Abstract
Background
Overuse of antibiotics and inappropriate prescribing has resulted in rapid development of antimicrobial resistance. Most antibiotics in the United Kingdom (71.4%) are prescribed in primary care by general practitioners, with about half prescribed for viral rather than bacterial illnesses.
Aims
To explore antibiotic prescribing and factors which may influence maternal decision making to seek antibiotics for their young children.
Methods
Data for children under five years were gathered using a mixed-methods case study approach. Quantitative general practice antibiotic prescribing data (n = 697 children) was statistically analysed and these results were further explored in six focus groups with mothers (n = 19) of children under five. The qualitative data was thematically analysed.
Results
Quantitative data identified nearly half of children received antibiotics. Children under one were prescribed the fewest antibiotics. Qualitative focus group data showed mothers trusted their general practitioner to provide expert care for their child and often wanted convenient and timely access to advice and reassurance rather than treatment.
Conclusion
Antibiotics are frequently prescribed for young children in primary care. Healthcare professionals need to understand the maternal influences contributing to antibiotic use in children and consider strategies and interventions to reduce unnecessary antibiotic prescriptions.
Impact statement-implications for research/practice
Nurses and health visitors should have a greater role in supporting maternal decision making for managing their children’s illnesses.
Introduction
The increased global use of antibiotics in healthcare, food production and animal welfare has raised real concerns over the development of antimicrobial resistance (AMR) (World Health Organisation (WHO), Citation2018). The onset of AMR is random and occurs when some microorganisms survive initial antibiotic exposure. This results in any surviving microorganisms passing on their resistant genes to the next generation. Consequently, the next time the microorganisms are exposed to the same antibiotic, it is more likely to survive, resulting in the antibiotic becoming less effective (WHO, Citation2018).
In England, 307 million primary care consultations are conducted annually (NHS Digital, Citation2018). Most antibiotics (71.4%) are prescribed by General Practitioners (GPs), who are doctors working in community services (Public Health England (PHE): English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR), 2019). It is estimated that at least 20% of all antibiotics are prescribed inappropriately (PHE, Citation2018; Smieszek et al., Citation2018), leading to increased morbidity and mortality rates and rising healthcare costs (O’Neill, Citation2016: WHO, Citation2018).
Despite most childhood illnesses being caused by self-limiting viruses (Neill et al., Citation2016), antibiotic use is especially high among children (Aversa et al., Citation2021). However, high antibiotic use is now contributing to an increase in AMR in children under five years of age (PHE, ESPAUR, Citation2018). As a result, children are presenting with more complex and difficult to treat infections, which may require longer antibiotic courses and increase the risk of AMR (PHE, ESPAUR, Citation2018). It is often difficult for clinicians and parents to identify serious illness and their related, causative organisms. For example, symptoms of fever may be caused by viral infections (not requiring antibiotics) or life-threatening bacterial infections, which require prompt antibiotic treatment, tht is, sepsis (National Institute of Health and Care Excellence (NICE), Citation2016). Therefore, despite the increased awareness of AMR, diagnostic uncertainty may influence clinicians to prescribe antibiotics ‘just in case’ (Horwood et al., Citation2016) as a safer course of action (Cabral et al., Citation2015). Additionally, parents may have difficulty judging illness severity and may seek reassurance (O’Neill, Citation2016) and expert medical advice regarding their children’s care (Bosley et al., Citation2018; Ingram et al., Citation2013). As such, further exploration relating to antibiotic prescribing practices is needed to understand maternal influences towards using antibiotics for their children.
2. Aim of the study
The aim of this paper is to explore antibiotic prescribing and factors that may influence maternal decision making to seek antibiotics for their young children. This paper is drawn from a larger doctoral study, exploring mothers’ experiences and expectations of using antibiotics to treat their young children in primary care.
