Abstract
Despite the potential benefits of mobile health (mHealth) services and applications, older adults face challenges and barriers to adopt mHealth. Published work on opportunities and challenges of mHealth for aging China has focused on trends in mHealth and its clinical applications, but not older adults’ perceptions or their processes of adoption. In this study, questionnaires and interviews were conducted to understand older adults’ perceptions and adoption of mHealth services in China. Conceptual models were generated using existing theories and refined using the findings of the user research. The proposed “pine tree model” illustrates the factors influencing Chinese older adults’ adoption of mHealth services and describes the process for better adoption. Based on the research, suggestions were proposed to promote mHealth adoption among older adults, which will inform better design of mHealth for the aging population in China.
1. Introduction
In 2020, the global population aged 60 years and older was already greater than 1 billion, representing 13.5% of the world’s population (WHO, Citation2020). With the extension of people’s life-span, “living a healthier independent life” becomes the main aspiration of older adults (Plaza et al., Citation2011), and “ensuring universal health coverage” becomes part of the United Nations’ sustainable development goals (Kuruvilla et al., Citation2018).
Mobile health (mHealth) is defined as the “medical and public health practice supported by mobile technologies” (WHO, Citation2011). It allows the general population to collect and manage their health data anytime and anywhere (Bashshur et al., Citation2011; Free et al., Citation2013; Kumar et al., Citation2013). The benefits of mHealth include encouraging healthy behaviors (Free et al., Citation2013), reducing or avoiding the emergence of health problems, helping patients with chronic diseases in self-management (Beratarrechea et al., Citation2014), and making possible real-time communication with doctors (Klasnja & Pratt, Citation2012; Shen et al., Citation2017). The amount of research on mHealth and older adults is rising rapidly (Tajudeen et al., Citation2021). Sun et al. (Citation2016) reviewed the trends in mHealth for aging China from the perspective of its clinical applications. In 2019, the rate of Chinese smartphone ownership reached 96% (iResearch, Citation2020). With the fast spread of smartphones, mHealth nowadays is also characterized by the use of mHealth applications (apps) that can be operated using smartphones (Perry et al., Citation2019).
Given the potential benefits mHealth services and apps can bring to older adults, it is important to understand older adults’ perception and adoption of mHealth services, thus helping better promote mHealth among them.
Factors influencing older adults’ adoption of mHealth services are often investigated in studies on technology acceptance. Although technology adoption/acceptance among older adults is not a new topic, studies on mHealth adoption among older people are far fewer than those on general technology adoption among older people (Berkowsky et al., Citation2017; Chen & Chan, Citation2011; Wang et al., Citation2017).
The technology acceptance model (TAM) and its extended variations (i.e., TAM2, TAM3, UTAUT, and UTAUT2) have been widely used in research on mHealth adoption (Alam et al., Citation2018; Deng et al., Citation2018; Leung & Chen, Citation2019; Miao et al., Citation2017; Schnall et al., Citation2015). The three original TAM factors, namely “perceived usefulness,” “perceived ease of use,” and “attitude toward use,” have been confirmed by the published studies as the main factors driving older adults’ intention to use mHealth apps (Askari et al., Citation2020). Different factors have been added to extend the existing models by researchers to explain older adults’ adoption of mHealth in different contexts. Deng et al. (Citation2018) extend the TAM with “trust” and “perceived risks” in studying mHealth adoption in China (Deng et al., Citation2018), and similar findings can be seen in a recent study in the Netherlands (Klaver et al., Citation2021). Alam et al. (Citation2018) add “perceived reliability” and “price value” to UTAUT in investigating mHealth adoption in Bangladesh (Alam et al., Citation2018). Salgado et al. (Citation2020) extend UTAUT2 with “personal empowerment,” which consists of consumer logic, processional logic, and community logic, through a survey in Portugal (Salgado et al., Citation2020).
Since mHealth adoption is a type of health behavior, the health belief model (HBM) and protection motivation theory (PMT) also prove helpful to understand mHealth adoption. In the research of health behavior, personal factors such as e-health literacy (Chan & Kaufman, Citation2011), self-efficacy (Lv et al., Citation2012), perceived vulnerability, perceived severity, and health consciousness (Cho et al., Citation2014) have also been listed as influencing factors to people’s adoption of health information technologies.
Most of the existing studies focus on the relationship between the influencing factors and the intention to adopt mHealth services, aiming to validate the dominant factors of mHealth adoption through quantitative analysis. However, older adults’ perceptions of mHealth and the process of how they adopt mHealth services have been largely neglected.
To complement published work, the authors conducted a qualitative inquiry in China to examine how older adults perceive and adopt mHealth services from a process perspective. The main objectives of this study are to:
Understand the perceptions of older adults and their perceived barriers to the adoption of mHealth.
Develop a conceptual model to help designers better understand not only the main factors but also the process of how older adults adopt mHealth services.
Propose suggestions to improve mHealth services and better promote mHealth among Chinese older adults.
2. Developing a preliminary model
Many different models (i.e., TAM, TAM2, TAM3, UTAUT, UTAUT2, HBM, and PMT) have been used in the study of mHealth adoption. The factors in these models tend to differ in names, but some have similar meanings. Therefore, the authors extracted the constructs in related models according to our research context by merging similar ones and generated a new theoretical model as the basis of this research.
