Abstract
Purpose
Primary progressive aphasia (PPA) is a language-led dementia associated with Alzheimer’s pathology and fronto-temporal lobar degeneration. Multiple tailored speech and language interventions have been developed for people with PPA. Speech and language therapists/speech-language pathologists (SLT/Ps) report lacking confidence in identifying the most pertinent interventions options relevant to their clients living with PPA during their illness trajectory.
Materials and methods
The aim of this study was to establish a consensus amongst 15 clinical-academic SLT/Ps on best practice in selection and delivery of speech and language therapy interventions for people with PPA. An online nominal group technique (NGT) and consequent focus group session were held. NGT rankings were aggregated and focus groups video recorded, transcribed, and reflexive thematic analysis undertaken.
Results
The results of the NGT identified 17 items. Two main themes and seven further subthemes were identified in the focus groups. The main themes comprised (1) philosophy of person-centredness and (2) complexity. The seven subthemes were knowing people deeply, preventing disasters, practical issues, professional development, connectedness, barriers and limitations, and peer support and mentoring towards a shared understanding.
Conclusions
This study describes the philosophy of expert practice and outlines a set of best practice principles when working with people with PPA.
Primary progressive aphasia (PPA) describes a group of language led dementias which deteriorate inexorably over time.
Providing speech and language therapy for people with PPA is complex and must be person centred and bespoke.
This study describes the philosophy of expert practice and outlines a set of best practice principles for speech and language therapists/pathologists working with people with people with PPA.
Implications for rehabilitation
Introduction
Primary progressive aphasia (PPA) is a rare dementia syndrome associated with slow and continuous decline of language function. Individuals with PPA present with difficulties in speech and language on an initial background of no, or few cognitive impairments [Citation1]. The condition affects around three in 100 000 people [Citation2,Citation3]; however, the true prevalence is difficult to determine due to heterogeneity of the underlying pathologies [Citation4–7]. As there are currently no curative treatments for PPA, the condition progresses relentlessly over time. In the later stages of the condition, symptoms evolve towards a more global dementia presentation and changes in episodic motor function, memory, behaviour and personality may emerge, overlapping with other dementia syndromes [Citation8–10]. Speech and language therapists/pathologists (SLT/Ps), have worked for many years with people with PPA, albeit typically in small numbers. Multiple interventions have emerged as being well-suited to ameliorate the impact of PPA [Citation11–14]. It remains unclear which interventions are most effective or most important to consider at different stages of the condition. As such, a gap in knowledge exists that increases the difficulties clinicians face when making management decisions.
The impact of primary progressive aphasia
The impact for those living with PPA and their families can be devastating and all-consuming. PPA has a profound effect, not only on communication itself (see Gorno-Tempini [Citation1] for an overview of diagnostic criteria and Etcheverry et al. [Citation15] for case examples), but also on participation in everyday activities (see O’Connor et al. [Citation16] for a theoretical overview; Bier et al. [Citation17] for case examples), quality of life and mood [Citation18,Citation19], relationships and families [Citation20,Citation21], and on carer wellbeing and finances [Citation22–24]. Provision of high quality, evidence-based care which is responsive, efficient, and provides ongoing and dynamic support, both for communication and the wider consequences of living with PPA, is therefore critical for people living with the condition and their families [Citation24,Citation25].
Continuum of care and SLT/P role
The needs of individuals living with PPA and their families change over time as the condition evolves, requiring ongoing and long-term support that remains dynamic and relevant to the individual. Phased treatment models, alongside case examples, have been proposed to assist people with PPA to functionally communicate and participate as successfully as possible for as long as they can; adjusting the focus of treatment and support in response to the progression and evolution of the clinical presentation over time [Citation26–28]. Given that communication difficulties are the most prominent symptoms experienced by people with PPA in the early and mid-stages of disease, SLT/Ps play a central role in the care pathway, supporting individuals and their families, both at the time of diagnosis, and across the continuum of care. Surveys completed in Australia, Germany, and the UK have, however, revealed variability and limitations in SLT/P service provision [Citation29–31]. A range of factors influence service delivery including: (i) awareness of the SLT/P role by potential referring parties, (ii) SLT/P knowledge and confidence in managing PPA, and (iii) the availability of funding to offer proactive and long-term services (or even the complete lack of funding or contractual arrangements for PPA within SLT/P services) [Citation29–31].
Management options
Knowledge of which interventions is most appropriate for managing PPA at a particular stage or context requires an understanding of the progressive and evolving nature of PPA, as well as consideration of other critical factors (e.g., environmental, personal, value-based variables) that influence person-centred management decisions [Citation26,Citation32]. Many of the interventions used in PPA have been adapted from the stroke-induced aphasia field and will be familiar to clinicians. In other instances, SLT/Ps have adapted models from dementia care to inform their practice [Citation33]. Whilst drawing on established intervention approaches is often appropriate, significant differences in application need to be considered, with management of PPA falling somewhere in along the continuum of aphasia and dementia care. Of critical importance, treatment decisions must be informed by understanding of aphasia and typical language mechanisms, as well as the changing nature of symptoms and the critical need for proactive, anticipatory, and ongoing care [Citation25]. Hinshelwood et al. have advocated for a phased treatment approach, whereby the SLT/P works to optimise language abilities at every stage, whilst responding to future decline [Citation26]. Still, for clinicians who are less experienced in either their careers or in working with PPA caseloads, treatment decisions can be challenging. An exploratory survey, for example, indicated that only 57% of SLPs in the USA had heard of PPA [Citation34] (n = 105). Such clinicians would benefit from published consensus on best practice principles to guide them through the myriad of decisions and practicalities that are encountered when working with individuals with PPA and their support networks. One notable consideration is that the expert opinions and treatment models that have been published typically reflect the practices of a particular team or service rather than reflecting consensus recommendations or more widely endorsed practices. Furthermore, five systematic reviews have been completed to date to determine which interventions have a stronger evidence base [Citation35–39] but these findings do not necessarily correspond with the interventions that will be most effective or appropriate for an individual client [Citation19] or ultimately adopted by expert therapists [Citation33]. As such, more widely developed and expert-generated principles to guide clinical practice are a priority for the PPA field.
Benefits of consensus best practice principles
Establishing best practice principles can help to promote the adoption of evidence-based interventions (in the broadest sense of the term “E3BP” [Citation19,Citation40]) and improve the quality of services, by synthesising expert opinion. They provide a means of benchmarking service provision and supporting clinical decision-making. An example of the successful implementation of this process in a similar area is the guidelines by Simmons-Mackie et al. on The Best Practice Recommendations for (stroke) Aphasia [Citation41]. For the purposes of this paper, we use the term principles to describe practice recommendations that span the continuum of care and have the potential to provide a meaningful reference point for people living with PPA and their families so that they know what to expect, what services and types of interventions can or should be offered and help plan for the future. The establishment of best practice principles is important to support both self-advocacy and autonomy for individuals and families as they make choices regarding their care [Citation19]. Consensus best practice principles can help SLT/Ps to advocate for improved service provision to address the widely recognised access issues faced by this community. Furthermore, such recommendations are valuable tools for service managers, funders and administrators when tasked with organising services and advocating for continued and long-term supports across the continuum of care in neurodegenerative caseloads.
