Abstract
Study Design: Systematic review and meta-analysis.
Objective: To compare the effectiveness and safety between anterior and posterior approach, and determine the best surgical methods for the treatment of ossification of the posterior longitudinal ligament (OPLL) in the cervical spine.
Methods: We searched the Cochrane Library, PubMed, CNKI and Wanfang Med Data databases from January 2007 to March 2018. Japanese Orthopaedic Association (JOA) scores, cervical lordosis, functional recovery rates, excellent and good outcomes of the surgical approaches, and complication and reoperation rates were analyzed. RevMan 5.3 was utilized for data analysis.
Results: Eleven studies were included in the meta-analysis. By comparing the anterior and posterior approaches for the treatment of OPLL in the cervical spine, statistically significant differences were found in the preoperative initial JOA, the postoperative final JOA scores, functional recovery rates, complication rates, excellent and good outcomes of the surgical approaches and reoperation rates. However, no statistically significant difference in the occurrence of the preoperative and postoperative cervical lordosis was noted.
Conclusion: The anterior approach is superior to the posterior approach in terms of the postoperative final JOA score, functional recovery rate, and clinical outcomes. Although the complication and reoperation rates of the anterior approach are higher than those of the posterior approach. We recommend the anterior approach for the treatment of OPLL when patients with occupying ratio ≥ 60%. In addition, high-quality studies with long-term follow-up and large sample size are also needed.
Introduction
Ossification of the posterior longitudinal ligament (OPLL), in which the spinal cord or nerve root is compressed, is a progressive disease. The prevalence of OPLL in Asia is as high as 3.0%, with estimated incidence rates of 0.1% to 1.7% in North America and Europe.Citation1,Citation2 The aim of surgery is to decompress the spinal cord and to preserve the stability of the spinal column. Surgical treatment should be performed in patients with moderate or severe cervical spondylotic myelopathy (CSM). Surgical decompression is the primary option in some patients who demonstrate hyperintensity on MRI T2-weighted images of the cervical cord.Citation3
The anterior approach usually includes anterior corpectomy with fusion (ACF) and discectomy with fusion (ADF), whereas the typical posterior approach involves laminectomy (LA) and laminoplasty (LP).Citation4 The choice of the surgical approach for OPLL remains controversial.Citation5,Citation6
Generally, patients with focal pathology tend to be treated with the anterior approach, but the selection of the posterior approach is usually based on the surgeon’s preference and the patient’s characteristics. Liu et al. recommended that patients with cervical OPLL involving less than 3–4 vertebrae below the C3 level with thicknesses less than 5–6 mm and spinal stenosis of less than 50% should be treated with anterior surgery. Patients with OPLL involving more than four segments, C1/C2 vertebrae, or cervical vertebrae lower than C6/C7, often resulting in poor surgical field of vision, should be treated with posterior surgery.Citation7 However, the selection criteria for the surgical approach were ambiguous in most studies. Additionally, ACF or ADF can rebuild cervical stability and relieve pressure on the level of the compressed cervical spinal cord. However, complications, primarily dural tearing, cerebrospinal fluid (CSF) leakage, haematoma and C5 palsy, should be considered.Citation8 In this regard, the anterior approach remains a significant surgical challenge, especially for multiple levels and high vertebral canal occupation ratios. Compared with the anterior approach, the posterior approach is an easier surgical technique. Indirect decompression via LA or LP allows the cervical spinal cord to float away from the ventral compression.
Currently, there are no standards or guidelines for the treatment of OPLL. We performed this meta-analysis to evaluate the preoperative initial JOA, postoperative final JOA, functional recovery rate, clinical outcomes, complications, reoperation and cervical lordosis prevalence in the treatment of cervical OPLL. This study aims to determine how to develop selection criteria to identify which condition anterior or posterior approaches should be performed.