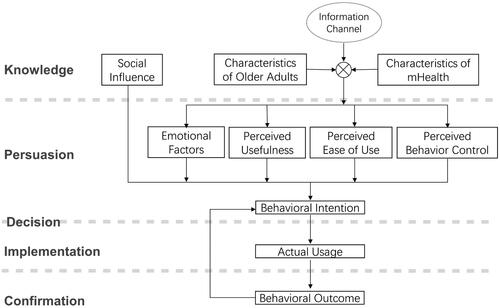
The new constructs are shown in . Since this research was conducted on older adults, and they could choose whether to use mHealth services by themselves, the authors excluded irrelevant factors such as “voluntariness” and “job relevance.”
Table 1. Constructs extracted from existing models.
The diffusion of innovation theory was introduced to explain the process of mHealth adoption. The theory was developed by E. M. Rogers in 1962; it has been used to study a variety of innovations. It explains how an idea, practice, or object diffuses and is accepted by people. The innovation, communication channels, time, and the social system are the four main elements of the diffusion process (Rogers, Citation2010). mHealth services or apps can be seen as innovations, hence the use of this theory in our study.
A typical mHealth adoption decision has five stages (see the text description on the left in ):
Knowledge: know how the mHealth service/app functions
Persuasion: formulate the intention of adopting mHealth services/apps based on intrinsic and extrinsic motivations
Decision: decide whether to adopt or reject the mHealth service/app
Implementation: actual use of the mHealth service/app
Confirmation: get reinforcement or reverse previous decision after using the mHealth service/app
The authors put the constructs from existing models into the five stages (). “Information channel” and “behavioral outcome” were added according to the diffusion of innovation theory.
Older adults’ perception of mHealth services is often formulated by their interaction with the service; the “characteristics of older adults” and the “characteristics of mHealth” should be taken into consideration. Existing research proves that user characteristics such as age, gender, education, and income (Czaja et al., Citation2006; Guo et al., Citation2015; Mitzner et al., Citation2014) affect people’s adoption of mHealth. Since our study places the emphasis more on building a conceptual model to describe the process of mHealth adoption among older adults in general, these factors were put together as “the characteristics of older adults.” Individual differences were not discussed in this paper.
This preliminary model () was built based on the analysis and synthesis of literature that is not specific to the Chinese context. The authors shall introduce how the model was developed further with primary data collection in China.
3. Methods
To develop and evaluate the preliminary model for the Chinese context, a qualitative study with Chinese older adults was conducted.
3.1. Participants
A total of 30 older adults were interviewed between July and August 2018. Convenience sampling was used; it is cost effective and has been widely accepted in information system studies (Ritchie et al., Citation2013). Participants were recruited from Gulin Community (n = 16), Yutang Community (n = 9), and Nanhu Community (n = 5) in Nanjing, China. The characteristics of the participants are shown in .
Table 2. Characteristics of the participants.
In Human Computer Interaction (HCI) studies, “old age” can be “any age older than 50.” In this study, the authors recruited “well-old users (Foong, Citation2016)” aged between 50 and 70 years. People with serious disease/impairments and aged older than 70 years were excluded; this was to ensure participants’ independence in taking part in the study (requiring mobility and basic understanding of the digital technology). The average age of the participants was 59.60 (SD = 4.63, range = 50–69).
Existing research suggests that health condition is influential to people’s intention to use mHealth services (Cho et al., Citation2014). Therefore, in this study, the participants were asked to rate their own perceived health condition from 1 to 5 (1 for “poor” and 5 for “excellent”).
The participation was voluntary. Before the study began, the participants had been told that all personal information would remain confidential, data gathered in the study would be stored anonymously and securely, and they could withdraw from the study at any time without giving a reason.
3.2. Data collection
The main elements in the preliminary model () were investigated in detail through a 15-minute questionnaire and a follow-up interview (about 30–60 minutes). Conducting face-to-face interviews after questionnaires can not only help get more detailed information from the participants but also help rectify any misunderstanding of the answers.
The questionnaire consists of five parts:
Part 1: basic demographic information, for example, age, gender, and education.
Part 2: barriers to the use of mobile products such as smartphones/tablets, for example, how aging factors impact the participants’ use of mobile products.
Part 3: mHealth and technology adoption, for example, how often the participant uses a health-related app/information.
Part 4: importance of mHealth functions, for example, for self-assessment, health monitoring, and communication with a doctor online.
Part 5: reasons for having/not having a smartphone/tablet.
To understand older adults’ “perceived behavior control” of using mHealth services (e.g., mobile apps), the participants were asked to rate how different age-related changes might stop them from using an app in Part 2, for example, “visual impairment,” “hearing loss,” “decline in memory,” “decline in the ability to understand written and spoken languages,” “decline in the ability to focus attention,” and “decline in movement control” (Fisk et al., Citation2020). “Generation gap” was also added because the authors found from our pilot study that older adults had difficulties in understanding new terms generated by the younger generation. For example, they were confused by the “menu” or “navigation” of a digital interface.
The interview had two steps. In step 1, older adults with or without mHealth service experience were not distinguished. Having mobile devices was used as the starting point to study their perception of mHealth services. The details of step 1 are shown in .
Table 3. Details of the interview: step 1.
To understand older adults’ “perceived usefulness” of mHealth services, the participants were asked to evaluate different types of mHealth services. The authors selected the top 50 health-related apps in both App Store (the iOS system) and Tencent MyApp (the Android system), and decomposed them into 13 different functions for evaluation.
The lack of understanding of mHealth services can lead to people’s reluctance to adopt mHealth services. Communication channel is important for innovation diffusion; therefore, information channels were investigated in step 1.
