Abstract
Purpose
To determine the feasibility, safety and preliminary effectiveness of preoperative functional high-intensity interval training (f-HIIT) for high-risk patients undergoing LSF.
Materials and methods
High-risk patients eligible for elective 1–3 level LSF were included. Feasibility and safety of the preoperative f-HIIT program was determined by measuring participation and attrition rates, training adherence, adverse events, reached training intensity and preoperative progression in physical fitness. Preliminary effect of the preoperative f-HIIT program was estimated on time to postoperative functional recovery and length of hospital stay (LoS) between high-risk patients who did and did not participate in the prehabilitation program.
Results
Eleven out of 23 high-risk patients opted to participate in the f-HIIT program, which was safe and feasible, as no adverse events occurred and only one out of 74 sessions was missed (1.4%). Trained high-risk patients improved their physical fitness with 21.2% on average and obtained faster time to functional recovery compared to matched untrained patients (median 4.5 vs 7.5 days; p = 0.013). No effect was seen on LoS (median 7 vs 8 days (p = 0.58)).
Conclusions
The preoperative f-HIIT program is feasible, safe and shortened time to postoperative functional recovery in patients who underwent LSF.
Preoperative high-intensity interval training is safe and feasible for high-risk patients opting for lumbar spinal fusion.
In a relatively small sample the study shows preoperative high-intensity interval training could reduce time to functional recovery in high-risk patients opting for lumbar spinal fusion.
Implications for rehabilitation
Introduction
Undergoing lumbar spinal fusion (LSF) is associated with a risk of (temporarily) decreased functioning, morbidity and mortality [Citation1]. Patients undergoing LSF are at various stages of deconditioning due to their chronic back pain restraining physical activities, resulting in large interindividual differences in risks for these negative outcomes [Citation2]. Patients who are less deconditioned have a higher physiological reserve, which is a prerequisite for withstanding surgical stress and achieving satisfactory postoperative outcomes [Citation3]. Consequently, patients who are more deconditioned (i.e., have a lower physiological reserve) are more at risk for negative postoperative outcomes. These so-called “high-risk” patients could benefit from preoperative exercise training to improve their physiological reserve [Citation3]. Preoperative high intensity interval training (HIIT) for high-risk patients is an effective intervention for improving postoperative outcomes of high-risk patients in different types of major surgery, such as total hip and knee replacement [Citation4,Citation5], elective cardiac surgery [Citation6] and elective oncological surgery [Citation7]. Studies on prehabilitation in LSF mainly focused on low-risk patients and cognitive behavioural therapy, and showed inconclusive results [Citation8]. Research on the effect of preoperative exercise training of high-risk patients opting for LSF is lacking. However, training frail and deconditioned patients might prove difficult, as for these patients exercise training, especially in a high intensity mode seems quite be contra-intuitive as many may think that there are health risks are involved with high-intensity training. Moreover, training should be functional and community-based, as training tasks specific to a patient’s context will accomplish more sustainable results [Citation7]. Therefore, the primary objective of this pilot study was to investigate if a preoperative functional high-intensity interval training (f-HIIT) program was feasible and safe for high-risk patients undergoing elective LSF. The secondary objective was to investigate the feasibility of participating in the risk stratification and f-HIIT program procedures. The third objective was to explore the preliminary effect of the preoperative f-HIIT program on functional recovery and length of hospital stay (LoS) of high-risk patients undergoing elective LSF.
Materials and methods
Study design
From February 2017 onwards, as part of standard care, patients scheduled for elective LSF underwent a preoperative risk screening. This population was used to determine baseline levels of the outcome and provide control patients for analysing preliminary effectiveness. From November 2018 onwards, the preoperative f-HIIT program became part of standard care and was offered to all high-risk patients undergoing LSF. Data on patients undergoing LSF until February 2020 was collected and analysed prospectively. The STROBE statement and CONTENT scale for therapeutic validity were used as reporting guidelines. The study was assessed by the local ethics committee and was considered not applicable to the Medical Research Involving Human Subject (WMO) Act (case numbers 2020-1838, 2019-1426).
