ABSTRACT
Background
Stroke has transitioned from an untreatable, unpreventable disease to a highly treatable and preventable disease over recent decades, and the number of stroke survivors is expected to increase. The number is also foreseen to grow larger as a result of an aging population. With an escalating number of stroke survivors, research on how to improve life after stroke is needed.
Aims
The primary aim was to determine which area of research related to life after stroke that stroke patients and their informal carers prioritized as being relevant and valuable.
Methods
A cross-sectional study of all patients who had completed the 12 months of follow-up in the EFFECTS trial. In the questionnaire the stroke patients and their informal carers were asked to prioritize areas of research they considered important and valuable with respect to their life after stroke.
Results
Of the 731 patients who were still alive after the 12 months-follow-up, 589 responded. The most prioritized areas of research were Balance and walking difficulties (290 (49%) responders) and Post-stroke fatigue (173 (29%) responders). Women answered the undefined alternative “other” more often than men (43 women (11%) versus 11 men (6%), p = .04). Younger patients prioritized Post-stroke fatigue to a higher extent (88 (45%) versus (22%), p < .001), and elderly prioritized Balance and walking difficulties (214 (54%) versus 76 (40%), p = .002) and Speech difficulties (38 (10%) versus 9 (5%), p = .045).
Conclusions
Life after stroke is perceived differentely with aging. Future research should address strategies to face challenges such as imbalance and walking difficulties and post-stroke-fatigue.
Introduction
Stroke is a growing health concern due to the aging population, and at the same time, more patients are surviving stroke as a result of improved treatment and stroke care, indicating that stroke should be viewed as a chronic disease rather than as a single, neurological incident. Citation1 Those surviving a stroke often suffer from residual functional disabilities, emotional problems, and cognitive deficits, and more insight is needed on how patients experience life after stroke and how to improve long-term care. Citation2 A Scottish study (n = 28) indicated that cognition was one of the most prioritized research areas on life after stroke. Citation3 Involving patients and the public in the planning of research on life after stroke provides a unique perspective with personal knowledge of the disease, and the day-to-day reality experience has proven to give greater relevance and quality to research. Citation3–5 It could also be argued that people affected by research should have a voice in how publicly funded research is undertaken. Research involving the patient is well recognized internationally and has proven to be cost-effective, and is increasingly regarded as essential to the legitimacy, relevance, and quality of the research, enabling the research to better match the needs of service users and caregivers. Citation6–8 The identification of research priorities of survivors of stroke and their relatives would ensure that scarce research resources are directed to areas that matter most to people affected by stroke. Differences in healthcare settings, culture, and resources can influence how patients perceive life after stroke, and how they make decisions related to their health. Therefore, it is important to address the situation of patients with stroke specifically in the context of their particular healthcare environment.
Aims
The primary aim was to determine which areas of research related to life after stroke that Swedish stroke patients and their informal carers consider to be relevant and valuable. The secondary aim was to assess whether priorities differed between subgroups of patients.
Methods
This is a cross-sectional study embedded in the Efficacy of Fluoxetine-a randomized controlled trial in stroke (EFFECTS) trial, an ongoing Swedish randomized clinical trial of 20 mg fluoxetine versus placebo once daily for six months after ischemic stroke or intracerebral hemorrhage. Citation9 The study population was all patients in the trial who had completed the 12-month follow-up as of August 2018. A questionnaire was sent out during the time period between August and November 2018.
The questionnaire was outlined and developed in accordance with earlier research in the area regarding patient involvement and adequate areas of research, as well as “The action plan for stroke in Europe 2018 to 2030” defined by the Stroke Alliance for Europe. Citation2,Citation3 Specialists within internal medicine, neurology, and rehabilitation medicine, all with significant experience of care of stroke patients, were also involved in the development of the questionnaire. To ensure that the questionnaire was relevant to patients suffering from stroke it was tested on patients of both sexes and their informal carers in an outpatient hospital stroke clinic 2 months after stroke. Changes were made accordingly to improve wording and understandability. The final questionnaire consisted of eleven research areas including one free-text alternative, from which patients were asked to prioritize two areas that, from their point of view, were most valuable on which to conduct further research.