Aims of the current study
The aim of this study was, therefore, to establish a consensus amongst clinical-academic SLT/Ps on best practice principles in the selection and delivery of speech and language interventions for people with PPA. A PPA Consensus Working Group was convened to identify principles that reflected expert opinion and to discuss and synthesise these with current research evidence.
Materials and methods
The study was approved by the Chairs of UCL Language and Cognition Department Ethics, Project ID LCD-2020-14. All work undertaken in this study was conducted in accordance with the Declaration of Helsinki. All data were anonymised and stored securely in line with the Data Protection Act, 2018 and UK General Data Protection Regulation guidance, 2016.
Participants and recruitment
Expert SLT/Ps were identified in the first instance from a recent systematic review of the research literature in this field [Citation38]. Authors of papers included in the review who met the inclusion criteria listed below were contacted by email to invite them to participate in the study. Authors were also asked to suggest any other individuals who met these criteria to continue recruitment via a snowball technique:
SLT/P by background;
Experience in both clinical and academic work in PPA;
Published authors on the topic of interventions for PPA.
Having consented, demographic data and information about their experience in the field of PPA were collected from participants. This included time since clinical qualification, number of people with PPA seen across their research and clinical careers, and information about setting and mode of delivery. All those who acted as participants were also invited to further engage in the interpretation of the study results and subsequent development of best practice principles as co-authors.
Procedures
There were three stages to the data collection and generation process. First, a nominal group technique (NGT) was completed. Second, the NGT results were disseminated to all involved and became the impetus for discussion during two subsequent focus groups with the same participants. Third, the themes developed from the qualitative analysis of the focus groups were once more disseminated. Finally, a last round of (optional) responses and comments sought from all participants and these were collated and integrated into the dataset.
Nominal group technique
The NGT is a commonly used method to establish consensus on a specific topic from multiple participants. The method has a strong focus on equity of contribution, ensuring that all participants are empowered to contribute and share their opinions in a structured and systematic way [Citation42]. It is also recognised as a reliable and valid method of data collection [Citation43] and therefore presents a viable method for this study in developing best practice principles.
The core research team (AV, JC, LR, DH, and SB) developed the central research question in advance: “What are the most important speech and language therapy interventions for people with PPA?”. The NGT comprised a two-stage ranking process: stage 1, initial ranking, involved a 90-min group meeting held over video conferencing software (Zoom) which was video-recorded for transcription and later review. In line with guidance for conducting NGT meetings [Citation44], participants were asked to generate ideas that they felt answered the central question, share these in a round robin format around the group, then contribute to group discussions to define and clarify these. Then, each participant individually and anonymously ranked the top eight items they felt best answered the question. Each of these items was assigned a number from 1 to 8 (where “most important” was ranked 8 and “least important” was ranked 1) and each participants’ list sent to members of the research team who were not themselves participants in the study (LR, DH). These research team members aggregated these rankings and converted them into total scores across the group. Items on the list which described the same or highly overlapping interventions were discussed and merged, with agreement amongst the research team. At this stage, items were assigned labels and definitions based on a review of the video transcripts. In stage 2, the re-rank, these preliminary results (a list of group-ranked interventions relevant to answering the central question, with brief descriptions) were circulated via email to all participants. Participants were asked to individually consider this aggregated list, re-rank their top eight interventions then return these new rankings. LR and DH aggregated these once more into final scores to demonstrate which interventions were most endorsed across the group.
Focus groups
After the NGT process was complete, a second 90-min meeting was held over video conferencing. In line with NGT methodology [Citation42] focus groups provided an opportunity for participants to explicate their rationale and address the complexity of working with people with PPA. Given the size of the group and the need to accommodate multiple international time zones, two separate focus groups were held. These were facilitated by SB and DH, who were not part of the research community, respectively, using topic guides developed in advance by the research team, with questions designed to: (i) address the participants’ experience of completing the NGT ranking process, (ii) discuss the complexities of delivering interventions for people with PPA (especially those that could not be captured by the NGT process), and (iii) to share opinions on best practices when working with PPA (see Supplementary Appendix 1).
Qualitative data analysis
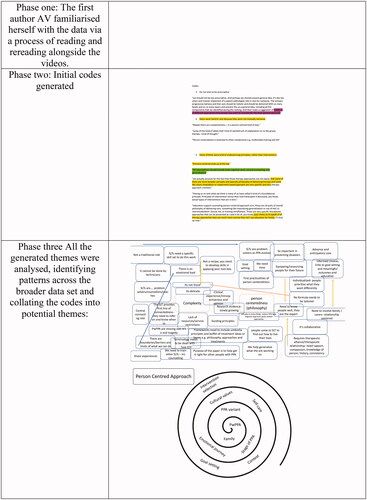
Transcriptions of the meeting were automatically generated by the video-conferencing software, then edited for accuracy and anonymised. Given the aim of collating the views of expert SLT/Ps, qualitative methods employing a reflexive thematic analysis were undertaken in multiple phases as described by Braun and Clarke [Citation45,Citation46]. In phase 1, the first author AV familiarised herself with the data via a process of reading and rereading alongside the videos. In phase 2, initial codes were generated by AV who systematically coded interesting features on a line-by-line basis. See for an illustration of work undertaken throughout the analysis. Images presented in this figure are not results, per se, but form part of the analytical process. As an example, the spiral diagram in phase 3 represents the process undertaken to collate codes into potential themes. To ensure rigour, each of the other members of the research team (JC, LR, DH, and SB) coded one quarter of the data independent of AV’s original codings [Citation47,Citation48]. The coding was completed in an inductive manner such that all team members coded in a data-driven way, rather than being guided by any expectations for the study results or any personal or professional views on the topic. AV compared the other raters’ codes to her own to ensure there were no large differences in interpretation, then a meeting of the research team was held to discuss the broad patterns and relationships between these codes, using a peer debriefing process [Citation49,Citation50]. In phase 3, AV analysed all the generated codes, identified patterns across the broader data set and collated the codes into potential themes, again debriefing with the research team. In phase 4, AV checked each potential theme against its codes and data extracts, then read across the entire data set, in order to ensure (i) that the data within each theme cohered together meaningfully whilst (ii) each theme had clear boundaries and was fairly distinct from the other themes. Interactions which did exist between themes were noted and later captured in our conceptualisation of the data as a whole under two core themes. AV also started to generate ideas for a preliminary thematic map or visual way of representing the relationships between themes (see ). Once a more thorough understanding of the dynamic relationships between the themes was agreed upon, the team used metaphors to brainstorm the second version of this visual representation (see Supplementary Appendices) and developed the clock analogy which will be explained below. In phase 5, the themes were refined and finalised. Each theme’s data extract was revisited and organised into a logical narrative which related back to the central research question. They were given final names and definitions by AV in consultation with the research team. Phases 5 (defining and naming themes) and 6 (writing the report) were expanded beyond Braun and Clarke’s [Citation45] original guidelines to include a formal member-checking process in which a video-recorded presentation by AV was developed to highlight and explain the themes, subthemes, and their relationships. All participants were sent this video and invited to comment on the process and results. Responses were incorporated into the interpretation, finalising and description of the themes and subsequent manuscript preparation (phase 6) in an iterative and collaborative way, given that all participants were also authors of this study in addition to the core research team.
