ABSTRACT
Introduction: Studies in Western countries show that VTE recurrent rates are lower in the presence of a transient provoking factor, older age, female sex and/or hormonal use, while thrombophilia (factor V Leiden or prothrombin mutation) has no predictive role. This study aimed to determine the incidence and risk factors of recurrent VTE in Asian patients.
Method: This is a retrospective cohort study in adult VTE patients who were diagnosed during 2004–2014, had no active cancer and followed-up for at least 1 year.
Results: There were 198 patients. The mean age was 58.2 ± 17.6 years and 68.2% were female. The diagnoses were deep vein thrombosis (56%), pulmonary embolism (32%) or both (12%). They were provoked by major surgery in 21.7%. Thrombophilia (antiphospholipid syndrome or protein C or protein S deficiency) was found in 11.6%. The recurrent rate during the median follow-up time of 52 months was 2.2 (95% confidence interval [CI] 1.46–3.31) per 100 patient-years. Presence of thrombophilia was independently associated with recurrences with the adjusted hazard ratio (aHR) of 3.52 (95% CI 1.32–9.42, p = 0.01). There were 144 patients who discontinued anticoagulants. During the median time of 55 months after stopping anticoagulants, the recurrent rate was 4.3 per 100 patient-years. Thrombophilia was associated with recurrences with aHR of 4.00 (95% CI 1.42–11.31, p = 0.01), while male sex, younger age, provoking conditions and hormone use showed no significant association.
Conclusion: VTE recurrent rate in Asians is comparable to Caucasians, but thrombophilia is the strongest risk factor.
Introduction
Venous thromboembolism (VTE) is a multifactorial disorder causing significant morbidity and mortality. The VTE incidence in Caucasians is 1 to 2 events per 1000 patient-years [Citation1,Citation2], which is 5–10 times higher than that of Asian population [Citation3–5].
Despite treatments, up to 25% of VTE patients will recur within 5 years after diagnosis [Citation6–8]. Studies in Western countries reveal the recurrent rate of approximately 8% in the first year followed by 4–5% per year afterwards [Citation6,Citation7,Citation9]. These recurrences may have serious consequences, including post-thrombotic syndrome, chronic pulmonary hypertension or fatal pulmonary embolism (PE). Extended therapy can prevent VTE recurrences, but relapses will appear once anticoagulants are stopped irrespective of prior drug durations [Citation10–12]. A predicting model for VTE recurrence is important for clinical decision to continue anticoagulants by weighing against bleeding risks in an individual patient [Citation13].
Active cancer is the strongest risk factors for VTE recurrences [Citation6,Citation7,Citation14], as well as for mortality. For non-cancer VTE, the risk factors for recurrences are the unprovoked event, the younger age of onset, male sex and VTE unrelated to female hormone [Citation6,Citation7,Citation15,Citation16]. The thrombophilia cannot strongly predict VTE recurrences in Western studies [Citation6,Citation7,Citation17–19]. However, the common hereditary thrombophilia types in Caucasians are factor V Leiden and prothrombin mutation [Citation17,Citation18], which are very rare in Asians [Citation20,Citation21]. On the other hand, inherited deficiencies of natural anticoagulants, protein C (PC), protein S (PS) or antithrombin (AT), which are the stronger risk factors for VTE, are more common in Asia [Citation21]. In one study, the anticoagulant protein deficiency is an independent risk factor for VTE recurrence in Caucasian patients [Citation22], but other studies in Caucasians usually excluded these patients [Citation23–25].
The recurrence rates of VTE have been reported to be low in Asian patients living in California [Citation26] and in a series of Korean patients [Citation27]. In addition, the risk factors are also different among races. In one study, the presence of transient provoking factors is not associated with the recurrent rate [Citation3]. In another study, antiphospholipid is associated with recurrences [Citation27]. Therefore, investigations specifically in Asian population are required as the significance of thrombophilia may be different among races.
The aim of the present study is to estimate the incidence of recurrent events after a first VTE in non-cancer patients and to identify the risk factors in Thai patients.
