Abstract
Purpose
Lower limb robotic exoskeletons can assist movement, however, clinical uptake in neurorehabilitation is limited. The views and experiences of clinicians are pivotal to the successful clinical implementation of emerging technologies. This study investigates therapist perspectives of the clinical use and future role of this technology in neurorehabilitation.
Methods
Australian and New Zealand-based therapists with lower limb exoskeleton experience were recruited to complete an online survey and semi-structured interview. Survey data were transposed into tables and interviews transcribed verbatim. Qualitative data collection and analysis were guided by qualitative content analysis and interview data were thematically analysed.
Results
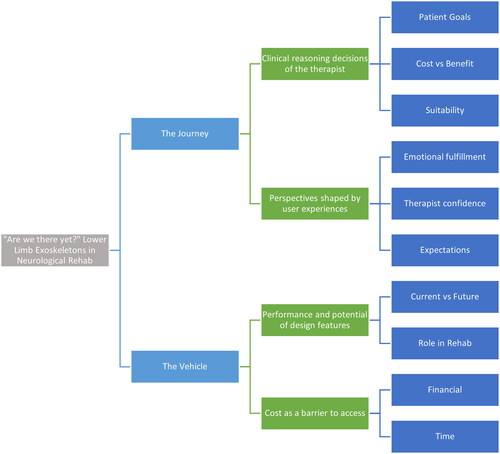
Five participants revealed that the use of exoskeletons to deliver therapy involves the interplay of human elements – experiences and perspectives of use, and mechanical elements – the device itself. Two overarching themes emerged: the “journey”, with subthemes of clinical reasoning and user experience; and the “vehicle” with design features and cost as subthemes, to explore the question “Are we there yet?”
Conclusion
Therapists expressed positive and negative perspectives from their experiences with exoskeletons, giving suggestions for design features, marketing input, and cost to enhance future use. Therapists are optimistic that this journey will see lower limb exoskeletons integral to rehabilitation service delivery.
Implications for Rehabilitation
Further innovation of design features, marketing, and cost are needed to enhance ongoing development and integration.
Routine clinical implementation of lower limb exoskeletons is unlikely at this time in Australia and New Zealand.
Therapists do expect lower limb exoskeletons to have an ongoing role in future rehabilitation.
Introduction
Neurological conditions such as spinal cord injuries, acquired brain injuries, and degenerative conditions, are associated with the substantial personal and financial burden. The global incidence of spinal cord injury (SCI) was estimated in 2013 by the World Health Organisation (WHO) to be up to 500,000 cases per year [Citation1]. Acquired brain injury (ABI) has been reported amongst the top causes of disability worldwide [Citation2,Citation3]. As a group, neurological disorders were classed as the top global cause of disability-adjusted life years between 1990 and 2016 [Citation4], and incidence has continued to rise with the ageing population [Citation4]. A contributor to the neurological disease burden is incomplete functional recovery and ongoing mobility impairment [Citation3,Citation5]. In recent years, we have seen advances in the development of lower limb robotic exoskeletons for use in rehabilitation, with the aim of bettering these recovery outcomes [Citation6]. Robotic lower limb devices facilitate functional task practice in weightbearing, with notably less manual handling for therapists [Citation3,Citation7]. Patient experiences using these devices have been largely positive [Citation8,Citation9]; however, adoption into routine clinical practice has not yet occurred. As clinicians are likely to influence this process, evaluation of their perceptions of potential barriers and enablers to the use of exoskeletal therapy is needed [Citation10].
Neurological rehabilitation typically involves high volumes of functional task practice to stimulate neurological recovery [Citation11]. Mobility is a key treatment area, focussing on increased independence as well as the prevention and management of secondary complications such as pressure areas, muscle atrophy, and cardiovascular diseases [Citation7,Citation9,Citation12]. Treatment sessions may involve whole task practice such as gait-retraining and sit-to-stand as well as the part practice of stepping, standing, balance, and weight shift. These tasks may place a heavy physical burden on therapists when treating highly impaired patients [Citation3]. In some cases, multiple therapists may be required for the manual handling of a single patient to support their trunk posture and lower limb movement through the gait cycle [Citation3].
