Abstract
Purpose
Post-stroke emotionalism (PSE) is a common consequence of stroke characterised by episodes of crying or laughing. There is only one published qualitative study exploring the experience of emotionalism to date. This study aimed to explore individual’s experience of PSE and develop a theoretical client-derived framework to shape future psychological interventions.
Materials and methods
A primary analysis of the qualitative pseudonymised pre-collected semi-structured interview data of the TEARS study was completed. Participants were recruited from nine acute stroke units in Scotland with participants commencing the study at baseline (two-weeks) and they either continued or dropped out. Interviews were completed at two-weeks, six-months and 12-months post-stroke.
Results
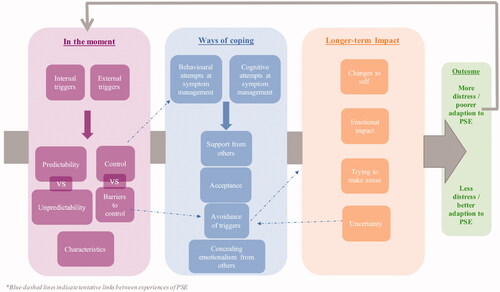
Data was analysed from 52 participants at two-weeks, 25 participants at six-months and 23 participants at 12-months. Three major themes were identified: “In the moment,” describing characteristics and triggers, “Ways of coping,” highlighted a variation of coping strategies including avoidance or acceptance and “Impact,” outlining the longer-term effects of PSE such as individuals’ beliefs.
Conclusion
The results indicate specific psychological aspects of PSE which could be viable targets in psychological interventions such as increasing adaptive coping strategies and challenging negatively held beliefs.
Emotionalism can cause emotional consequences such as distress, embarrassment and fear.
Helping individuals to develop insight into triggers for emotionalism could be beneficial to help gain understanding and awareness whereby post-stroke emotionalism (PSE) has the potential to be anticipated and adapted to psychologically.
Potential adaptive responses such as acceptance or control and better anticipation of episodes of emotionalism could help to reduce the emotional consequences of PSE.
IMPLICATIONS FOR REHABILITATION
Introduction
Stroke is a major public health problem and the single largest cause of adult disability in the United Kingdom [Citation1]. There are over 1.2 million people with stroke in the UK with one individual suffering a stroke every five minutes [Citation2] and approximately 30% of individuals who have had a stroke will experience another stroke [Citation3]. Worldwide, approximately 15 million individuals suffer a stroke each year [Citation4]. Stroke can have a lasting impact on individual lives and on the lives of carers and families. The effects of stroke can vary considerably, but can include loss of mobility, language, vision, cognition and sensory function.
Stroke can also have wide ranging mood and emotional consequences. For many individuals, adjusting psychologically to the sudden onset functional changes of a stroke may lead to a phase of heightened distress, low mood and/or anxiety [Citation5]. For some individuals, there may be more long-lasting mood difficulties. Research shows for example, that one-third of people with stroke experience post-stroke depression [Citation6] and one-quarter experience post-stroke anxiety [Citation7].
A common but much less researched consequence of stroke is emotionalism. The condition is also known as emotional incontinence, pseudobulbar affect, emotional lability, pathological laughing and crying or involuntary emotional expression disorder and it is not stroke-specific, arising following a range of neurological conditions including traumatic brain injury (TBI) and multiple sclerosis [Citation8]. The neurobiology of emotionalism is still relatively unknown. Emotionalism can occur as a consequence of both bilateral and unilateral strokes [Citation9]. Emotionalism produces a neurological lessening of the ability to control emotional expression [Citation10] and is believed to arise from lesions to the frontal lobes and descending corticobulbar-cerebellar circuits, which regulate motor control and the co-ordination of emotional expression [Citation11]. Additionally, disruptions to pathways in frontal, parietal and brainstem regions may cause involuntary crying or laughter episodes [Citation12].
Individuals with post-stroke emotionalism (PSE) experience episodes of crying or laughing that occur with little or no warning and which are not under usual social control. Typically, crying outbursts in PSE occur in situations in which the person would not have cried before the stroke or in response to a mildly emotive stimulus [Citation9]. Emotionalism can cause significant distress for the individual, and lead to associated social avoidance and reduced quality of contact with others [Citation13], as individuals with emotionalism fear uncontrollable crying outbursts and an embarrassment associated with these. Research has also suggested PSE can impact rehabilitation efforts with individuals less able to engage with services due to embarrassment or shame due to uncontrolled emotional outbursts [Citation9].
The prevalence of PSE has been found to be high. A systematic review and meta-analysis [Citation14] of 15 PSE prevalence studies found 17% of people with stroke experience PSE acutely, 20% at six-months and 12% beyond six-months. It is thought that approximately 82% of individuals with PSE will experience crying episodes only, 15% experience both crying and laughing episodes and 2% experience laughing episodes only [Citation15]. Research has shown that PSE is associated with high levels of burden and poor outcomes which highlights further research is required to understand the frequency of episodes longitudinally and to explore how individuals experience these episodes. This could help to identify which individuals experience difficulties with emotionalism and who would benefit from psychological intervention.
Emotionalism has been associated with depression and these two conditions have been found to be comorbid with research emphasising factors such as lesion location, social stress and disability caused by stroke playing a role in the development of both these conditions [Citation16]. Calvert et al. studied 448 people with stroke and found 38 had emotionalism and a clinically significant mood disorder [Citation15]. However, there are distinct differences [Citation17] with episodes of emotionalism being usually brief, subjectively uncontrollable and could be triggered by an emotional event rather than an individual’s mood, unlike with depression, where affect is proportionate and consistent with prolonged feelings of sadness [Citation18]. PSE is a disorder of emotional expression rather than emotional experience, so very often individuals will report crying episodes that are exaggerated or incongruent with situational context. Approximately one-third of people with stroke have been found to have depression one-month following their stroke and this remained at this level at nine-months [Citation19]. Research has found that PSE is a risk factor for developing depression following a stroke within the first year [Citation20].
Evidence of the effectiveness of pharmacological interventions has found that antidepressants have only a small positive effect, which is not specific to one drug or class of drugs [Citation21]. Selective serotonin reuptake inhibitors (SSRIs) have been found to reduce the frequency and severity of episodes of emotionalism however, some studies used outcome measures which were unvalidated [Citation22]. Medication can produce unwanted side effects and some people living with stroke may not wish to take medication or may simply prefer non-pharmacological treatments. Currently there are no randomised trials of non-pharmacological treatments and no psychological or behavioural model to understand and formulate PSE. Gillespie et al. investigated the types of non-pharmacological interventions provided by stroke professionals in inpatient stroke settings [Citation23]. They revealed stroke clinicians reported regular use of non-pharmacological interventions with the most common interventions being offering reassurance and talking to patients about their goals. There is therefore, an important gap in the literature whereby further research is required to improve our understanding of why some individuals do worse than others and which psychological or behavioural factors influence their recovery.
Research investigating how people with stroke adjust psychologically to emotionalism after stroke is limited. Taylor et al. [Citation5] adapted the Social Cognitive Transition Model to cancer [Citation24] by adding stroke-specific components developed from the evidence base and clinical practice. The model proposes that an individual’s assumptive world is important in shaping their adjustment following a stroke. If an individual’s assumptive world is rigid, i.e., they do not adjust their beliefs based on new information and the experience of stroke disconfirms certain previously held assumptions, i.e., “I am independent” this may impact on their duration and severity of adjustment distress. Furthermore, an attribution model of illness proposes those who believe that illness chronicity and severity is due to psychological causes express higher levels of distress and poorer psychosocial outcomes [Citation25]. Both these models attempt to explain a way to understand individual differences in post-stroke adjustment emphasising how some individuals may adjust better than others.