Population
Patients were included if they underwent a preoperative risk screening after they opted for elective one to three level LSF surgery between February 2017 and January 2020. Inclusion criteria were: ≥18 years old patients diagnosed with a degenerative disorder of the lumbar spine. Degenerative disorders of the lumbar spine were defined as: degenerative disc disease, spondylosis, spondylolysis/-olisthesis, spinal stenosis, adjacent level disease, post- herniotomy, post-laminectomy or (recurrent) disc herniation. Patients were excluded from the analysis if they had undergone LSF previously, had to undergo acute LSF, had cognitive or psychiatric disorders which would make them unable to undergo the preoperative screening or prehabilitation program.
Risk assessment
To identify a patient’s risk level (high or low risk) and level of deconditioning, all patients underwent a preoperative screening assessing their physical capacity four to six weeks before surgery. This preoperative risk screening was performed at a single university hospital by a hospital physiotherapist with experience in treating patients undergoing LSF (T0) () and consisted of tests for: aerobic capacity (steep ramp test (SRT)), muscle strength of the lumbar spine (Sorensen test), lumbar movement control (sitting one leg knee extension, posterior pelvic tilt, waiter’s bow and the one leg stance test), flexibility (finger-floor distance) and functional status (Timed Up and Go (TUG) and Morton Mobility Index (DEMMI)). High-risk patients were identified when the SRT performance was <2.5 Wpeak/kg.Footnote1
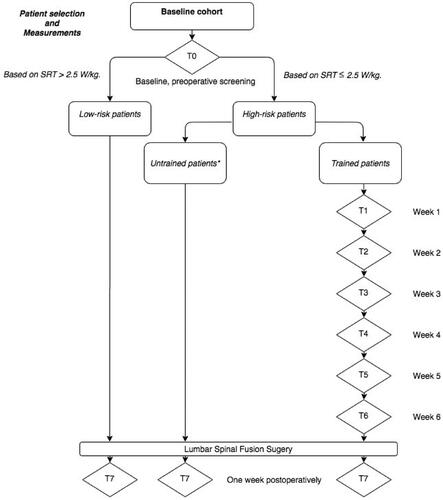
Figure 1. Flowchart of measurement time points (diamonds) of trained and untrained patients opting for 1–3 level lumbar spinal fusion surgery. SRT: Steep Ramp Test; T: time point.
Trained patients
From November 2018 onwards all high-risk patients were offered a preoperative f-HIIT program as part of standard care. This preoperative training consisted of a maximum of eight community-based training sessions of thirty minutes, guided by a trained primary care physiotherapist. The physiotherapists who guided the program had completed a three-day training course on f-HIIT prehabilitation. Each guided training session consisted of a five-minutes low to moderate intensity warm up phase, followed by 25 min of high intensity patient-specific functional interval training. Exercises during the training were modified to the patient’s individual needs and deficits elicited in the preoperative screening, based on the principles of functional home training described by Fleuren et al. [Citation9]. Examples of performed exercises are: intermittent walking exercises, stair climbing, cycling or repetition of transfers. Training intensity was monitored and adjusted using the BORG Rating of Perceived Exertion Scale (BORG RPE on a 0-10 scale) [Citation10] and heart rate (in beats per minute). Adequate intensity was achieved at a BORG RPE ≥7 and/or 90% of maximum heart rate (HR) (208-(0.7*age)) [Citation10,Citation11]. Next to the supervised sessions, patients were instructed to incorporate functional exercises into their everyday life. If patients did not make progress, their physical therapists would discuss this in their follow up session, adjust the training and increase the frequency of assessment of progression up until progression is again obvious from these assessments [Citation12]. Training progression was monitored weekly () by the physiotherapist using: the two-minute walk test (2MWT) [Citation13], TUG [Citation14] and 30-s chair-stand test (30CST) [Citation15]. The SRT was measured at screening (T0) and in the last week of training (T6) by the hospital physiotherapist to measure changes improvements in physiological reserve.