A lower limb robotic exoskeleton is a mechanised device which has powered joints [Citation13]. Several different lower limb exoskeletons have been developed, with gait training, sit-to-stand, stepping, and stair practice functions, requiring less therapist assistance [Citation7]. This may reduce the burden on therapists whilst maximising training volume [Citation3,Citation14]. Preliminary studies evaluating short-term benefits support therapeutic implementation in patients with spinal cord injury, acquired brain injury (including stroke), cerebral palsy, Parkinson’s disease, and multiple sclerosis [Citation3,Citation14,Citation15]. Short-term benefits in walking capacity, 6 min walk test, 10 m walk test, and timed up and go have been reported following robotic exoskeleton use [Citation3,Citation9], as well as improvements in lower limb motor function [Citation16]. Whilst these findings are encouraging, evidence has not shown exoskeleton use to be superior to traditional methods [Citation3]. A 2018 systematic review of the evidence for use in the ABI population found that whilst improvements in some functional outcomes such as balance and walking speed were achieved, this benefit was not superior when compared with conventional therapy [Citation3]. Findings also indicated a large degree of heterogeneity amongst studies, potentially masking the benefits in more specific populations [Citation3]. As research interest continues to grow, it is likely that the evidence base for these devices will become more conclusive, and therefore further research is needed into the perspectives of those who will use such technology clinically.
Despite the postulated benefits and a growing body of research investigating their use, clinical implementation is in its infancy, and in Australia and New Zealand, there are no guidelines for the implementation of this technology. A lack of long-term studies, and limited evidence of this technology’s superiority to current management, may contribute to this. Additionally, access to these devices is limited. Although numerous devices have been marketed worldwide, at the time of conducting this study, only two types had been used clinically in Australia and New Zealand, The REX [Citation17] and Rewalk [Citation18] (one REX in New Zealand, two REX in Australia, and three ReWalk in Australia), and clinics using them were all located in metropolitan areas. Cost is likely a limiting factor to distribution, with lower limb robotic exoskeletons reported to cost between $33,000 USD and $160,000 USD for larger multi-joint devices [Citation7,Citation19,Citation20]. In some rehabilitation settings, early budget analysis has shown the possibility of these devices to reduce the overall costs of treatment, potentially justifying expenditure [Citation19]. But, due to high variability between sites and treatment comparisons, further cost-benefit analysis is needed. Whilst cost may be a current barrier to personal ownership and use, increased competition and clinical uptake are likely to change this [Citation13,Citation19]. Overall, an important step in the clinical implementation process is the identification of the therapist perceived barriers and enablers to use [Citation10], which requires further exploration.
In a previous study by Hochstenbach-Waelen and Seelen [Citation10], therapists were interviewed to determine factors likely to influence their clinical acceptance of an upper limb robotic device. The main findings were grouped into “therapy-related criteria”, such as specificity, variability, and intensity of exercise features, “software-related criteria”, such as the difficulty of operation, ability to record results and provide feedback and “implementation-related criteria” such as evidence base, speed of use, patient acceptability and cost [Citation10]. Amongst these criteria, evidence of effectiveness was reported to have a strong influence on clinical reasoning for use of the device in daily practice [Citation10]. Two recent studies support these clinical priorities and have highlighted the need for clinicians to be involved in the research and development process for lower limb exoskeletons [Citation21,Citation22]. These findings highlight the role of therapists as key stakeholders in the clinical application of robotic exoskeletons, holding valuable clinical experience for the assessment of device performance [Citation10], and feedback to inform implementation [Citation23].
The limited clinical use of lower limb exoskeletons in neurorehabilitation in Australia and New Zealand prompted our preliminary investigation into the perceptions and attitudes of therapists, with lived experience of using an exoskeleton, regarding this intervention as a component of neurological rehabilitation with the aim of answering the following questions:
What are therapists’ perceptions of therapeutic lower limb robotic exoskeletons based on their experience of using them?
What are the therapist’s expectations about the future role of therapeutic lower limb robotic exoskeletons in neurorehabilitation?
Methods
This study involved semi-structured interviews with therapists experienced in using lower limb robotic exoskeletons. Qualitative content analysis [Citation24,Citation25] was used to guide data collection and analysis as this approach was congruent with our aim of gaining an in-depth understanding of therapist attitudes and beliefs.
Participants
Participants were recruited through expressions of interest, in response to advertisements of the study. Recruitment letters were sent to the three existing lower limb robotic exoskeleton distributors in Australia and New Zealand, “Making Strides” [Citation26], “Rex Bionics” [Citation17], and “Mobility Solutions Centre” [Citation27]. Additionally, a number of organisations known to have had access to demonstrations of exoskeletons were contacted, including the Spinal Cord Injury Association [Citation28], Neuromoves [Citation29], and Multiple Sclerosis Research Australia [Citation30]. Private neurological physiotherapy practices using either of the devices trialled in Australia and New Zealand, REX [Citation17] and ReWalk [Citation18], were also contacted. Therapists were eligible to participate if they had prior experience using an exoskeleton with at least one patient, either clinically or in research. Therapists from both Australia and New Zealand were included, due to similarities in health systems and service delivery. The sample size was anticipated to be small, due to the limited number of available therapists experienced in the use of lower limb robotic exoskeletons.