Methods
Search strategy
The primary sources of this meta-analysis were the Cochrane Library, PubMed, China National Knowledge Infrastructure (CNKI) and Wanfang Med Data databases. In all databases, “Publication dates (2007–2018)” was used as a filter, and the language was restricted to English and Chinese. The search terms for each of the databases included combinations of the following: (1) ossification of posterior longitudinal ligament OR OPLL; (2) anterior corpectomy with fusion OR anterior discectomy with fusion; (3) laminectomy OR laminoplasty OR posterior decompression; and (1) AND (2) OR (3). The aim was to find retrospective and prospective studies comparing the anterior and posterior approaches for multilevel cervical spondylotic myelopathy with OPLL. The references of the selected studies were reviewed to ensure that the inclusion criteria were met. Full-text copies of all potentially relevant studies were obtained.
Inclusion criteria
The inclusion criteria for the full texts and abstracts of the filtered articles were as follows: 1. adults with OPLL; 2. retrospective and prospective studies; 3. comparison of the anterior and posterior approaches for the treatment of OPLL; and 4. outcome measured in terms of the postoperative final Japanese Orthopaedic Association (JOA), functional recovery rate, clinical outcomes, complications, reoperation rate and the occurrence of postoperative cervical lordosis. All of the Chinese studies were from the ZHONGHUA series, representing the highest academic level of our country.
Data extraction
One author performed the data extraction. All basic characteristics of patients are extracted from the full text of the 11 studies, not by speculating in the abstract. The following information was extracted from each study: (1) study ID, (2) study design, (3) study location, (4) sample size, (5) length of the follow-up, (6) patient’s sex, (7) patient’s mean age, (8) preoperative occupation ratios, (9) preoperative and postoperative JOA scores, (10) functional recovery rate, (11) excellent and good outcomes (the criterion was the improvement rate (IR) and was calculated as follows: IR = (postoperative JOA score − preoperative JOA score/17 − preoperative JOA score) × 100%; the surgical outcome was defined by the IR as follows: excellent (IR ≥ 75%), good (75% > IR ≥ 50%), fair (50% > IR ≥ 25%), and poor (IR < 25%),Citation7 12) fair and poor outcomes, (13) reoperation, (14) complications, (15) postoperative cervical lordosis, and (16) surgical approach.
Dealing with missing data
The corresponding author of each study was contacted to obtain any missing information if necessary. Standard deviations (SDs) of some studies were not reported, and if the statistical data were unavailable, the study was excluded.
Statistical analysis
Data analysis was performed with RevMan 5.3 (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark). Both the 95% confidence interval (CI) and a P value of 0.05 were used as the level of statistical significance. Statistical heterogeneity was calculated using the I2 test, which describes the proportion of the total variation in the data analysis from 0% to 100%. For the pooled effects, the weighted mean difference (WMD) was calculated for continuous variables, and the odds ratio (OR) was calculated for dichotomous variables. Continuous variables are presented as the mean differences and 95% CIs, whereas dichotomous variables are presented as the ORs and 95% CIs. Random-effects or fixed-effects models were used depending on the heterogeneity (I2 > 50%) of the included studies according to the Cochrane instructions (9.5.3 Strategies for addressing heterogeneity). Non-randomized studies are expected to be more heterogeneous than randomized trials, given the extra sources of methodological diversity and bias. The cause of heterogeneity among the results of the studies was the surgical methods (for example, anterior approaches, including ADF and ACF). When we met high heterogeneity, we used subgroup analysis for reduce the heterogeneity. If the heterogeneity could not be reduced, we did not use subgroup analysis. Subgroup analysis was conducted according to the two anterior surgical methods; subgroup A included studies in which the surgical methods were ACF vs LP, subgroup B included studies in which the surgical methods were ADF vs LA, and subgroup C included studies in which the surgical methods were ADF and LP. A random-effect meta-analysis is intended primarily for heterogeneity that cannot be explained. However, heterogeneity can be explained and explored by conducting subgroup analyses. The pooled effect estimate from a fixed-effect meta-analysis is normally interpreted as being the best estimate of the intervention effect. Therefore, we used the fixed-effect model when the analysis outcomes indicated smaller than moderate heterogeneity.