Usual care
High-risk patients undergoing LSF before November 2018, patients who opted not to train and all low-risk patients received usual care. Data from high-risk patients undergoing LSF before November 2018 were used as a control group in the effectiveness analysis. Preoperative usual care included: information about the surgery and advice to stay physically active. Postoperative care was the same for both the trained and untrained patients. They received daily postoperative physiotherapy sessions during hospitalization. Physiotherapy after discharge was not recommended. Measurements in the untrained patients were performed at the preoperative screening (T0), by the hospital physiotherapist ().
Outcome measurements
Postoperative time to functional recovery was measured using the modified Iowa Level of Assistance Scale (mILAS) [Citation16]. This instrument was scored daily during hospitalization by a physiotherapist to score the degree of independent functioning of a patient. Five functional tasks are scored on this scale: supine to sit, sit to supine, sit to stand, transfer, walking and stair climbing. Each task was scored on a five-point scale whereby the sum score zero (or six in case the patient does not have stairs at home) meant the patient was recovered. LoS was defined as the number of days until discharge from the hospital, starting at the day of surgery.
Statistics
SPSS, Version 25.0 (IBM Corp. Released 2017. IBM SPSS Statistics. Armonk, NY: IBM Corp.) and R (version 3.3.2; http://www.r-project.org) were used for statistical analysis. A p-value of <0.05 was considered statistically significant. Patients were excluded from the analysis if they had missing data on the outcomes.
Feasibility f-HIIT for high-risk patients
Safety of the preoperative f-HIIT program was evaluated by the registration of the number of adverse events during the preoperative training period. Feasibility was assessed through adherence to the program by number of guided sessions missed, the maximum training intensity reached during the guided sessions and the progress of physical fitness made during the preoperative training period. Feasibility participation in the f-HIIT into clinical practice.
Feasibility of participation of the risk stratification procedure was evaluated by calculating the attrition rate for screening and for risk stratification. Moreover, the participation rate for the f-HIIT program after implementation was calculated.
Preliminary effectiveness
Preliminary effectiveness was measured by 1) calculating mean-differences between matched trained and untrained high-risk patients, and 2) an interrupted time series analyses (ITSA) before and after implementation of the f-HIIT program, on time to functional recovery and LoS. An independent samples t-test, or its non-parametric equivalent a Mann–Whitney U test, was used for calculating mean-differences. Untrained high-risk patients from the cohort up to November 2018 were used as a control group and matched with trained patients, using Propensity Score Matching based on a patient’s age, American Society of Anaesthesiologists (ASA) score, preoperative pain score (Visual Analogue Scale, VAS) and smoking status (smoker/non-smoker). These variables were identified in literature as potential confounding factors and thus required correction through propensity score matching [Citation17]. ITSA was used to demonstrate the impact of implementation of the preoperative f-HIIT program on time to functional recovery and LoS. Here, differences in results before and after implementation are compared using a regression analysis correcting for secular trends [Citation18]. For ITSA we assumed a level change (relative risk reduction) to occur when the f-HIIT program was implemented without lag (no transition period) [Citation18]. No slope change was expected to occur. This assumption was based on results from a previous pilot study [Citation19]. The ITSA was applied in the matched high-risk population to show the effect of prehabilitation in a real-world setting.
Results
During the study period a total of 183 patients opting for LSF entered the clinic of which 135 patients could be stratified into risk profiles, from which 46 were identified as high-risk and 89 as low-risk (). Baseline characteristics and pre-operative physical fitness levels of both risk groups can be found in . After implementation of the preoperative f-HIIT program in November 2018 eleven out of 23 high-risk patients opted to undergo prehabilitation. Of the eleven trained patients six patients had a cardiovascular disease, five had a pulmonary disease, one had diabetes mellitus type II, one had kidney failure and. Five out of eleven patients used some type of blood pressure regulating medication.
Figure 2. Flowchart of the in- and exclusion of patients. LSF: lumbar spinal fusion. *Outliers were defined as any value that is more than 1.5 IQR below the first quartile or above the third quartile.