Data collection
Volunteers were asked to complete an online survey using RedCap [Citation31] data collection software (see Appendix 1), to obtain demographic information about participants, and information about their level of the overall experience, and more specifically with lower limb robotic exoskeletons. This was followed by a semi-structured interview via the Zoom [Citation32] telecommunication platform. Interviews were conducted by NP (a PhD candidate) and JB (a fourth-year Physiotherapy Honours student), who were trained by an expert in qualitative methodology (LW). NP led the interviews using an interview guide (see Appendix 2), whilst JB took field notes. Interviews were audio-recorded and transcribed verbatim by a member of the research team. Participants were assigned pseudonyms in the transcription process to deidentify the data. Field notes were also documented during each session to capture non-verbal and contextual information was recorded. Process and reflection diaries were used throughout, to track decision-making and facilitate reflexivity in the data collection and analysis [Citation33]. Data collection and analysis occurred concurrently, with interview questions adjusted between participants to explore emerging perspectives as necessary.
Data analysis
Survey data were deidentified and downloaded into an excel spreadsheet with each variable reported as medians and ranges. These data were transposed into tables for comparison. Interview transcripts were read by a member of the research team, whilst simultaneously listening to the audio recording and consulting field notes. Data were then read phrase by phrase with initial codes of meaning allocated to each phrase. Data analysis was conducted by two researchers (NP and JB) independently and emerging thematic ideas discussed with the research team as a whole so that a range of perspectives could be considered. Following this, a third reading was performed by the entire research team, reviewing the original data, codes of meaning, and emerging analysis to ensure varied perspectives were considered. Gradually through a dialogical process between the analysis and the data, themes, and subthemes emerged. Data were managed using NVivo 12 software [Citation34].
Ethics approval
This project was approved by the University of Newcastle Human Ethics Committee (Reference number: H-2020-0045) and informed written consent was obtained from all participants. All data from focus group recordings and survey responses were kept secure under password protection with access only by the research team. All online survey, interview, and focus group data were de-identified prior to data analysis. Data collection occurred during August and September 2020.
Results
Participants
Nine therapists responded to recruitment advertisements expressing their interest. Two therapists failed to respond to further correspondence, two were unable to schedule an interview due to time constraints and the remaining five therapists were recruited to complete the online survey and interview. The five participants represented four of the five clinics in Australia and New Zealand known to have some experience with an exoskeleton. The clinic which wasn’t represented had one staff member who had received the training with an exoskeleton but had not used it since then. Four participants had used the REX and one had used the ReWalk, all in a clinical, private practice setting. Participant information can be found in .
Table 1. Participant information.
All participants reported completing training with an exoskeleton more than 12 months prior to the study. Two participants had access to the device for a period of only 1–3 months, whereas the remaining three participants had access for greater than 12 months. Two therapists reported using the device very infrequently, whilst one reported regular use and the remaining two reported very regular use. As shown in , those reporting more regular use and access to the exoskeleton for more than 12 months, also reported higher levels of confidence using the device. The exoskeleton was reported to be most commonly used with the spinal cord injury patient population. One therapist also reported commonly using the exoskeleton with stroke, brain injury, multiple sclerosis, Parkinson’s disease, and Friedrich’s ataxia presentations. illustrates varying perspectives of patient suitability, enjoyment, and predicted future use.
Table 2. Frequency, access and confidence with robotic lower limb exoskeleton use.
Table 3. Suitability and enjoyment of robotic lower limb exoskeleton use.
Thematic analysis
Analysis of interview transcripts revealed the overarching concept of “Are we there yet?”, where the implementation of these devices is an evolving process. Two key themes exist within this process: the human element, being the “Journey” of implementation, and the mechanical element as the “Vehicle” in which the journey is taking place on its way to the final destination. These themes and concepts are depicted in .
Theme 1: the journey of implementation
For those with access to an exoskeleton, a clinical application brought many opportunities and challenges. The decision to use this intervention with a patient included consideration of patient goals and preferences, available time, potential therapeutic benefits, and therapist preferences. The interplay of experiential factors led to the emergence of two key subthemes: clinical reasoning decisions of the therapist and perspectives shaped by user experiences.