Descriptive analyses were made on baseline characteristics and the number of observations, presented as number and percentages. Categorical data in the form of questionnaire answers, sex, and dichotomized age were compared using the Chi-square-test and presented as numbers and percentages. The significance level for all the statistical tests was set to 5% and presented with 95% confidence intervals (CI). Statistical analyses were performed using IBM SPSS Statistics for Mac version 26.
Written informed consent was obtained from all patients. This investigation was approved by the local ethical authorities in Sweden (2013/1265-31/2 and 2018/2012). This manuscript conforms to the STROBE guidelines.
Results
We sent the questionnaire to 731 patients together with a prepaid envelope for the return. Of these, 589 patients completed and returned the questionnaire (81.1%). Five questionnaires were undelivered due to incorrect address. shows the numbers of patients who were potentially eligible for the study and included.
shows the baseline characteristics of the patients in the study. The median time from stroke onset to receiving the questionnaire was 27 months (range 14–48). Of the respondents, 230 (39%) were female. The median age at the stroke onset was 72 years (range 20–92). Stroke severity at inclusion in EFFECTS was quantified by the National Institutes of Health Stroke Scale (NIHSS) with a median score of 3 out of a possible 42, with a range of 0–18. Citation10 MoCA test for cognition, patients responding to the questionnaire had scores just below normal with a median score of 24 out of a possible 30 (range 1–30). Citation11 A few baseline data were missing due to the fact that not all categories of variables were included in the pilot phase of the EFFECTS trial. A few baseline data were unknown. At most, baseline data was missing or unknown for 11.4% of patients included. When comparing the baseline characteristics with patients registered in the Swedish Stroke Register (Riksstroke), which has a 96% coverage of all stroke patients in Sweden, it showed that our population corresponds to the stroke population in Sweden with regards to stroke severity at stroke onset as measured by NIHSS. Citation12 Nevertheless, our study population was younger, healthier, and to a greater extent living at home as compared with the overall stroke population in Sweden.
Table 1. Baseline characteristics
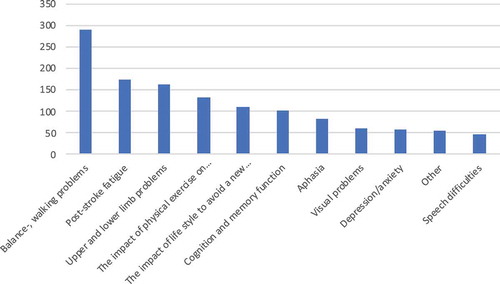
The area of research most chosen was Balance and walking difficulties, chosen by 49% (n = 290 patients) (). The second most prioritized area according to the patients was Post-stroke fatigue, which was chosen by 29% (n = 173 patients). The alternative, Other, where patients were able to write a free text was chosen by 9% (n = 54 patients). Most questionnaires were filled out by the patients themselves (93%), yet many commented that it was answered together with an informal carer. The number of informal carers responding to the questionnaire was 47 and by other personnel once. There was a significant association of the patients’ prioritization of some research areas and their symptoms at baseline such as visual problems, speech difficulties, balance, and walking difficulties.
Figure 2. Number of answers on each research area. Each patient was asked to prioritize two areas. Thirty-one patients chose more than two areas, five patients only chose one area. All priorities are presented in the figure
We performed subgroup analyses based on age and sex. Age was dichotomized to <70 and ≥70 years of age. Differences in questionnaire answers between age groups are presented in . Sixty-eight percent of respondents were ≥70 years of age. There was a significant difference between the age groups, where older patients prioritized Balance and walking difficulties (p = .002) and Speaking difficulties (p = .045) to a higher degree. Younger patients prioritized Post-stroke fatigue (p < .001). Analyses of sex showed no differences in the responses between men and women, except that more women (11% (n = 43) versus 6% men (n = 11)) provided answers in the free text area Other (p = .043).
Table 2. Differences in priorities between younger (<70 years) and elderly (≥70 years) patients with stroke
Discussion
In this study of Swedish patients’ priorities for research related to life after stroke, we found that balance and walking difficulties were the most requested area of research, especially among elderly. Although this area is discussed in the “Action plan for stroke in Europe 2018–2030” as important areas in life after stroke, it is not on the agenda of research for the European action plan. Citation2 Our results support that we should put more effort into investigating and adjusting strategies at discharge to alleviate balance and walking problems since this could prevent patients from falling and causing injury and subsequent long periods of hospitalization. Further, research in primary care setting addressing long-term balance and walking difficulties should be encouraged.
