?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
For several years, in traumatic surgery, surgical techniques have evolved towards minimally invasive methods. Recently Vendeuvre et al. (Citation2013) developed a novel method for tibial plateau fracture treatment using minimally invasive techniques named Tuberoplasty (). This allowed the surgeons to reduce the fracture with the inflation of a surgical balloon usually used in Kyphoplasty —vertebrae compression fracture reduction—. After balloon deflation and removing, the resulting cavity is filled with surgical PMMA cement. This method uses an anterior entry point. With the entry point close to the compression, surgeons never use Kirschner wires to support the balloon, contrary to a similar method which uses lateral entry point (Pizanis et al. Citation2012).
The evaluation of the biomechanical behavior for both methods is needed to determine which of the two methods is the best according to the clinical case.
Computer-assisted surgery has the potential to facilitate this task by the simulation of a per-operative —during the surgery— models. A considerable amount of study exists on the biomechanical behavior after balloon kyphoplasty —with cement injection—, however per-operative simulation to evaluate the kinematics of the fragments remains unknown.
This work aims to develop a patient-specific Finite Element (FE) simulation of hyperelastic balloon inflation in a model of tibial plateau fracture. The resulting model aims (1) to define which surgical method is preferable; (2) to develop new numerical tools for the preoperative planning task.
2. Methods
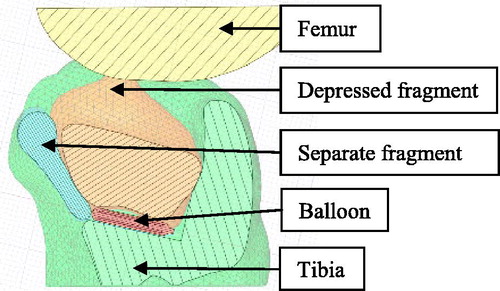
2.1. Geometries
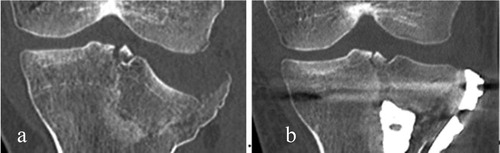
The patient was a 22-year-old woman with a tibial plateau fracture composed of two main fragments: a depressed and a separated fragment —type named Schatzker II—(Kfuri and Schatzker Citation2018) (). The geometries were obtained from the segmentation of a preoperative CT-scan image. We used a semi-automatic method based on region growing algorithm with 3 D Slicer Software (v4.6.2). With the SpaceClaim software tools (ANSYS, Canonsburg, USA)), we suppressed the geometry interferences dues to the geometries smoothing during segmentation. The geometry of the tibia was then modified to include the balloon in the model —along the anterior way—, in which resulting cavity filled by PMMA cement is visible on the postoperative 3D image.
The balloon geometry was designed from measurements of the balloon before inflation and during balloon inflation in the air.
2.2. FE model
To model the mechanical behavior, the bone material had a bilinear elastoplastic behavior:
(Carter and Hayes Citation1977)
The balloon had quasi-incompressible hyperplastic behavior (Eshghi et al. Citation2011).
The contacts were frictional with modification of the Coulomb law to soften the frictional forces above 60% of bone material yield strength, for the bone to bone contacts. The balloon inflation is controlled by its volume. The ‘Hydrostatic fluid’ software extension created elements into the balloon that simulate water injection was controlled with a mass flow parameter. Three springs between the tibia and the separate fragment modeled the soft tissues interactions. Their stiffness was
A
force on the separate fragment was modeling the clamp used during the surgery by the surgeon. The mesh of the bone geometries had 20782 triangular shell elements. The mesh of the balloon geometry had 20634 tetrahedral elements.
2.6. Reduction evaluation
We used Scilab software to evaluate position error regarding three inspection points (). The inspection points were localized on the depressed fragment; their final position was compared to the same inspection points localized in the real postoperative image. These latter were the reference for the position error.
Figure 3. Simulation results on the external tibial plateau geometries: displacement field at 1.93 injection. (The separate fragment is masked).
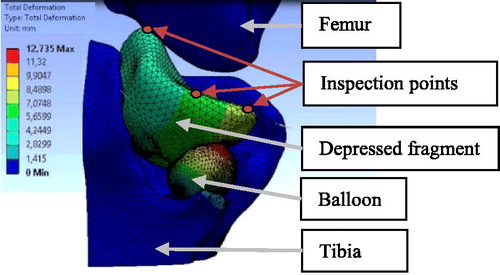
To measure the variation of the position of the fragment, we used anatomical points to define the transformation matrix between the preoperative coordinate system and the postoperative local coordinate system.
3. Results and discussion
shows the displacement field at the end of the simulation. The simulation shows the kinematics of the fragments in relation to the volume and the position of the balloon.
This approach makes it possible to analyze the contribution of the balloon position to improve fracture reduction.
Regarding the real postoperative image, we found that the position error of the simulated reduction is 5.49 ± 2.78 mm, after a inflation. This corresponds to the maximum inflation before non-convergency of the simulation. For this clinical case, the surgeon injected approximately
in the balloon.
The main non-convergency factors may be the integration of the balloon in the segmented geometries and the behavior of the contact. To handle reasonable simulation time, shell element meshed the bone geometries. In future work, we aim to consider tetrahedral mesh with flexible bone material behavior depending on the local Hounsfield unit.
The balloon material behavior was based on literature; it should be identified with experimental tests.
4. Conclusions
Although the current results do not allow us to determine the best technique for minimally invasive surgery, the results are encouraging to model a patient-specific case for the simulation of the reduction of tibial plateau fractures by surgical balloon inflation.
This approach could play a relevant contribution to minimally invasive surgery practices where open visualization of fractures is reduced, to better understand mechanisms of fracture reduction.
Acknowledgments
The authors would like to thank ANSYS SAS France.
References
- Carter DR, Hayes WC. 1977. The compressive behavior of bone as a two-phase porous structure. J Bone Joint Surg. 59(7):954–962.
- Eshghi N, Hojjati MH, Imani M, Goudarzi AM. 2011. Finite element analysis of mechanical behaviors of coronary stent. Proc Eng. 10:3056–3061.
- Kfuri M, Schatzker J. 2018. Revisiting the Schatzker classification of tibial plateau fractures. Injury. 49(12):2252–2263.
- Linde F, Hvid I. 1989. The effect of constraint on the mechanical behaviour of trabecular bone specimens. J Biomech. 22(5):485–490.
- Pizanis A, Garcia P, Pohlemann T, Burkhardt M. 2012. Balloon tibioplasty: a useful tool for reduction of tibial plateau depression fractures. J Orthop Trauma. 26(6):e88–e93.
- Vendeuvre T, Babusiaux D, Brèque C, Khiami F, Steiger V, Merienne J-F, Scepi M, Gayet LE. 2013. Tuberoplasty: minimally invasive osteosynthesis technique for tibial plateau fractures. Orthop Traumatol Surg Res. 99(4):S267–S272.