Subtheme 1.1: clinical reasoning decisions of the therapist
All therapists discussed the need for the exoskeleton to align with the patient’s goals and for treatment benefits to justify the time required for set up, transferring, and measuring. Therapists felt that the exoskeleton facilitated goal-based treatment by providing additional therapy options and opportunities to challenge and motivate patients in upright standing and/or walking, whilst being able to be hands-off when the device was static.
“If you’re going to do it [use an exoskeleton], you’ve got to have a really good reason for doing it…You have to have really strong goals” (Participant 2, regular exoskeleton user)
Decisions regarding patient suitability were also influenced by individual characteristics and the patient’s neurological condition. Bone density and the presence of autonomic dysreflexia were considerations. Behavioural changes and communication deficits also influenced therapist decisions about usability. In particular, the patient’s ability to follow instructions and provide ongoing consent were important. No formal assessment of these considerations was mentioned.
“I've had some people with some pretty severe cognitive impairments in it… the safety part is, if they are able to consistently communicate … ‘I want to stop’.” (Participant 1, very regular exoskeleton user)
The presence of spasticity, patient tolerance and anxiety were also considered in decisions to continue or discontinue use.
Sub-theme 1.2: perspectives shaped by user experiences
Therapists clearly expressed both positive and negative perspectives of exoskeleton use as part of their user experience. Positive experiences included increased engagement and enjoyment from both the patient and the therapist, being up to date with the latest technology, and emotional satisfaction of facilitating activities that were previously unachievable.
“The first time you stand every single person up is super emotional… super emotional. It’s the best part of doing it.” (Participant 5, very regular exoskeleton user)
“Therapy is beautiful with it because most of them… just want to walk, like that’s what they all say… “I just want to walk. I don’t care if it’s in a in a robot. I just want to walk”” (Participant 5, very regular exoskeleton user)
Additionally, perceptions were shaped by the frequency of use and familiarity with the device, with some commenting that they felt their confidence would improve with more frequent use.
“She’ll [other therapist] challenge people in it [the exoskeleton] you know… she really made more of it than we were in a position to do so because she was so familiar with it and had had [access to the exoskeleton] so long.” (Participant 4, very infrequent exoskeleton user)
Therapists’ confidence in using the exoskeleton was also shaped by their negative user experiences. One participant described an event of postural hypotension whilst the patient was in the device, explaining that it increased their confidence as the safety protocols were easy to complete and safe.
You know it’s all safe. I had someone completely pass out in the REX… he [the patient] was a C4 [SCI level of injury] … he was six foot … so he wasn’t the smallest person to pass out in the REX as well and, you know, we just did what we had to do, sit the REX down and … the REX had him. (Participant 1, very regular exoskeleton user)
Other participants described instances where the device became unstable due to uneven flooring, negatively impacting their confidence due to concerns over patient safety and the potential cost of damage to the device.
“So that rubber spongy floor was a no go for the REX. The carpet was okay but… it had slight unevennesses that we couldn’t see with the eye, but that made the REX almost tip over.” (Participant 3, very infrequent exoskeleton user)
“If the REX falls over… I don’t own it and it’s $150,000 worth of equipment.” (Participant 1, very regular exoskeleton user)
Some participants also felt the physical characteristics of the therapist also contributed to their confidence.
“You need to be like a physically strong competent, confident person to even stand people safely … Unfortunately, smaller people with a lower strength base just aren’t usually clinically appropriate in case something does go wrong” (Participant 5, very regular exoskeleton user)
Participants reported that patients often had over inflated hopes and expectations prior to using the devices.
“Unfortunately, clients have an often… unrealistic view [of what the device can do] initially… but once they’ve been educated on it clients get their head around it very quickly.” (Participant 1, very regular exoskeleton user)
Some participants attributed this to marketing strategies; however, it was agreed that this could be easily managed through education.
Theme 2: the vehicle
As the vehicle within which the journey takes place, participants shared experiences with two types of lower limb robotic exoskeletons: REX and ReWalk. Two recurring themes included current and future device features and cost as a barrier to access.
I’d love [the devices] to be cheaper. I'd love it to be more people using them… I would love the device to be better and more functional and everything. But I think we’re dealing with what we are right now…if more people are using them, there’s more… products on the market. And if they were cheaper… I would love that. I would welcome the competition. And I think it’d be better for everyone. (Participant 5, very regular exoskeleton user)
These subthemes were discussed with particular emphasis on accessibility, usability, and improvements for the future.
