a passive/cosmetic prosthesis considered comfort-related and appearance-related items more important, while myoelectric prosthesis users often considered function-related items more important. This is in line with the literature, in which those differences in preferences, needs, or reasons to abandon a prosthesis often also differed based on the type of prosthesis used [Citation2,Citation3,Citation31,Citation45]. Additionally, the non-users included in this study provided valuable information about specific items, such as “weight,” “functionality,” “ease of control,” and “phantom limb pain.” They considered these items important regarding not using a prosthesis. Apparently, prosthetic features were valued differently by users and non-users, which should be the topic of further research. Notably, there seem to be fewer studies in the literature that analyzed differences in items considered important by separate subgroups based on other demographic characteristics. In our study, subgroups with different demographic characteristics showed interesting differences in items that were considered important. For instance, for people with a more proximal level of ULA donning and doffing of the prosthesis was more important compared to other subgroups. A likely reason seems to be that donning and doffing of a prosthesis is more difficult with a more proximal level of ULA. Another example is that men indicated that “ease of control” was considered more important for them compared to the overall population, while women considered appearance-related items, independence, household, and overuse complaints more important. The differences in items considered important by the subgroups could be used as focus areas to inform patients who intend to use a prosthesis and to evaluate prosthesis use in clinical practice, and thereby lead to a more realistic expectation pattern of the patient.
This study focused on prosthesis use, which implies another concept than wearing time. For example, a user can be satisfied with their ULP, even though the prosthesis is only worn for several hours a week. Consequently, there may be a difference in the factors influencing wearing time and use. Therefore, it would be interesting to replicate this study with a focus on wearing time.
Recent literature suggested that age is one of the variables that may be related to prosthesis satisfaction [Citation46]. Although our study did not focus on satisfaction but on items considered important regarding prosthesis use, in our study age was also identified as a relevant predictor. Additionally, “not having a job” was identified as a relevant predictor. Possibly, unemployed people execute other tasks in daily living compared to employed people and therefore judge other items regarding prosthesis use more important. It should however be noted that the PLS analysis could only explain 13.5% of the variance in the choice of the selection of the top-10 most important items. On the one hand, this seems to be due to the relatively small data set used for this type of analysis. On the other hand, this result confirms that the background variables of an individual could provide focus areas for prosthesis selection and evaluation in clinical practice, but the personal situation and an individual’s own experiences with ULPs should also be taken into account.
The contents of the HealthFan survey were based on a meta-synthesis of qualitative literature and a focus group, which both only included the perspectives from people with ULA [Citation1]. Subsequently, the HealthFan survey was sent to people with ULA. Due to this strong involvement of people with ULA in the selection of a set of items that comprise the preferred usage features of ULP, the personal values of the target population are well represented in the new PUF-ULP, making it a user-relevant PROM with expectedly a high content validity. Because the measurement model reflects the perception and reporting of patients themselves, it is also less sensible for biases, such as coping and adaptation [Citation26,Citation30]. In a future study, we have planned to use the PUF-ULP in a group of ULP users.
The PUF-ULP is a short and practical measurement tool, which can be used in clinical practice or future research, to investigate to what extent features of terminal devices and sockets match the aspects considered most important by the prosthesis users. Although the PUF-ULP was primarily developed to evaluate prosthesis use, the information gathered with the PUF-ULP may be useful for prosthesis selection as well. For instance, this information can be used to develop a decision aid for patients who are considering wearing a prosthesis. Decision aids are tools designed to assist people in choosing between two or more health care options by providing information about the different options and to help by identifying and communicating about personal values that may affect the decision [Citation47]. Literature suggests that people using a decision aid feel more knowledgeable, better informed, more clear about their personal values, and they probably participate more in the decision-making process [Citation48]. Therefore, a decision aid for ULP could help the user and healthcare professional to determine which prosthesis hand fits the users’ values best.