3. Methods
A mixed-methods case study approach was chosen. The core principle of mixed methods is, when used in combination, quantitative and qualitative approaches provide a better understanding of the research question than either approach alone (Creswell, Citation2003). The quantitative phase involved the collection and analysis of GP antibiotic prescribing data, which was used to identify any key questions for further exploration in the qualitative focus groups. A case study approach was selected to describe, explain and explore everyday phenomena in their natural settings (Yin, Citation2014). It allows multiple data collection, quantitative and qualitative (Gerring, Citation2006; Yin, Citation2014), to explore a contemporary topic (maternal attitudes to antibiotic prescribing) in a real situation (local diverse population).
3.1. Case study setting
This study was conducted within a large UK city in Southern England. The case study boundary was set using postcodes, as this allowed statistical information regarding socioeconomic status and ethnicity of the local population to be collected from independent sources such as government departments. By using established communities, useful demographic and contextual data is often obtained and can be used to contextualise the population and explain the nature of the case (Bosley et al., Citation2019; Jackson et al., Citation2017a, Citation2017b). According to the Office of National Statistics (Citation2016), the population of this area is the most diverse in the county. This population includes families with young children and professional and non-professional people. The unemployment rate is 6.1% against the national average of 4.9%. Housing is a mix of private and rental properties, with 13.2% of properties provided by the local authority, compared to 7.5% in England. Most residents are aged between 16 and 49 years, with about 8% aged between 0 and 16 years old. There is a range of ethnic diversity, with approximately 11.7% recorded as Muslim, compared to 6.8% in the rest of the city. This local community data was used to identify a clearly defined accessible population to address the research phenomena. The participants were included in the study if they could speak, read and understand English and could provide informed consent.
3.2. Ethics
Ethics approval was obtained from the sponsoring University Faculty Research Ethics Committee (February 2017) and from the National Research Ethics Service (NRES) in May 2017 (application 217969).
3.3. Recruitment and data collection
All GP practices, in the case location, were approached to be included in the study to provide antibiotic prescribing data for children under five years of age, which minimised sampling bias. The study also used a research protocol, which explicitly outlined the process of data collection and analysis (Bryman, Citation2012).
3.4. Quantitative phase
All GP practices (n = 8) within the case were initially contacted via email and phone and invited to participate. Study information was provided, however, only one GP practice submitted data. This practice was the second largest in the case, consisting of over 13,000 registered patients and equating to 21% of the total case population. Of the patients registered in this practice, 5.9% (808) were aged between birth-four years (PHE, Citation2017) which equated to the average percentage of children under four registered with GP practices within the study setting. Basic demographic data was requested regarding the age of the children, reasons for consultations and antibiotics prescribed. A full year’s data was requested to reduce any seasonal variation (July 2016–2017). Antibiotic prescribing data was sought to contextualise the case and provide information on the frequency of antibiotics prescriptions and the conditions commonly treated.
3.5. Qualitative phase
The sample population was mothers, who are often the primary carers of young children and therefore involved in key decision making regarding their children’s health. Focus groups with mothers of children under five, living within the case study area were conducted. Participants were identified via local play groups and through searching publicly accessible websites, including local council-run programmes, mum’s networks, social media pages, local community centres, and by use of word of mouth. Play-leaders were initially contacted via email and study information sent with a request to attend the play group sessions. Once written approval was received, sessions were attended by the first-named author, who provided participant information to attending mothers. Once verbal consent was agreed upon, focus groups were arranged. All sessions were digitally recorded, and written consent was obtained prior to participation. A total of six focus groups (n = 19) were held to explore mothers’ expectations, attitudes and experiences of using antibiotics for their children. A topic guide was developed based on research identified in the literature review and contained questions relating to mothers’ experiences, beliefs, influences and knowledge of using antibiotics.
Focus group questions included:
Can you tell me about the last time you visited your GP?
Can you talk to me about the last time you received antibiotics for your child?
