Abstract
Purpose
Studies on functional recovery after pediatric forearm fractures are scarce. Outcome measures are usually (retrospectively) incorporated to compare treatments. How these parameters recover has only rarely fallen within the scope. Aim was to provide insight into “normal recovery” by evaluating how limitations, post-traumatic symptoms, range of motion (ROM) and dexterity recuperate.
Materials and methods
Prospective observational study regarding children 4 and 18 years with a reduced forearm fracture. Limitations, post-traumatic symptoms, ROM, and dexterity were evaluated 6 weeks, 3 and 6 months post-trauma. ROM of the unaffected side was used as a baseline.
Results
Of 54 participants 25.9% and 5.9% perceived limitations after 3 respectively 6 months. Pain, swelling and hypertrichosis were common symptoms. Movements distal from the elbow were restrained 6 weeks post-trauma. Supination and palmar flexion were most affected, followed by dorsal flexion and pronation. Palmar flexion and pronation were still affected after 3 months and associated with treatment invasiveness. Dexterity was diminished at 6 weeks only.
Conclusions
Mild limitations are common. Further investigation of the association between pain, reduced sensitivity and hypertrichosis with treatment invasiveness is warranted. Regarding ROM supination, pronation, palmar and dorsal flexion should be incorporated in future studies. Dexterity is an unsuitable outcome measure.
This study relates to monitoring recovery from pediatric forearm fractures.
Physicians ought to realize that one in four children experience limitations preceding 3 months post-trauma, in which case involvement of a hand therapist should be considered.
Pain, swelling and especially hypertrichosis are common post-traumatic symptoms in children and should on itself not immediately raise concerns for complex regional pain syndrome (CRPS).
To assess recovery of range of motion measuring pronation, supination, dorsal, and palmar flexion is sufficient.
IMPLICATIONS FOR REHABILITATION
Introduction
Forearm fractures are a common pediatric injury accounting for approximately one third (23-42%) of all pediatric fractures [Citation1–8]. In over 80% of cases, the distal forearm is affected. The fracture is situated in the shaft (9–13%) or the proximal radius and/or ulna (2–9%) less often [Citation1,Citation4,Citation9]. The incidence of forearm fractures shows a peak in both genders at the beginning of the prepubertal growth spurt, namely around age 10–11 in girls and 12–14 in boys [Citation1,Citation2,Citation8,Citation10]. A smaller peak incidence for both genders around age 5 has also been described [Citation2,Citation4,Citation7]. Consistently reported is the fact that the vast majority of forearm fractures is sustained by boys [Citation3,Citation4,Citation9,Citation11]. Despite an overall decrease in the incidence of pediatric fractures, especially of the lower extremity, the incidence of forearm fractures has shown an increase over time [Citation2,Citation5,Citation7,Citation10,Citation12]. This is true for forearm fractures as a whole as well as for distal fractures and diaphyseal both-bone fractures specifically [Citation2,Citation5,Citation10,Citation13]. Surely, to this should be added the exceptional situation during the Covid-19 pandemic, during which some studies demonstrated drastic decreases in the number of (forearm) fractures, while others did not [Citation14–16]. Decreases of such are most likely a reflection of the temporary decreases in activities associated with sustainment of fractures, such as sports. This is supported by the fact that the distribution according to fracture location regarding the upper extremity remained very similar [Citation14,Citation15].
Displaced fractures are generally treated by means of closed reduction followed by cast immobilization. Due to the remodeling capacity of bones with remaining growth potential, achieving perfect anatomic alignment in children is not always a necessity [Citation17]. However, the limits of angulation allowing for a conservative course are currently based on scarce (mostly retrospective) studies, case reports and expert opinions. Moreover, although there is no high-level evidence regarding if and when either conservative or operative treatment is superior, a clear trend leaning toward surgical intervention has been observed [Citation18–20]. With more children undergoing surgery, because of an inclined incidence and declined threshold for surgical intervention the question arises as to whether this leads to differences in functional outcome.