Sub-theme 2.1: performance and potential of design features
Design features were discussed by all therapists regarding the usability of current models, and preferred changes for future models. All participants found the current features to be beneficial, however, identified existing scope for improvement, such as REX’s ability to complete overground stepping and walking but becoming unstable with any uneven surface. ReWalk’s ability to be used remotely, in the community for outdoor mobility, and in a clinical setting, was praised as a feature that increased the accessibility of gait training in the neurological population.
“Quite a few remote users … They’re not close to any other clinical resources or clinicians and so they can use it [the exoskeleton] in a small country town, they can safely do some rehab.” (Participant 5, very regular exoskeleton user)
But it was also acknowledged that the device excluded patients without upper limb function, with the device requiring the use of crutches.
Participants reported that the variety of dynamic standing and weightbearing tasks made possible by the exoskeletons provided increased treatment possibilities. For example, when comparing current exoskeleton functionality to the exercise options achievable with a standing frame, one participant stated,
“I always use single leg stance or some kind of movement… I would very rarely just stand the patient because yes, then I would just use a standing frame.” (Participant 2, regular exoskeleton user)
Participants anticipated that lower limb exoskeletons will have an ongoing role in the future of neurological rehabilitation. Increased clinical input for device development was highlighted as an opportunity for improved device design and therefore usability, with features such as biofeedback, variable assist, functional electrical stimulation, smaller device size and weight, increased gait speed, increased stability, and a modular design agreed to add value to future models. When describing device stability, one participant expressed the desire for future models to require less stand-by assistance, stating,
“You would hope that you could finally step away and look at the client from a step apart. Because we always spot [support the patient], we’re always there holding them when they walk so to be able to step away… and watch for a moment would be great benefit.” (Participant 3, very infrequent exoskeleton user)
Some participants reported encountering feelings of concern about job security from other therapists, who had not used an exoskeleton, related to robots replacing therapists in the future.
“I often can feel quite sad that I spend a lot of time defending what the REX can do, and actually, robotics in general… there’s a lot of fear still… ‘It can’t do this; it can’t do that. Is it going to take my job?’… and I think I spent a lot of time defending that it’s [the exoskeleton] it’s got some amazing potential, and it’s not perfect but you know it’s got some amazing potential.” (Participant 1, very regular exoskeleton user)
Despite this, none of the therapists reported this as a concern after using the devices.
“For us, it actually didn’t reduce manpower at all.” (Participant 3, very infrequent exoskeleton user)
All participants reported feeling that whilst technology may improve, the therapist will always be involved in the treatment process.
“It is a therapeutic tool. It’s not ever going to replace a therapist.” (Participant 1, very regular exoskeleton user)
This perspective of therapist involvement remained consistent when describing exoskeleton use in the community and those purchased privately by patients.
Sub-theme 2.2: cost as a barrier to access
Cost was identified as a key barrier to access and long-term use, for both clinics and patients. “Cost” not only included the direct financial burden of purchasing, using, and maintaining the device, but also the time required for training, set up, measuring, and cleaning. Working in private practice, all participants reported being unable to access funding from government bodies to purchase a device. Four participants reported that without a larger organisation (either the manufacturer or a not-for-profit organisation) loaning them a device at no cost, their clinic would not have had access to the exoskeleton.
“At this price of $150,000. No, I don’t think, and I can’t see how private clinics would get him [the exoskeleton] … unless they’re of a bigger organization” (Participant 1, very regular exoskeleton user)
This perception of cost as a barrier did not change after experiencing clinical use of the exoskeleton. Participants reported that their practice still would not be able to justify the cost.
“You’d have to go in with a really business approach, which I don’t like… then you’re going to be picking therapy based on pricing.” (Participant 2, regular exoskeleton user)
This price restriction also constrains the purchase of exoskeletons by individual patients for personal use.
“You get to speak to so many people about what the ReWalk can do, and it attracts a lot of people in. And then you get to the sticky point in the conversation about the price point and that automatically rules, you know, 90% of them out.” (Participant 5, very regular exoskeleton user)
In addition to direct costs of purchase, the indirect cost of time was a recurrent concern with therapy delivered with exoskeletons requiring additional time for measuring and set up, as well as clinics bearing the costs of therapists missing clinical time to complete device training.
“You almost need half an hour before you see that client to set it up. And that’s a big downfall… because I don’t have that half hour.” (Participant 3, very infrequent exoskeleton user)
The need for increased mainstream use or acceptance by funding bodies was a common perspective shared by participants in order to reduce the cost and increase patient access.