Assessment of the risk of bias for the included studies
Both review authors independently assessed the risk of bias using The Cochrane Collaboration’s Risk of Bias Tool. The assessors were not blinded to the authors or source institutions. The appraisal criteria included the following: random sequence generation (selection bias), allocation sequence concealment (selection bias), blinding of participants (performance bias), blinding of outcome assessors (detection bias), incomplete outcome data (attrition bias), and selective reporting of outcomes (reporting bias). Each of these factors was recorded as yes (“low” risk of bias), no (“high” risk) or unclear, with a brief summary provided in a table format (see the Characteristics of the included studies section below). After this process, each paper was graded as being at low, unclear or high risk of bias. The results of the assessment of the methodological quality of each of the included trials are shown in Supplementary Fig. S1.
Results
Characteristics of the included studies
Our study has followed PRISMA guidelines. We searched 897 English language studies in the PubMed and Cochrane Library databases and 879 Chinese language studies in the CNKI and Wanfang Med Data databases. Of these, 1032 papers were excluded by screening the titles and abstracts because they were duplicates, irrelevant studies, revision surgeries, combined anterior and posterior surgeries, and reviews. A further 556 papers were excluded by screening the titles and abstracts. Ultimately, 82 papers were excluded due to the following reasons: (43 did not contain a JOA score, 25 were case reports, 5 used other surgical methods, 7 contains contained thoracic OPLL, and 2 reported fusion crosses at the cervicothoracic junction). As a result, a total of 12 papers were included in this meta-analysis.Citation3,Citation7,Citation9–18 The literature search procedure is shown in . All of the data were extracted without derivation derived from the percentage. Some extracted data were reorganized and calculated into our study. Basic characteristics of the patients who were extracted from the full texts of the 11 studies are shown in (Chen’s 2009 study contained 2 papersCitation10,Citation11). Chen's two papers reviewed the two surgical methods of OPLL and performed the same analysis of the indexes; therefore, we used Chen's two articles as one comparative study. According to the high prevalence of OPLL in Asia and the study search strategy, all of the selected papers in our study were from Asia. The weighted mean follow-up time of the 11 studies was 4.7 years. In the preoperative occupying ratios of 8 studies, the weighted mean preoperative spinal canal occupation ratios of the anterior and posterior groups were 56.83% and 50.87%, respectively. The proportion of patients in each study to all patients was considered the weighting factor of the above weighted mean. No statistically significant differences were found among the baseline data of the included studies.
Figure 1 Flowchart of the study selection. * Chen’s 2009s study contains 2 papers.Citation10,Citation11
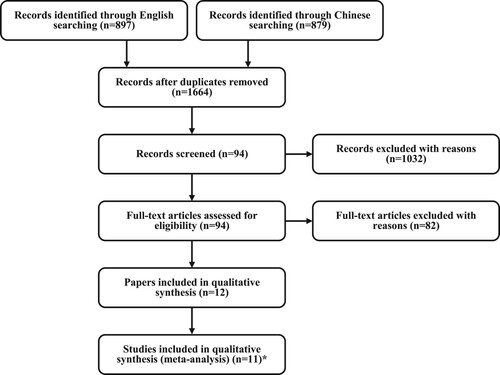
Table 1 Basic characteristics of the included studies.
Risk of bias in the included studies
Overall, 10 studies were retrospective case studies,Citation3,Citation7,Citation9–13,Citation15–18 and 1 was a prospective study,Citation15 and they had methodological flaws that put them at either unclear or high risk of bias for at least one domain. The risks of bias were categorized as a “low”, “unclear” or “high” risk of bias, as shown in Supplementary Fig. S1. The results of the selection bias analysis showed that all studies had a high risk of bias.Citation3,Citation7,Citation9–18 because they were retrospective or prospective studies. With regard to allocation concealment, all of the included studies performed this methodological step in an ambiguous manner.Citation3,Citation7,Citation9–18 All studies failed to report on detection and performance bias.Citation3,Citation7,Citation9–18 In contrast, all studies presented a low and unclear risk of bias for attrition, reporting and other forms of bias.