Functional outcome after forearm fractures in adults is often described in terms of range of motion (ROM). Similar studies in children are rare and usually describe functional results retrospectively at the end of follow-up, often comparing ROM of the affected hands or pain score of two treatment groups [Citation21–23]. Studies prospectively examining or describing how outcome measures reflecting hand function actually recover themselves, especially in relation to the unaffected hand, are very scarce [Citation24–26]. Furthermore, there seem to be no studies that have prospectively evaluated the presence or recovery of common post-traumatic symptoms, and the same holds true for dexterity.
The aim of this study is therefore to prospectively investigate how several commonly used outcome measures of hand function recover after reduction of forearm fractures in children. More specifically, this study focusses on self-perceived limitations, post-traumatic symptoms, ROM and dexterity. The research questions were as follows:
How many children still experience functional limitations at 3 and 6 months post-trauma, and of what do those exist?
What percentage of children experience post-traumatic symptoms (pain, swelling, redness, hypertrichosis, temperature asymmetry, reduced sensibility and/or allodynia) at 6 weeks, 3 months 6 months post-trauma? Are there differences in the incidences of these symptoms between children undergoing different treatments (closed reduction with or without internal fixation, open reduction)?
Is there a difference in the ROM of the affected side or dexterity of the affected hand in comparison to the unaffected hand at 6 weeks, 3 months and 6 months post-trauma?
Are type of treatment, gender, age, and the dominant hand being the affected hand associated with recovery of either ROM or dexterity?
Methods
Study design
A prospective observational study conducted at University Medical Center Groningen (UMCG). The current study was part of a broader study regarding outcome measures of functional recovery after reduced fractures of the distal upper extremity [Citation26]. Children were invited to participate in line with their first or second follow-up appointment at the hospital, thus usually after cast check-up, change or removal. Families received verbal as well as written information from the researchers on the study’s procedures and purpose. Written informed consent was obtained from the parents or legal guardian, but only after the child had also given consent to participate. The study received a waiver by the Medical Ethical Board of UMCG (M.14.150324).
Participants and procedures
All children and adolescents aged 4–18 years with a reduced displaced radial or both-bone fracture (distal or diaphysis) were invited to participate. The inclusion ran from 1 May 2014 until 1 May 2015. Children with proximal fractures, as well as Monteggia and Galeazzi fractures were excluded. Other exclusion criteria comprised neuromuscular diseases, general bone diseases, conditions interfering with normal growth, or fractures that (possibly) resulted from abuse. Finally, children with bilateral fractures that both met the inclusion criteria and children who could not be examined or followed for logistical reasons were excluded. All participants were invited for three measurements sessions: T1 at 6 weeks, T2 at 3 months, and T3 at 6 months post-trauma. Participants were not measured in the week following cast or osteosynthesis removal. In these cases, measurements were postponed with one week. In order to make participation accessible to all children and parents, home visits were offered when measurement sessions could not be planned for subsequently scheduled follow-up appointments at the hospital.
Outcome measurements
Demographic data (including age, gender, and hand-dominance) as well as fracture-specific information (comprising fracture mechanism, type of fracture, affected side and type of treatment) were registered. Independent researchers not involved in the treatment of the children assessed if the child experienced limitations. Children were asked if there were any activities that they could not perform as well as before, and named examples (dressing, writing/drawing, sports, other). Answers were confirmed by a parent. Thereafter, the researchers examined if there was any swelling, redness, temperature asymmetry or hypertrichosis. A numeric rating scale ranging from 0 (no pain) to 10 (worst pain imaginable) was used to establish the extent of pain. For the pre-school children, a Faces Scale with smileys was used (Wong Baker), as the use of the NRS is limited in children under the age of 8 [Citation27,Citation28]. For older children, the NRS can be considered functionally equivalent to visual scores, with exception of very mild pain [Citation28]. For this reason, the presence of pain was used in analyses rather than the extent of pain. Sensitivity was tested by means of sharp and blunt discrimination using a cotton bud, as well as by identifying left/right differences. The presence of allodynia was questioned with examples of normally non-painful stimuli and investigated with the same cotton bud.