To date, however, there is one small scale qualitative study ever progressed to investigate individuals with stroke experiences of emotionalism and how they manage their symptoms. McAleese et al. conducted semi-structured interviews with N = 18 individuals with PSE recruited from inpatient and outpatient stroke settings [Citation26]. They found individuals with negative experiences of PSE described associated social avoidance and embarrassment which impacted their quality of life. Additionally, social support, increased sense of control and optimism were found to increase positive experiences. The sample size was small with participants interviewed at mean/average time of 4.3 months’ post-stroke. There was some consideration of the lived experience of PSE at the acute stage (earliest interview = two-weeks) but none longitudinally, thus little consideration of PSE over time.
Therefore, it is important that larger scale qualitative research is conducted to more fully investigate people with stroke lived experiences of emotionalism to inform whether there is a change over time in individuals’ beliefs or behaviours, whether these perceptions influence the ways that they cope and in turn, how well they recover not only across the acute phase, but also longitudinally, over time. This current study will utilise pre-collected qualitative data from the Testing Emotionalism After Recent Stroke (TEARS) national cohort study which aimed to determine the prevalence and psychological correlates of PSE.
Aims
The current study aimed to explore individual’s experience of PSE and ways of coping. In line with a critical realist approach [Citation27] a further aim was to explain these experiences and common psychological “mechanisms” of emotionalism, causal structures that produce or trigger observable events that we may observe by developing a theoretical client-derived framework.
Research question
span[81]
Methodology
Epistemological perspective
The researcher used a critical realist approach to explore how participants understand and give meaning to their experience of emotionalism. Critical realism holds that there is an objective reality but this is only knowable through a social or subjective lens [Citation28]. As such, this position allowed a focus on investigation of common psychological “mechanisms” with the potential to develop explanatory relationships of a phenomenon or event whilst retaining sensitivity to subjective or social context.
Design
A primary analysis of the qualitative pseudonymised pre-collected semi-structured interview data of the TEARS study was completed as part of a larger national study. Semi-structured interviews gathered information from participants using closed questions as well as exploring their experience of pre-defined aspects of PSE using open questions to allow a focus on “making sense” or understanding the phenomenon [Citation27]. This data was gathered longitudinally, allowing development of a rich, detailed account of the experience of individuals with PSE and how this changes over time.
Ethical approval
Ethical approval for the “Testing for Emotionalism After Recent Stroke” (TEARS) study was granted from Scotland A Research Ethics Committee (reference 14/SS/1103; Integrated Research Application System reference 157483). As the current study is using the TEARS pre-collected data, a non-substantial amendment form was completed and agreed by study sponsor of the TEARS study indicating approval for the researcher’s involvement for the current study. Following this, approval was sought and confirmed from University of East Anglia’s Faculty of Medicine and Health Sciences (FMH) Research Ethics Committee. General Data Protection Regulation (GDPR) approval was granted from University of East Anglia’s Data Protection Information Compliance Specialist.
Anonymised TEARS pre-collected data
This research project used pseudo-anonymised pre-collected data from the TEARS cohort study (Testing Emotionalism After Recent Stroke: NHS Research Scotland Stroke Research Network Identification 18980; https://www.stroke.org.uk/research/understanding-difficulty-controlling-emotions-after-stroke; full protocol from first author). The TEARS study aimed to determine the prevalence, impact, neurological and neuropsychological phenotypes of PSE. This was an observational, longitudinal study of PSE following individuals who experienced a stroke at two-weeks, six-months and 12-months. A total of 277 participants took part in the TEARS cohort study, and 224 of these provided data within two weeks of their stroke, 159 at six-months and 83 at 12-months.
Participants
Participants were recruited within two weeks of stroke from nine acute stroke units in Scotland from October 1st 2015 to September 30th 2018 in the context of a longitudinal post-stroke emotionalism cohort study. The participants were followed longitudinally at two-weeks, six-months and 12-months and all commenced the study at baseline (two-weeks) and either continued or dropped out.
Inclusion criteria for the TEARS study were: (a) clinical diagnosis of ischemic or hemorrhagic stroke (first ever or repeat); (b) written informed consent or informed consent from nearest relative/welfare guardian; (c) male or non-pregnant female over the age of 18. Individuals with aphasia on Frenchay Aphasia Screening Test, a lack of spoken English, severe concurrent medical conditions or with life expectancy ≤ 3 months were excluded, as were individuals with distressing behaviours secondary to stroke/dementia, subarachnoid haemorrhage, other extra axial bleeds or suspected transient ischaemic attack (TIA).
All participants who took part in the TEARS study were eligible for inclusion in the current study however, participants were excluded if they did not consent to their interview being audio recorded. Sample size was determined on how many participants were identified as having emotionalism at each time-point.
Measures
Semi-structured diagnostic interview
The TEARS study interviews were conducted at three time-points; two-weeks, six-months and 12-months following stroke. Interviews were completed face-to-face at two-weeks and six-months and over the telephone at 12-months by pre-trained Scottish Stroke Research Network (SRRN) stroke research nurses. Participants completed a Testing for Emotionalism After Recent Stroke Interview (TEARS-IV) at each time point and the clinical interviews were recorded on an audio recorder. The semi-structured interview was developed based on House diagnostic criteria for PSE including increased tearfulness, crying suddenly with no warning, crying with a lack of control and crying occurring at least once a week [Citation10,Citation15,Citation29]. The interview schedule was developed as part of the national TEARS study designed to determine emotionalism prevalence and develop a psychometric measure of tearful emotionalism following stroke, and this qualitative arm was part of the TEARS study.
The semi-structured interview included both open and closed questions and the interview covered; post-stroke crying screen questions, case characteristics, frequency and impact, post-stroke laughter screen questions, case characteristics and case summary (Supplementary Appendix A). The same questions were asked across all three time-points. The interview included two screening questions whereby if participants answered “no” to both the interview was discontinued by the research nurses as they did not meet the criteria for emotionalism at that time-point. If participants answered “yes” to one or both screening questions the interview continued based on the participant meeting criteria for emotionalism. All participants answered the screening questions as part of the interview at each time-point to determine if emotionalism was absent or present. Examples of the open-ended questions were:
What have your emotions and emotional expression, in particular crying, been like since the stroke?
So, have you changed in any way then? What is that like?
What are the crying episodes actually like? Does the weepiness come suddenly, at times when you aren’t expecting it?
So, for instance, have you been able to stop yourself crying in front of other people? What did you do?
Data analysis plans
Qualitative analysis of the interview data was completed to explore participants’ experience of emotionalism longitudinally. In order to address the primary research questions regarding experience of PSE over time, the analysis involved qualitative content analysis which focused on the meaning of what participants have expressed and to provide an understanding of the phenomenon being investigated, and framework analysis to align the analysis with established frameworks for sense-making. During analysis the researcher therefore adopted a largely inductive approach working exclusively from the participants’ experience when deriving the codes and themes. However, there was also a deductive element as the a priori structuring of questions within the interviews was used to inform the framework analysis, which means that some a priori conceptualisation of psychological constructs was brought into the research process [Citation30].
The interviews were transcribed and the transcriptions were imported to NVivo software [Citation31]. The study followed four main stages of qualitative content analysis as outlined in [Citation32].
Table 1. Stages of qualitative content analysis.
The next stage of analysis involved framework analysis whereby the codes (“meaning units”) and themes from the previous stage of analysis were organised into matrices [Citation33]. The interview questions were also used to shape the framework. The framework was applied to several transcripts that had certain framework themes.
