1. Introduction
Radiotherapy applied to head and neck cancers causes fibrosis that is a very frequent side effect of this treatment. Fibrosis provides an increase of muscle stiffness, responsible for an impairment in the quality of life of patients (Langendijk et al. Citation2008), and can obstruct a possible catch-up surgery or a possible re-irradiation (Moloney et al. Citation2015). The appreciation of radiation-induced cervical fibrosis within the sterno-cleido-mastoid (SCM) muscle is subjective and radiotherapists have attempted to define standardized clinical measurement scales, which bring several objective criteria such as the level of indurations of cutaneous tissues and the quality of life. The correlation between these different classifications is often poor (Davis et al. Citation2003). Thus, the purpose of this study is to develop MR Elastography (MRE) protocol for healthy neck muscle to latterly used for patient having neck muscle fibrosis.
2. Methods
2.1. Participants
Five volunteers, without muscle abnormality and no history of muscle disease underwent a MRI neck acquisition. This study was approved by the Institutional Review Board (CPP IDF6).
2.2. Localization of the sterno-cleido-mastoid muscle
The subject lays supine inside the 3 T MRI Philips machine (GIE Faire-Faces) and a head coil was used inducing a stable position of the neck without tension. The sterno-cleido-mastoid (SCM) muscle is a neck muscle with two points of insertion in the upper (bony point behind the ear, occipital bone at the posterior and lower part of the skull) and lower (sternum, collarbone) sides of the neck.
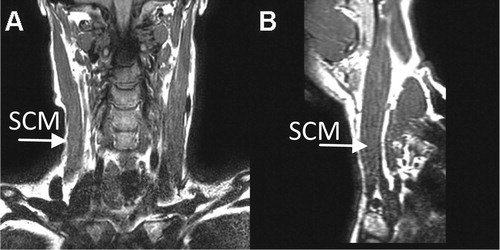
Accurate anatomical localization of the SCM has been performed with a coronal 3 D T1 sequence (coronal plane, ; sagittal plane ). The slice thickness was 2 mm and the pixel size 0.65 × 0.65 mm2.
2.3. Development of pneumatic drivers
In the literature, fibrosis has been quantified in pathological muscle (Bensamoun et al. Citation2015). This quantification was realized with Magnetic Resonance Elastography (MRE) technique which is combined with specific pneumatic drivers such as a silicone tube driver (Chakouch et al. Citation2015) wrapped around the thigh. The role of the driver is to generate a non-invasive vibration at the surface of the tissue. In the present study, three pneumatic drivers were developed: a tie shape placed around the neck, a rectangular bar in contact with the lower part of the SCM and a square cushion driver, made of memory form, placed above the collarbone.
2.4. Magnetic resonance elastography (MRE)
MRE is an imaging technique based on the propagation of shear waves in soft tissue allowing the quantification of mechanical properties. To follow the displacement of the waves, the motion encoding gradients in the three orthogonal directions have been performed with four time offsets. Subsequently, the waves have been generated with three different frequencies (60 Hz, 90 Hz, 120 Hz) for each pneumatic drivers in order to select the best wave propagation in the SCM. Moreover, different wave amplitudes (from 50 to 100%) have been tested to make the wave deeply penetrate the muscle.
Phase images were collected with a gradient-echo sequence (flip angle:20°; field of view: 24 cm; acquisition matrix: 256 × 256; TR/TE = 50.0/20.3, 55.5/14.1 and 58.3/11.3 ms at 60 Hz, 90 Hz and 120 Hz, respectively). The acquisition times per direction were 59 s, 54 s and 56 s at 60 Hz, 90 Hz and 120 Hz, respectively. Image processing has been performed with a directional filtering (Manduca et al. Citation2003) to limit the effects of interferences and cartography of elasticity has been obtained with inversion algorithm (Manduca et al. Citation2001).
