?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
Radcliffe’s principle of lateral stabilization (Radcliffe Citation1955) was the theoretical basis of many socket designs. It describes the balance of the weight, generating a moment at the hip, of the amputated person thanks to the socket design. This principle was summarised in Pritham (Citation1990). Considering subischial sockets, the pelvic tilt induced by this moment is stabilised when the femur is abducted and pressures the lateral wall of the socket thanks to the gluteus medius (GM) action. Yet, this often leads to painful shear stresses in the medial tissues of the thigh. On the contrary, ischial containment sockets (ICS) rely on an ischial support to compensate the pelvis tilt which reduces the need for the GM activation. However, this support is often pointed out to be uncomfortable. In ICS, the frontal balance of the amputated person is a trade-off between the force applied on the support and the forces of the muscles. Evaluation of muscle forces is thus crucial to improve people’s stability and comfort in their prosthesis. This could be achieved with musculoskeletal (MSK) modelling. However, few 3-dimensionnal models have been developed for transfemoral amputation in the literature (Bae et al. Citation2007; Mohamed Citation2018), and none of these models considered the vertical action applied by the ischial support. However, as emphasized by Pritham (Citation1990) it can be hypothesized that more than 83% of the amputated person’s weight is carried by the ischial support. Therefore, the moment at the hip induced by the ischial support cannot be neglected. This study presents a method to predict muscle forces in the residual limb from inverse dynamic and static optimisation from an MSK model. This method was applied on one transfemoral (TF) amputated person with different percentages of loading on the ischial support to evaluate its influence on muscle force estimation. The results were also compared to one Gritti–Stokes (GS) amputated subject for whom there is no ischial support. Muscles are also less impaired in GS amputations.
2. Methods
2.1. Data acquisition
One right GS (BMI = 27.4 cm kg−2) and one left TF (BMI = 26 cm kg−2) amputated subjects were involved in this study. Both underwent amputation more than seven years prior to this study. The protocol combined motion analysis data and whole-body EOS radiography in the upright position (EOS®, EOS-Imaging, France) following the protocol described in Al-Abiad et al. (Citation2020). Mean values of kinematic and dynamic variables were computed for the optimization.
2.2. Musculoskeletal modelling
The MSK model was implemented on Matlab (MATLAB R2014b The MathWorks, Inc., Natick, Massachusetts, United States). The OpenSim model Gait 2354_simbody (Seth et al. Citation2018) was used to define generic muscle insertions in bones anatomical frames and generic maximal isometric forces per muscle. Insertions that were distal to the amputation level were placed at the extremity of the residual femur.
2.3. Personalisation of MSK models
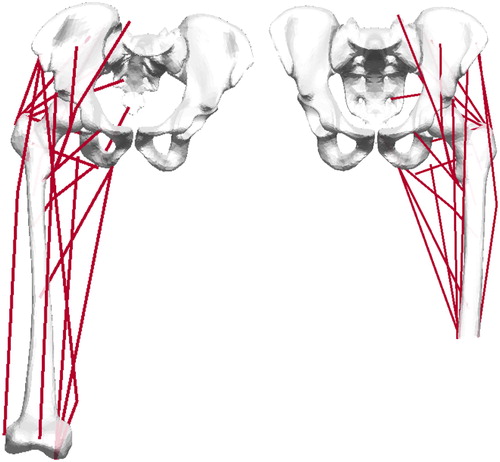
EOS reconstructions were used to define personalized bone geometries (Mitton et al. Citation2006; Chaibi et al. Citation2012). Subject-specific origins and pathways of muscles were computed from kriging of generic muscle points using bone mesh nodes as control points ().
2.4. Static optimisation
Static optimisation was based on the method proposed by Son et al. (Citation2012). The objective function is presented in EquationEquation (1)(1)
(1) and the conditions to be satisfied in EquationEquation (2)
(2)
(2) .