Figure 1. Visual record of phases of reflexive thematic analysis. This figure does not present results, but the analytical process undertaken to develop the results.
Results
Participant demographics
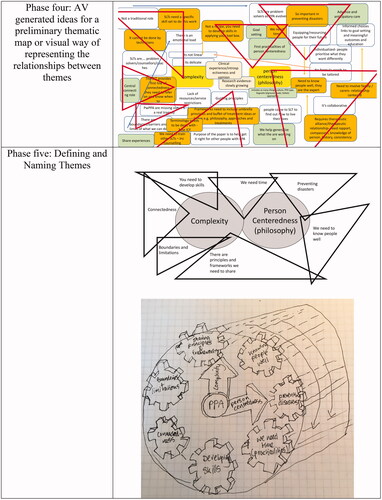
Unfortunately, due to constraints related to differing international time zones and despite careful planning, one person was unable to attend any of the meetings. Consequently, 15 participants took part in the study. All were female and met the inclusion criteria. They worked in Australia (n = 5), USA (n = 5), UK (n = 3), and Canada (n = 2). They reported providing services to people with PPA in a range of languages including English (n = 15), German (n = 3), French (n = 1), Russian (n = 2), Spanish (n = 1), Italian (n = 1), Polish (n = 1), Greek (n = 1), and Hindi (n = 1), in addition to providing advice on working with PPA to other SLT/Ps working with patients who spoke numerous languages including Portuguese, Farsi, Urdu, French, Catalan, and Cantonese. Although we state averages here (see for details) participants reported a wide and heterogeneous range of: years since SLT/P training (1.5–45 years, mean = 22.6 years), years working with people with PPA (3.5–30 years, mean = 14 years), and patients with PPA seen per annum over the past 5 years (5–100). Participants reported treating a wide-ranging number of participants across their entire careers, across both clinical and research settings, as shown in .
Figure 2. Number of patients seen by participants across their careers.
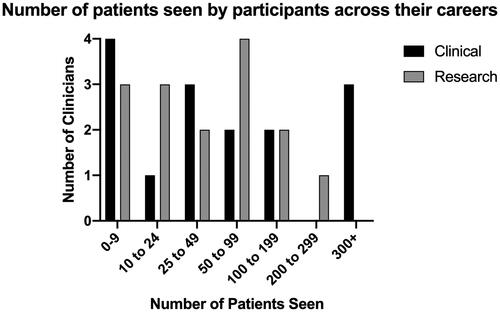
Table 1. Participant demographic data.
Nominal group technique
Seventeen items were identified and ranked in order of importance during the NGT. These are presented in their ranked order in , alongside definitions extracted from the NGT transcript, refined by the research team. Participants expressed concerns during the NGT about the ranking process and felt strongly that the results did not adequately represent the individualised and complex process of selecting and delivering interventions when working with people with PPA. It became clear that our group felt that speech and language interventions were not the only critical components that should be included in SLT/Ps practice.
Table 2. Results from nominal group technique ranking.
Thematic analysis
Having examined the results from the NGT, participants felt that the ranked list of treatment options did not reflect the complexity of working with people with PPA and the decision was made to hold two focus groups to facilitate further discussion. Two core themes and seven subthemes were identified in the data generated in the focus groups that followed the NGT work. The themes reflect the recurring important and understood ideas for the group and whilst bounded and agreed to be separate, do have interactions with the other themes. This speaks to the complexity of the core themes and the fact that this study’s results are trying to describe interventions that are responding to a changing illness profile and trajectory. The core themes that associated with overarching SLT/Ps therapeutic management were: (1) clinical complexity and (2) philosophy of person-centredness. Seven subthemes revolved around these two main themes. As will be further discussed, they are dynamic themes, inter-related and all related to the two main themes, which are, in turn, related. These subthemes included: knowing people deeply; preventing disasters; connectedness; practical issues; professional development; barriers and limitations; peer support and mentoring towards a shared understanding. There is no hierarchy to these subthemes, and each was identified as equally important; however, there are clearly some that are more related to delivery of speech and language therapy (knowing people deeply; preventing disasters, connectedness and practical issues), and others related to professional development and service-related issues (barriers and limitations and peer support and mentoring towards a shared understanding).
Clinical complexity
The multifactorial complexity of working with this specific yet variable client group was reflected throughout the NGT discussions, initially to emphasise the limitations of the ranked items from the NGT:
I was a little bit concerned during this ranking, that I hope it wasn't going to be used as prescription. [P8]
Another participant explained the experience further:
I think my struggle when I was ranking these is it was like comparing apples to oranges with all of these things being the different categories. [P9]
Many participants highlighted that working with people with PPA is complex because it is not just about language intervention but also support, education and counselling. They highlighted that this can be a complex process to negotiate:
That's a really delicate conversation that some speech therapists are very good at, but some find it really difficult. […] You know, actually they have still got to give people hope. It's a really difficult line to tread. That you're acknowledging, yes it's a progressive condition, but you're still giving them hope and still helping people manage and I think that's really skilled, I really do. I think it's something we really underestimate. [P3]
Managing and connecting different time periods of PPA was described as part of this complexity:
I also have a number of patients who actually just want to work on the word finding and nothing else at the beginning […] but in the mid stages, they require a little bit more than just working on their impairment level. [P6]
Participants emphasised that being able to judge how to work with people with PPA and their family members requires the SLT/P to consider the complex and unique needs of every individual:
How do you make that husband and wife communicate to the best of their ability, you can't take a cookbook to this condition because everyone is so different. [P2]
There are three variants currently described and further sub variants within variants have been proposed [Citation51]. As a result of this diversity of presentation and subsequent nature of progression, different factors need to be considered when suggesting interventions for each individual according to their needs:
Let's say in the same stage and the early stage of PPA, and let's say they all have the same goal of wanting to be able to order at a restaurant, right, and they have different PPA subtypes. Right. I'll have someone who says, ‘Well, I really don't want any help from my care partner. I want to completely do this on my own. I love exercises.’ So, we'll do personally relevant words. If they're semantic we’ll work on, you know, actually, recognising the food items on the menu, etc. But you can have another person in the mild stages that I've worked with who has said, ‘I am so anxious when they get to me, I would much prefer my care partner, just to order for me’ or I've also had people from a cultural standpoint, saying, ‘In my culture my husband or wife always orders for me’. And that's fine. And I've had others that have said, ‘Oh, I'm willing to use an external aid. You know, exercises make me very anxious. I don't want to practice exercises. I just want a quick fix. I just want to look at my phone, or I know I don't like phones, that's too difficult for me. I want to use this little card and order’ and that's okay too. [P9]
This quote also captures the overarching philosophy of person-centredness that respondents returned to throughout the discussions.
