1. Introduction
Transverse disorders of the lower extremities are frequently targeted by the surgical procedures offered to children and adolescents with cerebral palsy during multilevel surgery. Of these, femoral derotation is commonly performed.
When the kinematic deviations are asymmetrical, its indication may be one-sided and is reported as more effective on the pelvic rotation (Niklasch et al. Citation2015). Literature highlights two treatment strategies. The first is related to the type of neurological involvement, hemiplegia or diplegia. The second focuses on the nature of asymmetrical or symmetrical transverse kinematic disorders (Carty et al. Citation2014).
Is this second strategy effective? Are corrections of internal hip rotation, foot progression, or pelvic rotation proportional to the femoral derotation angle? What are the effects of this procedure on the transverse kinematics of the pelvis and on the contralateral hip rotation and foot progression angles?
2. Methods
2.1. Population
Among a database of 170 children with cerebral palsy, operated, with at least a clinical gait analysis before and after surgery, those having had a unilateral femoral derotation are included. Patients with tibial derotation are excluded.
2.2. Surgical indication
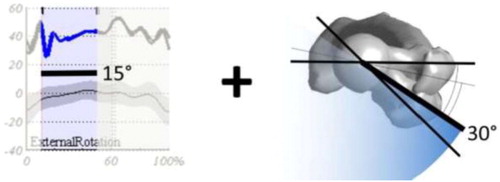
Femoral derotation was indicated when kinematic internal hip rotation was over 15° during single stance phase and femoral anteversion was more than 30° ()
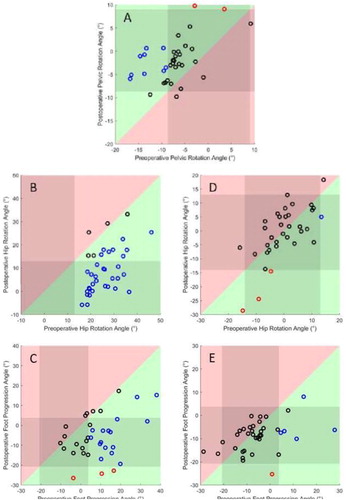
Figure 2. Kinematic effects on pelvic rotation (A), Ipsilateral and contralateral internal hip rotation (B, D), Ipsilateral and contralateral internal foot progression angle (C, E). The colour of each circle illustrate the outcome of each patient, black for unchanged, blue for improved and red for worsened.
2.3. Data collection
Clinical maximum hip rotations and femoral anteversion were measured in prone position. Gait analysis were performed with Vicon system. Lower limb marker placements were identical and kinematic data were computed with the same software based on a modified Helen Hayes (Kadaba et al. Citation1990; Davis et al. Citation1991) model with anatomical markers on the femoral condyles and the medial-malleolus.
2.4. Data analysis
The kinematic variations are compared by paired ttests and correlations by spearman test (p < 0.05). ‘Abnormal’ kinematics are defined as different from more than two standard deviations of the normal distribution (pelvis: µ=0.2 σ = 4.4°, hip: µ=0.5 σ = 6.8°, foot progression: µ=0.2 σ = 6.1°). Improvements of more than 1 σ are classified as ‘improved’.
3. Results and discussion
37 patients (12.7 ± 2.9 years - GMFCS I: 14, II: 22, III: 1) are included. They had preoperative femoral anteversion of 46 ± 9°. The surgical correction was 28 ± 5°. All the kinematics parameters have been significantly improved except contralateral hip rotations ( and ).
Table 1. Effects of unilateral derotations in degrees.
Preoperative sub-group analysis shows 15 pelvis in asymmetric rotation (13 ± 4°) and 24 ‘normal’ (5 ± 4°). Postoperatively the asymmetric group (5 ± 4°) and the ‘normal’ group (1 ± 5°) improved significantly. In the asymmetric group 73% (11/15) of the pelvis are classified improved,.
87% (35/40) of the operated hip had their internal rotation improved (7 ± 8°). 83% of the 24 ipsilateral feet with abnormal foot progression angle were improved from (15 ± 8°) to (−4 ± 10°). The 8 controlateral feet with abnormal foot progression angle were improved from (12 ± 7) to (1 ± 7).
No correlation is found between the amount of derotation and the kinematic correction of the hip and pelvis rotation or the step progression angle.
The unilateral derotation modifies the transverse kinematic parameters of the operated side. According to some results of the literature (Carty et al. Citation2014; Niklasch et al. Citation2015; Kim et al. Citation2017) this local correction has not only a joint effect on the hip but also an effect on the spatial positioning of the pelvis and the foot.
Concerning the effect on the contralateral side, this surgical procedure is effective in reducing pelvic asymmetry without altering contralateral hip kinematics, thus affecting the angle of progression of the contralateral foot.
4. Conclusions
Unilateral derotation modifies the transverse kinematic parameters of the operated side. This local correction has not only an effect on the operated hip kinematic but also on the spatial positioning of the pelvis and the feet including the contralateral side. However, none of the improvements are proportional to the surgical correction indicating that the surgical planning is not straightforward.
Acknowledgements
The authors are grateful to the medical and technical staff of Fondation Ellen Poidatz for useful discussions and for recording the data used for this work.
Additional information
Funding
References
- Carty CP, Walsh HPJ, Gillett JG, Phillips T, Edwards JM, deLacy M, Boyd RN. 2014. The effect of femoral derotation osteotomy on transverse plane hip and pelvic kinematics in children with cerebral palsy: a systematic review and meta-analysis. Gait Posture. 40(3):333–340.
- Davis RB, III, Ounpuu S, Tyburski D, Gage JR. 1991. A gait analysis data collection and reduction technique. Hum Mov Sci. 10(5):575–587.
- Kadaba MP, Ramakrishnan HK, Wootten ME. 1990. Measurement of lower extremity kinematics during level walking. J Orthop Res. 8(3):383–392.
- Kim HY, Cha YH, Byun JY, Chun YS, Choy WS. 2017. Changes in gait parameters after femoral derotational osteotomy in cerebral palsy patients with medial femoral torsion. J Pediatr Orthop B. 27(3):194–199.
- Niklasch M, Döderlein L, Klotz M. C, Braatz F, Wolf S. I, Dreher T. 2015. Asymmetric pelvic and hip rotation in children with bilateral cerebral palsy: Uni- or bilateral femoral derotation osteotomy? Gait Posture. 41(2):670–675.