Mothers were recruited from a broad range of age, ethnicity and socio-economic backgrounds, and a convenience sampling strategy was used to recruit as many mothers, who attended local playgroups with their children to the focus group study, as possible. The data was analysed following each focus group and data saturation was considered to have been reached when ‘additional data did not lead to any new emergent themes’ (Given, Citation2016, p. 135).
3.6. Data analysis
The research team spent considerable time determining the best approach to analysis of the quantitative data. Unfortunately, due to the limited data categories available and a substantial amount of missing data, it was deemed inappropriate to carry out additional statistical tests ON those that are described in the manuscript. Where possible, we conducted relevant statistical tests such as Chi-Square, but due to the nature of the dataset, descriptive statistics were felt to be more appropriate for the remaining data. Therefore, Microsoft Excel was deemed sufficient mechanism to support this analysis.
Qualitative data from the focus groups were digitally recorded, transcribed and thematically analysed. Each transcript was coded initially by the lead author, to identify initial themes. All data were anonymised, and any identifiable information was removed. The data was charted using Microsoft Excel software to provide a framework to order and manage the data and consisted of columns (cases) and rows (codes). Each cell summarised the data by category from the transcripts and recorded references to illustrative quotes. Words, patterns and themes were generated by drawing comparisons within and across the dataset (Ritchie & Lewis, Citation2003). Using Braun and Clarke’s approach to data analysis, themes were identified through a rigorous process of data familiarisation, data coding, theme development and revision (Braun & Clarke, Citation2013). Themes were then discussed with the full research team until a consensus was reached.
4. Results
4.1. Quantitative phase
4.1.1. Participant demographics
The number of children seen in each age range was similar, however, the specific age of the child was not captured only the age range (i.e. 0–12 months, 13–24 months).
4.1.2. Quantitative findings
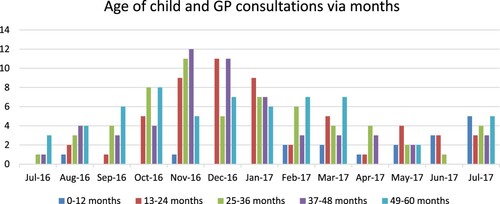
The data set revealed seasonal variations in the number of GP consultations undertaken (). and most consultations took place between November-January.
Children were prescribed antibiotics on the same day of the consultation. The relationship between days of the week antibiotics was prescribed, and the age of the child was analysed using a chi-square test. The analysis identified there was no statistically significant day of the week for consultations in any of the age groups (p = .05). In each age group, the test statistic was not more than the critical value of 9.49 (p = .05); therefore, there was no relationship in any age group. provides a summary of these results.
Table 1. Chi-square Test results.
Descriptive statistics suggested children aged 0–12 months were more frequently issued antibiotics on a Friday (39%), followed by the 25–36 months old (25%). Antibiotic prescriptions were more frequently issued on a Thursday in the 13–24 months old (32%) and 37–48 months old (25%) and Tuesday for 49–60 months old (28%) ().
Table 2. Antibiotics issued by day of the week.
The number of children seen in each age range was similar, however, the exact age of the child was not captured only the age range (i.e. 0–12 months, 13–24 months) ().
Table 3. Number and percentage of children prescribing antibiotics following GP consultations per age group.
Although similar numbers of children were seen across the age ranges, children aged 0–12 months did not receive as many antibiotic prescriptions, with only 13.7% of consultations resulting in antibiotic prescriptions, compared to 36.5% of children aged between 13 and 24 months. However, even when combining both these younger age groups (0–24 months), the number of children receiving antibiotics was still only 50.2% and not much higher than the other age groups. Children aged between 25 and 36 months received the highest number of antibiotics (45%), compared to 42% of children aged between 37 and 60 months ().