Philosophy of person-centredness
This philosophy was deemed integral to building a relationship with clients, understanding them and their needs:
We don't just launch into therapy, there's a whole component of time spent with the person and working out where they are in their journey emotionally, what they require personally, what their people around them require and who they are. [P12]
Participants emphasised the need to dedicate time and energy to gaining a deeper appreciation of the clients’ individual previous qualities, back story and demeanour to enable the clinician to genuinely support people over the long term:
You need time allocated to a comprehensive development of a true understanding of this individual and what's going on in their lives. [P8]
Person-centred care must be underpinned by research evidence demonstrating the effectiveness of selecting personally relevant materials and individualised therapies:
Every person with primary progressive aphasia deserves to receive a holistic evidence-based approach that is person-centred and dynamic in its nature and includes Therapy education and counselling. [P6]
It was also described as an overarching guiding principle when working with people with PPA:
In my view, we are working towards some kind of general statement that would reflect the fact that care has to be person-centred and has to incorporate education, support and therapy. But then we would list all sorts of therapy approaches that one may use so that we account for both the overall philosophy of providing person-centred care for people with PPA, but also acknowledge that there are different approaches. [P6]
A person-centredness philosophy was considered central to a framework or model of care:
The relationship issue or the relationship-centredness, person-centredness, the compassion that you're talking about is central. And then these other things, almost sort of like spokes out of it. [P15]
The seven subthemes identified in the data are interrelated and demonstrate the dynamic nature of the data.
Knowing people deeply
Participants emphasised the need to know people deeply, at a fundamental level. This requires the SLT/P to go beyond the tick box of knowing interests and vocation to truly knowing what things and values are important to the person and what brings their life meaning, whilst assisting the individual and their family to understand what PPA will mean for them and their daily lives:
Understanding them; their values, their culture, their identity – and obviously I haven't even mentioned PPA type – and whatever that individual’s areas of strengths and difficulty are. We have to do a lot of work, don't we, before we get to the point of even thinking about therapy. [P12]
This was felt to be a collaborative approach whereby people come to speech and language therapy to help the individual and their supporters to move forward on their journey. Participants explained this by emphasising the many deep, existential questions that their clients ask when making sense of the diagnosis and its impact:
A lot of clients get stuck in the why me? phase, ‘Why me? Why did I get this? I did everything right. I lived a healthy life. I did everything I was supposed to do’, and he [a person with PPA] said, ‘If you're in a building and it's on fire, you don't sit down and grab a chair and ask why. You get the hell out of there’. And so the question becomes not ‘why me?’, but ‘what now? what can I do?, how can I act?, how can I be empowered?’ and that's really what they're coming to you for. [P14]
The SLT/P is often the first to really discuss what this diagnosis will mean for the person and their daily life. Understanding the patient’s and their caregiver’s emotional needs and preconceived notions of the disease is important in this space:
Education, support and counselling both for the person with PPA, and the family. It's really important to make sure we include this, for some of the most heart-breaking work is with the family members who don't understand. [P4]
As the SLT/P gets to know the person well they become better placed to support them to live their lives:
They're coming for you to say, ‘How can I live my life? How can I exist with this? How can I have meaning with this? Where’s my hope? Where’s my purpose?’ And it gives them hope and purpose in small doses, you can keep them going along and you can give them reasons to get up in the next morning. [P2]
Preventing disasters
Participants discussed the importance of their role in terms of timeliness of referrals and service access to prevent disasters from occurring and to support anticipatory care. For example, participants described being referred people with PPA only after disasters had occurred, whereby important windows of opportunity for intervention and support had been missed, with profound consequences:
we often get patients who are referred to us due to some sort of a disaster that happened. We've had patients who spent the night in prison due to a communication issue where someone assumed that they were inebriated, or they've lost $100,000 due to a misunderstanding or a scam or being unable to pay something. [P1]
Indeed, it is not uncommon for people with PPA and their families to find out too late that there may have been something they could have done to prepare for such a situation:
they find out too late that they should have been talking to a social worker, potentially an attorney. You know, all of the specialists who need to be involved. [P5]
Empowering and enabling individuals to anticipate their future care needs was felt to be critical in preventing such disasters:
Anticipatory care is so important because connecting people to the multidisciplinary team is so important in preventing disasters further down the line. And that's the whole way early care of dementia is moving in the field in the community I’m in. That we're trying to provide more anticipatory care. [P8]
However, this was identified as a complex process that some people were more ready and able to participate in than others:
Some people are really prioritising their advanced decision-making and they come to me and they say,’ I want to be able to’, you know, they want to organise power of attorney. And some people aren’t at all ready. ‘No, I'm not ready to discuss that at all, ever’, so it's that emotional journey. [P12]
To safeguard against disasters participants described practical approaches, including the use of review and ongoing education and counselling sessions to ensure an informed and proactive approach to preparing for change over time:
I say to my people with PPA, if we've achieved certain person-centred goals, let’s get you on the books for six months because I want to see you back. I want to help you anticipate what might be coming down the road and think about different tools and so on. [P10]
Connectedness
Some of the complexity in working with people with PPA is in being the first specialist involved following a diagnosis, who will spend time with the person, getting to know them, resulting in a huge responsibility to connect people:
The speech pathologist is often the first specialist referral, but it's incumbent upon the speech pathologist to help the individual develop within the community outside of the hospital system, but within the community and identify their own multi-disciplinary team. [P8]
Participants emphasised that it is the role of the SLT/P to provide the first line of connectedness to other services:
I think it's really important for speech language pathologists to see ourselves as the first line of connectedness, because in many cases if they make it to us, we should see it as our role and we should convey to other clinicians that it is our role to find out what services people have been told about. [P5]
Specifically, this might include multiple different team members including a psychologist, neuropsychologist, dietitian, and social worker:
…it's really important to build that team for the individual of the primary healthcare provider, possibly a psychologist, the neuropsychologist. In the case of our non-fluent patients, a dietitian, maybe some physio and a social worker to help them access services. [P8]
Onward referral to services such as social work was identified as particularly important for supporting the entire family:
Social work is very crucial. I always ask a social worker to connect with them regardless because the family dynamics always come in some way to play. [P6]
Knowing how best to refer patients on is a skilled process that requires sensitivity and care (and notably one which is also connected to the subtheme of professional development):
I think it's something that has to be handled with care as well. Connecting people with services is sensitive and requires a great deal of skill and I worry that [.] clinicians aren't trained to do this. And so, I think the first important step in whatever product comes of our group to make it clear that this is this is not just about making phone calls. It's a skill also and it's incumbent upon us to develop our own connectedness in our communities. [P5]
Practical issues