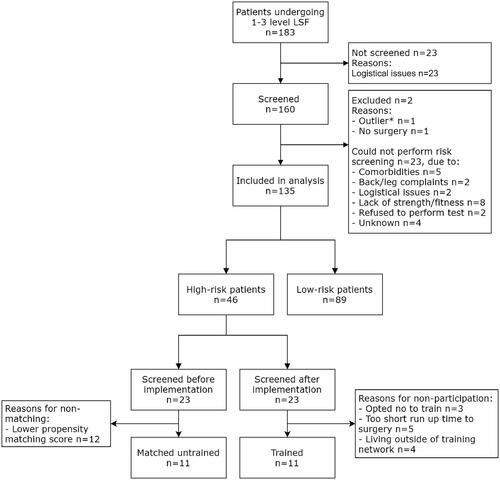
Table 1. Baseline characteristics for high-risk and low-risk patients undergoing elective level one to three LSF.
Feasibility f-HIIT for High-Risk patients
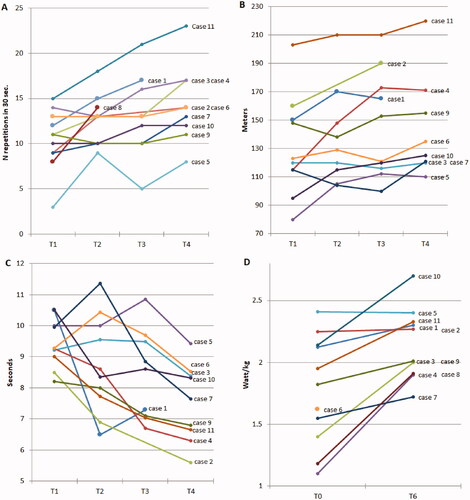
None of the eleven patients who participated in the preoperative f-HIIT program dropped out (0.0%). Patients took part in six preoperative supervised training sessions on average, only 1/74 sessions were missed (1.4%), due to an unrelated illness. Based on the BORG RPE-score, on average patients reached adequate training intensity in 71.2% of the supervised sessions. Based on 90% maximum HR 0.0% reached adequate training intensity. All patients showed improvements in preoperative physical fitness on at least two out of four tests (TUG, 2MWT, 30CST and SRT) during the preoperative training period, see . On average patients improved 32.9% on the TUG, 22.4% on the 2MWT, 48.27% on the 30CST and 21.2% on the SRT.
Figure 3. (a–d) Per patient progression on: a) the 30 s Chair Stand Test, b) the 2 min Walk Test and c) the Timed Up and Go test between week 0 and 4 of training, and d) per patient progression on the Steep Ramp Test between week 0 of training and directly preoperatively.
Feasibility implementation f-HIIT into clinical practice
The attrition rate for screening was 0.89 (158/178), twenty patients did not undergo risk screening, due to logistical reasons. Attrition rate for risk stratification was 0.84 (135/158), as 23 patients did not perform the SRT. Participation rate for training was 0.48 (11/23). Twelve patients did not train, due to: opted not to train (n = 3), run-up time to surgery was too short (n = 5) and they lived outside of the catchment area of the training network of physiotherapists (n = 4).
Preliminary effectiveness
Trained and untrained high-risk patients were matched on their propensity score to correct for important confounders when assessing effectiveness. As a result, matched trained and untrained cohorts did not differ on baseline characteristics (p = 0.11–1.00, see ). The median (IQR) time to functional recovery for the trained group was 4.5 (3–6) days and for the matched untrained group was 7.5 (5.75–12.5) days (p = 0.01) (). The median LoS (IQR) for the trained group was 7 (6–11) days and for the untrained group 8 (6–13) days (p = 0.58) ().
Figure 4. (a and b) A boxplot comparing the trained and untrained high-risk patients on postoperative: a) time to functional recovery and b) length of hospital stay.
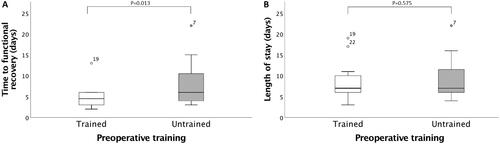
Table 2. Baseline characteristics for high-risk patients undergoing elective level one to three LSF.