Some limitations of this study should be mentioned. First, since we aimed to develop a most complete overview of items that may be important when using a prosthesis, the HealthFan diagram contained a large number of these. Consequently, selecting the top-10 items from the HealthFan diagram may have been difficult for some people. The fact that most of the items that were assigned as missing were already included in the HealthFan diagram, also suggests that the HealthFan diagram may not have been clear enough for everyone. Second, filling out a survey digitally also appeared to be difficult for some people. To resolve this problem, the reminder included a paper version of the HealthFan survey, which may have introduced some differences in responses [Citation49]. Third, the item “grip force” was not included in the HealthFan diagram by mistake. However, none of the participants identified “grip force” as missing, which makes it unlikely that this is one of the most relevant items regarding prosthesis use. Fourth, the importance of the missing items that were suggested by the participants is unknown. Fifth, it may be possible that not all duplicates were identified since participants from both rehabilitation centers and orthotic workshops were invited and duplicates could only be checked for if participants provided personal details. Inviting people from both sources had also advantages since we reached a large sample from this target population compared to the literature. Sixth, some people owned more than one type of prosthesis, while in the HealthFan survey we did not instruct the respondents to select the 10 most important items related to the prosthesis they used most. Seventh, non-users may be underrepresented in the study sample. Compared to other Dutch survey studies performed with the same target population, our sample included a relatively small proportion of non-users [Citation50,Citation51]. Therefore, this might not be a representative sample of the Dutch population of people with ULA. Last, the items considered important regarding prosthesis use may differ for people with ULA from other countries with other cultures and different health care systems. Therefore, results should be generalized cautiously.
In conclusion, “wearing comfort” was considered most important regarding prosthesis use by people with ULA, except for the MHP users. Additionally, other comfort-related and function-related items were considered important. These results emphasize the need to prioritize improvements of the wearing comfort of prostheses more. Based on the survey results, in which people with ULA identified which items regarding prosthesis use were most important to them, nine items were selected for a PROM to assess the preferred usage features of ULP: the PUF-ULP. Due to the strong involvement of people with ULA in the development of the PUF-ULP, the patient values are well represented in this new tool. The PUF-ULP is a short and practical measurement tool and therefore suitable to be used as an evaluation tool in clinical practice or future research. With the PUF-ULP valuable information can be gathered about the match between an individual and a prosthesis, which may be used to improve providing information about ULP in the clinic to create more realistic expectation patterns among patients. Ultimately, we hope this will contribute to lower rejection rates of ULP.
Supplemental Material
Download PDF (136 KB)Supplemental Material
Download PDF (180.5 KB)Supplemental Material
Download PDF (78.3 KB)Acknowledgements
The authors would like to thank C.J. Blekkink for administrative and logistic work. Furthermore, we would like to thank all people from participating rehabilitation centers and orthopedic workshops who helped to send the surveys: M.A.H. Brouwers and A. Rijkse from the Hoogstraat Rehabilitation; W.G.M. Janssen from Rijndam Rehabilitation Center; M. Heurman and J.S. Rietman from Roessingh Center for Rehabilitation; N. Ringeling, C. Vervoort, and E. Huijsman from Revant Rehabilitation Center; J.W.E. Verlouw from Adelante Rehabilitation; C. Utens, A. van Haelst, and D. ten Haaf from Libra Rehabilitation & Audiology; A. van der Grijn and S.M. Brink from Vogellanden, Centre of Rehabilitation Medicine & Special Dentistry; A.M. van de Ven, I. Vermeulen, and T.C.H. Singer from Military Rehabilitation Center Aardenburg; E. Mik, M. Ruiter-Geurts, and W. Akkerman from Livit Orthopedie; C. Vergeer, Y.L. Kerkum, K. de Jonge, and R. van Willegen from OIM Orthopedie. Last, we would like to thank X. Zhang for her help with , and V. Schuurmans, A. Hoogerkamp, and L. Boerema for their help with .
Disclosure statement
There were no conflicts of interest to be mentioned.
Data availability statement
Data that supports the findings of this study are availably on DataVerseNL under the following link: https://doi.org/10.34894/OCZJAL.
Additional information
Funding
References
- Kerver N, van Twillert S, Maas B, et al. User-relevant factors determining prosthesis choice in persons with major unilateral upper limb defects: a meta-synthesis of qualitative literature and focus group results. PLOS One. 2020;15(6):e0234342.
- Biddiss E, Beaton D, Chau T. Consumer design priorities for upper limb prosthetics. Disabil Rehabil Assist Technol. 2007;2(6):346–357.