Patients and methods
Patients
The medical records of all venous thromboembolism (VTE) patients diagnosed at our hospital from 2004 to 2014 with the primary diagnosis of deep vein thrombosis (DVT) or pulmonary embolism were reviewed. Only patients who were older than 15 years and followed-up for at least 1 year were included. We excluded patients with active malignancy from analyses.
All cases were definitely diagnosed by Doppler ultrasonography, computed tomographic (CT) scan, magnetic resonance imaging (MRI), CT pulmonary angiography or ventilation/perfusion scan. The recurrences also had to be confirmed by imaging studies.
Risk factors
Patients were classified as having provoked VTE if the patients had a major surgery within 3 months, bedridden state for more than 1 week, or current use of estrogen. Major surgery was defined as a requirement of general anesthesia and/or duration of at least 1 hour. All the other events were regarded as unprovoked VTE.
The investigations for thrombophilia, including antithrombin, protein C or S deficiency, and antiphospholipid syndrome, were left to the judgment of the treating physicians and were performed either before implementing anticoagulation or at least 3 weeks after completing oral anticoagulant therapy. Every abnormal test during the acute VTE period had to be repeated to confirm the presence of thrombophilia. The diagnosis of antiphospholipid syndrome was according to the Sapporo criteria that required repeated the abnormal tests at least 12 weeks apart in all cases [Citation28]. The tests included lupus anticoagulants, anti-cardiolipin IgG/IgM and anti-β2 glycoprotein I IgG/IgM.
Statistical analysis
Demographic variables including age, gender, underlying diseases, alcohol, smoking, immobilization, operation, hormonal use, family history, thrombophilia, type of event (PE, DVT, or both) and duration of anticoagulant were tested as potential predictors of recurrent VTE.
Statistical analysis was performed with Statistical Packages for Social Sciences version 21.0 (SPSS, IBM Corp.). Kaplan-Meier estimates and their 95% confidence intervals (CI) were calculated to assess the time-dependent risk of recurrent VTE. The evaluated time interval spanned from the date of the incident VTE event to the last day of follow-up or the day of recurrence. A subgroup that stopped anticoagulants was evaluated from the last day of anticoagulant to the last day of follow-up or the day of recurrence.
Variables that were significantly associated with the recurrent VTE in univariate analysis were entered in a multivariate Cox proportional hazard model to identify features independently associated with recurrences. The strengths of associations were expressed as hazard ratios (HR) and 95% confidence intervals (CI).
Results
Baseline characteristics
There were the total of 468 patients with first thrombotic events at our hospital between 1 January 2004, and 31 December 2014. A total of 290 patients were excluded because of the followings: active malignancies (124), lost to follow-up or deaths before 1 year (98), no definite diagnosis (42) or ages younger than 15 years old (6). Therefore, 198 patients were included in the study.
For the included patients, their mean (± SD) age at the onset was 58.2 ± 17.6 years, and 135 patients (68.2%) were female. Among them, 111 patients (56%) had DVT, 63 (32%) had PE and 63 (32%) had both DVT and PE. There were 43 (21.7%) VTE occurred within 3 months after major surgery. Of the postoperative VTE, 21 (48.8%) were after orthopedic surgery, 20 (46.5%) after general surgery, and 2 events (4.7%) after neurosurgery. Pharmacological prophylaxis was not routinely used in Thailand. Immobilization was identified in 44 (22.2%) cases. There was a history of hormonal use in 19 (14.1%) female patients. Provoking factors were present in 30.3% of patients. One hundred and fifty-five patients were tested for thrombophilia and found in 11.6%, which were antiphospholipid syndrome (5.6%), protein C deficiency (3%) and protein S deficiency (3%). shows the clinical characteristics of the patients.
Table 1. Clinical characteristics of venous thromboembolism (VTE) patients.