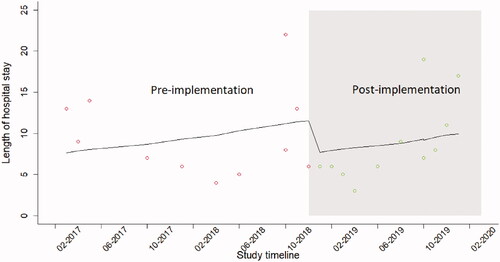
The effect (expressed as a relative risk (RR)) of implementation on the preoperative f-HIIT program on time to functional recovery was: RR = 0.54 (95%CI:0.32–0.92, p = 0.02) in the Propensity Score matched high-risk population (). RR = 0.65 (95%CI:0.41–1.03, p = 0.07) in the Propensity Score matched high-risk population ().
Figure 5. Effect of implementation of preoperative f-HIIT program on time to functional recovery (in days) in the matched high-risk population (n = 22).
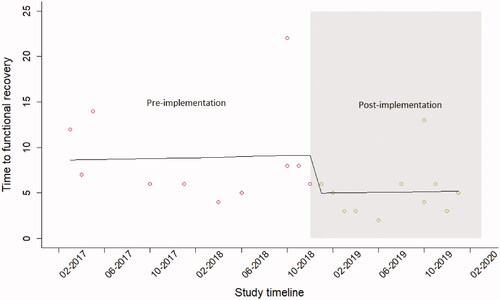
Figure 6. Effect of implementation of preoperative f-HIIT program on length of hospital stay in the matched high-risk population (n = 22).
Discussion
The current pilot study demonstrated that preoperative community-based f-HIIT is feasible and safe for high-risk patients opting for elective 1–3 level LSF. No adverse events occurred and only one (1.4%) supervised training session was missed. High-intensity was achieved in most training sessions (71.2%) according to the BORG RPE, but not according to the maximum HR (0.0%). All trained patients showed progression during their preoperative training period, although results fluctuated. Implementation of the pre-operative screening and risk stratification was feasible (92.1% and 91.4% attrition rates). However, participation in the f-HIIT program could be improved, as only 47.8% of eligible high-risk patients were trained, mainly caused by the limited catchment area and logistic issues with surgical planning. Finally, preoperative f-HIIT may be able to shorten time to functional recovery in high-risk patients undergoing LSF.
Prehabilitation can be applied to improve outcomes after major surgery, such as LSF, by mitigating pre-existing deconditioning as a risk factor for worse postoperative outcome. A recent systematic review concluded that most studies on preoperative interventions before LSF show inconclusive results [Citation8]. The marginal benefits could be caused by the inclusion of both high- and low-risk patients. Low-risk patients are likely to benefit less from undergoing preoperative training, as they do not suffer from pre-existing deconditioning. This was confirmed in our results, as low-risk patients had a significantly shorter time to functional recovery than high-risk patients in the total population (p = 0.005). Previously, two research groups investigated a preoperative exercise training program in patients undergoing spinal surgery [Citation20–22]. Both interventions were largely similar to our intervention, as all applied a personalized prehabilitation program provided by a trained physiotherapist. However, their intervention differed from ours since they did not apply a preoperative risk screening identifying high-risk patients [Citation21,Citation22]. Moreover, neither of the studies described a high-intensity interval training (HIIT). HIIT is be preferred over other types of exercise therapy since it elicits overload which results in benefits on physical functioning within a very short time span, making it very time-efficient in a preoperative period [Citation23,Citation24]. Moreover, its effectiveness is established in other prehabilitation programs before major surgery [Citation23,Citation24].
Our prehabilitation program is likely to be cost-effective in clinical practice. Although we did not analyse cost-effectiveness the overall cost of physiotherapy, hospitalization and complications are well-described in the Dutch costing-manual, used for economic evaluations [Citation25]. The average cost of a day of hospitalization in the Netherlands is approximately 500 euro per day. Whilst the cost of prehabilitation is approximately 264 euro per high-risk patient (based on eight physiotherapy sessions) and the screening cost by a physical therapist is approximately 66 euro per patient. Therefore, the extra cost per high-risk patient, taking into account that three patients need to be screened to identify one high risk patient is 330 euro. One day of hospitalization costs 476 euro. Based on these calculations one would save 146 euro per patient, based on the reduction of hospital length of stay by a single day. Therefore, based on our preliminary results prehabilitation is likely to be cost-effective program.