- Biddiss E, Chau T. Upper limb prosthesis use and abandonment: a survey of the last 25 years. Prosthet Orthot Int. 2007;31(3):236–257.
- Wright TW, Hagen AD, Wood MB. Prosthetic usage in major upper extremity amputations. J Hand Surg Am. 1995;20(4):619–622.
- McFarland LV, Hubbard Winkler SL, Heinemann AW, et al. Unilateral upper-limb loss: satisfaction and prosthetic-device use in veterans and servicemembers from Vietnam and OIF/OEF conflicts. JRRD. 2010;47(4):299–316.
- Salminger S, Stino H, Pichler LH, et al. Current rates of prosthetic usage in upper-limb amputees–have innovations had an impact on device acceptance? Disabil Rehabil. 2020;30:1–12.
- Prinsen CAC, Mokkink LB, Bouter LM, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–1157.
- U.S. Department of Health and Human Services Food and Drug Administration. Guidance for industry patient-reported outcome measures: use in medical product development to support labeling claims; 2009 [cited 2021 Jan 14]. Available from: https://www.fda.gov/media/77832/download
- Kotronoulas G, Kearney N, Maguire R, et al. What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol. 2014;32(14):1480–1501.
- Holmes MM, Lewith G, Newell D, et al. The impact of patient-reported outcome measures in clinical practice for pain: a systematic review. Qual Life Res. 2017;26(2):245–257.
- van Egdom LSE, Oemrawsingh A, Verweij LM, et al. Implementing patient-reported outcome measures in clinical breast cancer care: a systematic review. Value Health. 2019;22(10):1197–1226.
- Gallagher P, MacLachlan M. Development and psychometric evaluation of the trinity amputation and prosthesis experience scales (TAPES). Rehabil Psychol. 2000;45(2):130–154.
- Heinemann AW, Bode RK, O'Reilly C. Development and measurement properties of the orthotics and prosthetics users' survey (OPUS): a comprehensive set of clinical outcome instruments. Prosthet Orthot Int. 2003;27(3):191–206.
- Desmond DM, MacLachlan M. Factor structure of the trinity amputation and prosthesis experience scales (TAPES) with individuals with acquired upper limb amputations. Am J Phys Med Rehabil. 2005;84(7):506–513.
- Burger H, Franchignoni F, Heinemann AW, et al. Validation of the orthotics and prosthetics user survey upper extremity functional status module in people with unilateral upper limb amputation. J Rehabil Med. 2008;40(5):393–399.
- Sacristán JA. Patient-centered medicine and patient-oriented research: improving health outcomes for individual patients. BMC Med Inform Decis Mak. 2013;13(1):6.
- Reneman M, Brandsema K, Schrier E, et al. Patients first: toward a patient-centered instrument to measure impact of chronic pain. Phys Ther. 2018;98(7):616–625.
- Shahabeddin Parizi A, Krabbe PFM, Buskens E, et al. A scoping review of key health items in self-report instruments used among solid organ transplant recipients. Patient. 2019;12(2):171–181.
- Shahabeddin Parizi A, Krabbe PFM, Buskens E, et al. Health items with a novel patient-centered approach provided information for preference-based transplant outcome measure. J Clin Epidemiol. 2020;126:93–105.
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
- Abdi H. Partial least squares regression and projection on latent structure regression (PLS regression). WIREs Comp Stat. 2010;2(1):97–106.
- Pirouz DM. An overview of partial least squares. Bus Publ [Internet]; 2006 [cited 2021 Jan 25]; p. 24. Available from: https://ir.lib.uwo.ca/iveypub/24
- R Development Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2019. Available from: https://www.r-project.org/
- Wickham H, Averick M, Bryan J, et al. Welcome to the tidyverse. JOSS. 2019;4(43):1686.
- Krabbe P. The measurement of health and health status: concepts, methods and applications from a multidisciplinary perspective. San Diego (CA): Elsevier/Academic Press; 2016.
- Krabbe PFM, van Asselt ADI, Selivanova A, et al. Patient-centered item selection for a new preference-based generic health status instrument: CS-base. Value Health. 2019;22(4):467–473.
- Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev. 1956;63(2):81–97.
- Groothuis-Oudshoorn CGM, Van Den Heuvel ER, Krabbe PFM. A preference-based item response theory model to measure health: concept and mathematics of the multi-attribute preference response model. BMC Med Res Methodol. 2018;18(1):1–13.