Another important finding was that young stroke patients ranked post-stroke fatigue highest. For these younger stroke survivors, the responsibilities of family life and work, as well as the demands from society differ from those of older stroke survivors. Citation13 Post-stroke fatigue is one of the most disabling symptoms in stroke survivors; it reduces the quality of life, increases mortality, and is a barrier to stroke rehabilitation, and has also been shown to affect patients’ return to working life. Citation14,Citation15 In addition, health professionals still lack a regimen or a coping strategy to equip the patient with at discharge from hospital. Citation16 Efficient management of post-stroke fatigue should be a priority in stroke rehabilitation given the incidence of stroke and the prevalence and detrimental impact of post-stroke fatigue on independent living and overall survival. Citation17,Citation18
An area of research that has been greatly discussed in recent years is depression among stroke patients, but very few patients prioritized depression as an important research area in our study. One important reason for this was probably that depression was an exclusion criterion in the EFFECTS trial, and that half of the patients in the EFFECTS trial was randomized to treatment with fluoxetine for the first six months after stroke. Since EFFECTS is still ongoing, it is not possible to identify which patients that were in the treatment group versus the placebo arm.
Cognition was not highly prioritized in our study. However, in a Scottish study cognition came on top, while balance, gait, and mobility came in the seventh place. Citation3 Although the sample in the Scottish study was small (n = 28) and baseline data regarding, age, sex, onset of stroke, etc., were not presented making it more difficult to make further comparisons.
National guidelines often focus primarily on the acute care and early rehabilitation of stroke patients. Long-term care has received little attention and as a result, varies greatly between countries as well as within countries. In addition, primary care services often recommend that individuals make their own choices regarding health services and initiate contact if problems occur. These factors require a high level of capability on the part of the patient with respect to navigating the healthcare system and often result in unmet needs and further consequences for the individual as well as for society. According to the Riksstroke annual report from 2018, a quarter of Swedish stroke patients’ rehabilitation exercise needs is not sufficiently met, which was also seen in an observational study from 2016. Citation16 This is consistent with the results in our study as we found in the free-text alternative many requesting an increase in rehabilitation exercises, even though these results were not significant. Research into patients’ perspective with respect to life after stroke has been poorly prioritized which we believe is reflected in our results. This is in good agreement with a recent Swedish focus group investigation which also encouraged the implementation of larger studies. They concluded that comprehensive long-term follow-up that is accessible to all patients is essential and that structured follow-up, which is individually tailored, can empower patients. Citation19
The strength of this study is that it was performed on a large group of stroke patients from all over Sweden. External validity was partly confirmed when comparing baseline characteristics of the study group with patients registered in the Riksstroke registry. However, there was a difference in age, gender, and comorbidity. For instance, elderly women with severe disabilities after the incidence of stroke constitutes a significant number of stroke patients in Sweden, and they are not represented in this study.
One limitation of the study was that we used a questionnaire that has never been used before which limits the possibility to make comparisons with other populations. The questionnaire was also defined to 10 areas of research related to life after stroke and when performing analyses by sex, we found that women filled in the free text alternative more often than men, indicating that the women might prioritize areas that were not covered by the questionnaire. Further, the transferability of the findings beyond the Swedish healthcare context could be limited, even though the results do contribute with insights that are applicable to other contexts. Notable is also the uncertainty of the generalizability of results from participants who chose to be in a clinical trial compared to those who did not.
In conclusion, the potential to optimize life after stroke is vast and should be a frontier in stroke research. We found that the research areas most prioritized by the stroke patients differ with age and symptoms at stroke onset, indicating that rehabilitation strategies should be individualized and that this should be done already at discharge from hospital. To achieve major progress in stroke recovery, we need significant commitment to filling vital knowledge gaps and involving patients enables the best use of resources and funding based on greater knowledge of the patients.