Outcomes analysis
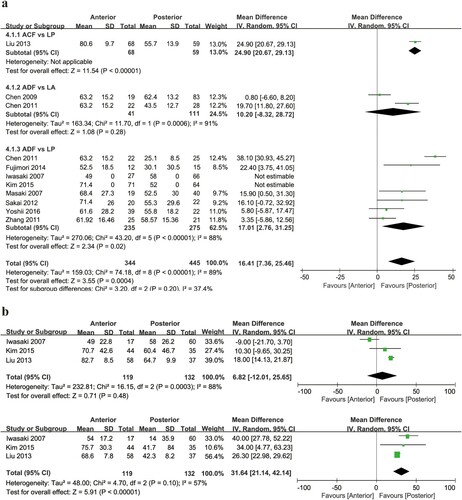
Functional recovery rate
The recovery rates of the JOA score at the final follow-up were analyzed in 10 studies.Citation3,Citation7,Citation9–16,Citation18 The SD was not reported for 2 studies;Citation3,Citation16 thus, these studies were excluded. Ultimately, 8 studies and 539 cases were included in the analysis, including 224 cases using the anterior approach and 315 cases using the posterior approach.Citation7,Citation9–15,Citation18 The mean recovery rates for the anterior and posterior groups were 65.4% and 48.8%, respectively. We performed a subgroup analysis of the data. The anterior group had a significantly higher postoperative functional recovery rate than the posterior group (WMD = 16.41, 95% CI, 2.76–25.46, P < 0.05, a). Significant heterogeneity existed among these studies (I2=89%, P = 0.0004) for the OPLL subgroup. In 3 studies,Citation3,Citation7,Citation16 patients with OPLL were divided into 2 subgroups according to occupying ratio of OPLL: first subgroup (occupying ratio < 60%), other subgroup (occupying ratio ≥ 60%). There was no statistically significant difference in recovery rate among patients with an occupying ratio < 60% (WMD = 6.82, 95% CI, −12.01–25.65, P = 0.48, b upper). However, among patients with occupying ratio ≥ 60%, result of analysis showed statistically significant difference in recovery rate that favored the anterior group (WMD = 31.64, 95% CI, 21.14–42.14, P < 0.05, b lower).
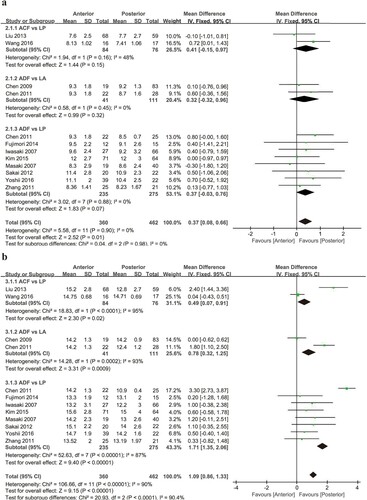
Preoperative and postoperative JOA scores
Preoperative initial JOA and postoperative final JOA scores (final follow-up) were analyzed in all 11 studies.Citation3,Citation7,Citation9–18 All studies and 800 cases were involved, including 338 cases using the anterior approach (ADF, n = 254; ACF, n = 84) and 462 cases using the posterior approach (LA, n = 111; LP, n = 351). Due to the sub-categories of the anterior and posterior approaches, we performed a subgroup analysis of the data. There was significant difference in the preoperative JOA scores between the anterior and posterior groups (WMD = 0.37, 95% CI, 0.08–0.66, P = 0.01, a), and the chi-square test indicated no statistical evidence of heterogeneity (I2=0%, P = 0.90). The anterior group had significantly higher postoperative JOA scores than the posterior group (WMD = 1.09, 95% CI, 0.86–1.33, P < 0.05, b), and moderate heterogeneity existed among these studies (I2 = 90%, P < 0.001).
Preoperative and postoperative cervical lordosis
Preoperative and postoperative cervical lordosis (final follow-up) was analyzed in 6 studies.Citation10–15,Citation17,Citation18 A total of 340 cases were involved, including 128 cases using the anterior approach and 212 cases using the posterior approach. We performed a subgroup analysis of the data. There were no significant differences in the presence of preoperative and postoperative cervical lordosis between the anterior and posterior groups (preoperative WMD = −1.31, 95% CI, −4.28–1.66, P > 0.05; postoperative WMD = 2.22, 95% CI, −2.08–6.52, P > 0.05, Supplementary Fig. S2a), and the chi-square test indicated no statistical evidence of high heterogeneity (preoperative I2 = 84%, P = 0.39; postoperative I2 = 98%, P = 0.31, Supplementary Fig. S2b).