4.2. Common infections receiving antibiotics
Only basic information including age of child, consultation date, type of antibiotic prescribed, and condition was recorded within the primary care dataset. The data did record the common infections seen by the GPs, resulting in an antibiotic prescription (). The most common infections treated with antibiotics were respiratory (chest/cough), followed by ear infections. The exception was children aged 0–12 months, when respiratory and ear infections were prescribed equally (22.5%). Over a third (37.7%) of children aged between 13 and 24 months received antibiotics for chest infections, followed by ear infections (20.7%). In children aged 25–36 months, 35.5% received antibiotics for a cough or a diagnosis of chest infection and 11.8% of antibiotics prescriptions were for ear infections.
Table 4. Top two reasons children received antibiotics per age group.
In children aged 37–48 months, 26.8% of antibiotic prescriptions were for chest infections or chesty coughs, followed by 23.2% of antibiotic prescriptions for ear infections. A diagnosis of a chesty cough (28%) or chest infection (8.6%) collectively resulted in 36.6% of antibiotic prescriptions in children aged 49–60 months, followed by ear infections (16.6%).
4.3. Efficacy and appropriateness of antibiotics prescribed
Amoxicillin was the most common antibiotic prescribed and is the recommended antibiotic for treating chest infections or ear infections, suggesting GPs are generally following prescribing guidelines. The age group with the highest prescribing compliance was for children between 13 and 24 months (84.9%). However, the use of phenoxymethylpenicillin in the older age groups to treat symptoms of fever, cough or sore throats was not the first line treatment in local prescribing guidelines resulting in prescribing variation within the age ranges ().
Table 5. Most frequently prescribed antibiotics per age group in a single GP practice.
With overall prescribing compliance being 78%, this indicates prescribing does not always follow the approved guidelines. However, it is difficult to ascertain from the data whether all prescriptions were appropriate as the rationale for antibiotic and diagnosis was not documented for all consultations. For example, the data set does not capture whether the child has a penicillin allergy, which would affect prescribing choice.
5. Results
5.1. Qualitative findings
5.1.1. Participant demographics
The demographic characteristics of group participants were mainly White, British, educated to degree level and aged between 26 and 35 years of age ().
Table 6. Characteristics of parent focus group participants (n = 19).
The majority (n = 17) of mothers were White, one was Black and one Asian, British. Most were aged between 26 and 35 years of age (n = 12). Four mothers were European, one Asian, one mother described herself as of mixed nationality and one from Oceania. The highest education achieved ranged from school (n = 2), college (n = 2), diploma (n = 2), degree (n = 12), to doctorate (n = 1). Sixteen mothers were married, and three described themselves as single. Nine mothers had only one child (see ).
Table 7. Number of children per participant age group.
Two main themes were found following thematic analysis of focus groups: seeking reassurance for maternal uncertainty; recognising maternal concerns, behaviours and triggers.
5.1.2. Theme 1: seeking reassurance for maternal uncertainty
All mothers acknowledged they used the NHS website for information, which was considered a reliable source. Most mothers used the internet to research symptoms and potential treatments, which they used to inform their expectations of the GP visit. However, most mothers still preferred to be seen by a clinician, for reassurance, despite feeling they knew what the illness may be.
The internet it’s not a one stop shop. I want to be mentally ready for what I’m going to hear when I go to the doctors. The more I read, the more concerned and I’m sure the doctors aren’t going to lie to me they do actually know. FG 1
Although this theme was present throughout the narratives, it may be that mothers of very young children visit their GP to seek reassurance more readily than mothers with older children. All mothers acknowledged the lack of experience of being a first-time mother influenced their reasons for seeing a GP.
I would always go to the doctor to get their advice and listen to the doctor, cos I think as a first-time mum not knowing what to do. FG 6
This reassurance was sought from experienced, qualified health professionals even when mothers felt they knew what the problem was. There was a sense of needing reassurance and affirmation that their child was not seriously ill, and most mothers sought this reassurance from a consultation and physical examination. Some mothers expressed concern if an illness was not identified and treated in a timely manner, as lasting damage may occur.