In step 2, the participants who had experience of using mHealth apps (n = 15) were interviewed in depth; the authors explored their process of adoption of mHealth services.
3.3. Data analysis
Descriptive statistics were used to summarize the participants’ characteristics and outline the general situation of mHealth adoption among older adults in China. Qualitative data from interviews were analyzed with the thematic analysis method. Quotations from the participants were referenced to support research statements. The interview data were analyzed with Braun and Clarke’s six-step thematic analysis approach (Braun & Clarke, Citation2006). The deductive approach (Fereday & Muir-Cochrane, Citation2006) was applied to continually reflect on, and refine, emerging themes. The deductive coding framework was synthesized using the theories of behavior change (e.g., Fogg behavior model [Fogg, Citation2009] and hooked model [Eyal, Citation2014]).
4. Results
4.1. Adoption of mHealth apps
Among all the participants, 30 (100%) can access the Internet and have a smartphone, 15 (50%) have a personal tablet, and 10 (33.3%) have smart wristbands. The average age of these participants was 59.70 (SD = 4.25, range = 54–67). Twenty out of the 30 participants had a positive perception (scores 4–5) of their own health.
All the participants had used their smartphone for health purposes, but only half of them (n = 15, 7 male, 8 female) had used mHealth apps. The mHealth apps they used are shown in . The main reasons for not using mHealth services are “never heard about it,” “no interest,” and “no need.” Some participants did not believe mHealth apps could effectively improve their health.
Table 4. mHealth apps used by the participants.
4.2. Perception of mHealth services
4.2.1. Perceived usefulness of mHealth services
To understand Chinese older people’s perceived usefulness of mHealth services, the participants were asked to evaluate 13 different functions using a scale from 1 to 5 (1 means “this function is not useful at all” and 5 means “this function is very useful”).
As shown in , the most highly valued function is “health monitoring,” followed by “for emergency” and “self-assessment or self-diagnose.” Most of the participants thought mHealth service was not essential. As one participant noted:
Table 5. Evaluation of mHealth functions.
It is a good service, but not necessary to me. I’m satisfied with life without it (P12, male, 64).
The participants were asked the reason for giving a low score (<3). From their answers, we found these older adults had evaluated the usefulness by weighing the benefits mHealth may bring to them against the cost. Their perceived benefits of mHealth depended on three aspects:
(1) Compatibility of their lifestyle. Only services in line with older adults’ daily medical habits were perceived to be useful. Some participants had their own way of taking care of themselves.
I’m not a health professional. Why should I use an app [to] self-diagnose instead of seeing a doctor? (P18, male, 62).
I usually print my health reports and put them in order; I don’t want to use an app for this (P21, female, 66).
Except for medical habits, some older adults had their specific attitude toward life.
(For) people at my age, we prefer to live as what we want (P7, male, 59).
I have my own living habit and I don’t want to use an app to tell me what to do (P15, female, 53).
(2) Obvious advantage. The older adults regarded “usefulness” as not about the mHealth service itself, but as the relative comparison with its competitors. Compared with their own way of taking care of themselves, the participants did not perceive sufficient advantages of using an mHealth app.
There is health preservation information everywhere, I don’t need more (P2, female, 57).
I can get information of the medicine from instructions or inside the package (of the medicine); I don’t think I need an app for that (P16, male, 63).
One participant who had used the function of online doctor consultation said:
I still have to go to hospital after I talked with a doctor online, then why bother? (P8, female, 52).
(3) Information reliability. Although the participants thought some of the functions were very helpful, they did not trust the authority or accuracy of the information, which reduced their rating of the usefulness of these functions.
The measurement by software may be inaccurate. If it’s not accurate, it’s totally useless (P22, male, 57).
I think online diagnosis is impossible with current technology. If you don’t get the correct diagnosis, it will be dangerous (P17, female, 60).
I don’t believe in apps. I think doctors are more reliable (P1, male, 67).
According to the participants, the cost of mHealth meant:
(1) Additional expenses. For those who were very confident in their health condition and independency, they “don’t need it” and they regarded mHealth as additional expenses and gave its “usefulness” a low score. Through interview, we found that these participants cared about the additional expenses of using mHealth.
Do I need to buy other devices? (P9, female, 54).
Does it cost money? If it’s free, I’ll try it (P27, female, 52).
(2) Efforts to learn. The effort to learn to use an app was seen as a cost of using mHealth apps.
Going to hospital is much easier than communicating with a doctor by using an app, which I need to pay much effort to learn (P11, male, 65).
It’s inconvenient (to set a reminder of taking medicine by an app). I’m not familiar with mobile apps. I’d prefer to set my alarm clock than taking a long time to learn to use an app for this. And my daughter always calls me to remind me of taking medicines (P5, female, 58).
(3) Risk of privacy leakage. The concern on privacy had hindered some participants from putting their personal information in their mobile phone or on the Internet.
I don’t want my information to be seen by others; what if I lose my phone? (P14, female, 60).
Will my health record be seen by others? (P17, female, 55).
Who can see the information I uploaded? Where do my data go? (P18, male, 62).
4.2.2. Perceived ease of use of mHealth services
To understand what affects older adults’ perceived ease of use of mHealth apps, the authors asked the participants the following questions in the interview:
What is “ease of use” of an app to you?
Which of these two apps you use is easier, and why?
The factors identified are “clarity of the language,” “text size,” “knowing where (which icon/button) to press,” “knowing what the icon/button means,” “finding what I need easily,” and “knowing how to use without learning,” and some participants pointed out that “too many pop-up ads” were annoying and made an app difficult to use.