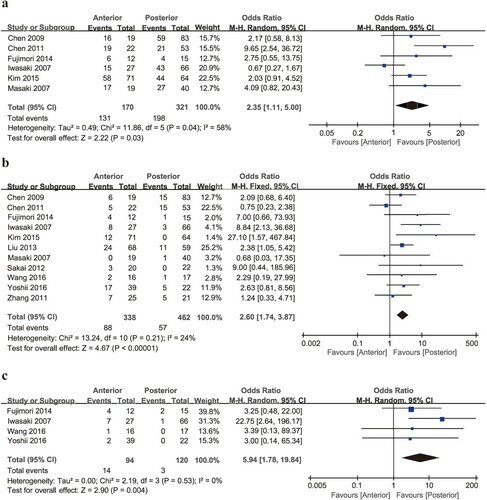
Excellent and good outcomes of the surgical approaches
The purpose of this study was to compare the outcomes of the anterior and posterior approaches. The JOA scoring system was utilized to evaluate the neurological status. For both approaches in 6 studies containing 491 patients, the overall prevalence of excellent and good outcomes was 67.0% (anterior 77.1%, posterior 61.7%).Citation3,Citation9–11,Citation13,Citation15,Citation16 Two studies reported only good and bad outcomes, but we merged the “excellent” and “good” results as “good” and analyzed them together.Citation3,Citation10 The anterior group had a higher incidence of excellent postoperative outcomes than the posterior group (OR 2.35, 95% CI, 1.11–5.00, P < 0.05, a). An analysis of the studies indicated moderate heterogeneity, with an I2 = 58% and P = 0.03. There was a statistically significant difference in excellent and good outcomes among the studies.
Complications
Eleven studies containing 145 patients with overall complications after cervical surgery out of a total of 800 patients were included.Citation3,Citation7,Citation9–18 Complications mainly included dural tearing, CSF leakage, haematoma, C5 palsy and others. shows that complications during the anterior approach occurred in 88 patients, whereas complications during the posterior approach occurred in 57 patients There was a statistically significant difference in two approaches. A total of 15 of 88 patients in the anterior group had both CSF leakage and dural tearing. Only 1 of the 88 patients in the posterior group had CSF leakage, and 1 experienced dural tearing.Citation7,Citation10–12,Citation15 The anterior group had a higher incidence of postoperative complications than the posterior group (OR 2.60, 95% CI, 1.74–3.87, P < 0.05, b). An analysis of the studies indicated low heterogeneity, with an I2 = 24% and P < 0.001. In terms of the surgical methods, patients who underwent the posterior approach had the highest rate of C5 palsy, while those who received the anterior approach had the highest rate of dural tearing.
Table 2 Complications*.
Reoperation
Reoperation was assessed in 4 studies.Citation3,Citation15,Citation17,Citation18 Of the 94 patients who received anterior surgery, 14 patients (14.9%) required reoperation. Of the 120 patients who received posterior surgery, only 3 (2.3%) required reoperation. The reoperation rate was significantly higher in the anterior surgery group than in the posterior surgery group. The anterior group had a higher postoperative incidence of reoperation than the posterior group (OR 5.94, 95% CI, 1.78–19.84, P < 0.05, c). No heterogeneity of incidence observed existed among these studies (I2 = 0%, P = 0.004).
Discussion
The ideal surgical treatment option for cervical OPLL remains controversial and presents a significant surgical challenge. In our studies, the weighted means of the preoperative occupation ratios for the anterior and posterior groups were 56.8% and 50.9%, respectively. The anterior approach produces a better neurological outcome for patients with cervical OPLL, especially those with an occupying ratio greater than 60%. However, for patients with an occupying ratio less than 60%, the postoperative recovery rate was similar for both groups. The anterior approach was a method that could remove the direct compression of the cervical spinal cord. The posterior approach in the treatment of multilevel cervical OPLL was indicated when there was lower 60% mean spinal canal occupation ratio.Citation15 No significant difference was observed for the preoperative occupation ratios and preoperative cervical lordosis occurrence. These findings indicate that the preoperative conditions of these two groups were similar. The anterior group had higher postoperative JOA scores and recovery rates; however, the heterogeneity in the postoperative JOA scores and recovery rates was high among the individual studies according to the I-squared value in the forest graph. Differences in the indexes containing numbers of patients, sex ratios and follow-up times may explain the heterogeneity among the studies. In addition, the surgical techniques and perioperative care were not clearly defined, which may have increased the statistical significance of the differences in the postoperative JOA scores and recovery rates. This finding indicates that the direct decompression of the anterior approach is associated with better functional recovery for the different treatments of cervical OPLL with a high mean occupation ratio.
