1. Introduction
Thoracic endovascular aortic repair (TEVAR) has expanded with thoracic aortic pathology. Successful TEVAR depends notably on proximal and distal stent-graft fixation zones (Nasr et al. Citation2019). However, the long-term consequences of the device implantation on the native aortic anatomy are not fully mastered (Roos et al. Citation2016). The follow-up with computed tomography angiography (CTA) coupled to the post processing techniques plays therefore a crucial role to analyze the vascular geometry before and after TEVAR considering long term evolution.
Based on the state of the native vascular structures the main concern of this work was therefore to analyze the remodeling of the thoracic aorta after TEVAR and assess its impact in a long time. For this purpose, a detailed analysis of the changes in aortic geometry over a period of time was conducted on the basis of CTA images and morphological index quantifications. The modifications that occurred in the geometry after stent-graft placement were actually characterized measuring the changes in the angles and diameters, the lengthening of the aorta and the neck of the aneurysm as well as the curvature of the aorta. It is important to note that, to our knowledge, this study proposes for the first time in the literature a long term (36 months) and regular (each year) patient follow-up and that patient population was focused on thoracic aorta aneurysm.
2. Methods
2.1. Population
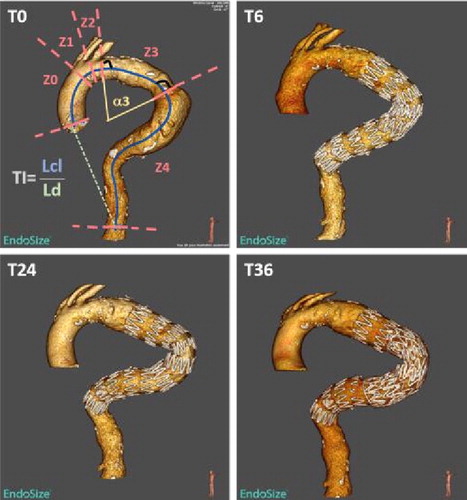
This retrospective study from 2009 to 2016, has been carried out on 185 patients receiving thoracic aneurysm repair in our institution. The indication to operate was retained for (i) a diameter above 60 mm, (ii) a diameter increase by more than 10 mm in 1 year, (iii) a compression of the neighboring organs (dysphagia, dysphonia) and (iv) a rupture (Mokashi and Svensson 2019). The main inclusion criterion was a preoperative CT-scan (T0) and 3 postoperative scans at 6 or 12 months (T6), 24 months (T24), 36 months (T36) after surgery, for each patient (). Twenty-five patients (average age 72, range 54–81; 20 males and 5 females) were retained with a long follow-up, and underwent hybrid endovascular repair (with debranching of one or more arch vessels) or endovascular procedure alone for aneurysm disease of the thoracic aorta.
Figure 1. Illustrative aorta at 4 times of follow-up. For T0, centerline (blue) is drawn, zones and some geometric parameters are shown.
All the TEVAR procedures were performed using the following stents: GORE Conformable TAG (W. L. Gore & Associates, Flagstaff, Arizona), Cook (Cook Medical, Bloomington, IN, USA) and Medtronic (Valiant TM or the Valiant CAPTIVIA generation). The diameter of the stent was oversized by 20%. The proximal anchoring zone was recorded according to Ishimaru’s classification (Ishimaru Citation2004).
2.2. Image acquisition and geometric analysis of the aorta
For each of the 25 patients and for each scan (that means about 100 scans), centerline path of the thoracic aorta (CL) was generated semiautomatically () using Endosize software (Therenva, Rennes, France). The CL was segmented into five anatomical zones (Z0 to Z4), according to Ishimaru classification. Diameter and stented lumen volume were measured directly with Endosize. Custom developed routines on Matlab were used to extract different geometric parameters from CL: curve lengths (L0 to L4), angles (α0 to α4) and tortuosity indexes (TI0 to TI4) for each zone.
2.3. Statistical analyses
Statistical analyses were performed with the non parametric Wilcoxon signed-rank test for matched samples. Statistical significance was defined as a two-tailed P value of less than 0.05.
3. Results and discussion
Morphological data analysis according to the different arch zones enabled parameter quantification and detection of variations within zones. Among all the obtained results, those showing statistically representative differences are summarized in .