Trustworthiness
The term trustworthiness is the most commonly used criterion to evaluate qualitative analysis and confirms the findings are “worthy of attention” [Citation34]. Conformability refers to the congruence between two or more independent coders. A trainee clinical psychologist (SF) was the lead analyst of the interview transcripts and 25% of the codes were reviewed by a second independent coder (trainee clinical psychologist) to increase the “trustworthiness” of the findings [Citation34]. Initial agreement between coders was 92%. Any discrepancies between coders were resolved through discussions and the revision of code definitions to reduce any overlap between codes and to ensure clarity. The newly revised code framework was reapplied to the transcripts and following this agreement rose to 100%.
Results
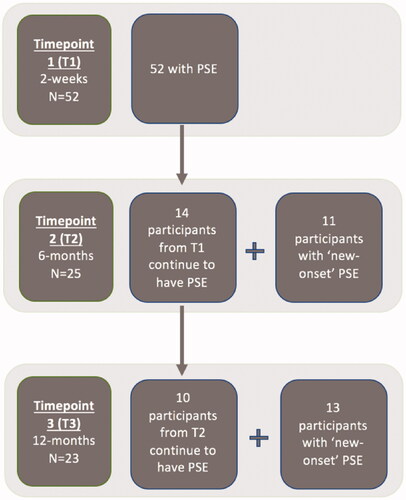
At two-weeks 52 of 62 participants (84%), at six-months 25 of 34 participants (73%) and at 12-months 23 of 27 participants (85%) consented to their interview being recorded thus providing the final included sample. Participants were followed across time-points with a total of 24 participants with PSE across more than one time-point, . Across time-points “new-onset” cases of PSE were identified such as participants who did not have PSE at baseline but did at six-months. At time-point two 14 participants continued to have PSE from time-point one with 11 participants with “new-onset” PSE. At time-point three 10 participants continued to have PSE from time-point two with 13 participants with “new-onset” PSE.
Figure 1. Flow of participants with emotionalism across time-points which shows “new-onset” cases of emotionalism.
The length of interviews ranged from eight minutes to 29 minutes.
Descriptive statistics
The mean age of the sample at two-weeks was 59 and at six-months and 12-months was 57 years. Similar numbers of men and women completed interviews across the time-points apart from at 12-months. The majority of participants left education after secondary school, had an infarct stroke, did not have a prior stroke and had a cortical or sub-cortical lesion location across the time-points. The mean Barthel Index score ranged from 15.7 to 17.25 (Table S1 – Supplementary material).
Research question one: how do individuals with PSE describe their experience of living with PSE?
Three master themes and 15 sub-themes emerged as providing an account of participants’ experience of living with PSE (). The first master theme “In the moment” highlights the experience that participants reported following the initial stages of an episode of emotionalism. The second master theme “Ways of coping” summarises participants’ responses to episodes of emotionalism and ways in which they attempt to regain control. The final master theme “Impact” emphasises the emotional consequences in terms of identity and attempts to make sense of their experiences of PSE.
Table 2. Overview of master themes and sub-themes.
Each major theme is presented with descriptions of each sub-theme whereby codes (“meaning units”) and quotes are outlined. Inter-relationships between themes and sub-themes are discussed in terms of patterns that emerged from analysis. A visual overview of each major theme has also been provided for the reader.
Master theme one: “in the moment”
This theme consists of five sub-themes: characteristics, control versus barriers to control, external triggers, internal triggers, predictability versus unpredictability (Figure S1 – Supplementary material). These capture participants key elements of episodes of emotionalism based on their experience and factors that trigger the onset.
a. Characteristics
Participants described a range of key characteristics of emotional episodes with a build-up of emotions over time, which led to an emotional display.
“I get I suppose just a build-up of emotion I have never really thought about that one I suppose there is a bomb that is going to happen and you have no control at that point,” 036, two-weeks, <59 years, Barthel Index:18.
“I feel it building up in me…I can feel it all bubbling up,” 012, two-weeks, <59 years, Barthel Index:20.
“I can feel it bubbling up” 041, 12-months, >57 years, Barthel Index:20.
Additionally, episodes being incongruent with their feelings at the time led to a discord with participants, which was another frequently reported characteristic.
“I am not feeling sad and I just start crying,” 016, six-months, <57 years, Barthel Index:20.
“When they come on I don’t feel sad before they come on it hits me,” 04, 12-months, >57 years, Barthel Index:14.
“It’s when I have news whether it is good news or bad news I tend to be tearful,” 010, 12-months, >57 years, Barthel Index:20.
The episodes were described by many participants as happening suddenly and lasting a few seconds to minutes.
“It feels as if like someone has a sledgehammer to you and all of a sudden,” 066, two-weeks, <59 years, Barthel Index:20.
“You just have tears for a minute or so and then it stops so its short bursts,” 052, two-weeks, >59 years, Barthel Index:7.
“It is just really for a couple of seconds,” 048, six-months, >57 years, Barthel Index:20.
b. Control versus barriers to control
On one end of a continuum participants described an ability to regulate their episodes of emotionalism once they had released some of their emotion.
“I would say I can after I have got it out somewhat…I can kind of reign it in a little bit,” 054, two-weeks, <59 years, Barthel Index:20.
“I would say probably about a minute…I can manage to do something about it,” 075, two-weeks, >57 years, Barthel Index:18.
Other participants highlighted being able to restrain episodes of emotionalism whereby they could prevent the episode from developing or described a battle to stop the emotions from being displayed.
“I can feel it coming but I stop it so I stop that emotion coming out,” 01, two-weeks, <59 years, Barthel Index:19.
“I could handle it…cos you can I think you can get a grip of yourself,” 022, two-weeks, <59 years, Barthel Index:20.
“What happens is when you feel something like that coming on you try and fight it now,” 052, six-months, >57 years, Barthel Index:7.
In contrast at the other end of the continuum some participants described a battle to control episodes of emotionalism once they had begun.
“I couldn’t control it I tried my best, but I couldn’t” 05, two-weeks, <59 years, Barthel Index:20.
“I find it very difficult at times to control it… it’s terrible what gets you is you can’t control” 010, 12-months, >57 years, Barthel Index:20.
“It’s like you trying to control diarrhea,” 01, 12-months, <57 years, Barthel Index:19.
Episodes occurring out of the blue, i.e., unexpectedly, seemingly coming from nowhere, were frequently reported by most participants as a barrier, which made controlling the episodes difficult or harder to compose themselves.
“I couldn’t hold myself together so for the first couple of days I felt myself very prone to crying than previously which I felt unusual,” 05, two-weeks, <59 years, Barthel Index:20.
“I am just sitting on a bus and before I know it I am starting to cry for no reason at all,” 016, six-months, <57 years, Barthel Index:20.
“It’s just completely out of the blue,” 017, 12-months, >57 years, Barthel Index:20.
Participants highlighted a difference in their ability to control episodes of emotionalism dependent on the intensity of their episodes of emotionalism or the situational context.
“It depends how big the cry is…I have tried but it doesn’t always help,” 020, two-weeks, >59 years, Barthel Index:16.
“Because I couldn’t take myself out of the situation I couldn’t stop myself,” 029, 6-months, <57 years, Barthel Index:19.
“I would say maybe it depends on the circumstances,” 043, 12-months, >57 years, Barthel Index:10.
c. External triggers
Participants described a range of triggers which occurred due to environmental stimuli including; seeing emotional content on the television, others leaving and talking about the stroke.
“Comes on more of when people are going away or leaving me that’s it mostly friends or family it just seems to be when people are going away,” 018, two-weeks, <59 years, Barthel Index:20.
“If I hear anything sad that is definitely a trigger for me I become emotional and I feel for other people,” 06, two-weeks, <59 years, Barthel Index:14.