- Krabbe PFM. A generalized measurement model to quantify health: the multi-attribute preference response model. PLOS One. 2013;8(11):e79494.
- Smail LC, Neal C, Wilkins C, et al. Comfort and function remain key factors in upper limb prosthetic abandonment: findings of a scoping review. Disabil Rehabil Assist Technol. 2020;19:1–10.
- Stephens-Fripp B, Jean Walker M, Goddard E, et al. A survey on what Australians with upper limb difference want in a prosthesis: justification for using soft robotics and additive manufacturing for customized prosthetic hands. Disabil Rehabil Assist Technol. 2020;15(3):342–349.
- Yamamoto M, Chung KC, Sterbenz J, et al. Cross-sectional international multicenter study on quality of life and reasons for abandonment of upper limb prostheses. Plast Reconstr Surg. 2019;7(5):e2205.
- Bates TJ, Fergason JR, Pierrie SN. Technological advances in prosthesis design and rehabilitation following upper extremity limb loss. Curr Rev Musculoskelet Med. 2020;13(4):485–493.
- Das N, Nagpal N, Bankura SS. A review on the advancements in the field of upper limb prosthesis. J Med Eng Technol. 2018;42(7):532–545.
- Parajuli N, Sreenivasan N, Bifulco P, et al. Real-time EMG based pattern recognition control challenges and future implementation. Sensors. 2019;19(20):4596.
- Wolf EJ, Cruz TH, Emondi AA, et al. Advanced technologies for intuitive control and sensation of prosthetics. Biomed Eng Lett. 2020;10(1):119–128.
- Peerdeman B, Boere D, Witteveen H, et al. Myoelectric forearm prostheses: state of the art from a user-centered perspective. J Rehabil Res Dev. 2011;48(6):719–737.
- Vujaklija I, Farina D, Aszmann OC. New developments in prosthetic arm systems. Orthop Res Rev. 2016;8:31–39.
- Farina D, Amsuss S. Reflections on the present and future of upper limb prostheses. Expert Rev Med Devices. 2016;13(4):321–324.
- Diment LE, Thompson MS, Bergmann JH. Three-dimensional printed upper-limb prostheses lack randomised controlled trials: a systematic review. Prosthet Orthot Int. 2018;42(1):7–13.
- ten Kate J, Smit G, Breedveld P. 3D-printed upper limb prostheses: a review. Disabil Rehabil Assist Technol. 2017;12(3):300–314.
- Franzke AW, Kristoffersen MB, Bongers RM, et al. Users' and therapists' perceptions of myoelectric multi-function upper limb prostheses with conventional and pattern recognition control. PLOS One. 2019;14(8):e0220899.
- Luchetti M, Cutti AG, Verni G, et al. Impact of Michelangelo prosthetic hand: findings from a crossover longitudinal study. J Rehabil Res Dev. 2015;52(5):605–618.
- Cordella F, Ciancio AL, Sacchetti R, et al. Literature review on needs of upper limb prosthesis users. Front Neurosci. 2016;10:209.
- Resnik L, Borgia M, Heinemann AW, et al. Prosthesis satisfaction in a national sample of veterans with upper limb amputation. Prosthet Orthot Int. 2020;44(2):81–91.
- Volk RJ, Llewellyn-Thomas H, editors. The 2012 IPDAS background document: an introduction. In: Update of the international patient decision aids standards (IPDAS) collaboration’s background document; 2012. Available from: http://ipdas.ohri.ca/resources.html
- Stacey D, Légaré F, Lewis K, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;(4):CD001431.
- Juniper EF, Langlands JM, Juniper BA. Patients may respond differently to paper and electronic versions of the same questionnaires. Respir Med. 2009;103(6):932–934.
- Postema SG, Bongers RM, Brouwers MA, et al. Upper limb absence: predictors of work participation and work productivity. Arch Phys Med Rehabil. 2016;97(6):892–899.
- Postema SG, Bongers RM, Brouwers MA, et al. Musculoskeletal complaints in transverse upper limb reduction deficiency and amputation in The Netherlands: prevalence, predictors, and effect on health. Arch Phys Med Rehabil. 2016;97(7):1137–1145.