Active ROM of the elbow and wrist and abduction of the thumb were measured with a goniometer. Flexion and extension of the elbow were measured using the lateral olecranon as reference point. Dorsal and palmar flexion of the wrist were measured by placing the goniometer at the dorsum of the wrist, with the lever between metacarpals II and III, whilst keeping the fingers relaxedly flexed. The lunatum was used as point of reference for wrist deviations and abduction of digit I while the handmade full contact with the table. Pronation and supination of the forearm were measured with a pronation/supination inclinometer, with the shoulder in neutral position, the elbow in 90° flexion and the fingers folded into a fist. The unaffected side was measured at the first measurement session as reference value.
Hand dexterity was tested using the nine hole peg test (9-HPT). This is a quick tool to screen dexterity in children that reflects multiple aspects of motor control, such as preshaping the hand, grasping, moving and releasing an object [Citation29,Citation30]. It is widely used amongst hand therapists and is a valid method for testing hand dexterity in children aged 4 years and older with a high inter-rater and test-retest reliability [Citation29,Citation31] Purpose of this test is to insert nine pegs into nine respective holes in a peg board as quickly as possible, then remove them one by one as quickly as possible using one hand. The procedure was followed in accordance with earlier descriptions[Citation29,Citation31]. Both the affected and the unaffected hand were tested at each measurement session. Participants were allowed to practice once with each hand before the actual timed stopwatch test took place.
Statistical analysis
Characteristics of the study population and perceived limitations were described using descriptive statistics. The presence of common post-traumatic symptoms with respect to the different treatment modalities was tested with Fisher’s exact test. Scores of the affected and the unaffected hand for ROM and dexterity were compared using the paired Student t-test after visually ascertaining the normality of data. Finally, mixed-model for repeated measurements analyses were performed to determine if the underwent treatment was associated with the pattern recovery of ROM and/or dexterity over time. Age and gender were added to the models possible confounders. All statistical analyses were performed using SPSS 23.0 for Windows (IBM SPSS Inc., Armonk, NY). Results were considered to be significant if the p-value was ≤0.05.
Results
Patient characteristics
A total of 73 children were treated with reduction for either a radial or a both-bone fracture. A total of 6 children did not meet the inclusion criteria and another 13 children were excluded for other reasons (refusal to participate, logistic reasons, or bilateral fractures that both met the inclusion criteria). The final study population thus consisted out of 54 children, in which a vast majority of 39 fractures (72.2%) was sustained by boys. Closed reduction followed by fixation with Kirschner wires or Nancy nails was the treatment in 23 cases (42.6%), and closed reduction without any means of fixation in 22 cases (40.7%). Open reposition followed by fixation (Kirschner wire, nail or plate) was used in 9 cases (16.7%). A vast majority of 83.3% (N = 45) the children participated in all three follow-up measurement sessions, the remaining 16.7% (N = 9) in two sessions. An enrollment flow diagram is shown in , and a more detailed overview of the study population can be found in . None of the children underwent a rehabilitation course nor hand therapy.
Figure 1. Enrollment flow diagram.
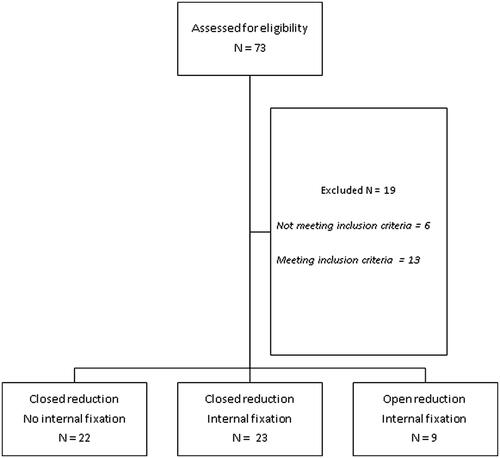
Table 1. Overview of the study population according to fracture type.