“If I watch something on the telly that is sad I can feel myself welling up,” 012, six-months, <57 years, Barthel Index:20.
“It is always someone that triggers it,” 060, six-months, <57 years, Barthel Index:6.
“Talking about the stroke because it is hard to talk about…I know it seems so stupid to some people,” 049, 12-months, <57 years, Barthel Index:20.
d. Internal triggers
A variety of internal triggers were highlighted by participants including; thoughts, being reminiscent of losses and remembering past memories.
“Start thinking about things that have happened to you in the past,” 052, two-weeks, >59 years, Barthel Index:7.
“I can be sitting contemplating and thinking,” 063, six-months, <57 years, Barthel Index:10.
“When I am sitting thinking about things and it comes on,” 012, six-months, <57 years, Barthel Index:20.
“I was just thinking of my husband at the time which normally I can think and I am ok,” 010, 12-months, >57 years, Barthel Index:20.
e. Predictability versus unpredictability
Predictability could be seen as on a continuum where some participants described the occurrence of a prior warning to the onset of episodes of emotionalism, the episodes being re-occurring or noticing a pattern.
“I have warning,” 044, two-weeks, <59 years, Barthel Index:5.
“I got myself a bit better and then it goes back again it comes back again as quick as it goes away,” 068, two-weeks, >57 years, Barthel Index:16.
Some participants highlighted how the predictability of their episodes of emotionalism impacted their behaviour such as withdrawing.
“I can wake up and I can know I am going to have a bad day so I tend to just stay in bed,” 041, 12-months, >57 years, Barthel Index:20.
“I would say there is a pattern…because I notice a pattern I take myself completely out of that…I remove myself, 053, 12-months, >57 years, Barthel Index:18.
However, the nature of emotionalism was described by other participants as unpredictable and captured the element of surprise and no prior warning before the emergence of episodes of emotionalism.
“Just like the stroke no warning,” 039, two-weeks, >59 years, Barthel Index:20.
“You are never expecting it,” 052, two-weeks, >59 years, Barthel Index:7.
“It just comes on when I am not expecting it,” 057, two-weeks, >59 years, Barthel Index:5.
“I just find myself surprised that I have tears rolling down my face,” 011, 12-months, <57 years, Barthel Index:20.
A change in the predictability of emotionalism was highlighted by a few participants over time in comparison to how they described their experience at previous time-points. Participants now described noticing a pattern or experiencing a warning before the onset of episodes of emotionalism.
“I sometimes get a warning, I know when it’s coming,” 065, >59 years, Barthel Index:15.
“When I first had my stroke yes (it was out of the blue) but not so much now … I find myself crying getting upset about something that has happened but not just out of the blue, for no reason” 012, <57 years, Barthel Index:20.
“In the last couple of weeks, I would say there is a pattern…I notice a pattern now,” 053, 12-months, >57 years, Barthel Index:18.
Master theme two: “ways of coping’
This theme consists of six sub-themes: acceptance, avoidance of triggers, concealing emotionalism from others, behavioural attempts at symptom management, cognitive attempts at symptom management and support from others (Figure S2 – Supplementary material). “Ways of coping” incorporates the diverse ways that participants described managing episodes of emotionalism as well as help from others in an attempt to discover workarounds to the difficulties the symptoms provoke.
a. Acceptance
This sub-theme highlighted participants recognition of episodes of emotionalism without attempting to change these.
“I just assume it is all part and parcel of what is happening I just assume that is pretty normal,” 054, two-weeks, <59 years, Barthel Index:20.
“I just let them happen, if they are going to happen they are going to happen,” 018, two-weeks, <59 years, Barthel Index:20.
“I just accept it now,” 030, 12-months, >57 years, Barthel Index:Not reported.
Additionally, participants frequently reported attempts to normalise their experience of emotionalism and at times highlighted the benefits of not challenging them.
“Just like my limbs aren’t back to normal my emotions aren’t back to normal,” 05, two-weeks, <59 years, Barthel Index:20.
“I think bringing it out in the open if anything is beneficial to me,” 06, two-weeks, <59 years, Barthel Index:14.
“I just let it out it’s better out,” 07, 12-months, >57 years, Barthel Index:12.
“I kind of expected that see just after the stroke…everyone is different,” 025, 12-months, >57 years, Barthel Index:20.
Participants described optimism regarding their emotionalism in the future and remaining hopeful that these will improve over time.
“I know it is going to be alright,” 034, two-weeks, <59 years, Barthel Index:20.
“I think in time I hope that will change back…as time goes on everything is getting better slowly,” 052, six-months, >57 years, Barthel Index:7.
b. Avoidance of triggers
Within this sub-theme participants frequently reported avoiding specific triggers as an attempt to reduce the onset of episodes of emotionalism such as through sharing limited information with others regarding their feelings or certain topics.
“When I speak to people I try and stay away from certain subjects,” 05, two-weeks, <59 years, Barthel Index:20.
“I wasn’t telling them how I felt,” 040, two-weeks, <59 years, Barthel Index:20.
Additionally, participants described avoiding emotional content that they were aware could trigger their episodes of emotionalism such as films, news, TV programmes or speaking on the phone.
“I would get rid of it if it was something on the telly I would get rid of it,” 035, two-weeks, <59 years, Barthel Index:12.
“She was just telling me something sad and I just had to put my hand up,” 029, six-months, <57 years, Barthel Index:19.
“I have stopped reading papers I don’t watch the news something that comes on there that is sad I just burst into tears it’s awful,” 04, 12-months, >57 years, Barthel Index:14.
“I don’t want to talk to anyone on the phone…sometimes when my family want to speak to me I say I will call them back I put it off as long as possible,” 016, six-months, <57 years, Barthel Index:20.
Avoidance of social situations was also highlighted by participants which was a change from before they had the stroke.
“I used to always talk to people on the buses but now I don’t I just sit ignore everything,” 04, 12-months, >57 years, Barthel Index:14.
“It’s avoiding everything that includes family and everything because I don’t want them to see,” 053, 12-months, >57 years, Barthel Index:18.
c. Concealing emotionalism from others
Participants described an attempt to disguise their emotions or hide their emotions from their family when they experience episodes of emotionalism.
“With a hankie pretending to blow my nose or cough,” 071, two-weeks, >59 years, Barthel Index:20.
“I would just walk away,” 076, two-weeks, <59 years, Barthel Index:20.
“If I have something in my hands I will be using that,” 029, six-months, <57 years, Barthel Index:19.
“I try hide it from the wee one I don’t like it my boy seeing me…I don’t like my Mrs see me,” 027, six-months, <57 years, Barthel Index:18.
“I lock myself in the toilet until I am finished,” 047, 12-months, <57 years, Barthel Index:20.
“I go in the kitchen and take yourself away from it for a wee bit,” 053, 12-months, >57 years, Barthel Index:18.
“If the kids are in and that is happening they will say are you ok I will say aye I have just got a runny nose and a cold,” 03, 12-months, >57 years, Barthel Index:19.
d. Behavioural attempts at symptom management
Participants reported a variety of behavioural strategies that were described as helpful to manage episodes of emotionalism that included breathing and looking away to allow time to pass before returning.
“I breathe in and breathe out…give myself some bursts of breathing in and out,” 016, six-months, <57 years, Barthel Index:20.
“I just have to do some deep breathing and just clear my mind,” 011, 12-months, <57 years, Barthel Index:20.
“Looking away helps when people are asking me things,” 047, 12-months, <57 years, Barthel Index:20.
“I just try and do something completely different,” 051, six-months, >57 years, Barthel Index:20.
e. Cognitive attempts at symptom management
Cognitive strategies incorporated helpful techniques reported by participants that changed their perspective and could be used discreetly without the awareness of others.