Participants identified a range of practical issues that need to be addressed to enable comprehensive, coordinated, and person-centred care. These issues reflected the logistics of service provision, such as managing goal setting sessions, scheduling enough time for periods of treatment and review, and having clear materials available to help explain PPA to team members as well as clients themselves. Participants identified the need to organise service provision in a way that supported goal setting, ensuring enough time for goal setting conversations and involving the relevant partner:
We have a conversation with the partner and the patient. Then we separate the two. We look at the goals within both of their profiles and then jointly, and they are usually very different. [P1]
Allowing for ongoing conversations as symptom and situations evolve over time requires long-term support:
You have to have a repeat of some of these conversations, but it becomes a little bit more fine-grained. In the beginning you just have essentially the first conversation someone's had about even having a selective language impairment. [P1]
Moreover, speech and language therapy services need to make sure communication, written reports, and verbal information, are delivered to people with PPA in a way that is clear and accessible:
they didn't receive the information at a time or in a manner that was accessible to them because as we all know, people need to be given information in doses and at the appropriate time and using the right kind of communication approach. [P5]
During different stages over the disease journey people may require services structured in different ways, for example, outpatient appointments may be more important in the first instance whilst home visits may become increasingly important over time:
We get a lot of people who are perhaps a bit further down the line, for whom we do home visits, so people don't come to us. We go and see the people that won't go anywhere or do anything and that that's a different kind of clientele than when I worked in clinic and people came to us and they were really insightful and really desperate for help. [P3]
Flexibility with time was identified as a critical requirement to actually implement interventions. This was not just in the initial stages to establish and build rapport, but also during therapy to assist in generalisation:
They needed more therapy to actually generalise what they were doing, and problem solve and that needed repetition and redundancy. [P12]
Given people with PPA are expected to change over time, being proactive rather reactive (and therefore risking disasters) was advocated by participants. Regular re-assessment and review was again identified as a practical solution to monitoring these changes:
I feel really strongly about recurrent reassessment. You know the dental model, in the US, we get our teeth cleaned every six months whether or not you think you need it, you just go. [P10]
Professional development
Although having a strong connection to the subtheme peer support and mentoring others to a shared understanding, this subtheme is focused on one’s own personal experience (as an SLT/P) and professional development of skills over time. Participants described the importance of the SLT/P’s development, the experiences that will inform their knowledge, skills and insight when working with people with PPA:
I think we're on a journey too. So, we've got our own little kit of experiences. [P2]
The clinicians spoke of developing knowledge of the “tools” available to them over time:
I think that some of the treatment decisions become much easier because we know our toolboxes. [P15]
It was emphasised that many SLT/Ps do not have this experience and without this knowledge it is possible the therapist may not meet the person’s evolving needs:
She [another SLT/P] said after the two sessions, she thought was successful, she was, she was quite happy to discharge them. She thought they got it, but she didn't understand that need to do more. [P12]
The SLT/P must change their understanding of goal setting from a traditional model, which may be more about improvement, to the context of a progressive condition, where the focus is on life participation and compensatory goals:
I think one of the problems when we think about goal setting is that traditionally it's been a very impairment-based model, right? So you do standardised testing. Then whatever their weaknesses are, you come up with goals and then you work on those exercises and drills to meet those goals. … Even the electronic health record systems in the United States, at least the ones we use, they have goal banks that therapists are just clicking the goals for each person and they're completely impairment based, they're not life participation goals. [P9]
Working with people with PPA was described as constantly changing and dynamic, meaning that the SLT/P has to be self-aware:
This is the hardest area I've ever worked in in my life because it's constantly changing and it's constantly dynamic. You can't just sit there and be prescriptive. You can't just give this list and say now go out and be. First, you've got to become yourself, you know, yourself as a therapist. You've got to grow, and you've got to be willing to make mistakes because, you know, of course I'm going to look back at some patients that I did, particularly early on and go ‘I wish I'd done that differently’ and but it's what you do with that, you know, where do you take that? How do you grow from that? And it's always evolving, no matter who's sitting here today, we will still look back at what we're doing today and go, ‘I wish I could tweak that, change that and that’. [P14]
This also requires the SLT/P to act in many different roles as counsellor, educator, and coach, as well as being a reflective clinician. This diverse and emotional load can be challenging to manage and may not suit everyone:
It's a really hard area and you have to be really good at counselling. You have to be really good at support. You have to be really good at education, you have to be really good at centring on the patient. And if you're not willing to do any of those things, and all you want to do is impairment-based therapy, don't come, don't come in. [P14]
Barriers and limitations
Participants reported that many people with PPA may not have the opportunity to access the range of required services, and this was identified as a significant problem, a disaster or tragedy in some cases:
Our patients are missing out on critical components of their care. And it's a real tragedy, they find out too late that they should have been talking to a social worker, potentially an attorney. You know, all of the specialists who need to be involved. [P5]
This paucity of referral options may be context specific:
I was also reflecting on the different jurisdictions we're talking about for some of these things. My experience of working in the UK and when to introduce that [decision-making and power of attorney] was slightly different than my experience of working in Australia and how to talk about that there, so that we're talking not only about how different places are funded but also setting, for example mental health trust [health care organisation] or physical health trust [health care organisation]. [P12]
Of concern, barriers to accessing speech and language therapy were identified as resulting in a reduced likelihood of timely access to other supports:
If they've just had, you know, information given to them in a quick exchange with a neurologist, there's so much more work to be done […] it terrifies me to think that there are people for whom that's the end of the story because, by and large, people are still not getting referred for speech and language therapy who have this diagnosis and then that means they're also not getting referred to all of those other really important services. [P5]
Similarly, a lack of continuity from local speech and language therapy services with restrictive service models was also identified as a serious concern:
You're off our books until you end up in hospital again with a fall or something. [P2]
Participants compared the experiences of people with PPA to those with other diagnoses and recognised the inequity in the care they receive:
If you had Motor Neurone Disease you will have a case manager. But these people are falling in the cracks. [P2]
Peer support and mentoring towards a shared understanding
Participants felt strongly that the current situation could be improved by providing guidance, and training to others within the speech and language therapy profession. This was central to our discussions after the ranking exercise and informed the shape that best practice principles should take. It was felt that collegial guidance could be presented as an overarching philosophy alongside specific information on appropriate treatments:
We are working towards some kind of general statement that should reflect the fact that the care has to be person-centred and has to incorporate education, support and therapy. But then we would list all sorts of therapy approaches that one may use so that we account for both the overall philosophy of providing care for people with PPA, but also acknowledge that there are different approaches. [P6]
Possible frameworks for such guidance were captured in a number of metaphors used by participants including “layers” to capture the overarching philosophies and a “buffet” of different intervention approaches:
Care should be holistic and should be delivered with so many facets and on so many layers and [we should] present this as a general idea, including all the components that we identified during the ranking. And then make a suggestion or buffet of different approaches that people may want to incorporate into their general approach. [P6]
Others described the philosophies as the “umbrella” and referred to the treatment approaches as “buckets”:
Umbrella approach of the general philosophy of how you approach the treatment. But within that also have these buckets of domains that you can go into that are all guided by principles of maximizing generalization or patient wellbeing while also depending on the patient. [P1]
The overarching philosophies and the “buffet” analogy were explicated throughout the discussion as participants started developing some consensus around this guidance:
Education, support, counselling, person-centred approach, those are all parts of the overall philosophy of delivering care, something like maximizing generalization or use of AAC or neuromodulation, or training mindfulness. Those are very specific therapeutic approaches that can be presented as a list of, you know, your menu so to speak of therapy approaches they are much more narrow than let's say education for family. [P6]
This discussion also incorporated possible recommendations on influencing graduate education when working with people with a neurocognitive condition such as PPA:
So perhaps even thinking about recommendations for what speech pathologists, what kind of experiences they should have when it comes to some training in this area. [P10]
The two core overarching themes and the subthemes identified through the thematic analysis are represented in the clock model (). The subthemes are depicted as interconnected cogs that are dynamic and changing over time. The rotation of the clock hands through time further represents the changing and progressive nature of PPA. The clock model captures that working with PPA is complex, and that the themes identified here are inexorably related. The arms of the clock (labelled “Person-centredness” and “Complexity”) are able to move around to any of the subthemes. At any one time, the SLT/P may need to focus intervention on different areas concurrently, and then as the clock arms continue to move, this focus may need to change. The smallest (third) arm demonstrates the importance of frequent review by the SLT/P over time. We wanted to demonstrate how they influenced each of the subthemes and could also coincide themselves considering the overlap of these two core themes. The cogs represent the notion that as one “theme” or element moves, it can affect the turning of others, thus capturing the interactions between the elements. The 3D nature of the figure captures changes of all these dynamic elements in time; that there is a process of continual movement in the model to represent the approach to PPA as continuously shifting. The overall effect leaves the observer with an unease – that each element can turn and affect others. This unease mirrors the lack of predictability of the course of PPA: of the road to diagnosis, to appropriate services, to a recognition first of language changes and later of cognitive changes. The figure also demonstrates how the consensus of the expert group is not just about recommending a therapeutic approach, but instead is about many elements that are required for this: self-awareness and counselling skills in the face of devastating, existential questions from people and their families; a deep knowledge of the person and how they change in time; an understanding of the role and services from other members of the team; and an ability to look ahead and prevent people from falling through the cracks or experiencing more avoidable difficulties. Whilst this figure aims to visually represent what it is like to work with people with PPA, and capture its complexity, the themes outlined in this study have been further developed to form best practice principles for working with PPA in (see section “Discussion”).
Figure 3. The clock model.
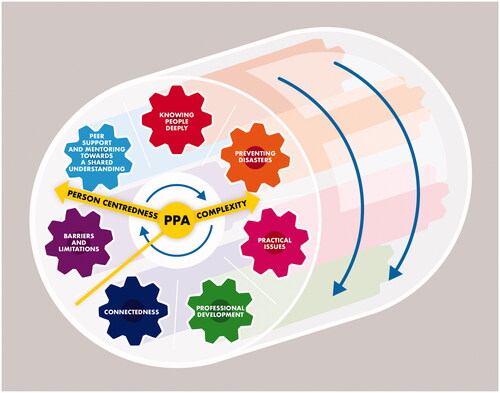
Table 3. Best practice principles when working with people with PPA.
Discussion
This study has highlighted that the philosophy of current practice in selection and delivery of speech and language therapy interventions for people with PPA cannot be captured by a list of ranked items. This is a complex area requiring the SLT/P to use a person-centred, dynamic and evolving approach to craft a bespoke intervention that meets the needs of the individual. A clinician must consider both the broader principles of practice as well as the “buffet” of interventions most suitable to the individual at a particular time during the illness trajectory. Working with PPA involves an expanded role to provide sensitively tailored interventions and to work as an advocate to link across aphasia and dementia services. With this in mind, the authors offer a set of best practice principles and philosophies to guide practicing clinicians, presented in . The ranked list still captures important intervention options for SLT/Ps to consider when working with people with PPA; however, the best practice principles should guide the complex decisions regarding “how” and “when” they should be applied and used.
Importantly, speech and language approaches for PPA differ from existing models of care for stroke aphasia and dementia. First, as a neurodegenerative disease rather than a focal injury, people with PPA (particularly mild) can still make robust gains over the shorter term that are on par with or even exceed those with stroke induced aphasia. Equally therapy may be focused on maintenance, which is not generally the target when working with someone with stroke induced aphasia [Citation52]. Second, in comparison to many other dementias, interventions do not need to address memory, which is broadly intact during early stages, but instead the dissolution of semantic, phonological, and grammatical impairments impacting on communication [Citation53]. Whilst we have a general understanding of the progression of Alzheimer’s disease, PPA has a heterogenous presentation that can result in differing language or cognitive, or motoric changes [Citation3–5]. It is, therefore, often not possible to fully anticipate the evolution of the PPA disease pathway a person may travel, and given the centrality of language, the SLT/P is often the sole health care professional involved for a period of time. The impact on all those affected by the PPA diagnosis, both the person and their loved ones [Citation20,Citation21], means investing time and effort in knowing the person and those around them is paramount. Where at all possible, significant others need to be actively involved from the start and investing in interventions which support the relationship will prove ecologically valuable.
An important role of the SLT/P working with a person with PPA is counselling and supporting them as they experience grief and loss. Dealing with a terminal diagnosis requires the SLT/P to provide counselling alongside speech and language therapy and do this throughout the relationship [Citation54]. Despite being so different from other dementias, people with PPA may eventually access carefully selected support from generalist dementia services. At this point, the SLT/P is often instrumental in negotiating these transitions, supporting and educating colleagues and team members [Citation33]. The SLT/P must therefore fulfil a complex role in supporting people with PPA.
SLT/Ps value the evidence base, but also principles such as person-centredness, that underpin clinical decision making in a real-world setting [Citation55]. Given that a previous consensus study with six UK based SLT/Ps demonstrated that person-centredness underpins practice when working with people with semantic variant PPA [Citation33], the results of this study may be unsurprising. Importantly, the person-centred approach allows SLT/Ps to understand the financial constraints, cultural preferences, family dynamics, occupational experience, and emotional wellbeing and resilience of the person with PPA [Citation26,Citation32]. Understanding the complexity of all of these factors, some of which are internal, enables the SLT/P to cultivate an appropriate and effective intervention plan that is unique to the individual. The process of disentangling these factors takes due diligence on the part of the SLT/P. This approach is similar to the work SLT/Ps do with people with stroke aphasia and the term life participation approach to aphasia (LPAA) can be considered synonymous with person-centred care for the purposes of this publication (see Box 1). However, the importance of allowing for time and space to process the diagnosis and its impact cannot be overemphasised: it is in this realm that individuals are able to distil what is most essential to them. Given this time and the support needed to do so, the intervention plan can be born out of a place of trust and vulnerability.
The “Life Participation Approach to Aphasia” (LPAA) puts the life concerns of the person affected by aphasia at the centre of all decision making. The approach supports people in achieving immediate and longer term life goals, focusing on engagement in life. The approach has been clearly outlined by the LPAA Project Group in their publication Life Participation Approach to Aphasia: A Statement of Values for the Future [Citation56].