Limitations and post-traumatic symptoms
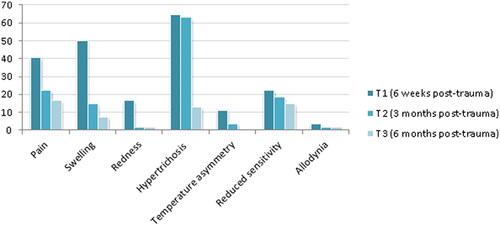
At T1, 25.9% (N = 14) of children still perceived limitations in their daily functioning. Not being able to fully resume sport and being fearful were most reported in 14.8% and 5.6% of cases, respectively. Also mentioned solely were limitations in undressing, writing/drawing, waiving, and one limitation not otherwise specified. At T2, 5.6% (N = 3) children still perceived limitations, none of these were new complaints. All charted post-traumatic symptoms showed a decrease over time, as can be seen in . Swelling (50.0% at T1, 14.8% at T2), pain (40.7% at T1, 22.2% at T2), and especially hypertrichosis (64.8% at T1, 63.0% at T2) showed to be common symptoms in children, with a tendency to persist over a longer period of time. Reduced sensitivity occurred less frequently (22.2% at T1), but showed the least reduction over time (14.8% at T3). Redness (16.7% at T1) and temperature asymmetry (11.1% at T1) were observed more sporadically.
Figure 2. Percentage of children experiencing a specific symptom at T1, T2, and T3.
ROM
For all participants with a unilateral fracture (N = 51), the ROM of the affected side at each measurement sessions was compared to the reference ROM of the unaffected side as measured at the first session. Results showed a significant difference at T1 in detriment of the affected side for pronation and supination of the forearm, dorsal and palmar flexion of the wrist, deviations of the wrist and lateral abduction of the thumb. The most affected movements concerned supination and palmar flexion with an average loss of 18°, followed by dorsal flexion and pronation with an average loss of 15° and 13°, respectively. Palmar flexion and pronation were still significantly affected at T2, although in both cases the difference between the affected and unaffected side was reduced to below 10°. By contrast, all other movements measured had normalized at this point. An extensive overview of the results can be found in .
Table 2. Range of motion and dexterity of affected versus unaffected side.
Dexterity
The difference in dexterity between the affected and unaffected hand was only significant at T1, with a difference of 2.1 s in favor of the unaffected hand. The scores at T2 and T3 were less than 1 s apart, as can be seen in . Moreover, the scores of both hands improved over the measurement sessions, and the difference in score between T1 and T2 was significant for the affected (p < 0.001) as well as the unaffected hand (p = 0.049).
Type of treatment
Time passed after sustainment of the fracture was positively associated with improvement of ROM of all movements, with the exception of extension of the elbow and lateral abduction of the thumb (). Invasiveness of treatment underwent showed a negative association with the recovery of palmar flexion (p = 0.015) and ulnar deviation (p = 0.020). No difference in the pattern of recovery of ROM over time was found for any of the movements between participants who received a different treatment (time × treatment). Time passed and age were positively associated with dexterity of both hands. The course of treatment showed no association with the score of either hand. Results of these mixed-model repeated measurements analysis for ROM and dexterity can be found in .
Table 3. Variables of influence on recovery of ROM and dexterity over time.