“Think of something else you take your mind of it,” 041, two-weeks, >59 years, Barthel Index:20.
“Put things into perspective,” 054, two-weeks, <59 years, Barthel Index:20.
“Try and use my brain and think why am I doing this, I don’t need to do it,” 040, two-weeks, <59 years, Barthel Index:20.
“I tell myself to stop keep saying stop crying stop crying,” 012, six-months, <57 years, Barthel Index:20.
“I will go oh pull yourself together,” 031, six-months, <57 years, Barthel Index:20.
“I try and distract myself,” 047, 12-months, <57 years, Barthel Index:20.
f. Support from others
Participants frequently reported others’ support as helpful when they experienced episodes of emotionalism such as being comforted, reassured, others showing encouragement and emotional assistance. These appeared to assist with reducing participants level of distress.
“He just cuddled me because that is what I felt I needed,” 063, six-months, <57 years, Barthel Index:10.
“Give me a hug and it is fine,” 011, 12-months, <57 years, Barthel Index:20.
“She comes and wipes the tears off my face and cuddles into me,” 027, two-weeks, <59 years, Barthel Index:18.
“They tend to reassure me all the time…they keep saying it is going to be alright,” 01, two-weeks, <59 years, Barthel Index:19.
“Put my mind to ease when they tell me not to worry about these things,” 054, two-weeks, <59 years, Barthel Index:20.
“They come down all the time and they come and see if I am ok,” 031, two-weeks, <59 years, Barthel Index:20.
“I am lucky that I have got friends I just need to phone them and they come up,” 042, six-months, <57 years, Barthel Index:14.
Some participants described instances of others attempts to provide support such as offering empathy which unintentionally exacerbated their emotionalism symptoms.
“When I have cried a kind word from others makes it worse,” 074, 2-weeks, >59 years, Barthel Index:10.
“I have found kindness that has been shown to me…makes me very emotional,” 06, 2-weeks, <59 years, Barthel Index:14.
“If they try and to be nice to me and talk to me it makes it worse,” 012, six-months, <57 years, Barthel Index:20.
Master theme three: “impact”
This theme consists of four sub-themes: changes to self, emotional impact, trying to make sense and uncertainty (Figure 3 – Supplementary material). “Impact” highlights participants’ experience of adjusting to a new experience in terms of their emotional response and how emotionalism affected their sense of identity and their views of the future.
a. Changes to self
Participants highlighted episodes of emotionalism as having been a new experience since the stroke with an emphasis on responding differently in emotional terms than before the stroke which would have not happened before.
“I was battling something that wasn’t very important and I would be very upset and crying where before it would not bother me and I would answer back and stand up for myself more now I am not,” 020, two-weeks, >59 years, Barthel Index:16.
“Everything has changed,” 031, six-months, <57 years, Barthel Index:20.
“It’s not how I would have dealt with it before I would have probably shouted and got it off my chest but now I just find myself…just tears running down my face quietly crying and that definitely isn’t me,” 011, 12-months, <57 years, Barthel Index:20.
“Before the stroke I was quite emotionless,” 047, 12-months, <57 years, Barthel Index:20.
Participants emphasised certain perceptions/beliefs about how they viewed themselves and preconceived gender stereotypical views of displays of emotions. Participants described a process of mean making where some seemed to struggle to make sense of their emotional experience which is at odds with social attitudes they subscribe to or at odds with their own pre-injury relationship to emotion.
“To me I am broken,” 076, two-weeks, <59 years, Barthel Index:20.
“I was a tough cookie I don’t mean that dead hard or cold but I can feel the difference,” 014, two-weeks, <59 years, Barthel Index:18.
“I usually am a tough sort of person,” 04, six-months, >57 years, Barthel Index:14.
“I’m just totally different I was always happy easy go lucky person,” 042, six-months, <57 years, Barthel Index:14.
“I am quite an old school kind of guy… men don’t cry,” 027, 12-months, <57 years, Barthel Index:18.
b. Emotional impact
Participants highlighted a range of feelings that were caused as a consequence of experiencing episodes of emotionalism. The most frequently reported increase in emotions were distress and embarrassment which was emphasised by feeling foolish.
“I find it distressing I shouldn’t be crying,” 021, 12-months, <57 years, Barthel Index:20.
“I find it embarrassing very because I don’t like people seeing me like that you know,” 049, 12-months, <57 years, Barthel Index:20.
“You feel like a complete total idiot to be honest,” 048, two-weeks, >59 years, Barthel Index:20.
“Because I go down the shops and I start crying and everyone is looking at you as if you are daft and I begin to agree with them,” 03, 12-months, >57 years, Barthel Index:19.
c. Trying to make sense
As a result of the episodes of emotionalism following their stroke, participants stressed the importance of ‘trying to make sense’ of their experience by searching for a cause.
“I need explanations…I need a reason for everything,” 076, two-weeks, <59 years, Barthel Index:20.
“I’m just been worried about it and hoping to get some answers,” 038, two-weeks, <59 years, Barthel Index:20.
Participants emphasised the difficulty in explaining their episodes of emotionalism to others, which seemed to be complicated by the issue that participants felt they have not got the answers.
“Very upsetting… you can’t explain it to somebody why you are crying,” 020, two-weeks, >59 years, Barthel Index:16.
“I don’t know what to call what it is…as I don’t know I can’t explain why,” 042, two-weeks, <59 years, Barthel Index:14.
Additionally, participants frequently reported that their episodes of emotionalism did not make sense.
“Well I have wondered what this has been about all this cos I don’t get it,” 035, two-weeks, <59 years, Barthel Index:12.
“They don’t make sense it doesn’t make sense I was feeling ok I was just watching the film with the kids and the next minute the tears were just flowing and I was like huh?,” 03, 12-months, >57 years, Barthel Index:19.
d. Uncertainty
The sub-theme “uncertainty” captured participants concerns about the future in terms of feeling fearful and their descriptions of a battle ahead.
“I think the fear of the unknown,” 07, two-weeks, >59 years, Barthel Index:12.
“Because I don’t want it happening outside or anything,” 025, two-weeks, >59 years, Barthel Index:20.
“It’s just an uphill battle that I have got in front of me,” 039, two-weeks, >59 years, Barthel Index:20.
Participants frequently reported racing thoughts related to the past, current and future.
“I maybe just thinking what is going to happen, what can happen, what has happened,” 028, two-weeks, <59 years, Barthel Index:15.
“Your imagination is running away and it does but when you are lying in here on your own,” 07, six-months, >57 years, Barthel Index:12.
Discussion
To date this is the only study that has explored people with stroke experience of emotionalism, ways of coping and how their experience of emotionalism may change over time using a longitudinal qualitative approach. Overall three major themes were identified: “In the moment” included characteristics, triggers and aspects of control; “Ways of coping” highlighted a variation in participants strategies such as avoidance or acceptance; and “Impact” emphasised longer-term effects of PSE. Over time, some participants described an increased awareness of triggers for episodes of emotionalism which highlighted an element of predictability which may indicate that psychologically there are aspects that enable people to develop better anticipation of their symptoms and adaptive coping strategies.
Strengths and limitations of the study
A key strength of this study was the use of a longitudinal qualitative approach. This has allowed for a rich in-depth exploration of participants’ experiences as well as exploring differences over time. The analysis was summarised into a framework/model which could help inform clinical practice by improving clinicians’ knowledge and earlier detection of distress, embarrassment and beliefs about PSE and shaping future psychological formulations of PSE. Furthermore, this study had a large sample size of N = 100 participants with PSE, which allowed for multiple experiences of PSE to be explored in the analysis of the interview data.