The majority of patients were initially treated by subcutaneous low molecular weight heparin (LMWH, 67.2%) or intravenous unfractionated heparin (20.2%). Thrombolytic therapy, surgical thrombectomy and inferior vena cava filter were used in 9 (4.5%), 3 (1.5%) and 1 (0.5%) patients, respectively. For long-term therapy, warfarin was used in 97.5%, followed by direct oral anticoagulants (1.5%) and LMWH (1%). The median duration of anticoagulants was 12 months (interquartile range [IQR]: 6.0, 35.3).
Cumulative incidence and risk factors of first VTE recurrence
During the median follow-up duration of 52 months (IQR: 30, 85), there were a total of 22 recurrences. The cumulative incidence of first definite recurrence was 11.1%. The estimated incidence rate was 2.2 (95% confidence interval [CI] 1.46–3.31) per 100 patient-years. There was no recurrence while on anticoagulant.
Potential risk factors for recurrent VTE were studied. Only thrombophilia was significantly associated with VTE recurrences with the hazard ratio (HR) of 4.59 (95% CI 1.95–10.81, p < 0.001). There was no significant difference in recurrent rates relating to age, sex, diabetes mellitus, hypertension, immobilization, perioperative VTE, hormonal use or presence of provoking condition.
In a multivariate analysis, the presence of thrombophilia was independently associated with recurrent events with the adjusted hazard ratio (adjusted HR) of 3.52 (95% CI 1.32–9.42, p = 0.01).
The recurrent rate and risk factors after stopping anticoagulants
Since all recurrences occurred after stop using anticoagulant, we performed an analysis to explore the risk factor and recurrent rate after anticoagulant had been stopped. The index dates were reset at the time anticoagulant had been stopped. There were 144 patients left in this cohort.
shows clinical characteristics of VTE patients who had stopped anticoagulant. Their mean (± SD) age at the onset was 57.97 ± 17.56 years, and 96 patients (66.7%) were female. Among these, 85 (59%) had DVT, 48 (33.3%) had PE and 11 patients (7.7%) had both DVT and PE. There were 34 (23.6%) patients with postoperative VTE after orthopedic (13.9%), general (11.1%) and neurological (0.7%) surgeries. Immobilization was present in 27 (18.8%) cases. For a female, there was a history of hormonal use in 15 (15.8%) cases. Provoking factors were identified in 30.6%. Thrombophilia tests were performed in 115 patients. Thrombophilia was found in 11.1%, which were antiphospholipid syndrome (3.5%), protein C deficiency (4.2%) or protein S deficiency (4.2%).
Table 2. Clinical characteristics of venous thromboembolism (VTE) patients after stopping anticoagulants.
The majority of patients were initially treated with intravenous unfractionated heparin (18.8%) or LMWH (78.6%). Thrombolytic therapy, surgical thrombectomy and IVC filter were applied in 4.86%, 1.4% and 0.7%, respectively. Long-term anticoagulant was warfarin in 98.6%. The median duration of anticoagulant treatment was 8 months (interquartile range [IQR]; 6.0, 18.75).
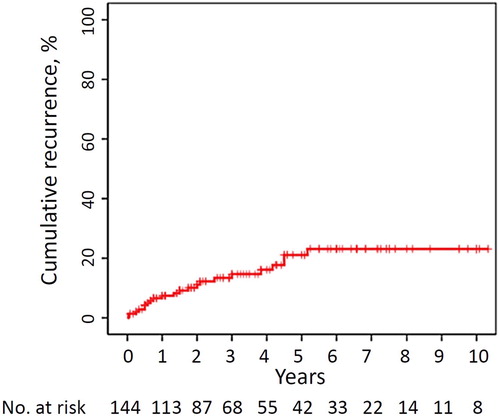
During the median follow-up time of 55 months (IQR 33–88), the cumulative incidence of a first definite recurrence was 15.3% (). The estimated incidence rate was 4.3 per 100 patient-years. Two patients with recurrences had a persistent risk factor of immobilization without thrombophilia. The anticoagulant was stopped because the treating physicians decided that the risk of bleeding outweighed the risk of recurrences.