4.2.3. Perceived behavior control
The external constraints for mHealth adoption such as access to Internet and ownership of smartphones have been investigated. For internal constraints, the participants ranked how aging factors might stop them from using an app. The higher the score, the greater the influence. The results are shown in .
Table 6. How aging factors influence older people’s adoption of mobile apps.
“Generation gap” has the most influence on older adults’ adoption of mobile apps. “Visual impairments” have the second biggest influence, followed by “decline in memory.”
4.2.4. Information channel
The sources of the older adults’ health information are shown in . The most effective channels for them to receive health information are via the authorities and their interpersonal relationships.
Table 7. Information channel of health information.
The participants’ knowledge of mobile apps came from different sources (shown in ). Similar to health information, interpersonal relationships and social networks play an important role in the diffusion of mHealth apps.
Table 8. Information channel of mobile apps.
4.3. Process of mHealth adoption
The participants with experience of using an mHealth app were interviewed to understand their process of mHealth adoption. The results are summarized into three themes: behavioral triggers, motivation, and suggestions.
4.3.1. Triggers
In the theory of innovation diffusion, “knowledge” is the first stage when people get to know how the mHealth service/app functions. However, in our research, 12 participants initially adopted mHealth apps without “knowledge.” The triggering factors of their initial adoption behavior mainly came from external intervention, such as gifts or recommendations from relatives and friends or giveaways from insurance companies.
Nine participants began their initial adoption of mHealth apps after they were given an mHealth device as a gift: They used it because they did not want to “waste the gift.” Sometimes they did not really know what the app was about, but they did not want to reject the kind advice from people close to them.
Only three participants were self-triggered. They discovered and used mHealth apps by themselves. The apps they use were pre-installed in their phones or from the advertisement forwarded by WeChat (a popular social media app in China).
After an mHealth app was adopted for the first time, how to attract users to use the app again varied depending on the type of the service. The need for medical services (e.g., making appointments with doctors, communicating with doctors online) was a common internal trigger. If they understand the functions of the service, they will actively use the service when in need. Fitness-related apps (e.g., step counter and exercise guide) usually use external triggers such as pop-up reminders to attract users to access the apps.
Most mHealth apps have more than one function. Often a combination of internal and external triggers was used to attract users to reuse the apps. However, frequent single triggers might reduce the effect and even irritate the user. For example, a participant complained:
It [the exercise pedometer] jumps out all the time. I don’t know how to stop it, and I can only ignore this (P7, male, 59).
4.3.2. Motivation
The intention of adopting mHealth services/apps was often related to intrinsic and extrinsic motivations. The intrinsic motivation of mHealth adoption of the participants can be summarized in a threefold manner:
(1) Keeping healthy and independent. Whether the mHealth apps were recommended by others or downloaded by themselves, the older adults were mainly motivated to use them to stay healthy. The use of mHealth also reflects older adults’ desire to be independent and have control over their health conditions.
With this [smart wristband], I can know how many steps I take every day, the quality of my sleep, and whether my heartbeat is abnormal (P23, male, 65).
They did not want to cause trouble to their loved ones.
We should avoid being sick at this age and should not cause trouble to our children (P2, female, 58).
(2) Social belonging. The sense of belonging included integration into the circle of friends; not falling behind the time and becoming old-fashioned. The former was mainly reflected in the use of fitness-related apps:
All my colleagues use this app, and we can see who walks the most (P4, female, 54).
The latter was mainly reflected in the use of apps for making appointments with doctors.
It is very convenient to make appointments with doctors online. Now young people all use this, and I have to keep up with the trend (P19, male, 60).
After retirement, older adults began to worry that they would be out of touch with society, as one who was about to retire mentioned:
After retirement, you still have to contact with colleagues who are not retired and care more about the changes outside. Don’t lock yourself up; otherwise you will know nothing about what’s happening outside (P4, female, 54).
(3) Taking care of their loved ones. Chinese older adults often play an important role in their family, paying much attention to their younger family members.
Young people nowadays are facing great pressure and have no time to take care of themselves. When I see health-related information, I will send [it] to my daughter to make her pay more attention to her health (P2, female, 58).
I use it for contacting the doctor of my grandson. Little kids can easily catch some ailments. It doesn’t necessarily mean that there is a big issue. By contacting the doctor online, I can set my mind at peace (P4, female, 54).
Some participants pointed out that the apps for diagnosing online were mainly used for others rather than for themselves:
I’ll go to the hospital directly whenever I feel sick. It (using the app) was mainly for my friends and relatives. When they are sick and I cannot go to the hospital for them, I will search the symptoms to find out what the problem is and what to pay attention to. If it’s a serious disease, I’ll urge them to go to hospital as soon as possible (P28, female, 60).
The extrinsic motivation of mHealth adoption of the participants are as follows:
(1) Saving time and efforts. Compared with the traditional medical treatment model, mHealth services have obvious advantages: saving time and effort.
Making appointment online is very convenient. I don’t need to queue at the hospital anymore (P4, female, 54).
I can check my health report by this app. If everything is fine, I don’t need to go to hospital just for fetching the report (P19, male, 60).
(2) Rich and diverse health information. Most mHealth services provide much healthcare information, which was liked by the participants.
This app has a lot of health knowledge, which is very interesting. I like learning this knowledge (P6, female, 55).
There are many videos of health lectures by experts, such as this one telling you what you can eat and what you should eat less; I think it is still very useful (P10, female, 59).