Discussion
The concept of “Are we there yet?” explored in this study illustrates that whilst the use of exoskeletons in neurorehabilitation can contribute positively to therapy in selected cases, the journey to reaching their full potential is ongoing. The derived human and mechanically-based themes offer an experience-based insight into key clinical reasoning decisions, the user experience, the practicality of design features, and cost in the clinical setting as current barriers and enablers to use.
Therapists’ clinical reasoning decisions were based on a cost-benefit analysis of each patient scenario. As an adjunct to therapy, the exoskeleton needed to meet expected “criteria” and the benefit of treatment needed to outweigh the additional time costs and environmental challenges. This finding corresponds to Hochstenbach-Waelen and Seelen’s [Citation10] proposed “therapy-related criteria”, whereby alignment with patient goals and cognitive ability is considered integral in clinical reasoning, to determine the suitability of the exoskeleton for each individual. Interestingly, elements of the “software and hardware-related criteria” listed, such as adjusting the device to each patient being “quick and easy” [Citation10], were also raised by participants of this study and were considered to be needs that have not yet been addressed. The time required to set up and prepare the device and patient may result in the decision not to use the device, as this impacts negatively on the cost-benefit component of the clinical reasoning process [Citation22]. We also postulate that it is pertinent to objectively evaluate a patient’s suitability to use this type of treatment modality, and formalise the evaluation of particularly cognition, bone density, and the impact of autonomic dysreflexia on a patient, given some of the reported adverse events whilst using an exoskeleton. For this reason, a clinical reasoning tool specific to the use of lower limb exoskeletons would be clinically useful, and further research is required to hone in on which patient types are most suitable for each device.
The “user experiences” of therapists contributed positively and negatively towards their perspectives of exoskeletons. Consistent with the findings of Heinemann et al. [Citation35], facilitation of upright standing and gait retraining was found to contribute to emotional fulfilment for both patients and therapists when aligned with patient goals. Key components of therapist’s user experiences contributing to positive perspectives included increased patient and therapist engagement and facilitation of functional retraining options in standing for patients otherwise unable to participate. To date, multiple studies [Citation8,Citation35,Citation36] have highlighted the positive psychological impacts of eye-level gaze in a population that is primarily wheelchair-bound. This indirect benefit, as well as the increased variability in treatment described by this study, contribute positively to the user experience.
User experiences also impacted negatively on therapist perspectives. Wolff et al. [Citation37] listed four key priority areas influencing potential use as falls risk, cost, user comfort, and ease of transfers [Citation37]. When compared to the experiences of our participants who had used exoskeletons in practice, and those in a recent Canadian study [Citation22], a number of similar areas were highlighted as barriers, indicating a need for ongoing innovation. Issues of stability, the risk of the device falling over on uneven surfaces, and the impact of cost on accessibility in particular, were repeatedly described by our participants as negative factors. The discord reported in this study between patients’ expectations and the reality of device offerings were consistent with previous findings [Citation22,Citation38]. Participants reported this as a contributor to negative patient perceptions of exoskeletons. This indicates a need for more appropriate marketing and education surrounding the use of these devices. Participants in this study reported that patients responded well to therapist education, however more informative advertisement from the outset may reduce false expectations [Citation39].
The current device features such as dynamic standing, upright standing and gait training reportedly add benefit to therapy interventions. Conversely, device limitations of weight, instability, and the need for hands-on or stand-by assistance serve as barriers to implementation. The perspectives shared in this study reiterated those of previous studies [Citation21,Citation22,Citation38,Citation39], calling for increased clinical input into the design phase of exoskeleton development to maximise functionality for end users. Suggestions for future features explored in this study were consistent with those reported by Heinemann et al. [Citation35], particularly the integration of functional electrical stimulation, increased stability and terrain options and improvements in fitting the device to the user. Despite these limitations, therapists remained optimistic that exoskeletons will have a future role in neurological rehabilitation and welcomed the prospect of continued improvements to maximise patient outcomes.