Additional information
Funding
References
- Jonsson AC , Delavaran H , Lovkvist H , et al. Secondary prevention and lifestyle indices after stroke in a long-term perspective. Acta Neurol Scand . 2018;138:227–234.
- Norrving B , Barrick J , Davalos A , et al. Action plan for stroke in Europe 2018-2030. Eur Stroke J . 2018;3:309–336. doi:10.1177/2396987318808719.
- Pollock A , St George B , Fenton M , Firkins L. Top 10 research priorities relating to life after stroke–consensus from stroke survivors, caregivers, and health professionals. Int J Stroke . 2014;9:313–320. doi:10.1111/j.1747-4949.2012.00942.x.
- Hirst E , Irving A , Goodacre S. Patient and public involvement in emergency care research. Emergency Med J . 2016;33:665–670. doi:10.1136/emermed-2016-205700.
- Gradinger F , Britten N , Wyatt K , et al. Values associated with public involvement in health and social care research: a narrative review. Health Expectations . 2015;18:661–675. doi:10.1111/hex.12158.
- Brett J , Staniszewska S , Mockford C , et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expectations . 2014;17:637–650. doi:10.1111/j.1369-7625.2012.00795.x.
- Hoddinott P , Pollock A , O’Cathain A , et al. How to incorporate patient and public perspectives into the design and conduct of research. F1000Res . 2018;7:752. doi:10.12688/f1000research.15162.1.
- Dalton J , Chambers D , Harden M , Street A , Parker G , Eastwood A . Service user engagement in health service reconfiguration: a rapid evidence synthesis. J Health Serv Res Policy . 2016;21:195–205. doi:10.1177/1355819615623305.
- Mead G , Hackett ML , Lundstrom E , Murray V , Hankey GJ , Dennis M . The FOCUS, AFFINITY and EFFECTS trials studying the effect(s) of fluoxetine in patients with a recent stroke: a study protocol for three multicentre randomised controlled trials. Trials . 2015;16:369. doi:10.1186/s13063-015-0864-1.
- Brott T , Adams HP , Olinger CP , et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke . 1989;20:864–870. doi:10.1161/01.STR.20.7.864.
- Nasreddine ZS , Phillips NA , Bédirian V , et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc . 2005;53:695–699. doi:10.1111/j.1532-5415.2005.53221.x.
- Riksstroke . Riksstroke. Fem Och Tre År Efter Stroke [Internet] . Umeå: Riksstroke; 2018.
- Blomgren C , Samuelsson H , Blomstrand C , Jern C , Jood K , Claesson L . Long-term performance of instrumental activities of daily living in young and middle-aged stroke survivors-impact of cognitive dysfunction, emotional problems and fatigue. PloS One . 2019;14:e0216822. doi:10.1371/journal.pone.0216822.
- Broussy S , Saillour-Glenisson F , Garcia-Lorenzo B , et al. Sequelae and quality of life in patients living at home 1 year after a stroke managed in stroke units. Front Neurol . 2019;10:907. doi:10.3389/fneur.2019.00907.
- Westerlind E , Persson HC , Eriksson M , Norrving B , Sunnerhagen KS . Return to work after stroke: a Swedish nationwide registry-based study. Acta Neurol Scand . 2020 Jan; 141 (1):56-64.
- Ullberg T , Zia E , Petersson J , Norrving B . Perceived unmet rehabilitation needs 1 year after stroke: an observational study from the Swedish stroke register. Stroke . 2016;47:539–541. doi:10.1161/STROKEAHA.115.011670.
- Wu S , Kutlubaev MA , Chun HY , et al. Interventions for post-stroke fatigue. Cochrane Database Syst Rev . 2015 Jul 2; (7): Cd007030.
- Chen K , Marsh EB . Chronic post-stroke fatigue: it may no longer be about the stroke itself. Clin Neurol Neurosurg . 2018;174:192–197. doi:10.1016/j.clineuro.2018.09.027.
- Kjork EK , Gunnel C , Lundgren-Nilsson A , Sunnerhagen KS . Experiences, needs, and preferences for follow-up after stroke perceived by people with stroke and healthcare professionals: A focus group study. PloS One . 2019;14:e0223338. doi:10.1371/journal.pone.0223338.