If it scars his lungs he’s going to have it for the rest of his life. How would you know ifsomething is wrong if you don’t check? FG 2
Although mothers preferred to see a GP, they would consider making an appointment with other healthcare professionals, including health visitors and practice nurses. Health visitors were perceived differently within the focus groups and decisions to access health visiting services depended on whether there was an established personal relationship.
I find I can always go to my health visitor. I got the same one for all three of my kids, but I guess it’s the continuity cos she knows my three, I feel I can trust and ask do you think I should go or what do you reckon. FG 3
A couple of mothers reported when they had asked for general advice regarding a child’s health including rashes and temperatures, the health visitor had advised them to see a GP.
I found them not very helpful. I did speak to them about his rash, but they were like, we don’t know. FG 1
Several mothers expressed they were happy to see a practice nurse, following good prior experience and just wanted a healthcare professional (a trained experienced professional) to see their children for reassurance.
A nurse would be is fine … … . they’re trained, aren’t they? FG 6
They trusted the practice nurse’s advice as they were seen as healthcare trained and some mothers felt the nurses may have extra training which would inform, their expertise.
Nurses at the practice who are doing it like extra training so they can field stuff for the doctor. I’m more than happy to go and see one of the nurses. FG 3
Most mothers felt that it was difficult to know what was wrong with young children as their children were unable to verbalise what they were feeling. Mothers felt illness was easier to manage when children could communicate their feelings and symptoms.
It’s easier to manage with a child who can tell you what is going on. FG 3
Some mothers did say they would try and persuade GPs to prescribe antibiotics to avoid return appointments. Whilst other mothers were content to use weekend or out of hours GP services, some were not, with reasons being a previously poor experience, long waiting times and inconvenient locations.
I think I’m not going to come back; I’ve gone all out to get this appointment so want it dealt with today. FG 1
My son is prone to tonsillitis and my doctor likes to give him antibiotics for it, cos he’s got enlarged tonsils anyway and he’s really prone to it. So, when I call up they say ok we’ll send over a prescription for some antibiotics and we don’t even generally go in anymore. FG 3
All mothers identified the importance of trusting the GP’s decision-making regarding their child’s illness. These feelings of trust influenced whether mothers were willing to wait before starting antibiotic treatment. However, some mothers expressed feelings of guilt for waiting too long to seek treatment and that may have resulted in a perception of prolonged suffering for their child.
He was miserable. I don’t want him to be ill longer than he needs to be. FG 3
It was more trusting he (GP) was making the right decision to hold back, so I did feel a bit guilty in the end as she (child) did actually need it(antibiotics). FG 1
These feelings were especially experienced by mothers whose children had ended up being prescribed antibiotics.
6. Discussion
By using mixed methods, GP quantitative and focus group qualitative data has provided an insight into the correlation between antibiotic prescribing practices and maternal attitudes, experiences and expectations of using antibiotics for their children. In children 0–12 months, GP data indicated fewer antibiotic prescriptions were issued. Although these results are not statistically significant, analysis of focus group narratives (theme one) suggested mothers may be seeking medical reassurance rather than treatment; these findings correspond with findings from other studies (Brookes-Howell et al., Citation2013: Maguire et al., Citation2018). This included first-time mothers who felt less confident managing their child’s illness and who therefore wanted medical reassurance (Rousounidis et al., Citation2011). Mothers were also more anxious with young children, who were not able to tell them what was wrong, contributing to GP visits. However, older children are likely to have more exposure to common circulating viruses from contact and interaction with other potentially infectious children. This is commonly via communal childcare settings, such as nurseries or playgroups. These activities and environments involve close contact and often crowding, resulting in exposure to other potentially infectious children (Rooshenas et al., Citation2014). Older children were also more likely to be prescribed antibiotics, for chest infections, as their age increased, which could be due to increased clinician confidence in their diagnosis (Williams et al., Citation2018).