The surgical approaches for OPLL have been studied for a long time. On the one hand, many new techniques and methods have been applied to remove OPLL. On the other hand, the risks of complications have been recognized, and measures are now taken to prevent these complications from occurring. In our study, the anterior group had a higher postoperative incidence of complications than the posterior group. Dural tearing (8.0%, P < 0.05) and CSF leakage (6.5%, P < 0.05) were more often reported in the anterior group, while axial neck pain (3.3%, P < 0.05) were reported more frequently in the posterior group. There was no statistically significant difference in C5 palsy (5.6%, P > 0.05) and haematoma (1.3%, P > 0.05). shows that above results.
The reoperation rate of the anterior group (14.9%) was nearly six times that of the posterior group (2.3%) in 4 studies (). Similarly, Liu et al. also found that the reoperation rate was higher in the anterior groups than in the posterior groups.Citation7
Based on our findings, we summarized how to choose surgical approaches. 5 outcomes indexes suggest anterior surgery. shows that above results. The limitations of our study are as follows: First, the included publications are from Asia; thus, a potential region bias may exist in this meta-analysis. Second, clinical heterogeneity may be caused by the different counts of involved segments of OPLL and the surgical skills of the operator. Third, there were variable lengths in the follow-up times among some of the studies, which complicated the evaluations and comparisons of the surgical results. Finally, both retrospective and prospective studies were included in this meta-analysis, and their selection bias is unclear. Thus, further high-quality, randomized controlled studies with more patients should be performed. Multi-centre, larger-scale and higher-quality studies are needed to provide more reliable evidence for future evaluations.
Table 3 Preference choice of the 2 surgical approaches for OPLL.
Conclusion
Both the anterior and posterior approaches are common surgical methods for the treatment of OPLL. Although the results of this meta-analysis show that the complication and reoperation rates of anterior surgery are higher than those of posterior surgery, the anterior approach results in better postoperative final JOA scores, functional recovery rates, and clinical outcomes. We recommend the anterior approach for the treatment of OPLL when patients with occupying ratio ≥ 60%. In addition, high-quality studies with long-term follow-up and large sample size are also needed. Future prospective studies are warranted to better elucidate the benefits of anterior versus posterior approach only in patients with OPLL.
Disclaimer statements
Contributions JZ performed the literature search, article selection, wrote the methods and results, created all figures and tables, and edited and revised the final manuscript for submission. DQ and XW assisted in article selection and wrote the discussion section of the manuscript. QA and ZZ assisted in article selection, wrote the introduction section of the manuscript, and edited all figures and tables. JF and QL conceived the manuscript idea and provided clinical expertise about spinal cord injuries in various sections of the manuscript.
Funding None.
Conflicts of interest Authors have no conflicts of interest to declare.
Supplemental Material
Download Zip (793.9 KB)Acknowledgements
We acknowledge the support received from the Shanxi Provincial People’s Hospital and Shanxi Medical University. In particularly, Useful suggestions and supports given by Dr Jiefu Song, Dr Dean Qin and Dr Xiaojian Wang of Shanxi Provincial People’s Hospital are also acknowledged.