A person-centred approach is where the person is placed at the centre of treatment planning. Support focuses on achieving the person's aspirations and is tailored to their needs and unique circumstances.
The authors acknowledge that there are nuanced differences between these approaches, however for the purposes of this publication, the term person-centred approach is used as synonymous with the life participation approach to aphasia. A person-centred approach is overlapping with other centredness terms which include family and relationship centred care [Citation57]. We can also see that the dignity and respect offered through the LPAA reflects the centredness approaches and therefore we draw parallels with that LPAA approach as one of the most influential in the aphasia field and therefore of relevance here.
Internationally, there are only a handful of SLT/Ps who have specialised in working and doing research with people with PPA. This small community have been working independently, without previously connecting to discuss practice. In this context, it is of interest that one of the important subthemes in this study was that SLT/Ps working in PPA need to be part of a broader community of specialist PPA practitioners who can support each other, share resources and expertise. Systematic reviews [Citation35–38] have synthesised the current research evidence on specific interventions for PPA. Whilst these identify the evidence base, they do not reflect how to select what is most relevant for an individual client, nor the knowledge of the expert practitioner (practice-based evidence). This study presents data collated from a number of internationally known specialists in the field. Considered jointly, the NGT data and consequent focus groups and thematic analysis describe the philosophy of current practice. The authors have coalesced these data to offer a set of best practice principles and philosophies to guide other SLT/Ps in delivering care to people with this diagnosis in . This paper offers an opportunity to bring this expertise together into one place; to address the underpinning philosophies and principles that guide these experts. This will form a basis for the sharing of more detailed information on intervention in the future.
Strengths and limitations
The aim of this study was to employ the NGT, which incorporates mathematical voting techniques to aggregate group judgements equally [Citation44], to establish a consensus amongst clinical-academic SLT/Ps on best practice principles in the selection and delivery of speech and language treatments for people with PPA. NGT does not allow for anonymity in the way that other consensus methods such as Delphi do, and can thus bias the responses of participants. Importantly, however, the group identified that the aim of the study was not adequately captured by a list of ranked items. The NGT does, however, make provision for additional focus groups to elicit opinions and discussion from participants. Including these focus groups allowed the researchers to capture the complexity of working with people with PPA. Additionally, member checking during the reflexive thematic analysis ensured participants were actively involved throughout the analysis process. Bringing this small community together in the focus groups was valued by the participants, with many commenting they felt validated and enjoyed meeting people within their own community of practice. To negate dominance of one voice, and provide everyone the opportunity to contribute, these meetings were facilitated by two speech and language academics, who were not part of the existing community of PPA practitioners and academics. During this process, one participant withdrew from the final phase of the study, prior to authorship, due to time constraints. Remaining participants demonstrated their commitment and their desire to share practice recommendations as authors of this paper.
Future directions
The establishment of best practice principles will support both self-advocacy and autonomy for people with PPA and their families as SLT/Ps work with them to make choices regarding their care [Citation19]. This work will support further research with people with PPA and their significant others to identify what speech and language interventions help and which do not, exploring how they themselves have adapted to overcome their own language difficulties, as well as dealing with increasing dependency. This work will enable SLT/Ps to optimise therapeutic approaches and interventions, informing the broader evidence base [Citation19]. In fact, the active involvement of people with lived experience, through patient and public involvement or as consumers in our research endeavours will ensure we are able to meet the needs of the communities we are endeavouring to support (UK PI Standards [Citation55,Citation58]).
Conclusions
This study describes the philosophy and principles of expert practice of working with people with PPA. Our findings reinforce that this is a complex area requiring a person-centred approach to craft a bespoke intervention that meets the needs of the individual and their family as they change over time. This area of practice for SLT/Ps requires skill and experience. The authors have addressed this by unpacking the complexity to reveal what is essential when working with people with PPA. This work, drawing on consensus from experts, should support further practical research to specify the interventions and approaches which best meet the needs of people living with PPA and those who support them through the journey of this highly challenging condition.
Supplemental Material
Download MS Word (68.8 KB)Acknowledgements
We would like to acknowledge jempomak.com who develop the artwork for this paper.
Disclosure statement
AV is supported by an NIHR Development Skills Enhancement Award. During this project, LR was supported by an Australian Government Research Training Scheme.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Gorno-Tempini ML, Hillis AE, Weintraub S, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76(11):1006–1014.
- Coyle-Gilchrist IT, Dick KM, Patterson K, et al. Prevalence, characteristics, and survival of frontotemporal lobar degeneration syndromes. Neurology. 2016;86(18):1736–1743.
- Marshall CR, Hardy CJ, Volkmer A, et al. Primary progressive aphasia: a clinical approach. J Neurol. 2018;265(6):1474–1490.
- Louwersheimer E, Keulen MA, Steenwijk MD, et al. Heterogeneous language profiles in patients with primary progressive aphasia due to Alzheimer's disease. J Alzheimers Dis. 2016;51(2):581–590.
- Mesulam MM, Rogalski EJ, Wieneke C, et al. Primary progressive aphasia and the evolving neurology of the language network. Nat Rev Neurol. 2014;10(10):554–569.
- Leyton CE, Hodges JR, McLean CA, et al. Is the logopenic-variant of primary progressive aphasia a unitary disorder? Cortex. 2015;67:122–133.
- Utianski RL, Botha H, Martin PR, Schwarz CG, et al. Clinical and neuroimaging characteristics of clinically unclassifiable primary progressive aphasia. Brain Lang. 2019;197:104676.
- Hodges JR, Patterson K. Semantic dementia: a unique clinicopathological syndrome. Lancet Neurol. 2007;6(11):1004–1014.
- Matias-Guiu JA, Cabrera-Martín MN, Moreno-Ramos T, et al. Clinical course of primary progressive aphasia: clinical and FDG-PET patterns. J Neurol. 2015;262(3):570–577.
- Mesulam MM. Primary progressive aphasia. Ann Neurol. 2001;49(4):425–432.
- Croot K. Treatment for lexical retrieval impairments in primary progressive aphasia: a research update with implications for clinical practice. Semin Speech Lang. 2018;39(3):242–256.
- Taylor-Rubin C, Nickels L, Croot K. Exploring the effects of verb and noun treatment on verb phrase production in primary progressive aphasia: a series of single case experimental design studies. Neuropsychol Rehabil. 2021;6:1–43.
- Volkmer A, Rogalski E, Henry M, et al. Speech and language therapy approaches to managing primary progressive aphasia. Pract Neurol. 2020;20(2):154–161.
- Beales A, Cartwright J, Whitworth A, et al. Exploring generalisation processes following lexical retrieval intervention in primary progressive aphasia. Int J Speech Lang Pathol. 2016;18(3):299–314.
- Etcheverry L, Seidel B, Grande M, et al. The time course of neurolinguistic and neuropsychological symptoms in three cases of logopenic primary progressive aphasia. Neuropsychologia. 2012;50(7):1708–1718.
- O’Connor CM, Ahmed S, Mioshi E. Functional disability in primary progressive aphasia. Aphasiology. 2014;28(8–9):1131–1149.