(3) Additional rewards. Additional rewards can improve some users’ motivation of using mHealth services continually. They took different forms. Spiritual rewards like “rankings” and “achievement medals” can give users a sense of fulfillment.
Here you can see the ranking of everyone (walking). I keep myself in the top three every day (P21, female, 66).
Economic rewards in the form of virtual currency are also be attractive to the participants:
You can get “gold coins” when you walk, and then you can buy things in this (online) mall with these coins (P3, female, 67).
There are reward points for logging in everyday, and I can use the points to contact the doctors for free (P28, female, 60).
4.3.3. Suggestions
When explaining their adoption of mHealth services, the participants also made some suggestions.
(1) Accessible help. The difficulty perceived by the participants mainly comes from the initial setup of software and wearable devices. They have to register and link their devices to the corresponding apps before starting using mHealth services. They often need help (e.g., from their children) to complete the setup.
I don’t know how to set it up. The wristband was bought by my son, and he set it up for me. He also installed the software. I can use it directly when I get it (P18, male, 62).
They hope they can get some help or training in setting up and using the apps or devices, so they do not need to depend on others.
When some problems occur, I have to wait for my children to come and help me (P5, female, 58).
It would be better if someone of the company (of wristband) can help me anytime I need (P16, male, 63).
(2) Expansion of service contents and scope. The participants who constantly used mHealth services all indicated that the services they used met their expectations and needs. Some participants put forward further improvement expectations of expanding the contents and scope of the services.
I like the health information in it, but the updating is slow. I hope it can be updated frequently (P3, female, 67).
There are only a few doctors for contact at any time like this. It would be nice if more doctors in hospitals could open up this kind of services (P28, female, 60).
Some (examination) reports still have to be retrieved from the hospital, and I hope they can all be viewed online (P4, female, 60).
(3) Improving the effectiveness. The participants who abandoned mHealth services after use expressed dissatisfaction with the effectiveness of the services. The outcome of using the mHealth service did not meet their expectations.
This app is not accurate; sometimes it doesn’t work and there is no record. It is not as good as a traditional pedometer (P6, male, 55).
This can measure steps, heartbeat, and sleep, but in general it’s not very useful. I wonder what are the data for? If these data can be used to predict disease or explain my health conditions, they could be useful (P18, male, 62).
5. Refining the model
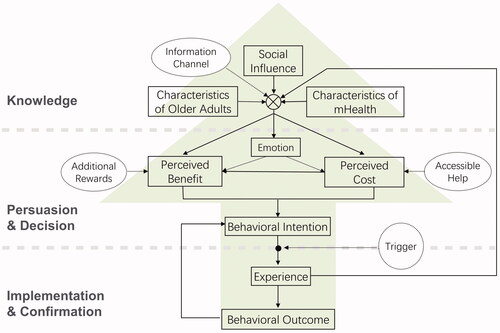
Based on the data collected from the qualitative study conducted with older adults in Nanjing, the authors refined the preliminary model. The pine tree model (shown in ) was proposed to describe the influencing factors and the process of mHealth adoption among Chinese older adults.
The older participants could not differentiate clearly “perceived usefulness,” “perceived ease of use,” and “perceived behavior control” of mHealth. Therefore, the authors replaced them by “perceived benefit” and “perceived cost” as often mentioned by the participants. “Actual usage” was substituted by “experience” and linked back to the knowledge stage in order to make the iterative process of mHealth adoption more understandable.
Other incentives to promote mHealth adoption, namely “triggers,” “accessible help,” and “additional rewards,” were added to the model. The authors gave the model a pine tree shape, making it easy to remember.
The novelty of the pine tree model lies in its combination of technology adoption factors (validated through the user study), the process of adoption (based on the innovation diffusion theory), and design suggestions (drawn from the findings of the study).
6. Design implications
Design implications were extracted to help make mHealth apps more desirable and acceptable to older adults in China.
The implications fall into four categories: suitable information channel, various behavior triggers, obvious benefits, and low cost. Specific suggestions are shown in .
Table 9. Design implications.
7. Discussion and conclusions
As people age, usability barriers may prevent them from using mHealth services (Engelsma et al., Citation2021; Georgsson & Staggers, Citation2016; Wildenbos et al., Citation2018). Wildenbos et al. proposed a MOLD-US framework to summarize the evidence of aging barriers on mHealth use experienced by older adults (Wildenbos et al., Citation2018). They identified four key barriers: cognition, motivation, physical ability, and perception. Based on the MOLD-US framework, Engelsma et al. synthesize barriers to older adults with Alzheimer’s disease and related dementias and further identified two categories: (1) frame of mind and (2) speech and language (Engelsma et al., Citation2021).
Our findings with Chinese older adults (with no dementia) are broadly in agreement with the findings of Wildenbos et al. In addition, our study suggested that the “generation gap” might bring a significant challenge to Chinese older people’s understanding of apps, which could be relevant to language use (Engelsma et al., Citation2021), although our study was with healthy older adults and Engelsma’s study was focused on older adults with Alzheimer’s disease and related dementias.
Our study also explored perceived “usefulness” in greater detail. It was found that Chinese older adults tended to evaluate the usefulness of mHealth by weighing the benefits against the cost. Only services that are compatible with their lifestyle, have obvious advantages, and provide reliable information were perceived to be useful. Additional expenses, efforts to learn, and the risk of privacy leakage were perceived as the cost of adopting mHealth services. Their intrinsic motivation of using mHealth services was to keep healthy and independent; to integrate into the society; and to take care of their loved ones. Their extrinsic motivation of using mHealth included saving time and efforts; getting rich and diverse health information; and getting rewards (spiritual or economical).