Cost remains a key consideration in future device models with a balance to be found between broadening inclusion criteria and maximising treatment value, without adding significant manufacturing costs. Design features and improved functionality become irrelevant if neither therapy services nor patients can afford the device. The disconnect between current limitations of cost and clinical reasoning considerations for application serves as a barrier to further implementation of exoskeletons into practice. As exoskeletons operate as adjuncts to therapy, it is not currently feasible for most Australian or New Zealand-based private practices to outlay the financial costs of purchasing, maintaining, and training. Fritz et al. [Citation39] emphasised the consideration of device inclusion/exclusion criteria, magnifying the divide between cost and benefit with a niche population of patients suitable for use, particularly when alternative adjunct therapies may yield similar or better results [Citation3]. It seems that the implementation process is caught in a cyclical problem of technology needing enough sales to reduce costs, whilst the initial cost is too high to facilitate sales. The requirement to address affordability has been previously recognised [Citation22,Citation37,Citation39] and resonated with our participants who would like more clinical input into marketing strategies and liaising with funding bodies. Australia is geographically vast with a comparatively small population and is isolated from countries responsible for the manufacturing and servicing of the included devices. The authors postulate that this, coupled with the barriers to implementation mentioned in this study, as well as previous literature, put Australia in a challenging position in terms of the implementation of this technology. Despite reporting clinical benefits and foreseeing even greater potential benefits in the future, most participants reported they could not justify the cost of purchasing their own exoskeleton which emphasises the significance of the cost barrier to implementation.
Strengths and limitations
Clinical uptake of lower limb exoskeletons in Australia and New Zealand is low, and the population of therapists experienced in exoskeleton use is small. Whilst this resulted in a small sample size, it can be argued that relative to the target population, the sample is sufficiently large to gain in-depth insight into the perceptions of the target groups. This study included therapists experienced in the use of both types of exoskeletons currently in use in Australia and New Zealand. This ensures a broad perspective of therapist perceptions not limited to the experience of a singular model. It was not feasible to interview participants more than once over time, which may have provided a more thorough insight into their perspectives. Additionally, within the sample, there was only one male participant compared to four female participants which may not be representative of the ratio of therapists working in neurorehabilitation. However, the transferability of the findings is strengthened by the provision of demographic data, allowing an indication of the population encompassed by our sample.
Conclusions
In the journey of implementation of robotic lower limb exoskeletons into routine practice, significant opportunity for growth remains. Participants reported favourable experiences as well as obstacles to implementation. As key stakeholders, these clinicians offered practical suggestions for design features, marketing input, and cost to enhance ongoing development and widespread integration of exoskeletons into practice. It is clear that therapists expect this technology to have a role in future therapy and remain optimistic that whilst the journey is still ongoing, the end destination will see lower limb exoskeletons as an integral part of rehabilitation service delivery.
Author contributions
NP proposed the study which was then designed in collaboration with JB, LW and JM. NP and JB conducted the data collection with analysis conducted by NP, JB, LW and JM. NP and JB prepared the manuscript with edits proposed by LW, JM, NS and AB. All authors have reviewed and approved this manuscript.
Supplemental Material
Download MS Word (495.2 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- World Health Organisation. Spinal cord injury. 2013 [cited 2020 Apr 18]. Available from: https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- Whyte E, Skidmore E, Aizenstein H, et al. Cognitive impairment in acquired brain injury: a predictor of rehabilitation outcomes and an opportunity for novel interventions. PM R. 2011;3(6 Suppl 1):S45–S51.
- Postol N, Marquez J, Spartalis S, et al. Do powered over-ground lower limb robotic exoskeletons affect outcomes in the rehabilitation of people with acquired brain injury? Disabil Rehabil Assist Technol. 2019;14(8):764–775.
- Bannick MS, Beghi E, Blake N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18:459–480.
- Hartigan C, Farris R. The futire promise of lower limb robotic exoskeletons. J Nurse Life Care Plan. 2015;15:854–859.
- Viteckova S, Kutilek P, Jirina M. Wearable lower limb robotics: a review. Biocybern Biomed Eng. 2013;33:96–105.
- Esquenazi A, Talaty M, Jayaraman A. Powered exoskeletons for walking assistance in persons with central nervous system injuries: a narrative review. PM R. 2017;9(1):46–62.
- Manns PJ, Hurd C, Yang JF. Perspectives of people with spinal cord injury learning to walk using a powered exoskeleton. J Neuroeng Rehabil. 2019;16:94.
- Shackleton C, Evans R, Shamley D, et al. Effectiveness of over-ground robotic locomotor training in improving walking performance, cardiovascular demands, secondary complications and user-satisfaction in individuals with spinal cord injuries: a systematic review. J Rehabil Med. 2019;51(10):723–733.
- Hochstenbach- Waelen A, Seelen HAM. Embracing change: practical and theoretical considerations for successful implementation of technology assisting upper limb training in stroke. J Neuroeng Rehabil. 2012;9:52–52.
- Carr J. Neurological rehabilitation: optimising motor performance. 2nd ed. Edinburgh: Churchill Livingstone; 2010.
- Nas K, Yazmalar L, Şah V, et al. Rehabilitation of spinal cord injuries. World J Orthop. 2015;6(1):8–16.