3. Results and discussion
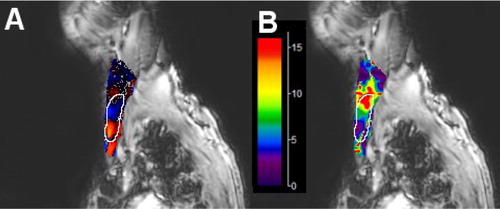
showed shear waves in the SCM muscle and the associated cartography of shear modulus (µ) (). This result has been obtained with the square cushion driver, a frequency of 90 Hz, an amplitude of 90% and a motion encoding applied in the anterior-posterior direction. These parameters associated to the cushion driver allow to consistently visualize the propagation of the waves in the SCM. However, shows a heterogeneous cartography with a red spot revealing an irregular propagation of the waves due to experimental problems. The next step will be to obtain a better propagation with consistent wavelength along the SCM. The variation of wavelength induced a high (7.91 kPa) standard deviation. The average shear modulus (7.76 kPa) in the region of interest, represented by white border line, is in agreement with other studies which have performed shear wave elastography on SCM (Ewertsen et al. Citation2018, Liu et al. Citation2015) but must be confirmed with additional MRE tests. These results (phase image, elasticity) show the feasibility of this MRE protocol to quantify the mechanical properties of SCM muscle.
Figure 2. Phase image (A) and elastic shear modulus (µ=E/3) image in kPa (B) in the region of interest of SCM represented by white border line.
This MRE protocol will be further improved by adjusting the placement of the driver in a reproducible way. The next step will be to apply this protocol for patient having neck muscle fibrosis after radiotherapy, and to correlate quantitative measurements (elasticity, viscosity) to the subjective results obtained with functional and clinical scales, in patients with different stages of fibrosis.
4. Conclusions
There is currently a significant lack of studies on the treatment of complications and side effects of radiotherapy. The present protocol could bring a decisive element (benefit/risk ratio) to better guide the patients for surgical treatment and/or reirradiation.
Acknowledgements
We thank the Mayo Clinic (Dr Ehman) for its technical support.
Additional information
Funding
References
- Bensamoun SF, Charleux F, Debernard L, Themar-Noel C, Voit T. 2015. Elastic properties of skeletal muscle and subcutaneous tissues in Duchenne muscular dystrophy by magnetic resonance elastography: a feasibility study. IRBM. 36(1):4–9.
- Chakouch MK, Charleux F, Bensamoun SF. 2015. Quantifying the elastic property of nine thigh muscles using magnetic resonance elastography. Plos One. 10(9):e0138873.
- Davis AM, Dische S, Gerber L, Saunders M, Leung SF, O'Sullivan B. 2003. Measuring postirradiation subcutaneous soft-tissue fibrosis: state-of-the-art and future directions. Semin Radiat Oncol. 13(3):203–213.
- Ewertsen C, Carlsen J, Perveez MA, Schytz H. 2018. Reference values for shear wave elastography of neck and shoulder muscles in healthy individuals. Ultrasound Int Open. 04(01):E23–E29.
- Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, Slotman BJ. 2008. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol. 26(22):3770–3776.
- Liu KH, Bhatia K, Chu W, He LT, Leung SF, Ahuja AT. 2015. Shear Wave Elastography-A new quantitative assessment of post-irradiation neck fibrosis. Ultraschall in Med. 36(04):348–354.
- Manduca A, Lake DS, Kruse SA, Ehman RL. 2003. Spatio-temporal directional filtering for improved inversion of MR elastography images. Med Image Anal. 7(4):465–473.
- Manduca A, Oliphant TE, Dresner MA, Mahowald JL, Kruse SA, Amromin E, Felmlee JP, Greenleaf JF, Ehman RL. 2001. Magnetic resonance elastography: Non-invasive mapping of tissue elasticity. Med Image Anal. 5(4):237–254.
- Moloney EC, Brunner M, Alexander AJ, Clark J. 2015. Quantifying fibrosis in head and neck cancer treatment: an overview. Head Neck. 37(8):1225–1231.