7.1. Novelty and contributions
Existing models such as TAM and its extended variations are often used in the studies on older adults’ adoption of technology. In these models, the adoption process usually starts from the “knowledge” stage; however, our study suggested that Chinese older adults’ initial adoption of mHealth services was mainly externally triggered and there were many potential incentives in their adoption process (shown in the dotted circles in ). Informal channels such as interpersonal relationships and social networks play an important role in the diffusion of mHealth services among Chinese older adults. Accessible help and additional reward may encourage their adoption of mHealth services.
The significance of the study lies in its two contributions to the mHealth field.
7.1.1. Theoretical contribution
Our conceptual models were generated based on literature review and user research. The pine tree model (shown in ) not only illustrated the factors influencing older adults’ adoption of mHealth services but also showed their adoption process and design suggestions. It described older adults’ adoption of mHealth services as an iterative process. The factors in all stages are important: People may break the loop and stop using mHealth services at any stage.
7.1.2. Practical contribution
The authors not only investigated older adults’ perceptions and adoptions of mHealth but also proposed suggestions to promote mHealth adoption among older adults. Existing design suggestions (e.g., Engelsma et al., Citation2021) were extracted from published papers. In our study, the design implications and specific suggestions (shown in ) were built upon the findings of our user study to support better design of mHealth services, and they were incorporated into the pine tree model to assist designers.
7.2. Limitations and future work
Several limitations should be noted. First, our sample size is relatively small. User characteristics such as age, gender, education, and income (Czaja et al., Citation2006; Guo et al., Citation2015; Mitzner et al., Citation2014) affect their adoption of mHealth. However, due to the small sample, this study could not make meaningful comparison of the differences. All the participants were from urban areas in Nanjing; they were relatively well educated and all had access to Internet and smartphones. They do not represent the general older population of China where many live in rural areas and do not have access to the Internet or smartphones. However, our participants can be seen as “early adopters” of mHealth services; the high rates of Internet and smartphone ownership of the participants make this research more focused on the acceptance and perception of mHealth services and less affected by factors such as the lack of access to the Internet/devices.
Second, in our study the number of apps covered is limited, and only 15 (50%) participants had experience using mHealth apps. However, the authors had selected typical mHealth apps for both iOS and Android systems and summarized the most popular functions. As the participants represent more affluent urban older adults, their 50% adoption rate of mHealth services suggests that among the general older population in China, the adoption of mHealth is probably much lower than 50%, despite the very high (more than 95%) smartphone ownership. mHealth also has the potential to achieve the accessibility and equality of high-quality medical resources (Sun et al., 2016). In our study, most of the mHealth apps used by the participants were developed by technology companies or Internet companies rather than credible bodies of health care, and the samples did not cover a broad range of older population, so it was difficult to explore mHealth’s potential on accessibility and equality of high-quality medical resources.
Future work will involve a larger sample size with a broader geographic coverage and more mHealth apps (especially those developed by credible organizations). The pine tree model can be further refined, and its value will be tested by designers of mHealth services/apps.
7.3. Conclusions
This article uncovered Chinese older adults’ perception and adoption of mHealth services using qualitative data collected from questionnaires and interviews in Nanjing, China. The study has achieved the three objectives outlined:
To understand the perceptions of older adults and their perceived barriers to the adoption of mHealth: The barriers identified were not only the usability issues caused by older adults’ decline of physical, perception, and cognitive capabilities but also usefulness issues reflected typically by their comparison of cost against benefits.
To develop a conceptual model to help designers: A pine tree model was developed to help designers better understand not only the main factors but also the iterative process of how older adults adopt mHealth services. The model has incorporated technology adoption factors, the process of adoption (based on the innovation diffusion theory), and design suggestions.
To propose suggestions to improve mHealth services: Design suggestions (e.g., suitable information channel, various behavior triggers, obvious benefits, and low cost) were proposed to improve mHealth services and better promote mHealth among Chinese older adults.
The nuanced usability issues enriched the current understanding of barriers to mHealth adoption among older adults; the pine tree model and design suggestions extracted from the user study will help better mHealth services in the future.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
Jing Pan
Jing Pan is a lecturer in College of Art and Design, Nanjing Tech University. She obtained her PhD from College of Architecture and Urban Planning, Tongji University. She was a visiting PhD student at Queen Mary University of London. Her research interest mainly focuses on inclusive design, service design, and user experience.
Hua Dong
Hua Dong is Dean of Brunel Design School. She is Fellow of the Design Research Society and the convenor of DRS InclusiveSIG. Hua shares her passion and expertise in inclusive design through around 200 publications, invited speeches at international conferences, and initiating new courses and research programs.
References
- Alam, M. Z., Hu, W., & Barua, Z. (2018). Using the UTAUT model to determine factors affecting acceptance and use of mobile health (mHealth) services in Bangladesh. Journal of Studies in Social Sciences, 17(2), 137–172.