Study limitations
The results of this study are aimed at, exploring the potential effectiveness of prehabilitation in LSF, improving the intervention for a larger scale study and aiding other hospitals in the implementation of similar strategies. Some limitations were apparent in this study. The f-HIIT program was a new method of training in a specific population for the local network of physiotherapists. Although all physiotherapists followed a three-day training course on f-HIIT prehabilitation, it is likely that a learning curve may have influenced the efficacy of training and its intensity [Citation26]. Secondly, using LoS as an outcome measure for recovery after surgery is debatable, since it is highly dependent on external factors other than functional (e.g., logistics, planning) or medical recovery alone [Citation27]. This could explain the lack of effect of the prehabilitation intervention on LoS. Thirdly, the process of selecting controls via matching is based on known confounding factors from a previously published prediction rule for postoperative success chance [Citation17]. This means our results were controlled for likely confounders and thereby are less prone to confounding bias, similar to a randomized controlled trial (RCT). However, a larger sample size is a prerequisite for valid conclusions on population effects. A strength of this pilot study was the pragmatic design whereby the inclusion of the patients was based on real-life practice and detailed data was collected from individual cases to evaluate their response to training. This is an advantage over RCTs, as evidence reflects real-life variation and facilitates implementation into clinical practice [Citation28].
Recommendations
Preoperative exercise training provides patients and surgeons with feasible and safe means for reducing the risk of negative surgical outcomes. Long-term effects (e.g., long-term recovery rate, quality of life and pain) in a more representative population still need to be investigated. Recommendations for research are that 1) the risk stratification method should be validated externally, 2) surgical planning should be optimized to allow for preoperative screening and training, and 3) participation rates should be improved by enlarging the catchment area of physiotherapists providing prehabilitation.
Conclusions
The current study showed that a preoperative f-HIIT program is feasible and safe for high-risk patients undergoing 1–3 level elective LSF. Implementation of the preoperative f-HIIT program into clinical practice can and should be optimized by improving surgical planning and enlarging the prehabilitation catchment area. The preoperative f-HIIT program shortened time to functional recovery in our patient population.
Disclosure statement
The authors report no conflicts of interest
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, EJ. The data are not publicly available due to restrictions e.g., their containing information that could compromise the privacy of research participants.
Notes
1 Based on univariate logistic regression analysis of the first 80 patients who underwent the screening a cut-off point was calculated to determine which patients were at risk for delayed inpatient recovery (>4 days). Associations between physical fitness tests of the preoperative screening and postoperative inpatient functional recovery were calculated using univariate logistic regression. The SRT was the only variable with discriminative ability for prolonged functional recovery (high-risk) or normal functional recovery (low-risk) (p = 0.002). A patient could be identified as high-risk when the SRT performance was <2.5 Wpeak/kg (AUC = 0.75, sensitivity = 0.83, specificity = 0.54), emphasizing sensitivity to not miss any high-risk patients.
References
- Carli F, Scheede-Bergdahl C. Prehabilitation to enhance perioperative care. Anesthesiol Clin. 2015;33(1):17–33.
- Phillips FM, Slosar PJ, Youssef JA, et al. Lumbar spine fusion for chronic low back pain due to degenerative disc disease: a systematic review. Spine (Phila Pa 1976). 2013;38(7):E409–22.
- Santa Mina D, Clarke H, Ritvo P, et al. Effect of total-body prehabilitation on postoperative outcomes: a systematic review and meta-analysis. Physiotherapy. 2014;100(3):196–207.
- Ibrahim MS, Khan MA, Nizam I, et al. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med. 2013;11:37.
- Swank AM, Kachelman JB, Bibeau W, et al. Prehabilitation before total knee arthroplasty increases strength and function in older adults with severe osteoarthritis. J Strength Cond Res. 2011;25(2):318–325.