A limitation of this study was the interview schedule was structured so that no interview data could be explored for those who had recovered from emotionalism. This study commenced after the completion of the TEARS cohort study, which meant that the questions to be asked to the participants could not be shaped however, the TEARS interview schedule was devised based on clinical formulation and current literature of emotionalism. To increase the richness of the analysis and add to a proposed model/framework of PSE it would have been helpful to ask questions to participants who had recovered from emotionalism at a subsequent time-point. Further questions for example “what do you feel helped contribute to your recovery of PSE?” could have been added to the interview schedule. Additionally, participants who did not have emotionalism were not asked any further questions across the time-points which meant during analysis the experience of participants with emotionalism were not able to be compared to those without.
The participants in this study were recruited from the West of Scotland with the sample with generally low NIHSS/Barthel scores, few had further education and were in the older age category which highlights potential limitations regarding the generalisability of the findings to individuals for example with aphasia and emotionalism. Reasons for attrition in the TEARS study were difficult to obtain so this could have influenced the data and whether there were any significant differences between the total potential population, those who remained in the TEARS study across time-points and the subsets of participants in this current study. Furthermore, previous research has diagnosed participants with PSE using the PLACS [Citation35] or CNS-LS [Citation36] which has limitations. However, in this study a new measure of the TEARS-IV was used based on House’s criteria [Citation10] and is now validated which has shown high internal consistency and diagnostic accuracy of tearful episodes [Citation37].
Some caution should be taken when interpreting these findings based on the researchers’ epistemological perspective. The experiences of participants were understood within a critical realist perspective whereby some degree of interpretation is needed to provide access to the underlying mechanisms of the data, as although the data is informative of reality this does not simply mirror it [Citation27]. Furthermore, as the data was pre-collected this influenced how the data was analysed as the researcher was unable to collect data from multiple sources, unable to reflect on own experiences of the interviews, certain aspects were already pre-determined such as the interview time-points and in the TEARS study participants were asked factual-type questions about PSE and how it affects them but these questions were designed with a diagnostic focus of emotionalism based on psychological constructs and clinical practice.
When completing qualitative analysis, ensuring codes are reviewed by a second-coder is seen as good practice to increase transparency, promote reflexivity and ensure a systematic approach to coding [Citation38]. Investigator triangulation was completed through the use of a second coder however, this study could have triangulated data sources further by interviewing partners or carers to explore their views to support participants experiences. This could have provided further information regarding changes and ways of coping if participants felt embarrassed or lacked insight into their experience of PSE.
Previous research
Previous research exploring individuals’ experience of emotionalism following a stroke highlighted those with negative experiences reported greater disability and avoidance as well as embarrassment and that social withdrawal had a negative effect on individuals’ quality of life [Citation26]. The current study found participants described avoidance, heightened emotional consequences and negatively held beliefs about episodes of emotionalism which appeared to maintain poor psychosocial outcomes in those with PSE. These findings support the limited qualitative research to date and provides further evidence of ways of coping, beliefs held by individuals and changes over time which is important to shape future psychological interventions. There are no studies showing psychological interventions are efficacious in this population however previous research has shown that clinicians use behavioural/psychological interventions but for which there is currently no evidence base [Citation23]. The application of psychological models requires further investigation through clinical trials, although the themes identified in this current study are useful starting points.
Interpretation of the study findings
Master theme one: “in the moment”
Participants reported a range of internal triggers: thinking about the past, memories, thoughts, feeling sorrowful, reminiscent of losses and external triggers: others leaving, emotional content on the television, seeing family, talking about the stroke, others perceptions, others being unaware and separation from family which led to episodes of emotionalism. Many of the triggers could be objectively considered potentially “moving” and participants themselves highlighted how their responses differed from how they might have reacted pre-stroke. PSE is a neurological condition which is believed to arise due to lesions to the frontal lobes and descending corticobulbar-cerebellar circuits, which regulate motor control and the co-ordination of emotional expression and leads to this change in emotional response as described by participants [Citation11].
A kind word from others was frequently reported by participants as a trigger. Compassion from others often accompanied by the motivation to help [Citation39] was highlighted as both intensifying episodes of emotionalism whilst also described as helpful to feel reassured and comforted. Insight into triggers for emotionalism is valuable to gain further understanding and awareness, which is helpful for clinicians in clinical practice when offering support to individual’s with emotionalism. This could potentially help individuals to anticipate episodes of emotionalism and adapt to these psychologically.
The ability to control episodes of emotionalism varied for participants as well as changing over time for some participants. Locus of control refers to an individual’s belief about the ability to change a situation [Citation40]. Research has shown a relationship between locus of control and recovery from disability and rehabilitation in people with stroke [Citation41]. An individual’s perceptions of their ability to control their circumstances following a stroke is an important factor to consider in an individual’s recovery as they may believe their ability to recover is due to chance or medical staff have control over their condition and this could impact engagement in rehabilitation [Citation42]. Some participants described the ability to control an episode of emotionalism at the onset, which then allowed them to engage in coping strategies. However, participants who highlighted barriers to control emphasised the difficulty to find helpful ways to reduce the emotional intensity. This highlights key information regarding how the ability to control can influence an individual’s perception and action, which would be important to incorporate in future psychological interventions. Increasing an individuals’ internal locus of control is important as if they believe that health is determined by oneself this could positively impact behaviour performance and lead to better health outcomes [Citation43].
Master theme two: “ways of coping”
Avoidance was common across all time-points. Participants frequently reported withdrawing from social interactions, sharing limited information with others and avoidance of emotional content that could trigger episodes of emotionalism. This supports previous research which has found emotionalism can cause distress, embarrassment and social avoidance [Citation13]. Participants highlighted the distress caused by episodes of emotionalism at the onset as well as over time. Calvert et al. found ideas of reference, beliefs of everyday occurrences resulting from individuals’ thoughts or actions and emotionalism were associated with embarrassment potentially interacting in this relationship [Citation15]. The authors explained this association may occur due to the potentially embarrassing nature of emotionalism and socially disabling effects. In the current study, participants highlighted high levels of embarrassment caused by episodes of emotionalism and described how these shaped beliefs individuals held about their experience. Their embarrassment led to beliefs such as “I am a fool” when they were unable to control their episode of emotionalism and they highlighted negative beliefs about others perceptions of them. This emphasises the interaction of levels of distress, embarrassment, avoidance and beliefs about emotionalism whereby earlier detection and intervention could support to break this cycle.
Some participants emphasised the process of acceptance through normalising their experience, remaining optimistic and refraining from attempting to change their emotional response. Acceptance of oneself as intrinsically worthy is central to achieving psychological adjustment following a disability according to the theory of acceptance of disability [Citation44]. Whilst the disability may be considered by the individual as restrictive and a loss they are able to regard the disability as non-evaluative. Additionally, the final stage within a model of adjustment following a stroke highlights the process of acceptance and adjustment of a new reality [Citation45]. This current study supports these models whereby some participants reflected on adjustment and normalising their experience “Just like my limbs aren’t back to normal my emotions aren’t back to normal.” They were able to view their change in emotional responses neutrally without holding negative beliefs about themselves and remained optimistic about the future “As time goes on everything is getting better slowly.” Adjustment to PSE could to some degree be considered alongside adjustment to other consequences of stroke as highlighted in models of adjustment following a disability and Brennan’s [Citation24] adapted Social Cognitive Transition Model [Citation5] which proposes adjustment following a stroke is shaped by an individual’s assumptive world. The participants’ descriptions of their adjustment to PSE in this current study supports these models whereby those with rigid beliefs/perceptions of their displays of emotions highlighted a struggle to make sense of and adjust to their new emotional experience.