Figure 1. Kaplan-Meier estimates of cumulative incidence of venous thromboembolism (VTE) recurrence after stopping anticoagulant. The X axis represents years of follow-up after the day of stopping anticoagulant. The Y axis shows the percentage of recurrences. The numbers of patients at risk are shown below the graph.
shows the univariate and multivariate HR and 95% CIs for recurrent events. The presence of thrombophilia was independently associated with recurrent events in a multivariate analysis with the adjusted HR of 4.00 (95% CI 1.42–11.31, p = 0.01) as shown in .
Figure 2. Cumulative incidences of recurrent thrombotic events in patients with thrombophilia and without thrombophilia after stopping anticoagulants. The X axis represents years of follow-up after the day of stopping anticoagulant. The Y axis shows the percentage of recurrences. The numbers of patients at risk are shown below the graph.
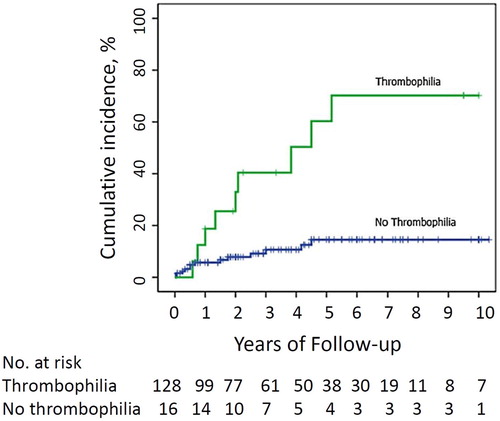
Table 3. Univariate and multivariate cox proportional hazards analyses of potential predictors of first venous thromboembolism recurrence after stopping anticoagulant.
Discussion
In this retrospective cohort of Thai VTE patients who were followed up for a long period of time after a first venous thrombotic event, we found the VTE recurrent rate of 11.1% in 52 months. The estimated incidence rate was 2.2 per 100 patient-years. The rate of recurrent VTE was relatively low but the confidence interval covered the range of the previously reported incidence in Caucasians [Citation6–8]. An important difference of these studies was the exclusion of cancer patients, who were likely to have high recurrent rates. After stopping anticoagulants, the recurrent rate of VTE in this cohort was 4.3 per 100 patient-year or over 20% in five years comparable to those reports in Western countries [Citation9,Citation29].
It is still controversial whether thrombophilia is a risk factor for recurrent thrombosis [Citation17–19]. VTE is multi-factorial in etiology. Although thrombophilia is one of the strongest risk factors for the first VTE event, multiple factors usually coexist when VTE occurs. A combination of all the other factors may contribute more to VTE recurrences than thrombophilia. In our study, thrombophilia was found to be an independent risk factor for recurrent VTE in both the whole cohort and in the cohort that had stopped anticoagulants with the adjusted HR of 4.0 and 3.5, respectively. This may be explained by the different genetic background for VTE between Caucasian and East Asian populations [Citation21,Citation30]. Protein S deficiency and protein C deficiency are more common in the Thais [Citation31,Citation32], but the weaker thrombophilia mutations are common in Caucasians [Citation17,Citation18].
Our study suggests that thrombophilia workups are potentially helpful for the recurrent risk stratification in Thai VTE patients without cancer. Patients with positive tests after confirmation are candidate for long-term anticoagulants after considering bleeding risks and patient preference. However, testing for such thrombophilia in every patient with VTE may not be cost-effective due to the low positive rate. In an attempt to find subgroups of patients who would benefit from testing for thrombophilia, we compared patients with and without thrombophilia. Patients with thrombophilia tend to be younger (mean age 43.1 vs. 60.2 years old), and have no provoked condition (95.7% vs. 66.3%). Further prospective studies should be performed.
Regarding other risk factors, we found a trend towards lower risk of recurrences in VTE with a transient provoking condition, which is the most important risk factor in Western studies. This association became weaker in a multivariate analysis () probably because thrombophilia was less common in this group. In addition, we did not find the different recurrences between sexes. These results are similar to those in Taiwan population [Citation3]. Whether this is common in all Asians remain to be determined. Furthermore, the significant association with age was not found. Although younger age appeared to have more recurrences in a univariate analysis, the trend disappeared in a multivariate analysis. This may be explained by the more common thrombophilia in younger patients.