- Askari, M., Klaver, N. S., van Gestel, T. J., & van de Klundert, J. (2020). Intention to use medical apps among older adults in the Netherlands: Cross-sectional study. Journal of Medical Internet Research, 22(9), e18080. https://doi.org/10.2196/18080
- Bashshur, R., Shannon, G., Krupinski, E., & Grigsby, J. (2011). The taxonomy of telemedicine. Telemedicine Journal and e-Health: The Official Journal of the American Telemedicine Association, 17(6), 484–494. https://doi.org/10.1089/tmj.2011.0103
- Becker, M. H. (1974). The health belief model and personal health behavior. Health Education Monographs, 2(4), 409–473. https://doi.org/10.1177/109019817400200407
- Beratarrechea, A., Lee, A. G., Willner, J. M., Jahangir, E., Ciapponi, A., & Rubinstein, A. (2014). The impact of mobile health interventions on chronic disease outcomes in developing countries: A systematic review. Telemedicine Journal and e-Health: The Official Journal of the American Telemedicine Association, 20(1), 75–82. https://doi.org/10.1089/tmj.2012.0328
- Berkowsky, R. W., Sharit, J., & Czaja, S. J. (2017). Factors predicting decisions about technology adoption among older adults. Innovation in Aging, 1(3), igy002. https://doi.org/10.1093/geroni/igy002
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Chan, C. V., & Kaufman, D. R. (2011). A framework for characterizing eHealth literacy demands and barriers. Journal of Medical Internet Research, 13(4), e94. https://doi.org/10.2196/jmir.1750
- Chen, K., & Chan, A. H. S. (2011). A review of technology acceptance by older adults. Gerontechnology, 10(1), 1–12. https://doi.org/10.4017/gt.2011.10.01.006.00
- Cho, J., Quinlan, M. M., Park, D., & Noh, G. Y. (2014). Determinants of adoption of smartphone health apps among college students. American Journal of Health Behavior, 38(6), 860–870. https://doi.org/10.5993/AJHB.38.6.8
- Czaja, S. J., Charness, N., Fisk, A. D., Hertzog, C., Nair, S. N., Rogers, W. A., & Sharit, J. (2006). Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE). Psychology and Aging, 21(2), 333–352. https://doi.org/10.1037/0882-7974.21.2.333
- Davis, F. D. (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly, 13(3), 319–340. https://doi.org/10.2307/249008
- Deng, Z., Hong, Z., Ren, C., Zhang, W., & Xiang, F. (2018). What predicts patients’ adoption intention toward mHealth services in China: Empirical study. JMIR mHealth and uHealth, 6(8), e172. https://doi.org/10.2196/mhealth.9316
- Engelsma, T., Jaspers, M. W. M., & Peute, L. W. (2021). Considerate mHealth design for older adults with Alzheimer’s disease and related dementias (ADRD): A scoping review on usability barriers and design suggestions. International Journal of Medical Informatics, 152, 104494. https://doi.org/10.1016/j.ijmedinf.2021.104494
- Eyal, N. (2014). Hooked: How to build habit-forming products. Penguin.
- Fereday, J., & Muir-Cochrane, E. (2006). Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods, 5(1), 80–92. https://doi.org/10.1177/160940690600500107
- Fishbein, M., & Ajzen, I. (1977). Belief, attitude, intention, and behavior: An introduction to theory and research. Addison-Wesley.
- Fisk, A. D., Czaja, S. J., Rogers, W. A., Charness, N., & Sharit, J. (2020). Designing for older adults: Principles and creative human factors approaches. CRC Press.
- Fogg, B. J. (2009). A behavior model for persuasive design [Paper presentation]. Proceedings of the 4th international Conference on Persuasive Technology. Persuasive, Claremont, California, USA. https://doi.org/10.1145/1541948.1541999
- Foong, P. S. (2016). The value of the life course perspective in the design of mobile technologies for older adults. In S. S. Lim (Ed.), Mobile communication and the family (pp. 165–181). Springer. https://doi.org/10.1007/978-94-017-7441-3_10
- Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., Patel, V., & Haines, A. (2013). The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Medicine, 10(1), e1001362. https://doi.org/10.1371/journal.pmed.1001362
- Georgsson, M., & Staggers, N. (2016). An evaluation of patients’ experienced usability of a diabetes mHealth system using a multi-method approach. Journal of Biomedical Informatics, 59, 115–129. https://doi.org/10.1016/j.jbi.2015.11.008
- Guo, X., Han, X., Zhang, X., Dang, Y., & Chen, C. (2015). Investigating m-health acceptance from a protection motivation theory perspective: gender and age differences. Telemedicine Journal and e-Health: The Official Journal of the American Telemedicine Association, 21(8), 661–669. https://doi.org/10.1089/tmj.2014.0166
- iResearch. (2020). 2020 white paper of Chinese artificial intelligence mobile phone (in Chinese). https://www.iresearch.com.cn/Detail/report?id=3704&isfree=0
- Klasnja, P., & Pratt, W. (2012). Healthcare in the pocket: Mapping the space of mobile-phone health interventions. Journal of Biomedical Informatics, 45(1), 184–198. https://doi.org/10.1016/j.jbi.2011.08.017
- Klaver, N. S., van de Klundert, J., van den Broek, R., & Askari, M. (2021). Relationship between perceived risks of using mHealth applications and the intention to use them among older adults in the Netherlands: Cross-sectional study. JMIR mHealth and uHealth, 9(8), e26845. https://doi.org/10.2196/26845