The day of the week antibiotics was issued was variable across the age ranges and not statistically significant. However, the most common day, in children 0–12 months, was Friday. Analysis of the focus groups suggested mothers may seek appointments with their own GP prior to the weekend, to avoid using out of hours services with GPs they did not know. Some mothers also identified the issue of convenience and felt once they had an appointment, they were reluctant to leave without feeling adequately reassured.
Mothers’ decisions to seek a GP appointment were influenced by the perceived severity of the illness. This included mothers asking for antibiotics and return GP visits if it was felt they were needed. Other factors influencing maternal decision making included previous positive experiences of antibiotic use and emotional influences such as a feeling of guilt watching their child suffering. The results from the GP prescribing data do not identify whether antibiotics were prescribed under the ‘just in case’ approach, which is a delayed prescription in cases of diagnostic uncertainty (Cabral et al., Citation2016; Lucas et al., Citation2015). Reasons for antibiotics prescriptions were not documented in 4.8% (n = 32/697) of the consultations. Finally, although prescribing practices generally reflected local guidelines, it was difficult to ascertain true compliance due to the lack of data available or inaccurate coding regarding individual prescribing decisions (Smieszek et al., Citation2018). Further information and support for mothers from healthcare professionals may ensure mothers have confidence in their decision making. The findings indicate that seeking reassurance about their child’s health is a substantial contributor to mothers asking for treatments in the form of antibiotics.
Our study found mothers expressed a willingness to access alternative professionals for support and advice, which they valued. Nurses and other health professionals offer additional resources and services to support antibiotic stewardship and managing maternal experiences and expectations to using antibiotics (Johnstone, Citation2016). A way to increase access would be to relocate health visitors’ services within GP practices as they previously were and return to child health clinics being held in GP practices. Practice nurses’ roles could be developed and broadened to include appointments for minor illness, which would release GP appointment times, thereby increasing appointment time and capacity for other patients. The benefits of improving utilisation of primary care services will result in longer-term cost savings by improving health and wellbeing (NHS England, Citation2016). Within the context of the study, less antibiotics may be prescribed if mothers are adequately reassured, thereby reducing the risk of inappropriate antibiotics prescribing and the development of AMR.
7. Study limitations
In primary care services, there are variations in the patient record data base systems. This meant the data available was limited as data such as ethnicity, or socio-economic background was not recorded. Consultations require manual data entry to include a reason for presentation, action taken, and any medication prescribed and relies upon accurate documentation. Also, the data does not capture whether the same child was seen on more than one occasion or detail the antibiotic prescribing rationale. For example, a child may present on more than one occasion before receiving antibiotics. The data does also not provide information on the actual dose prescribed for the child, just the quantity dispensed. Therefore, it is not possible to know if the dose and duration of the prescription were appropriate for the condition being treated. The prescribers may also be different, and therefore, personal preferences may influence prescribing practices. The relatively small sample size should be acknowledged; however, by using mixed methods, rich and detailed information was provided from the focus groups that informed results.
8. Conclusion
This paper has identified some patterns between GP prescribing practices and how mothers feel using of antibiotics for their children. Although this is a relatively small study, data suggests mothers’ seek reassurance and timely access to healthcare professionals, especially for young children. By understanding the influences and motivators for mothers accessing and seeking GP services, measures can be developed to provide more support to mothers in their decision making, with an aim to reduce appointments and a possible reduction in antibiotics prescribing. Further research would be beneficial using accurate and detailed antibiotic prescribing practices for children to gain a more in-depth and robust understanding of practices and ultimately to reduce antibiotics exposure and the inevitable development of AMR.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aversa, Z., Atkinson, E., Schafer, M., Theiler, R., Rocca, W., Blaser, M., & LeBrasseur, N. (2021). Association of infant antibiotic exposure with childhood health outcomes. Mayo Clinic Proceedings, 96(1), 66–77. https://doi.org/https://doi.org/10.1016/j.mayocp.2020.07.019
- Bosley, H., Appleton, J. V., Henshall, C., & Jackson, D. (2019). Using local communities to establish geographical boundaries for case studies. Nurse Researcher. https://doi.org/https://doi.org/10.7748/nr.2019.e1623
- Bosley, H., Henshall, C., Appleton, J. V., & Jackson, D. (2018). A systematic review to explore influences on parental attitudes towards antibiotic prescribing in children. Journal of Clinical Nursing, 27(5-6), 892–905. https://doi.org/https://doi.org/10.1111/jocn.14073
- Braun, V., & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners. Sage.