(1)
(1)
(2)
(2)
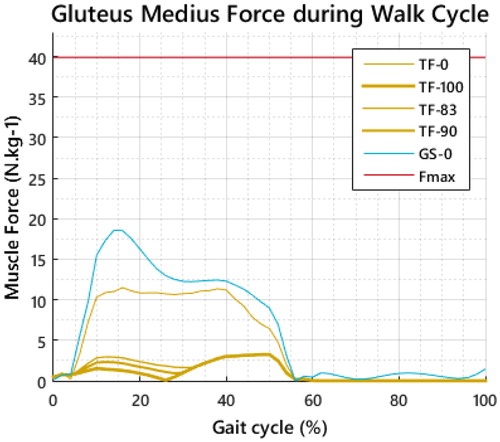
where n is the number of muscles, Fi the force of the ith muscle, Fmax the maximal isometric force, r the muscular lever arms and M the moment at the hip deduced from inverse dynamics. Lever arms were computed using effective origins and insertions of muscles as in Zajac and Gordon (Citation1989). The authors hypothesized no ischial support for the GS subject while this support was assumed to decrease the adduction/abduction moment by 83, 90 and 100% for the TF subject. Prediction with no ischial support (0%) was also computed for comparison purposes.
3. Results and discussion
Results are only detailed for the GM as it is the main muscle responsible for the lateral stabilisation. Differences in the strategy of walking are noticeable comparing both types of amputation with 0% ischial support since the GM is more recruited by the GS subject (). The influence of the ischial support is also noticeable for the TF subject: the lower the adduction moment, the lower the GM action. As explained earlier: the tilting of the pelvis must be balanced by the femur abduction through the GM action. Moreover, as the support under the ischial tuberosity increases in ICS, the need for abduction is reduced. Pattern and force of activation are supported by electromyographic (EMG) studies (Wentink et al. Citation2013).
4. Conclusions
Evaluation of muscle forces is relevant to understand walking strategies of amputated subjects. Such results could be implemented in finite element modelling to study the interaction between the residual limb and the socket by adding muscles to the model to improve pressure prediction at the interface. Further studies are needed to accurately estimate the percentage of vertical loads supported by the ischial support and to evaluate the results with, for example, EMG data.
Acknowledgements
The authors thank the INI/CERAH and Julia Facione (HIA Percy) and volunteers who participated in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Al-Abiad N, Pillet H, Watier B. 2020. A mechanical descriptor of instability in human locomotion: experimental findings in control subjects and people with transfemoral amputation. Appl Sci. 10(3):557.
- Bae TS, Choi K, Hong D, Mun M. 2007. Dynamic analysis of above-knee amputee gait. Clin Biomech. 22(5):557–566.
- Chaibi Y, Cresson T, Aubert B, Hausselle J, Neyret P, Hauger O, de Guise JA, Skalli W. 2012. Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Eng. 15(5):457–466.
- Mitton D, Deschênes S, Laporte S, Godbout B, Bertrand S, de Guise JA, Skalli W. 2006. 3D reconstruction of the pelvis from bi-planar radiography. Comput Methods Biomech Biomed Eng. 9(1):1–5.
- Mohamed A. 2018. Modeling and simulation of transfemoral amputee gait. [Place unknown]: University of New Brunswick.
- Pritham CH. 1990. Biomechanics and shape of the above-knee socket considered in light of the ischial containment concept. Prosthet Orthot Int. 14(1):9–21.
- Radcliffe CW. 1955. Functional considerations in the fitting of above-knee prostheses. Artif Limbs. 2(1):35–60.
- Seth A, Hicks JL, Uchida TK, Habib A, Dembia CL, Dunne JJ, Ong CF, DeMers MS, Rajagopal A, Millard M, et al. 2018. OpenSim: simulating musculoskeletal dynamics and neuromuscular control to study human and animal movement. PLoS Comput Biol. 14(7):e1006223
- Son J, Hwang S, Kim Y. 2012. A hybrid static optimisation method to estimate muscle forces during muscle co-activation. Comput Methods Biomech Biomed Eng. 15(3):249–254.
- Wentink EC, Prinsen EC, Rietman JS, Veltink PH. 2013. Comparison of muscle activity patterns of transfemoral amputees and control subjects during walking. J Neuroeng Rehab. 10(1):87.
- Zajac FE, Gordon ME. 1989. Determining muscle’s force and action in multi-articular movement. Exerc Sport Sci Rev. 17(1):187–230.