References
- Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine (Phila Pa 1976). 2012;37:E309–14. doi: https://doi.org/10.1097/BRS.0b013e318241ad33
- An HS, Al-Shihabi L, Kurd M. Surgical treatment for ossification of the posterior longitudinal ligament in the cervical spine. J Am Acad Orthop Surg. 2014;22:420–9. doi: https://doi.org/10.5435/JAAOS-22-07-420
- Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Advantages of anterior decompression and fusion over laminoplasty. Spine (Phila Pa 1976). 2007;32:654–60. doi: https://doi.org/10.1097/01.brs.0000257566.91177.cb
- Cunningham MR, Hershman S, Bendo J. Systematic review of cohort studies comparing surgical treatments for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2010;35:537–43. doi: https://doi.org/10.1097/BRS.0b013e3181b204cc
- Ogawa Y, Toyama Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, et al. Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine. 2004;1:168–74. doi: https://doi.org/10.3171/spi.2004.1.2.0168
- Yalamanchili PK, Vives MJ, Chaudhary SB. Cervical spondylotic myelopathy: factors in choosing the surgical approach. Adv Orthop. 2012;2012:783762. doi: https://doi.org/10.1155/2012/783762
- Liu H, Li Y, Chen Y, Wu W, Zou D. Cervical curvature, spinal cord MRIT2 signal, and occupying ratio impact surgical approach selection in patients with ossification of the posterior longitudinal ligament. Eur Spine J. 2013;22:1480–8. doi: https://doi.org/10.1007/s00586-013-2707-7
- Mizuno J, Nakagawa H, Matsuo N, Song J. Dural ossification associated with cervical ossification of the posterior longitudinal ligament: frequency of dural ossification and comparison of neuroimaging modalities in ability to identify the disease. J Neurosurg Spine. 2005;2:425–30. doi: https://doi.org/10.3171/spi.2005.2.4.0425
- Masaki Y, Yamazaki M, Okawa A, Aramomi M, Hashimoto M, Koda M, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech. 2007;20:7–13. doi: https://doi.org/10.1097/01.bsd.0000211260.28497.35
- Chen Y, Chen D, Wang X, Lu X, Guo Y, He Z, et al. Anterior corpectomy and fusion for severe ossification of posterior longitudinal ligament in the cervical spine. Int Orthop. 2009;33:477–82. doi: https://doi.org/10.1007/s00264-008-0542-y
- Chen Y, Guo Y, Chen D, Wang X, Lu X, Yuan W. Long-term outcome of laminectomy and instrumented fusion for cervical ossification of the posterior longitudinal ligament. Int Orthop. 2009;33:1075–80. doi: https://doi.org/10.1007/s00264-008-0609-9
- Zhang B, Dai M, Tang Y, Fan H, Yao H, Liu H. Surgical treatment of ossification of the posterior longitudinal ligament of cervical spine. Orthop J Chin. 2011;19:1601–04.
- Chen Y, Guo Y, Lu X, Chen D, Song D, Shi J, et al. Surgical strategy for multilevel severe ossification of posterior longitudinal ligament in the cervical spine. J Spinal Disord Tech. 2011;24:24–30. doi: https://doi.org/10.1097/BSD.0b013e3181c7e91e
- Sakai K, Okawa A, Takahashi M, Arai Y, Kawabata S, Enomoto M, et al. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine (Phila Pa 1976). 2012;37:367–76. doi: https://doi.org/10.1097/BRS.0b013e31821f4a51
- Fujimori T, Iwasaki M, Okuda S, Takenaka S, Kashii M, Kaito T, et al. Long-term results of cervical myelopathy due to ossification of the posterior longitudinal ligament with an occupying ratio of 60% or more. Spine (Phila Pa 1976). 2014;39:58–67. doi: https://doi.org/10.1097/BRS.0000000000000054
- Kim B, Yoon DH, Shin HC, Kim KN, Yi S, Shin DA, et al. Surgical outcome and prognostic factors of anterior decompression and fusion for cervical compressive myelopathy due to ossification of the posterior longitudinal ligament. Spine J. 2015;15:875–84. doi: https://doi.org/10.1016/j.spinee.2015.01.028
- Wang W, Hai Y, Guan L, Liu Y, Chen X, Zhu W. Anterior or posterior approaches for cervical ossification of posterior longitudinal ligament: a mid-term follow-up. Chin J Spine Spinal Cord. 2016;26:577–84.
- Yoshii T, Sakai K, Hirai T, Yamada T, Inose H, Kato T, et al. Anterior decompression with fusion vs. posterior decompression with fusion for massive cervical ossification of the posterior longitudinal ligament with a ≥50% canal occupying ratio: a multi-center retrospective study. Spine J. 2016;16:1351–7. doi: https://doi.org/10.1016/j.spinee.2016.07.532