- Brookes-Howell, L., Wood, F., Verheij, T., Prout, H., Cooper, L., Hood, K., Melbye, H., Torres, A., Godycki-Cwirko, M., Fernandez-Vandellos, P., Ystgaard, M., Falk Taksdal, T., Krawczyk, J., & Butler, C. (2013). Trust, openness and continuity of care influence acceptance of antibiotics for children with respiratory tract infections: A four-country qualitative study. Family Practice, 31(1), 102–110. https://doi.org/https://doi.org/10.1093/fampra/cmt052
- Bryman, A. (2012). Social research methods (4th ed.). Oxford University Press.
- Cabral, C., Ingram, J., Lucas, P., Redmond, N., Kai, J., Hay, A., & Horwood, J. (2016). Influence of clinical communication on parents antibiotic expectations for children with respiratory tract infections. The Annals of Family Medicine, 14(2), 141–147. https://doi.org/https://doi.org/10.1370/afm.1892
- Cabral, C., Lucas, P., Ingram, J., Hay, A., & Horwood, J. (2015). “It’s safer to … ” parent consulting and clinician antibiotic prescribing decisions for children with respiratory tract infections: An analysis across four qualitative studies. Social Science & Medicine, 136-137, 156–164. https://doi.org/https://doi.org/10.1016/j.socscimed.2015.05.027
- Creswell, J. W. (2003). Research design: Qualitative and quantitative approaches and mixed methods approaches. Sage.
- Gerring, J. (2006). Case study research: Principles and practices. Cambridge University Press.
- Given, L. M. (2016). 100 questions (and answers) about qualitative research. Sage.
- Horwood, J., Cabral, C., Hay, A., et al. (2016). Primary care clinician antibiotic prescribing decisions in consultations for children with RTIs: A qualitative interview study. British Journal of General Practice, 66(644), 207–213. https://doi.org/https://doi.org/10.3399/bjgp16X683821
- Ingram, J., Cabral, C., Hay, A., Lucas, P., & Horwood, J. (2013). Parents’ information needs, self-efficacy and influences on consulting for childhood respiratory tract infections: A qualitative study. BMC Family Practice, 14(1), 1. https://doi.org/https://doi.org/10.1186/1471-2296-14-106
- Jackson, D., Durrant, L., Bishop, E., Walthall, H., Betteridge, R., Gardner, S., Coulton, W., Hutchinson, M., Neville, S., Davidson, P., & Usher, K. (2017a). Health service provision and the use of pressure-redistributing devices: Mixed methods study of community dwelling individuals with pressure injuries. Contemporary Nurse, 53(3), 378–389. https://doi.org/https://doi.org/10.1080/10376178.2017.1364973
- Jackson, D., Durrant, L., Bishop, E., Walthall, H., Betteridge, R., Gardner, S., Coulton, W., Hutchinson, M., Neville, S., Davidson, P., & Usher, K. (2017b). Pain associated with pressure injury: A qualitative study of community-based, home-dwelling individuals. Journal Advanced Nursing, 1–9. https://doi.org/https://doi.org/10.1111/jan.13370
- Johnstone, M. J. (2016). Editorial: The moral significance of antimicrobial resistance and the rise of ‘apocalyptic superbugs’. Journal of Clinical Nursing, 25(15-16), 2079–2082. https://doi.org/https://doi.org/10.1111/jocn.13350
- Lucas, P., Cabral, C., Hay, A. D., & Horwood, J. (2015). A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care. Scandinavian Journal Primary Health Care, 33(1), 11–20. https://doi.org/https://doi.org/10.3109/02813432.2015.1001942. Epub 2015 Feb 26. PMID: 25716427; PMCID: PMC4377734.
