1. Introduction
According to WHO figures, the number of toothless people in the world is increasing (Douglass et al. Citation2002). Thus, counted at 34 million in 2000, the figure would be around 38 million in 2020 in the United States. This increase is linked to an increase in life expectancy correlated with an increase in toothlessness with age (Bourgeois et al. Citation1999). The development of new technologies is a necessity in order to cope with the increasing needs.
The CAD/CAM (computer-aided design and computer-aided manufacturing) system changed the manufacturing concepts of complete dentures. After decades of artisanal manufacturing by the pack-and-press technique, then by injection, the milling process of polymerized PMMA discs reverses the denture elaboration chain by placing the polymerization upstream of the shaping.
The purpose of this study was to compare the mechanical properties, Vickers hardness, wettability, and roughness of three different denture base resins after aging ().
Table 1. Denture base materials according their manufacturing processes.
2. Methods
2.1. Materials
2.2. Aging
3 samples (20 × 4 × 2 mm) of each material were artificially aged in artificial saliva at 55 °C, 75 °C or 90 °C for 0, 30, 60 days.
2.3. Three-point flexural test
Modulus of elasticity and ultimate flexural strength were measured by a 3-point flexural test using an AGS-X 5kNX Serie testing machine (Shimadzu Corporation) and Trapezium software. The distance between supports was 15 mm. The penetration speed was 5 mm/min.
2.4. Contact angle test
The wettability was tested with sterile water and measured using a DropMaster DMs 401 Contact Angle Measuring Stand (Kyowa Interface Science Co., Ltd.) and FAMAS software.
2.5. Measure surface roughness
Surface roughness was measured using a 3D microscope VHX-5000 (Keyence) at x1000 magnification and VHX software.
2.6. Vickers microhardness test
Vickers microhardness was evaluated using Metkon’s MH-3 microdurometer at 500 g load for 20 seconds.
2.7. Fracture surface analysis
The fracture surfaces were analyzed using the JSM-6400 (JEOL) scanning electron microscope (SEM) at x50 and x500 magnifications. The images were acquired using Orion (Saturn) software.
2.8. Test statistics
ANOVA (Tukey’s test) tests, Shapiro-Wilk tests, and t-tests were used for statistical analyses (α=.05).
3. Results and discussion
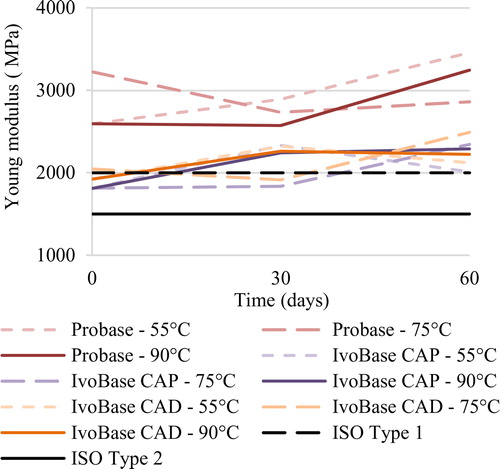
After 60 days, the mechanical properties of the 3 PMMA resins complied with the ISO 20795-1: 2013 standard. During the aging process, all three materials followed the same kinetics and evolution. The modulus of elasticity increased (), the ultimate flexural strength decreased, and the Vickers microhardness decreased. This reflected a change in the behavior of the materials. As a result, during aging, the stiffness of PMMA resins increased. They became more brittle and more prone to fracture. On the other hand, the decrease in their hardness during aging corroborated this hypothesis (Hae‐Hyoung et al. Citation2012). It should be noted that the fracture facies of the materials retained their initial characteristics. The conventional resin had a distinctive more brittle behavior as compared to the High Impact resins which underwent more deformation before fracture.
Limited roughness optimizes wettability and therefore has a positive influence on the retention quality of complete dentures. The threshold for roughness is defined by the patient comfort and the need to facilitate hygiene (Cortés-Sandoval et al. Citation2015). All three resins exhibited low roughnesses throughout the aging process, consistent with the initial polishing. The wettability of the complete dentures reflects the retention ability of the dentures (Jin et al. Citation2009). It should be noted that the use of Ringer's solution for this type of evaluation would have had little or no influence due to its protein-free composition. Indeed, wettability is mainly affected by the presence of protein elements. The different resins showed a hydrophilic behavior favorable to the retention of the prostheses. On the other hand, the oral environment is subject to significant changes in temperature and pH, as well as bacterial aggression. These elements remain to be taken into consideration in the aging process of complete removable prostheses whose life expectancy varies between 5 and 7 years (Rignon-Bret and Rignon-Bret Citation2002).
The new processes made it possible to change the composition of PMMA materials. The old requirements for limiting polymerization shrinkage were circumvented with the injection process and allowed the addition of plasticizers. Machinable discs are the result of this evolution and display properties closer to injected materials than conventional materials (Pacquet et al. Citation2019).
4. Conclusions
The results presented are preliminary. The results of this study suggest that resin bases manufactured by machining are in compliance with the ISO 20795-1: 2013 standard (3). Resins machined by CAD/CAM technology have properties equivalent to injection molded resins. Therefore, they combine the advantages of the latter while standardizing their manufacturing processing.
Acknowledgements
We would also like to show our gratitude to the URB2i teamwork and Ivoclar-Vivadent which provided the denture base materials.
No potential conflict of interest was reported by the authors.
Disclosure statement
References
- Bourgeois D, Berger P, Hescot P, Leclercq MH, Doury J. 1999. Oral health status in 65-74 years old adults in France, 1995. Rev Epidemiol Sante Publ. 47(1):55–59.
- Cortés-Sandoval G, Martínez-Castañón GA, Patiño-Marín N, Martínez-Rodríguez PR, Loyola-Rodríguez JP. 2015. Surface roughness and hardness evaluation of some base metal alloys and denture base acrylics used for oral rehabilitation. Mater Lett. 144:100–105.
- Douglass CW, Shih A, Ostry L. 2002. Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent. 87(1):5–8.
- Hae‐Hyoung LE, Chung‐Jae LE, Asaoka K. 2012. Correlation in the mechanical properties of acrylic denture base resins. Dent Mater J. 31:157–164.
- Jin N-Y, Lee H-R, Lee H, Pae A. 2009. Wettability of denture relining materials under water storage over time. J Adv Prosthodont. 1(1):1–5.
- Pacquet W, Benoit A, Hatège-Kimana C, Wulfman C. 2019. Mechanical Properties of CAD/CAM Denture Base Resins. Int J Prosthodont. 32(1):104–110.
- Rignon-Bret C, Rignon-Bret J. 2002. Prothèse amovible complète Prothèse immédiate Prothèses supraradiculaire et implantaire. Paris: Editons CdP.