This study does have limitations due to its retrospective nature. Some data may not be complete and thrombophilia testing was not performed in all patients. Small sample size may make our study underpowered to detect all risk factors from previous studies.
Our data demonstrated that VTE recurrent risks in Asians may be different from those of Western patients. In this study, patients without thrombophilia still had high risks for recurrence (over 15% in 5 years [Citation33], ). More research is needed to select patients that do not require long-term anticoagulation.
In conclusion, the VTE recurrent rate in Thai patients is comparable to those of Western countries. Patients with inherited deficiency of protein C or protein S or presence of antiphospholipid antibody have an increased risk of recurrent VTE.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Ponlapat Rojnuckarin http://orcid.org/0000-0001-7912-1996
Additional information
Funding
References
- Oger E, EPI-GETBP Study Group. Incidence of venous thromboembolism: a community-based study in Western France. Thromb Haemost. 2000;83:657–660. doi: 10.1055/s-0037-1613887
- Anderson FA Jr, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. Arch Intern Med. 1991;151:933–938. doi: 10.1001/archinte.1991.00400050081016
- Lee CH, Lin LJ, Cheng CL, et al. Incidence and cumulative recurrence rates of venous thromboembolism in the Taiwanese population. J Thromb Haemost. 2010;8:1515–1523. doi: 10.1111/j.1538-7836.2010.03873.x
- Cheuk BLY, Cheung GCY, Cheng SWK. Epidemiology of venous thromboembolism in a Chinese population. Br J Surg. 2004;91:424–428. doi: 10.1002/bjs.4454
- Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the health insurance review and assessment service database. J Thromb Haemost. 2011;9:85–91. doi: 10.1111/j.1538-7836.2010.04108.x
- Heit JA, Mohr DN, Silverstein MD, et al. Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study. Arch Intern Med. 2000;160:761–768. doi: 10.1001/archinte.160.6.761
- Hansson P-O, Sorbo J, Eriksson H. Recurrent venous thromboembolism after deep vein thrombosis. Arch Intern Med. 2000;160:769–774. doi: 10.1001/archinte.160.6.769
- Prandoni P, Lensing AW, Cogo A, et al. The long term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1–7. doi: 10.7326/0003-4819-125-1-199607010-00001
- Baglin T, Douketis J, Tosetto A, et al. Does the clinical presentation and extent of venous thrombosis predict likelihood and type of recurrence? A patient-level meta-analysis. J Thromb Haemost. 2010;8:2436–2442. doi: 10.1111/j.1538-7836.2010.04022.x
- Agnelli G, Prandoni P, Santamaria MG, et al. Three months versus one year of oral anticoagulant therapy for idiopathic deep venous thrombosis. N Engl J Med. 2001;345:165–169. doi: 10.1056/NEJM200107193450302
- Schulman S, Lindmarker P, Holmström M, et al. Post-thrombotic syndrome, recurrence, and death 10 years after the first episode of venous thromboembolism treated with warfarin for 6 weeks or 6 months. J Thromb Haemost. 2006;4:734–742. doi: 10.1111/j.1538-7836.2006.01795.x
- Campbell IA, Bentley DP, Prescott RJ, et al. Anticoagulation for three versus six months in patients with deep vein thrombosis or pulmonary embolism, or both: randomised trial. Br Med J. 2007;334:674. doi: 10.1136/bmj.39098.583356.55
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149:315–352. doi: 10.1016/j.chest.2015.11.026
- Prandoni P. Cancer and venous thromboembolism. Clinical implications of strong association. Pathophysiol Haemost Thromb. 2006;35:111–115. doi: 10.1159/000093552