Discussion
To our knowledge, this is the first study to prospectively evaluate how self-perceived limitations and common post-traumatic symptoms recover after reduction of pediatric fractures of the forearm. In line with incidence studies, the vast majority of forearm fractures in the current study was sustained by boys (72%) [Citation3,Citation4,Citation9,Citation11]. This was particularly true for the distal radius fractures, of which a staggering 94% was sustained by males. A quarter of children still perceived limitations in their daily functioning 3 months post-trauma. At 6 months, this percentage had decreased to 5.9%. Pain, swelling and especially hypertrichosis are common and lingering post-traumatic symptoms in children. These symptoms are sometimes feared to be associated with complex regional pain syndrome, especially in combination with mobility impairments, as they are part of the Budapest (research) criteria [Citation32]. However, the Budapest criteria are not a validated diagnostic tool for pediatric CRPS and all post-traumatic symptoms do show a clear reduction over time, only affecting a minority of children 6 months post-trauma [Citation33]. The incidence of pain and reduced sensitivity showed a trend corresponding with the invasiveness of treatment. Pain was perceived the least in the CR group at all three measurement sessions (33.3% at T1, 9.1% at T2 and 10.0% at T3), notably increasing in the CRIF group (47.6% at T1, 27.3% at T2, 30.0% at T3) and ORIF group (62.5% at T1, 44.4% at T2, 11.1% at T3). Similarly, reduced sensitivity showed the lowest incidence in the CR group (14.3% at T1, 4.5% at T2, 0% at T3), increasing in the CRIF group (25.0% at T1, 30.4% at T2, 25.0% at T3) and the ORIF group (50.0% at T1, 22.2% at T2, 33.3% at T3). However, these differences between treatment groups were not significant, which is probably due to the low number of children in the ORIF group. As stated before, no other studies evaluating post-traumatic symptoms could be identified, therefore comparison to literature was not possible.
With respect to ROM, except for flexion and extension of the elbow, all movements were significantly restrained at 6 weeks post-trauma. Most affected were supination and palmar flexion, followed by dorsal flexion and pronation. Palmar flexion and pronation were not only still significantly affected 3 months post-trauma, but furthermore significantly associated with the invasiveness of treatment. The ORIF group was associated with the worst outcome for both movements. However, overall loss of ROM for all movements could be considered mild with an average maximum difference below 20°. At 6 months, results evidenced a significant difference in favor of the affected hand for supination, which was an unexpected finding. A possible explanation is that measuring supination with a pronation/supination inclinometer is susceptible to “cheating” by slightly lowering the grip of the fifth digit. Children might figure this out as the measurements progress. Since the reference measurement was not performed again after 3 and 6 months, this might explain the subtle difference favoring the affected hand. A retrospective cohort study conducted in the Netherlands compared ROM of the affected hand with the unaffected hand in children with re-angulated pediatric forearm fractures [Citation22]. For both the re-manipulation and the secondary conservatively treated group they found mild limitations in pronation/supination (4°–6°, respectively), dorsal/palmar flexion of the wrist (2°), and deviations (5°). Our longer-term results at 6 months post-trauma are very similar, amounting to a limitation in pronation/supination of 6°, dorsal/palmar flexion of the wrist of 1°, and deviations of 3°. A systematic review by Westacott et al. (2011) aimed to compare functional outcome following intramedullary nailing versus plate fixation of pediatric diaphyseal both-bone fractures [Citation23]. Unfortunately, due to the large variations between studies statements on significant differences could not be made. In a retrospective study, for the group undergoing open reduction with internal fixation (N = 17) as well as the group undergoing closed reduction with internal fixation (N = 17) group Kar Hao Teah et al. (2009) reported restrictions of less than 10° for pronation and supination of the forearm and negligible restrictions in flexion and extension of the elbow – long-term results again being very similar [Citation21].
To our knowledge, the current study is the first to evaluate recovery of dexterity by using the 9-HPT as an outcome measurement after traumatic injuries of the upper extremity in children. Dexterity of the affected hand showed to be significantly diminished at 6 weeks post-trauma, but no such difference could be ascertained at 3 months or 6 months post-trauma. Moreover, the score of the 9-HPT improved significantly between 6 weeks and 3 months for the affected as well as the unaffected hand. Lastly, no association was found between 9-HPT score and invasiveness of treatment. The improvement in score of both hands between consecutive measurement sessions could very well represent a learning effect rather than a functional improvement. Another possible explanation is simply that scores of the 9-HPT are known to quickly and steadily improve with age, especially during pre-adolescence. This would also explain “age” having a significant influence on the scores of both hands in the mixed-model repeated measurements analysis [Citation31]. All in all, the 9-HPT seems to be an unsuitable test for recovery of hand function after pediatric forearm fractures. Based on these results and earlier research by the same group, we strongly recommend that future studies incorporate grip strength and potentially key grip strength as outcome parameters of recovery after pediatric fractures, as loss of strength has shown to be more prominent and prolonged with a higher invasiveness of course of treatment chosen [Citation26].