Master theme three: “impact”
Participants frequently reported the longer-term impact of emotionalism in relation to changes to self and beliefs they held about their experience. A comparison of the self pre-stroke and post-stroke was emphasised by many participants accompanied with feelings of frustration, distress and hopelessness. Dependency and lack of control following a stroke has been found to contribute to a significant decline in individuals’ self-concept [Citation46]. A stroke can negatively impact an individual’s sense of self and those with a negative self-concept can experience difficulties in making positive adjustments, taking control and accepting any disabilities [Citation47] and could also have implications in terms of rehabilitation. Overall, this current study highlighted participants with a negative experience of emotionalism described avoidance, unhelpful beliefs and a lack of acceptance. These components are important and could be preliminary areas to target in psychological interventions such as CBT or third wave Acceptance and Commitment Therapy (ACT) with individuals with emotionalism [Citation48]. Both of these therapeutic approaches require an engagement with the current potentially distressing reality as a first step and could potentially help to increase insight into triggers of episodes of emotionalism, acceptance of one’s emotional experience, reduce avoidance and help to develop a more compassionate relationship with their experience in the long-term [Citation49]. To date, there is not an evidence-base for the use of psychological therapy with individuals with PSE thus, further research is required before definitive conclusions can be drawn about the efficacy of psychological interventions. CBT has been found to lead to improvements in other stroke populations such as post-stroke anxiety [Citation50] therefore we could postulate that psychological interventions could be helpful for individuals with PSE. However, further development research is needed to build on the present findings before any potential candidate treatment model can be tested to determine feasibility, efficacy and acceptability to patients.
Longer-term consequences were frequently reported by participants trying to make sense of their experience. In the acute phase, participants described a search for an explanation for their episodes of emotionalism and finding it hard to describe to others. Worry and fears for the future were frequently reported with this seen to exacerbate feelings of distress. Uncertainty plays an important role in the rehabilitation of individuals following a stroke [Citation51]. Worry and uncertainty could be seen to feedback into avoidance in participants, which then limits an individual’s opportunity to challenge held beliefs and the consequences of emotionalism. This highlights the requirement for psycho-education regarding emotionalism to be offered in clinical practice to individuals which could help to reduce uncertainty and provide understanding of this condition. This would be in line with National Clinical Guideline for Stroke [Citation52] which recommends the provision of advice to patients/carers after stroke.
Model/framework summarising themes identified from qualitative analysis contributing to a psychological account of the common psychological mechanisms and experience of PSE over time
The qualitative interview data has been summarised into a diagram to visually propose a model/framework to account for the experiences and common psychological mechanisms of PSE described by participants included in this research project ().
This model/framework indicates the onset of episodes of emotionalism as described by participants being triggered by internal or external triggers, which appeared to be considered as “emotionally moving” and differed from how they might have reacted pre-stroke. Neurologically, individuals with emotionalism show greater emotional activity in somatosensory and motor areas to neutral and mildly emotive stimuli which suggests a failed top-down regulatory system [Citation53]. This then led to key elements such as the predictability or unpredictability of the episodes and their perception of self-control.
Following the onset of episodes of emotionalism, participants moved into ways of coping. The gate-control theory proposes disruptions to the corticobulbar/cerebellar pathways or lesions in the frontal lobes may contribute to the development of emotionalism and impact the ability to regulate emotional expression [Citation54]. If participants described an ability to control episodes, they engaged in “in-the-moment” coping behavioural or cognitive strategies. However, participants who felt they had no control or experienced barriers to control described engaging in longer-term coping strategies such as avoidance and concealment. These could be hypothesised as mechanisms that maintain poor psychosocial outcomes in those with PSE and could be reversible maintaining factors targeted through psychological interventions.
Longer-term consequences of emotionalism such as distress and embarrassment may lead to more hypervigilance to PSE episodes in certain people thus, these episodes may appear more frequent or amplified to that individual. Acceptance was highlighted by participants as a helpful coping strategy such as normalising their experience and could be hypothesised as a psychological mechanism which helps with assisting recovery from PSE. This is in line with models of adjustment [Citation5,Citation44] following a stroke whereby participants who were more accepting did not attempt to change their experience but instead adjusted to their new emotional experience without holding negative beliefs about themselves.
Clinical implications
This study was the first to explore experiences of emotionalism over time using longitudinal qualitative methods, which helps to shape further understanding. Participants with negative experiences of emotionalism described high levels of avoidance, negative perceptions, lack of understanding of the condition, distress and embarrassment. Participants who described acceptance of emotionalism described less distress and normalised their experience. These findings help to improve our knowledge of potential mechanisms of emotionalism and inform clinical practice. This research has highlighted that psychological factors affect an individuals’ belief about emotionalism, how they interpret their symptoms and manage episodes of emotionalism. Previous research has revealed emotionalism is under-recognised and under-diagnosed [Citation55]. The current study highlights the clear importance of earlier detection of emotionalism, which could help to support individuals in terms of adaptive coping strategies and challenging negative beliefs. This is important to hopefully prevent maladaptive beliefs/assumptions and in turn, poor outcomes that have been found to be associated with emotionalism.
Recommendations for future research
Further research is needed to explore experiences of individuals who have recovered from emotionalism focusing on aspects of what helped, what changed and barriers to recovery. This could help further our understanding of individuals’ experience of emotionalism and further highlight individuals’ beliefs regarding emotionalism and how this impacts their coping and/or experience. Additionally, further research could test the efficacy of psychological interventions using single-case experimental designs (SCEDs) or randomised controlled trials (RCTs) focused on testing factors relevant to psychosocial outcomes which tentatively emerged from the analysis such as reducing aspects of avoidance, enhancing acceptance of their experience, learning relaxation/mindfulness strategies such as controlled breathing and providing psycho-education to create greater awareness of triggers for episodes of emotionalism. As PSE is a neurological condition, PSE symptoms can continue to occur irrespective of psychological factors but the findings of this study highlight important psychological mechanisms which are crucial for determining individuals with poorer psychosocial outcomes or individuals who do worse because of their interpretations of their symptoms.
Figure S4. Codes and sub-themes within the 'Impact' theme
Download TIFF Image (5.3 MB)Figure S3. Codes and sub-themes within the 'Ways of coping' theme
Download TIFF Image (5.6 MB)Figure S2. Codes and sub-themes within the 'In the moment’ theme
Download TIFF Image (5.1 MB)supplementary-materials.docx
Download MS Word (14.4 KB)Appendices.docx
Download MS Word (27.3 KB)Acknowledgements
We sincerely thank our stroke nurses, Scottish Stroke Research Network and National Health Service Greater Glasgow and Clyde Research and Development colleagues, and all of our Testing Emotionalism After Recent Stroke study participants.
Disclosure statement
There is no conflict of interest. This research was conducted as part of the first authors Doctorate in Clinical Psychology Training at the University of East Anglia (UEA).
Additional information
Funding
References
- Department of Health. 2007. National Stroke Strategy; [cited 2021 Nov 03]. Available from: https://webarchive.nationalarchives.gov.uk/20130105121530/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyandguidance/dh_081062
- Stroke Association. 2018. State of the Nation: stroke statistics; [cited 2021 Nov 03]. Available from: https://www.stroke.org.uk/system/files/sotn_2018.pdf
- Public Health England. 2018. First stroke estimates in England; [cited 2021 Nov 03]. Available from: https://www.gov.uk/government/publications/first-stroke-estimates-in-england-2007-to-2016
- World Health Organisation. 2002. The World Health Report – Reducing Risks, Promoting Healthy Life; [cited 2021 Nov 03]. Available from: https://www.who.int/whr/2002/en/
- Taylor GH, Todman J, Broomfield NM. Post-stroke emotional adjustment: a modified social cognitive transition model. Neuropsychol Rehabil. 2011;21(6):808–824.