- Hulzebos EH, Smit Y, Helders PP, et al. Preoperative physical therapy for elective cardiac surgery patients. Cochrane Database Syst Rev. 2012;11:CD010118.
- Berkel AEM, Bongers BC, Kotte H, et al. Effects of community-based exercise prehabilitation for patients scheduled for colorectal surgery with high risk for postoperative complications: results of a randomized clinical trial. Ann Surg. 2022;275(2):e299-e306.
- Janssen ERC, Punt IM, Clemens MJ, et al. Current prehabilitation programs do not improve the postoperative outcomes of patients scheduled for lumbar spine surgery: a systematic review with Meta-analysis. J Orthop Sports Phys Ther. 2021;51(3):103–114.
- Fleuren MAH, Vrijkotte S, Jans MP, et al. The implementation of the functional task exercise programme for elderly people living at home. BMC Musculoskelet Disord. 2012;13(1):128.
- Scherr J, Wolfarth B, Christle JW, et al. Associations between borg's rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol. 2013;113(1):147–155.
- Scheid JL, O’Donnell E. Revisiting heart rate target zones through the lens of wearable technology. ACSMs Health Fit J. 2019;23(3):21–26.
- Glasziou P, Irwig L, Mant D. Monitoring in chronic disease: a rational approach. BMJ. 2005;330(7492):644–648.
- Unnanuntana A, Ruangsomboon P, Keesukpunt W. Validity and responsiveness of the two-minute walk test for measuring functional recovery after total knee arthroplasty. J Arthroplasty. 2018;33(6):1737–1744.
- Podsiadlo D, Richardson S. The timed "up & go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148.
- Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119.
- Elings J, Zoethout S, Ten Klooster PM, et al. Advocacy for use of the modified Iowa level of assistance scale for clinical use in patients after hip replacement: an observational study. Physiotherapy. 2019;105(1):108–113.
- Janssen ERC, Punt IM, van Kuijk SMJ, et al. Development and validation of a prediction tool for pain reduction in adult patients undergoing elective lumbar spinal fusion: a multicentre cohort study. Eur Spine J. 2020;29(8):1909–1916.
- Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355.
- Heldens AF, Bongers BC, de Vos-Geelen J, et al. Feasibility and preliminary effectiveness of a physical exercise training program during neoadjuvant chemoradiotherapy in individual patients with rectal cancer prior to major elective surgery. Eur J Surg Oncol. 2016;42(9):1322–1330.
- Lindbäck Y, Tropp H, Enthoven P, et al. PREPARE: presurgery physiotherapy for patients with degenerative lumbar spine disorder: a randomized controlled trial. Spine J. 2018;18(8):1347–1355.
- Nielsen PR, Andreasen J, Asmussen M, et al. Costs and quality of life for prehabilitation and early rehabilitation after surgery of the lumbar spine. BMC Health Serv Res. 2008;8:209.
- Nielsen PR, Jørgensen LD, Dahl B, et al. Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil. 2010;24(2):137–148.
- Bongers BC, Dronkers JJ, Hulzebos EH, et al. Optimizing perioperative physical therapy care in major elective surgery to improve surgical outcome in high-risk patients: the better in, better out™ concept. Nederlands Tijdschrift Voor Anesthesiologie. 2016;29(6):134–139.
- Grootswagers P, de Regt M, Domić J, et al. A 4-week exercise and protein program improves muscle mass and physical functioning in older adults – a pilot study. Exp Gerontol. 2020;141:111094.
- Tan SS, Bouwmans CA, Rutten FF, et al. Update of the dutch manual for costing in economic evaluations. Int J Technol Assess Health Care. 2012;28(2):152–158.
- Schlachta CM, Mamazza J, Seshadri PA, et al. Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum. 2001;44(2):217–222.
- Elings J, van der Sluis G, Goldbohm RA, et al. Development of a risk stratification model for delayed inpatient recovery of physical activities in patients undergoing total hip replacement. J Orthop Sports Phys Ther. 2016;46(3):135–143.
- Schork NJ. Personalized medicine: time for one-person trials. Nature. 2015;520(7549):609–611.