A strong point of the current study is that a relatively large variety of physical outcome measurements was evaluated in a prospective setting at set moments in time. The follow-up rate was high, with all children participating in at least two measurement sessions, and the vast majority (83.3%) in all three sessions. The most important limitation is the heterogeneity of the study population with respect to age, type of fracture and treatment, leading to small groups in subgroup analyses, especially in the ORIF group. Still, we could not find a larger prospective study on functional recovery after reduced pediatric forearm fractures. Another limitation is that due to the very high percentage of boys in the study population, girls might be underrepresented. To obtain a larger or less heterogeneous study population, future research should either have a (much) longer duration of inclusion or be multi-center in setup. We hope that this study provides insight into useful outcome measurements.
In conclusion, a quarter of children (25.9%) still perceive limitations in their daily functioning 3 months post-trauma. At 6 months, this percentage decreased to 5.9%. Pain, swelling and especially hypertrichosis are common post-traumatic symptoms in children. Although their presence tends to persist, they only affect a minority 6 months post-trauma. We would advise further investigation of the association between pain, reduced sensitivity and hypertrichosis with treatment invasiveness. All movements distal from the elbow showed to be significantly restrained in comparison to the unaffected side 6 weeks post-trauma. Supination and palmar flexion were affected most severely, followed by dorsal flexion and pronation. Palmar flexion and pronation were affected the longest and, moreover, significantly associated with the invasiveness of the course of treatment chosen. The 9-HPT seems to be an unsuitable test for recovery of hand function after pediatric forearm fractures. Based on earlier research the authors advise incorporating grip strength and potentially key grip strength as outcome parameters in recovery after pediatric fractures instead [Citation26].
Acknowledgments
The authors thank all the children as well as their parents for participating in the current study. The researchers would also like to thank B. Kamies for his assistance with measurements.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- Hedström EM, Svensson O, Bergström U, et al. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81(1):148–153.
- Mäyränpää MK, Mäkitie O, Kallio PE. Decreasing incidence and changing pattern of childhood fractures: a population-based study. J Bone Miner Res. 2010;25(12):2752–2759.
- Lyons RA, Delahunty AM, Kraus D, et al. Children’s fractures: a population based study. Inj Prev. 1999;5(2):129–132.
- Rennie L, Court-Brown CM, Mok JY, et al. The epidemiology of fractures in children. Injury. 2007;38(8):913–922.
- Khosla S, Melton LJ 3rd, Dekutoski MB, et al. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290(11):1479–1485.
- Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6(2):79–83.
- Tiderius CJ, Landin L, Düppe H. Decreasing incidence of fractures in children: an epidemiological analysis of 1,673 fractures in Malmö, Sweden, 1993–1994. Acta Orthop Scand. 1999;70(6):622–626.
- Cooper C, Dennison EM, Leufkens HG, et al. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res. 2004;19(12):1976–1981.
- Alrashedan BS, Jawadi AH, Alsayegh SO, et al. Patterns of paediatric forearm fractures at a level I trauma centre in KSA. J Taibah Univ Med Sci. 2018;13(4):327–331.
- Sinikumpu JJ, Pokka T, Serlo W. The changing pattern of pediatric both-bone forearm shaft fractures among 86,000 children from 1997 to 2009. Eur J Pediatr Surg. 2013;23(04):289–296.
- Brudvik C, Hove LM. Childhood fractures in Bergen, Norway: identifying high-risk groups and activities. J Pediatr Orthop. 2003;23(5):629–634.