- Gorgey AS. Robotic exoskeletons: the current pros and cons. World J Orthop. 2018;9(9):112–119.
- Calabrò R, Cacciola A, Bertè F, et al. Robotic gait rehabilitation and substitution devices in neurological disorders: where are we now? Neurol Sci. 2016;37(4):503–514.
- Palermo AE, Maher JL, Baunsgaard CB, et al. Clinician-focused overview of bionic exoskeleton use after spinal cord injury. Top Spinal Cord Inj Rehabil. 2017;23(3):234–244.
- Tsai C-Y, Delgado AD, Weinrauch WJ, et al. Exoskeletal-assisted walking during acute inpatient rehabilitation leads to motor and functional improvement in persons with spinal cord injury: a pilot study. Arch Phys Med Rehabil. 2020;101(4):607–612.
- Rex Bionics. REX product information. 2019 [cited 2019 Oct 30]. Available from: https://www.rexbionics.com/product-information/
- ReWalk Robotics. ReWalk. 2019 [cited 2019 Sep 18]. Available from: https://rewalk.com/
- Pinto D, Garnier M, Barbas J, et al. Budget impact analysis of robotic exoskeleton use for locomotor training following spinal cord injury in four SCI model systems. J Neuroeng Rehabil. 2020;17:4–4.
- Rupal BS, Rafique S, Singla A, et al. Lower-limb exoskeletons: research trends and regulatory guidelines in medical and non-medical applications. Int J Robot Syst. 2017;14:1–27.
- Vaughan-Graham J, Brooks D, Rose L, et al. Exoskeleton use in post-stroke gait rehabilitation: a qualitative study of the perspectives of persons post-stroke and physiotherapists. J Neuroeng Rehabil. 2020;17:123.
- Mortenson WB, Pysklywec A, Chau L, et al. Therapists’ experience of training and implementing an exoskeleton in a rehabilitation Centre. Disabil Rehabil. 2020;44:1–7.
- Lam MY, Tatla SK, Lohse KR, et al. Perceptions of technology and its use for therapeutic application for individuals with hemiparesis: findings from Adult and Pediatric Focus Groups. JMIR Rehabil Assist Technol. 2015;2(1):e1.
- Sandelowski M. What’s in a name? Qualitative description revisited. Res Nurs Health. 2010;33(1):77–84.
- Sandelowski M. Whatever happened to qualitative description? Res Nurse Health. 2000;23:334–340.
- Making Strides. The making strides experience: ReWalk exoskeleton. [cited 2020 June 3]. Available from: https://www.makingstrides.com.au
- ReWalk Robotics. Rewalk: Distribution and Point of Sale. [cited 2020 June 10]. Available from: https://rewalk.com/locations/mobility-solutions-centre-dunedin/
- Spinal Cord Injuries Australia. [cited 2020 Oct 28]. Available from: https://scia.org.au
- Spinal Cord Injuries Australia. Neuromoves: specialised exercise therapy for improved health, mobility and independence. [cited 2020 Oct 28]. Available from: https://scia.org.au/neuromoves-exercise/
- MS Research Australia. [cited 2020 Oct 28]. Available from: https://msra.org.au
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- Zoom Video Communications Inc. About Zoom. [cited 2020 June 3]. Available from: https://zoom.us/about
- Fisher K. The qualitative interview and challenges for clinicians undertaking research: a personal reflection. Aust J Prim Health. 2011;17(1):102–106.
- QSR International. Nvivo. [cited 2020 June 3]. Available from: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/about/nvivo
- Heinemann AW, Jayaraman A, Mummidisetty CK, et al. Experience of robotic exoskeleton use at four spinal cord injury model systems centers. J Neurol Phys Ther. 2018;42(4):256–267.
- Thomassen GK, Jorgensen V, Normann B. “Back at the same level as everyone else”-user perspectives on walking with an exoskeleton, a qualitative study. Spinal Cord Ser Cases. 2019;5(1):103.
- Wolff J, Parker C, Borisoff J, et al. A survey of stakeholder perspectives on exoskeleton technology. J Neuroeng Rehabil. 2014;11:208–229.
- Hill D, Holloway CS, Morgado Ramirez DZ, et al. What are user perspectives of exoskeleton technology? A literature review. Int J Technol Assess Health Care. 2017;33(2):160–167.
- Fritz H, Patzer D, Galen SS. Robotic exoskeletons for reengaging in everyday activities: promises, pitfalls, and opportunities. Disabil Rehabil. 2019;41(5):560–563.