- Maguire, F., Murphy, M. E., Rourke, M., Morgan, F., Brady, G., Byrne, E., & O'Callaghan, M. E. (2018). A cross-sectional study of antibiotic prescribing for childhood upper respiratory tract infections in Irish general practice. Irish Medical Journal, 111(10), 835.
- National Institute of Health and Care Excellence (NICE). (2016). Sepsis: Recognition, diagnosis and early management (CG 51). London. Retrieved from May 7, 2021, from https://www.nice.org.uk/guidance/ng51
- Neill, S. J., Jones, C. H., Lakhanpaul, M., Roland, D. T., & Thompson, M. J. (2016). Parents’ help-seeking behaviours during acute childhood illness at home: A contribution to explanatory theory. Journal of Child Health Care, 20(1), 77–86. https://doi.org/https://doi.org/10.1177/1367493514551309
- NHS Digital. (2018). Retrieved from May 7, 2021, from https://digital.nhs.uk/data-and information/publications/statistcal-appointments-in-general-practice
- NHS England. (2016). General practice forward view. Retrieved from April 21, 2021, from https://www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf
- Office of National Statistics. (2016). Retrieved from July 3, 2021, from https://www.ons.gov.uk/
- O’Neill, J. (2016). Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. Review on Antimicrobial Resistance. Wellcome Trust and HM Government. Retrieved from July 3, 2021, from https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
- Public Health England. (2017). Retrieved from July 3, 2021, from https://fingertips.phe.org.uk/profile/general practice/data#page/10/gid/2000005/pat/152/par/E38000136/ati/7/are/K84004
- Public Health England. (2018). English Survillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2018, London. Retrieved from July 3, 2021, from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/759975/ESPAUR_2018_report.pdf
- Ritchie, J., & Lewis, J. (2003). Qualitative research practice: A guide for social science students and researchers. Sage.
- Rooshenas, L., Wood, F., Brookes-Howell, L., Evans, M., & Butler, C. (2014). The influence of children’s day care on antibiotic seeking: A mixed methods study. British Journal of General Practice, 64(622), e302–e312. https://doi.org/https://doi.org/10.3399/bjgp14X679741
- Rousounidis, A., Papaevangelou, V., Hadjipanayis, A., Panagakou, S., Theodoridou, M., Syrogiannopoulos, G., & Hadjichristodoulou, C. (2011). Descriptive study on Parents’ knowledge, attitudes and practices on antibiotic Use and misuse in children with upper respiratory tract infections in Cyprus. International Journal of Environmental Research and Public Health, 8(12), 3246–3262. https://doi.org/https://doi.org/10.3390/ijerph8083246
- Smieszek, T., Pouwels, K. B., & Dolk, F. C. K. (2018). Potential for reducing inappropriate antibiotic prescribing in English primary care. Journal Antimicrobial Chemotherapy, 73(Supplement 2), ii36–ii43. https://doi.org/https://doi.org/10.1093/jac/dkx500
- Williams, M. R., Greene, G., Naik, G., Hughes, K., Butler, C. C., Hay, A. D. (2018). Antibiotic prescribing quality for children in primary care: An observational study. British Journal of General Practice, 68(667), e90–e96. https://doi.org/https://doi.org/10.3399/bjgp18X694409
- World Health Organisation. (2018). Retrieved from April 13, 2018, from http://www.who.int/mediacentre/factsheets/fs194/en/
- Yin, R. K. (2014). Case study research design and methods (5th ed.). Sage.