- Hackett ML, Pickles K. Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke. 2014;9(8):1017–1025.
- Knapp P, Dunn-Roberts A, Sahib N, et al. Frequency of anxiety after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke. 2020;15(3):244–255.
- Schiffer R, Pope LE. Review of pseudobulbar affect including a novel and potential therapy. J Neuropsychiatry Clin Neurosci. 2005;17(4):447–454.
- Allman P. Emotionalism following brain damage. Behav Neurol. 1991;4(1):57–62.
- House A, Dennis M, Molyneux A, et al. Emotionalism after stroke. BMJ. 1989;298(6679):991–994.
- Engelman W, Hammond FM, Malec JF. Diagnosing pseudobulbar affect in traumatic brain injury. Neuropsychiatr Dis Treat. 2014;10:1903–1910.
- Colamonico J, Formella A, Bradley W. Pseudobulbar affect: burden of illness in the USA. Adv Therapy. 2012;29(9):775–798.
- Allman P, Hope T, Fairburn CG. Crying following stroke: a report on 30 cases. Gen Hosp Psychiatry. 1992;14(5):315–321.
- Gillespie DC, Cadden AP, Lees R, et al. Prevalence of pseudobulbar affect following stroke: a systematic review and Meta-analysis. J Stroke Cerebrovasc Dis. 2016;25(3):688–694.
- Calvert T, Knapp P, House A. Psychological associations with emotionalism after stroke. J Neurol Neurosurg Psychiatry. 1998;65(6):928–929.
- Kim JS, Choi-Kwon S. Poststroke depression and emotional incontinence: correlation with lesion location. Neurology. 2000;54(9):1805–1810.
- Robinson RG, Parikh RM, Lipsey JR, et al. Pathological laughing and crying following stroke: validation of a measurement scale and a double-blind treatment study. Am J Psychiatry. 1993;150(2):286–293.
- Cummings JL, Arciniegas DB, Brooks BR, et al. Defining and diagnosing involuntary emotional expression disorder. CNS Spectr. 2006;11(S6):1–11.
- Townend E, Tinson D, Kwan J, et al. Feeling sad and useless’: an investigation into personal acceptance of disability and its association with depression following stroke. Clin Rehabil. 2010;24(6):555–564.
- Carota A, Berney A, Aybek S, et al. A prospective study of predictors of poststroke depression. Neurology. 2005;64(3):428–433.
- Hackett ML, Yang M, Anderson CS, et al. Pharmaceutical interventions for emotionalism after stroke. Cochrane Database Syst Rev. 2019;(3):CD003690.
- Ahmed A, Simmons Z. Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag. 2013;9:483–489.
- Gillespie DC, Cadden AP, West RM, et al. Non-pharmacological interventions for post-stroke emotionalism (PSE) within inpatient stroke settings: a theory of planned behavior survey. Top Stroke Rehabil. 2020;27(1):15–24.
- Brennan J. Adjustment to cancer – coping or personal transition? Psycho‐Oncol. 2001;10(1):1–18.
- King JB. Illness attributions and the health belief model. Health Educ Q. 1983;10(3–4):287–312.
- McAleese N, Guzman A, O’Rourke SJ, et al. Post-stroke emotionalism: a qualitative investigation. Disabil Rehabil. 2019;43(2):192–200.
- Maxwell JA. A realist approach for qualitative research. Thousand Oaks: Sage; 2012.
- Sayer A. Realism and social science. Thousand Oaks: Sage; 1999.
- Eccles S, House A, Knapp P. Psychological adjustment and self reported coping in stroke survivors with and without emotionalism. J Neurol Neurosurg Psychiatry. 1999;67(1):125–126.
- Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks: Sage; 1998.
- QSR International Pty Ltd. 2020. NVivo; [cited 2021 Nov 03]. Available from: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14.
- Ritchie J, Lewis J, Nicholls CM, et al. (Eds.). Qualitative research practice: a guide for social science students and researchers. Thousand Oaks: Sage; 2013.
- Lincoln YS, Guba EG. Establishing trustworthiness. Naturalistic Inquiry. 1985;289(331):289–327.
- Robinson RG. Treatment issues in poststroke depression. Depress Anxiety. 1998;8(S1):85–90.
- Moore SR, Gresham LS, Bromberg MB, et al. A self report measure of affective lability. J Neurol Neurosurg Psychiatry. 1997;63(1):89–93.
- Broomfield NM, West R, House A, et al. Psychometric evaluation of a newly developed measure of emotionalism after stroke (TEARS-Q). Clin Rehabil. 2021;35(6):894–903.
- O’Connor C, Joffe H. Intercoder reliability in qualitative research: debates and practical guidelines. Int J Qual Methods. 2020;19:160940691989922.
- Singer T, Klimecki OM. Empathy and compassion. Curr Biol. 2014;24(18):R875–R878.
- Rotter JB. Social learning and clinical psychology. Englewood Cliffs: Johnson Reprint Corporation; 1954.
- Johnston M, Morrison V, Macwalter R, et al. Perceived control, coping and recovery from disability following stroke. Psychol Health. 1999;14(2):181–192.
- Lei T-T, Han H-M, Liu X-J. Multiple mediation effects of health locus of control and hope on the relationship between stroke patients’ social support and self-management. Front Nurs. 2020;7(1):49–57.
- Bonetti D, Johnston M. Perceived control predicting the recovery of individual‐specific walking behaviours following stroke: Testing psychological models and constructs. Br J Health Psychol. 2008;13(Pt 3):463–478.
- Dembo T, Leviton GL, Wright BA. Adjustment to misfortune – a problem of social-psychological rehabilitation. Artificial Limbs. 1956;3(2):4–62.
- Wade DT, Langton Hewer R, Skilbeck CE, et al. Stroke: a critical approach to diagnosis, treatment and management. London: Chapman and Hall Medical; 1985.
- Ellis-Hill CS, Horn S. Change in identity and self-concept: a new theoretical approach to recovery following a stroke. Clin Rehabil. 2000;14(3):279–287.
- Hole E, Stubbs B, Roskell C, et al. The patient’s experience of the psychosocial process that influences identity following stroke rehabilitation: a metaethnography. Sci World J. 2014;2014:1–13.
- Kangas M, McDonald S. Is it time to act? The potential of acceptance and commitment therapy for psychological problems following acquired brain injury. Neuropsychol Rehabil. 2011;21(2):250–276.
- Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1–25.
- Kneebone II, Jeffries FW. Treating anxiety after stroke using cognitive-behaviour therapy: two cases. Neuropsychol Rehabil. 2013;23(6):798–810.
- Ni C, Peng J, Wei Y, et al. Uncertainty of acute stroke patients: a cross-sectional descriptive and correlational study. J Neurosci Nurs. 2018;50(4):238–243.
- Intercollegiate Stroke, ICSWP, Bowen A, James M, et al.. National clinical guideline for stroke. (5th ed.). London: Royal College of Physicians; 2016.
- Haiman G, Pratt H, Miller A. Brain responses to verbal stimuli among multiple sclerosis patients with pseudobulbar affect. J Neurol Sci. 2008;271(1–2):137–147.
- Parvizi J, Coburn KL, Shillcutt SD, et al. Neuroanatomy of pathological laughing and crying: a report of the american neuropsychiatric association committee on research. J Neuropsychiatry Clin Neurosci. 2009;21(1):75–87.
- Work SS, Colamonico JA, Bradley WG, et al. Pseudobulbar affect: an under-recognized and under-treated neurological disorder. Adv Ther. 2011;28(7):586–601.