Table 1. P values of proximal neck diameter (PND), distal neck diameter (DND), Z3 and Z4 lengths (LZ3 and LZ4 respectively), Z3 length plus, Z4 length (LZ3-LZ4), and total length (Ltot). Ti/Tj means Ti versus Tj. P < 0.05 are in red.
This analysis showed that the diameters of proximal and distal aortic neck diameter increase consistently over time following after TEVAR. For the other morphologic parameters and anatomical zones, was found a statistically significant increase in overall aortic length (Ltot) after TEVAR, along the followup between T0 and T36 (P = 0.0494). During the follow-up, an increase in descending thoracic aorta (LZ3-LZ4) length was observed between T6 and T24 (P = 0.0371). Zone 3 tends to lengthen from the first check: T0/T6, T0/T24 and T0/36 (P = 0.0249, P = 0.0029 and P = 0.0391). An increase length of zone 4 for T6/T24 (P = 0.0353) and T24/T36 (P = 0.0353) was put into light. The angle of the descending thoracic aorta and aortic arch decreased for T0/T24 (P = 0.0096, P = 0.0068 data not shown). Geometric analysis of the tortuosity index showed changes in descending thoracic aorta. The aortic arch (Z0Z1Z2) showed a reduction in TI between T6 and T24 (P = 0.0371) and T24 and T36 (P = 0.0391). The population showed an increase of tortuosity of the descending thoracic aorta (Z3 and Z4) for T0/T24 and for T0/T36 (P = 0.0322, P = 0.0078), as well as T6 against T24 and T36 (P = 0.0039, P = 0.0078). We found a statistically significant increase of the descending thoracic aorta (LZ3-LZ4) length, which could explain late type III endoleaks. Naguib et al. (Citation2016) also described a significant change in the overall length of the aorta at 12 months after the first intervention, with an increase up to 9.3% in patients treated for aortic aneurysm. Mestres et al. (Citation2017) analyzed the changes in the aortic arch after TEVAR, measuring, in particular, the tortuosity, and they demonstrated that after TEVAR the normal curvature of the proximal descending aorta decreases because of the longitudinal stiffness of the stent-graft. This study shows that the influence of aortic anatomy on favorable clinical outcomes after TEVAR, with regard to the underlying pathology treated and the location of the sealing area is fundamental. The present work brings additional lighting. Our results indeed suggest that quantifications of thoracic aortic tortuosity, neck lengths and angulations may allow stratification of the risk of late endoleaks after endovascular treatment and help the clinician in choosing aortic cover, as well as achieving a greater overlap between two endoprostheses.
4. Conclusion
Our study shows that less than 1 year after TEVAR procedure, geometrical modifications are already highlighted and continue for the next two years. Our results suggest that stent-graft monitoring, with a long and regular follow-up, must be an integral part of the treatment of thoracic aortic aneurysms to anticipate potential unfavorable evolution. In order to improve our suggestions, work is currently in progress to correlate favorable and unfavorable TEVAR evolution with morphological parameters.
References
- Ishimaru S. 2004. Endografting of the aortic arch. J Endovasc Ther. 11(6_suppl):II-62–II-71.
- Mestres G, Garcia M E, Yugueros X, Urrea R, Tripodi P, Gomez F, Maeso J, Riambau V. 2017. Aortic arch and thoracic aorta curvature remodeling after thoracic endovascular aortic repair. Ann Vasc Surg. 38:233–241.
- Mokashi SA, Svensson LG. 2019. Guidelines for the management of thoracic aortic disease in 2017. Gen Thorac Cardiovasc Surg. 67(1):59–65.
- Naguib NNN, Zima B, Nour-Eldin N-EA, Gruber-Rouh T, Fischer S, Schulz B, Eichler K, Schmitz-Rixen T, Moritz A, Balzer J O, et al. 2016. Long-term changes in aortic length after thoracic endovascular aortic repair. J Vasc Interv Radiol. 27(2):181–187.
- Nasr B, Savean J, Albert B, Badra A, Braesco J, Nonent M, Gouny P, Visvikis D, Fayad H. 2019. Thoracic stent-graft migration: the role of the geometric modifications of the stent-graft at 3 years. Ann Vasc Surg. 58:16–23.
- Roos H, Tokarev M, Chernoray V, Ghaffari M, Falkenberg M, Jeppsson A, Nilsson H. 2016. Displacement forces in stent grafts: influence of diameter variation and curvature asymmetry. Eur J Vasc Endovasc Surg. 52(2):150–156.
