1. Introduction
Around 5% of all traumas result in Peripheral Nerve Injuries (PNI). More than one million people per year are affected in Europe and the USA (Chen et al. Citation2015), and healthcare costs are estimated to exceed £1Bn per year in the USA alone (Grinsell and Keating Citation2014). Paralysis and loss of sensation are hallmarks of severe PNIs, which can lead to lifelong pain and loss of autonomy for patients. Current treatments for large-gap PNIs use an autograft to bridge between proximal and distal nerve stumps, inducing donor-site morbidity and with underwhelming functional recovery in many cases (Palispis and Gupta Citation2017).
Engineered Neural Tissue (EngNT, Georgiou et al. Citation2013), which comprises cylindrical anisotropic cellular hydrogels surrounded by a sheath of material to mimic the properties of nerve tissue, is being developed to address these issues. EngNT constructs provide a supportive microenvironment to promote neurite and blood vessel growth between nerve stumps, and the technology enables careful spatial seeding of therapeutic cells to facilitate this.
Here we consider vascularisation of the injury site, which is essential to deliver nutrients (e.g., oxygen, glucose) to the evolving cell population. Seeded cells, under low oxygen conditions, release vascular endothelial growth factors (VEGF); diffusive gradients of VEGF act as chemical cues for the migration of endothelial cells (EC) and formation of a new microvessel network (Odedra et al. Citation2011). This raises a range of both fundamental and applicative questions such as how to model the complex arrays of mechanisms underlying vessel growth? Or what seeded cell distribution will facilitate revascularisation, maximise long-term cell density and improve nerve repair?
2. Methods
Investigating such questions using experiments in isolation can be costly and time consuming that is why we propose here a mathematical framework to explore the impact of different seeded cell distributions upon oxygen concentration, cell densities, VEGF gradients and vascular network formation. This framework comprises a cell-solute model, parameterised against in vitro data, which quantify cell density, oxygen uptake and VEGF release at a range of ambient oxygen conditions (Coy et al. Citation2020), overlaid with a discrete model for endothelial sprout growth, blood flow and intravascular transport of oxygen. This framework considers the EngNT as a cylinder of cell-seeded hydrogel surrounded by an impermeable sheath of material, so that molecular exchanges with the outside tissue and EC invasion only happen at the proximal and distal stumps.
In this context, the cell-solute model considers the cell-seeded hydrogel as a continuum, so that cell density along with oxygen and growth factor concentrations are described through a system of coupled non-linear diffusion-reaction equations. Coupling terms include cell proliferation at high oxygen concentration, upregulation of VEGF secretion at low oxygen concentration and oxygen consumption by the cells.
With regard to angiogenesis, we consider the sprouts to be composed of a Tip Endothelial Cell (TEC) attached to a string of Stalk Endothelial Cells (SECs). the TEC explores the hydrogel cylinder in a stochastic manner, starting from the nerve stumps, with a biased towards high VEGF concentration and gradient. As a sprout grows, a fraction of its SECs can become TECs, effectively branching out, creating tree-like structures. Then, when a TEC meets another sprout, a loop is formed, allowing the blood to flow, perfusing the network with oxygen. The blood flow itself is solved using a pore-network model that considers the blood as a monophasic, non-Newtonian fluid with an apparent viscosity (Lorthois et al. Citation2011). Regarding the intravascular transport of oxygen, we assimilate the vessels as one-dimensional elements and extend the effective advection-diffusion-reaction equation describing the cross-section average concentration derived by Berg et al. (Citation2020) for a generic nutrient to the case of oxygen. The coupling between this model and the cell-solute model is achieved by means of a membrane condition with an effective permeability to describe the local flux of oxygen going from the vessel to the hydrogel.
3. Results and discussion
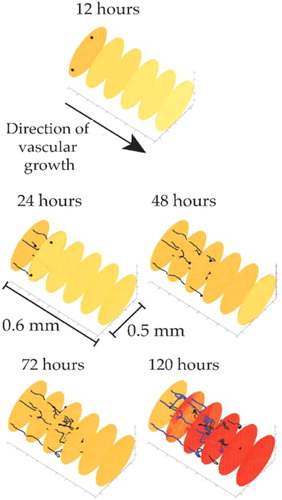
First simulations were run using MATLAB for the resolution of the angiogenesis, blood flow and intravascular transport model and coupled with COMSOL Multiphysics for the resolution of the cell-solute interactions. These simulations were performed for a range of increasing initial cell density, including non-uniform seeding, highlighting that the largest initial cell densities do not necessarily lead to the best revascularisation. Results also include the spatial and temporal distribution of oxygen and growth factors throughout the EngNT, and the complex interplay between these distributions, the cell density, and evolution of the vascular network as illustrates.
4. Conclusions
The proposed framework indicates new avenues for cell seeding strategies that may accelerate vascularisation of a repair construct and increase long-term cell density. In this way, it can be used to explore a wide variety of parameters and help inform future repair strategies as well as being integrated with experiment to improve the fundamental understanding of nerve repair.
Additional information
Funding
References
- Berg M, Davit Y, Quintard M, Lorthois S. 2020. Modelling solute transport in the brain microcirculation: is it really well mixed inside the blood vessels? J Fluid Mech. 884:A39.
- Chen S-L, Chen Z-G, Dai H-L, Ding J-X, Guo J-S, Han N, Jiang B-G, Jiang H-J, Li J, Li S-P, et al. 2015. Repair, protection and regeneration of peripheral nerve injury. Neural Regen Res. 10(11):1777–1798.
- Coy R, Al-Badri G, Kayal C, O'Rourke C, Kingham PJ, Phillips JB, Shipley RJ. 2020. Combining in silico and in vitro models to inform cell seeding strategies in tissue engineering. J Royal Soc Interface. 17(164):20190801.
- Georgiou M, Bunting SCJ, Davies HA, Loughlin AJ, Golding JP, Phillips JB. 2013. Engineered neural tissue for peripheral nerve repair. Biomaterials. 34(30):7335–7343.
- Grinsell D, Keating CP. 2014. Peripheral nerve reconstruction after injury: a review of clinical and experimental therapies. Biomed Res Int. 2014:698256.
- Lorthois S, Cassot F, Lauwers F. 2011. Simulation study of brain blood flow regulation by intra-cortical arterioles in an anatomically accurate large human vascular network: Part I: Methodology and baseline flow. Neuroimage. 54(2):1031–1042.
- Odedra D, Chiu LL, Shoichet M, Radisic M. 2011. Endothelial cells guided by immobilized gradients of vascular endothelial growth factor on porous collagen scaffolds. Acta Biomater. 7(8):3027–3035.
- Palispis WA, Gupta R. 2017. Surgical repair in humans after traumatic nerve injury provides limited functional neural regeneration in adults. Exp Neurol. 290:106–114.