- Kyrle PA, Minar E, Bialonczyk C, et al. The risk of recurrent venous thromboembolism in men and women. N Engl J Med. 2004;350:2558–2563. doi: 10.1056/NEJMoa032959
- Tosetto A, Iorio A, Marcucci M, et al. Predicting disease recurrence in patients with previous unprovoked venous thromboembolism: a proposed prediction score (DASH). J Thromb Haemost. 2012;10:1019–1025. doi: 10.1111/j.1538-7836.2012.04735.x
- Baglin T, Luddington R, Brown K, et al. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523–526. doi: 10.1016/S0140-6736(03)14111-6
- Kyrle PA, Rosendaal FR, Eichinger S. Risk assessment for recurrent venous thrombosis. Lancet. 2010;376:2032–2039. doi: 10.1016/S0140-6736(10)60962-2
- Christiansen SC, Cannegieter SC, Koster T, et al. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352–2361. doi: 10.1001/jama.293.19.2352
- Angchaisuksiri P, Atichartakarn V, Aryurachai K, et al. Risk factors of venous thromboembolism in Thai patients. Int J Hematol. 2007;86:397–402. doi: 10.1007/BF02983995
- Angchaisuksiri P. Venous thromboembolism in Asia--an unrecognised and under-treated problem? Thromb Haemost. 2011;106:585–590. doi: 10.1160/TH11-03-0184
- De Stefano V, Simioni P, Rossi E, et al. The risk of recurrent venous thromboembolism in patients with inherited deficiency of natural anticoagulants antithrombin, protein C and protein S. Haematologica. 2006;91:695–698.
- Rodger MA, Kahn SR, Wells PS, et al. Identifying unprovoked thromboembolism patients at low risk for recurrence who can discontinue anticoagulant therapy. Can Med Assoc J. 2008;179:417–426. doi: 10.1503/cmaj.080493
- Eichinger S, Heinze G, Jandeck LM, et al. Risk assessment of recurrence in patients with unprovoked deep vein thrombosis or pulmonary embolism: the Vienna prediction model. Circulation. 2010;121:1630–1636. doi: 10.1161/CIRCULATIONAHA.109.925214
- Ensor J, Riley RD, Moore D, et al. Systematic review of prognostic models for recurrent venous thromboembolism (VTE) post-treatment of first unprovoked VTE. BMJ Open. 2016;6:e011190. doi: 10.1136/bmjopen-2016-011190
- White RH, Zhou H, Romano PS. Incidence of idiopathic deep venous thrombosis and secondary thromboembolism among ethnic groups in California. Ann Intern Med. 1998;128:737–740. doi: 10.7326/0003-4819-128-9-199805010-00006
- Kim TM, Kim JS, Han SW, et al. Clinical predictors of recurrent venous thromboembolism: a single institute experience in Korea. Thromb Res. 2009;123:436–443. doi: 10.1016/j.thromres.2008.05.009
- Miyakis S, Lockshin MD, Atsumi T, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006;4:295–306. doi: 10.1111/j.1538-7836.2006.01753.x
- Prandoni P, Noventa F, Ghirarduzzi A, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199–205. doi: 10.3324/haematol.10516
- Miyata T, Maruyama K, Banno F, et al. Thrombophilia in East Asian countries: are there any genetic differences in these countries? Thromb J. 2016;14(Suppl 1):25. doi: 10.1186/s12959-016-0109-x
- Akkawat B, Rojnuckarin P. Protein S deficiency is common in a healthy Thai population. J Med Assoc Thai. 2005;88(Suppl 4):S249–S254.
- Sirachainan N, Chuansumrit A, Sasanakul W, et al. R147w in PROC gene is a risk factor of thromboembolism in Thai children. Clin Appl Thromb Hemost. 2018;24:263–267. doi: 10.1177/1076029617709085
- Kearon C, Iorio A, Palareti G. Risk of recurrent venous thromboembolism after stopping treatment in cohort studies: recommendation for acceptable rates and standardized reporting. J Thromb Haemost. 2010;8:2313–2315. doi: 10.1111/j.1538-7836.2010.03991.x