- Clark EM. The epidemiology of fractures in otherwise healthy children. Curr Osteoporos Rep. 2014;12(3):272–278.
- Sinikumpu JJ, Lautamo A, Pokka T, et al. The increasing incidence of paediatric diaphyseal both-bone forearm fractures and their internal fixation during the last decade. Injury. 2012;43(3):362–366.
- Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40(8):737–379.
- Nabian MH, Vosoughi F, Najafi F, et al. Epidemiological pattern of pediatric trauma in COVID-19 outbreak: data from a tertiary trauma center in Iran. Injury. 2020;51(12):2811–2815.
- Olech J, Ciszewski M, Morasiewicz P. Epidemiology of distal radius fractures in children and adults during the COVID-19 pandemic – a two-center study. BMC Musculoskelet Disord. 2021;22(1):306–04128-5.
- Kosuge D, Barry M. Changing trends in the management of children’s fractures. Bone Joint J. 2015;97-B(4):442–448.
- Eismann EA, Little KJ, Kunkel ST, et al. Clinical research fails to support more aggressive management of pediatric upper extremity fractures. J Bone Joint Surg Am. 2013;95(15):1345–1350.
- Abraham A, Kumar S, Chaudhry S, et al. Surgical interventions for diaphyseal fractures of the radius and ulna in children. Cochrane Database Syst Rev. 2011;(11):CD007907.
- Vopat ML, Kane PM, Christino MA, et al. Treatment of diaphyseal forearm fractures in children. Orthop Rev (Pavia). 2014;6(2):5325.
- Teoh KH, Chee YH, Shortt N, et al. An age- and sex-matched comparative study on both-bone diaphyseal paediatric forearm fracture. J Child Orthop. 2009;3(5):367–373.
- Roth KC, Denk K, Colaris JW, et al. Think twice before re-manipulating distal metaphyseal forearm fractures in children. Arch Orthop Trauma Surg. 2014;134(12):1699–1707.
- Westacott DJ, Jordan RW, Cooke SJ. Functional outcome following intramedullary nailing or plate and screw fixation of paediatric diaphyseal forearm fractures: a systematic review. J Child Orthop. 2012;6(1):75–80.
- Barvelink B, Ploegmakers JJW, Harsevoort AGJ, et al. The evolution of hand function during remodelling in nonreduced angulated paediatric forearm fractures: a prospective cohort study. J Pediatr Orthop B. 2020;29(2):172–178.
- Colaris JW, Allema JH, Reijman M, et al. Which factors affect limitation of pronation/supination after forearm fractures in children? A prospective multicentre study. Injury. 2014;45(4):696–700.
- Hepping AM, Barvelink B, Ploegmakers JJW, et al. Recovery of strength after reduced pediatric fractures of the forearm, wrist or hand: a prospective study. PloS One. 2020;15(4):e0230862.
- Tomlinson D, von Baeyer CL, Stinson JN, et al. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics. 2010;126(5):e1168-98–e1198.
- von Baeyer CL. Children’s self-reports of pain intensity: scale selection, limitations and interpretation. Pain Res Manag. 2006;11(3):157–162.
- Mathiowetz V, Rogers SL, Dowe-Keval M, et al. The purdue pegboard: norms for 14- to 19-year-olds. Am J Occup Ther. 1986;40(3):174–179.
- Poole JL, Burtner PA, Torres TA, et al. Measuring dexterity in children using the nine-hole peg test. J Hand Ther. 2005;18(3):348–351.
- Smith YA, Hong E, Presson C. Normative and validation studies of the nine-hole peg test with children. Percept Mot Skills. 2000;90(3 Pt 1):823–843.
- Harden RN, Bruehl S, Perez RS, et al. Validation of proposed diagnostic criteria (the “Budapest criteria”) for complex regional pain syndrome. Pain. 2010;150(2):268–274.
- Mesaroli G, Hundert A, Birnie KA, et al. Screening and diagnostic tools for complex regional pain syndrome: a systematic review. Pain. 2021;162(5):1295–1304.