- Bier N, Paquette G, Macoir J. Smartphone for smart living: using new technologies to cope with everyday limitations in semantic dementia. Neuropsychol Rehabil. 2018;28(5):734–754.
- Medina J, Weintraub S. Depression in primary progressive aphasia. J Geriatr Psychiatry Neurol. 2007;20(3):153–160.
- Ruggero L, Nickels L, Croot K. Quality of life in primary progressive aphasia: what do we know and what can we do next? Aphasiology. 2019;33(5):498–519.
- Pozzebon M, Douglas J, Ames D. Facing the challenges of primary progressive aphasia: the spousal perspective. J Speech Lang Hear Res. 2018;61(9):2292–2312.
- Pozzebon M, Douglas J, Ames D. “It was a terrible, terrible journey”: an instrumental case study of a spouse’s experience of living with a partner diagnosed with semantic variant primary progressive aphasia. Aphasiology. 2017;31(4):375–387.
- Galvin J, Howard D, Tatton N, et al. Social and economic burden of frontotemporal degeneration: O1. J Neurochem. 2016;138:224–225.
- Kaiser S, Panegyres PK. The psychosocial impact of young onset dementia on spouses. Am J Alzheimers Dis Other Demen. 2007;21(6):398–402.
- Nickels L, Croot K. Understanding and living with primary progressive aphasia: current progress and challenges for the future. Aphasiology. 2014;28(8–9):885–899.
- Khayum B, Wieneke C, Rogalski E, et al. Thinking outside the stroke: treating primary progressive aphasia (PPA). Perspect Gerontol. 2012;17(2):37–49.
- Hinshelwood H, Henry M, Fromm D. Helping them hold on: through phased treatment, speech-language pathologists can help clients with primary progressive aphasia function as normally as possible—for as long as they can. Leader. 2016;21(10):44–51.
- Murray LL. Longitudinal treatment of primary progressive aphasia: a case study. Aphasiology. 1998;12(7–8):651–672.
- Rogers MA, Alarcon NB. Dissolution of spoken language in primary progressive aphasia. Aphasiology. 1998;12(7–8):635–650.
- Riedl L, Last D, Danek A, et al. Long-term follow-up in primary progressive aphasia: clinical course and health care utilisation. Aphasiology. 2014;28(8–9):981–992.
- Taylor C, Kingma RM, Croot K, et al. Speech pathology services for primary progressive aphasia: exploring an emerging area of practice. Aphasiology. 2009;23(2):161–174.
- Volkmer A, Spector A, Warren JD, et al. Speech and language therapy for primary progressive aphasia: referral patterns and barriers to service provision across the UK. Dementia. 2020;19(5):1349–1363.
- Ruggero L, Croot K, Nickels L. How evidence-based practice (E3BP) informs speech-language pathology for primary progressive aphasia. Am J Alzheimer's Dis Other Dement. 2020;27:35.
- Kindell J, Sage K, Cruice M. Supporting communication in semantic dementia: clinical consensus from expert practitioners. Qual Age Older Adults. 2015;16(3):153–164.
- Wooley M. Role of speech-language pathologists in aphasia therapy and rehabilitation as reported by practicing speech-language pathologists [Doctoral dissertation]. The University of Mississippi; 2014.
- Cadório I, Lousada M, Martins P, et al. Generalization and maintenance of treatment gains in primary progressive aphasia (PPA): a systematic review. Int J Lang Commun Disord. 2017;52(5):543–560.
- Carthery-Goulart MT, Silveira AD, Machado TH, et al. Nonpharmacological interventions for cognitive impairments following primary progressive aphasia: a systematic review of the literature. Dement Neuropsychol. 2013;7(1):122–131.
- Jokel R, Graham NL, Rochon E, et al. Word retrieval therapies in primary progressive aphasia. Aphasiology. 2014;28(8–9):1038–1068.
- Volkmer A, Spector A, Meitanis V, et al. Effects of functional communication interventions for people with primary progressive aphasia and their caregivers: a systematic review. Aging Ment Health. 2020;24(9):1381–1393.
- Cotelli M, Manenti R, Ferrari C, et al. Effectiveness of language training and non-invasive brain stimulation on oral and written naming performance in primary progressive aphasia: a meta-analysis and systematic review. Neurosci Biobehav Rev. 2020;108:498–525.
- Dollaghan CA. The handbook for evidence-based practice in communication disorders. Baltimore: Paul H Brookes Publishing; 2007.
- Simmons-Mackie N, Worrall L, Murray LL, et al. The top ten: best practice recommendations for aphasia. Aphasiology. 2017;31(2):131–151.
- McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38(3):655–662.
- Harvey N, Holmes CA. Nominal group technique: an effective method for obtaining group consensus. Int J Nurs Pract. 2012;18(2):188–194.
- Delbecq AL, Van de Ven AH, Gustafson DH. Group techniques for program planning: a guide to nominal group and Delphi processes. Illinois: Scott Foresman; 1975.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2020;14:1–25.
- Hall WA, Long B, Bermbach N, et al. Qualitative teamwork issues and strategies: coordination through mutual adjustment. Qual Health Res. 2005;15(3):394–410.
- Richards KA, Hemphill MA. A practical guide to collaborative qualitative data analysis. J Teach Phys Educ. 2018;37(2):225–231.
- Cornish F, Gillespie A, Zittoun T. Collaborative analysis of qualitative data. In: Flick U, editor. The SAGE handbook of qualitative data analysis. London: Sage; 2013. p. 10.
- Patton MQ. Variety of qualitative inquiry frameworks: paradigmatic, philosophical, and theoretical orientations. Qualitative research and evaluation methods. 4th ed. Thousand Oaks (CA): SAGE Publications; 2015. p. 109.
- Ruksenaite J, Volkmer A, Jiang J, et al. Primary progressive aphasia: toward a pathophysiological synthesis. Curr Neurol Neurosci Rep. 2021;21(3):1–2.
- Croot K, Nickels L, Laurence F, et al. Impairment‐ and activity/participation‐directed interventions in progressive language impairment: clinical and theoretical issues. Aphasiology. 2009;23(2):125–160.
- Morhardt D, Weintraub S, Khayum B, et al. The CARE pathway model for dementia: psychosocial and rehabilitative strategies for care in young-onset dementias. Psychiatr Clin North Am. 2015;38(2):333–352.
- Holland AL, Nelson RL. Counselling in communication disorders: a wellness perspective. Plural Publishing; 2018. p. 29.
- Worrall L. The seven habits of highly effective aphasia therapists: the perspective of people living with aphasia. Int J Speech Lang Pathol. 2019;21(5):438–447.
- Chapey R, Duchan JF, Elman RJ, et al. Life participation approach to aphasia: a statement of values for the future. ASHA Lead. 2000;5(3):4–6.
- Hughes JC, Bamford C, May C. Types of centredness in health care: themes and concepts. Med Health Care Philos. 2008;11(4):455–463.
- UK Standards for Public Involvement; 2021 [cited 2021 Jul]. Available from: https://sites.google.com/nihr.ac.uk/pi-standards/home