- Kumar, S., Nilsen, W. J., Abernethy, A., Atienza, A., Patrick, K., Pavel, M., Riley, W. T., Shar, A., Spring, B., Spruijt-Metz, D., Hedeker, D., Honavar, V., Kravitz, R., Lefebvre, R. C., Mohr, D. C., Murphy, S. A., Quinn, C., Shusterman, V., & Swendeman, D. (2013). Mobile health technology evaluation: The mHealth evidence workshop. American Journal of Preventive Medicine, 45(2), 228–236. https://doi.org/10.1016/j.amepre.2013.03.017
- Kuruvilla, S., Sadana, R., Montesinos, A. V., Beard, J., Vasdeki, J. F., de Carvalho, I. A., Thomas, R. B., Drisse, M.-N. B., Daelmans, B., & Goodman, T. (2018). A life-course approach to health: synergy with sustainable development goals. Bulletin of the World Health Organization, 96(1), 42. https://doi.org/10.2471/BLT.17.198358
- Leung, L., & Chen, C. (2019). E-health/m-health adoption and lifestyle improvements: Exploring the roles of technology readiness, the expectation-confirmation model, and health-related information activities. Telecommunications Policy, 43(6), 563–575. https://doi.org/10.1016/j.telpol.2019.01.005
- Limayem, M., Hirt, S. G., & Cheung, C. M. (2007). How habit limits the predictive power of intention: The case of information systems continuance. MIS Quarterly, 31(4), 705–737. https://doi.org/10.2307/25148817
- Lv, X., Guo, X., Xu, Y., Yuan, J., & Yu, X. (2012). Explaining the mobile health services acceptance from different age groups: a protection motivation theory perspective. International Journal of Advancements in Computing Technology, 4(3), 1–9. https://doi.org/10.4156/ijact.vol4.issue3.1
- Miao, R., Wu, Q., Wang, Z., Zhang, X., Song, Y., Zhang, H., Sun, Q., & Jiang, Z. (2017). Factors that influence users’ adoption intention of mobile health: A structural equation modeling approach. International Journal of Production Research, 55(19), 5801–5815. https://doi.org/10.1080/00207543.2017.1336681
- Mitzner, T. L., Rogers, W. A., Fisk, A. D., Boot, W. R., Charness, N., Czaja, S. J., & Sharit, J. (2014). Predicting older adults’ perceptions about a computer system designed for seniors. Universal Access in the Information Society, 15, 271–280. https://doi.org/10.1007/s10209-014-0383-y
- Perry, K., Shearer, E., Sylvers, P., Carlile, J., & Felker, B. (2019). mHealth 101: An introductory guide for mobile apps in clinical practice. Journal of Technology in Behavioral Science, 4(2), 162–169. https://doi.org/10.1007/s41347-019-00108-8
- Plaza, I., Martín, L., Martin, S., & Medrano, C. (2011). Mobile applications in an aging society: Status and trends. Journal of Systems and Software, 84(11), 1977–1988. https://doi.org/10.1016/j.jss.2011.05.035
- Ritchie, J., Lewis, J., Nicholls, C. M., & Ormston, R. (2013). Qualitative research practice: A guide for social science students and researchers. Sage.
- Rogers, E. M. (2010). Diffusion of innovations. Simon and Schuster.
- Rogers, R. W. (1975). A protection motivation theory of fear appeals and attitude change. The Journal of Psychology, 91(1), 93–114. https://doi.org/10.1080/00223980.1975.9915803
- Salgado, T., Tavares, J., & Oliveira, T. (2020). Drivers of mobile health acceptance and use from the patient perspective: Survey study and quantitative model development. JMIR mHealth and uHealth, 8(7), e17588. https://doi.org/10.2196/17588
- Schnall, R., Higgins, T., Brown, W., Carballo-Dieguez, A., & Bakken, S. (2015). Trust, perceived risk, perceived ease of use and perceived usefulness as factors related to mHealth technology use. Studies in Health Technology and Informatics, 216, 467–471.
- Shen, C., Wang, M. P., Chu, J. T., Wan, A., Viswanath, K., Chan, S. S. C., & Lam, T. H. (2017). Health app possession among smartphone or tablet owners in Hong Kong: Population-based survey. JMIR mHealth and uHealth, 5(6), e7628. https://doi.org/10.2196/mhealth.7628
- Sun, J., Guo, Y., Wang, X., & Zeng, Q. (2016). mHealth for aging China: opportunities and challenges. Aging and disease, 7(1), 53. https://doi.org/10.14336/AD.2015.1011
- Tajudeen, F. P. B., Maw Pin, N., Saedon, T., & Izzati, N. (2021). Mobile technologies and healthy ageing: A bibliometric analysis on publication trends and knowledge structure of mHealth research for older adults. International Journal of Human–Computer Interaction, 38(2), 1–13. https://doi.org/10.1080/10447318.2021.1926115
- Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. D. (2003). User acceptance of information technology: Toward a unified view. MIS Quarterly, 27(3), 425–478. https://doi.org/10.2307/30036540
- Venkatesh, V., Thong, J. Y., & Xu, X. (2012). Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Quarterly, 36(1), 157–178. https://doi.org/10.2307/41410412
- Wang, K. H., Chen, G., & Chen, H.-G. (2017). A model of technology adoption by older adults. Social Behavior and Personality: An International Journal, 45(4), 563–572. https://doi.org/10.2224/sbp.5778
- WHO. (2011). mHealth: New horizons for health through mobile technologies: Based on the findings of second global survey on eHealth. WHO. https://apps.who.int/iris/handle/10665/44607
- WHO. (2020). Decade of healthy ageing: Baseline report. https://www.who.int/publications/m/item/decade-of-healthy-ageing-baseline-report
- Wildenbos, G. A., Peute, L., & Jaspers, M. (2018). Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). International Journal of Medical Informatics, 114, 66–75. https://doi.org/10.1016/j.ijmedinf.2018.03.012