Abstract
The Ebola virus disease (EVD) epidemic entered Liberia through Lofa County in February 2014 and spread to two health districts where the nongovernmental organization Global Communities had been implementing community-led total sanitation (CLTS) since 2012. By December 2014 the county had 928 Ebola cases (422 of them confirmed) and 648 deaths. Before the epidemic, CLTS was triggered in 155 communities, and 98 communities were certified as Open Defecation Free (ODF). Using mixed quantitative and qualitative methods, we determined that no cases of EVD were found in ODF communities and in only one CLTS community that had not reached ODF status. No differences were found between EVD and non-EVD communities in tribe, religion, ethnic group, or major sources of Ebola information. Radio was the most common source of information for all communities, but health workers were the most trusted information sources. CLTS ODF communities attributed their avoidance of EVD to Water, Sanitation, and Hygiene behaviors, especially hand washing with soap and disposal of feces that they learned from CLTS prior to the epidemic. Communities that got EVD blamed their strong initial resistance to Ebola response messages on their distrust that Ebola was real and their reliance on friends and family for advice. A strong inverse correlation between EVD and CLTS with or without ODF emerged from the regression analysis (R = –.6).
Lofa County is the second largest county and fourth most populated political subdivision in Liberia (Government of Liberia, Citation2014). Global Communities, a U.S.-based humanitarian nongovernmental organization (NGO), introduced Community-Led Total Sanitation (CLTS) as part of the USAID-funded Improving Water, Sanitation, and Hygiene (IWASH) project in two of Lofa County’s six health districts in 2012. By February 2014, 98 of 115 CLTS communities had been certified as Open Defecation Free (ODF), meaning they had received independent Government of Liberia verification that they met national CLTS criteria.
Ebola virus disease (EVD) entered Liberia from Guinea through neighboring Foya District in February 2014 and quickly spread to other districts in the county. The epidemic spread quickly, and there were new cases until mid-2015. The last confirmed new EVD case in Lofa County was in November 2014, months before Liberia was declared Ebola free. By that time there had been 928 reported cases (422 confirmed), with 648 deaths in Lofa County (key informant interview [KII], Lofa County Health Team, personal communication, February 2015).
Purpose of the Study
Because the exact reasons for the decline in some areas were not clear, the World Health Organization (WHO) called for studies of success stories such as that of Lofa County to understand why some areas stopped or dramatically reduced EVD transmission whereas others, even in the same vicinity and with similar population profiles, remained areas of intense transmission:
Did the striking and robust declines in Lofa County, Liberia … occur because devastated populations learned first-hand which behaviors carried a high risk and changed them or could the declines be attributed to simultaneous and seamless implementation of the full package of control measures, as happened in Lofa County? (WHO, Citation2015)
Even before WHO called for success story studies about halting the epidemic, IWASH/CLTS communities and the Lofa County Health Team had reported that CLTS ODF communities never had any cases of EVDFootnote1 even when similar communities nearby had cases. At the height of the epidemic, community-related factors in EVD prevention and epidemic response received little attention (D’Harcourt, Citation2014). USAID and Global Communities supported an independent study to (a) validate claims that there were no EVD cases in CLTS ODF communities; (b) determine whether CLTS-specific interventions were a likely explanation for differences between EVD and non-EVD communities; (c) control for other plausible explanations (other than CLTS) for differences between outcomes in similar communities; and (d) where possible, identify which community-based EVD-specific activities were most effective in disseminating EVD information and promoting disease prevention and effective response behaviors.
Literature reviews found no evidence that EVD transmission occurs through either contaminated water or fecal environmental contamination, which are the usual focus intervention areas for Water, Sanitation and Hygiene (WASH) programs, including CLTS. The available EVD research largely focused on inpatient clinical treatment and not on community or public health factors. Nevertheless, reflecting on lessons learned as of early 2015, WHO (Citation2015) acknowledged, “Community engagement is the one factor that underlies the success of all other control measures. It is the linchpin for successful control.”
Successful CLTS depends on complete community engagement. CLTS ODF communities in the study population were already experienced in partnering with CLTS implementers (including the government) to achieve common objectives (ODF status) well before the epidemic began. If existing community resilience factors contributed to some communities’ capacity to respond to health emergencies and other crises, those factors had not yet been investigated.
Study Sample and Methods
The study population was selected from a total of 435 communities in the two project districts (an estimated 21,587 households). CLTS was started in 115 communities with 6,865 households and an estimated population of 34,235. By February 2014, at the start of the epidemic, 98 communities had already been validated as ODF according to Government of Liberia CLTS criteria (Government of Liberia, Citation2012).
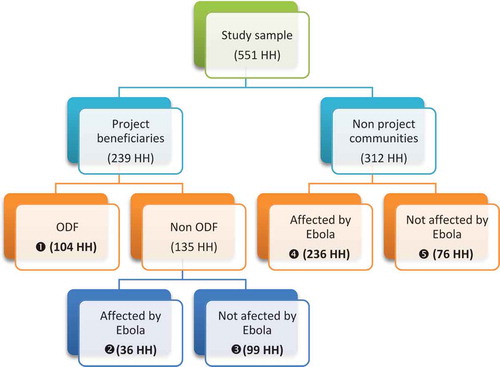
Mixed quantitative and qualitative methods were used, including (a) a review of available data and key documents and (b) a quantitative survey of 551 households conducted in CLTS and non-CLTS, as well as EVD and non-EVD, communities. CLTS communities were further separated into those that had achieved ODF status prior to the epidemic and those that had not. Qualitative methods included focus group discussions (FGDs) in CLTS and non-CLTS communities and KIIs with project staff, government officials, and community leaders.
Sampling Methodology
Respondents for the household survey were selected using purposive, proportionate, and stratified random sampling techniques. Both districts were equally represented in the study. CLTS communities were matched with non-CLTS communities according to geographical location and proximity to each other, population size, and tribe. From among the CLTS communities, those that had been verified as ODF were identified. EVD communities were identified from non-CLTS communities. Extremely small communities or communities located far from CLTS communities were excluded (see ).
William Cochran’s formula for cross-sectional surveys (Cochran, Citation1963) required a minimum sample size of 534 households. This was based on a 95% confidence interval, a tolerance of a 5% margin of error, an assumption that 50% of the households had been exposed to EVD, and an assumption that 20% of household questionnaires would be invalid for some reason.Footnote2 To ensure that a sufficient number of ODF communities was included, we added additional ODF communities, for a total sample of 551 households.
The level of intervention for CLTS was the community rather than the individual or household, so population-level matching was done. Data were collected at the household level but analyzed at the community level. Systematic random sampling identified individual households within each community.
Primary data were collected using a questionnaire administered to heads of households in the local language by a locally hired experienced enumerator. Household demographic characteristics and standard WASH survey indicators, such as knowledge and behaviors related to water, sanitation, and hygiene, were collected. Ebola-specific questions related to where respondents obtained information about Ebola and actions to take, whom they most trusted to provide this information, knowledge of EVD signs and symptoms, and how EVD is transmitted and can be prevented were included in the survey. Secondary data sources used in the study included project reports and databases, county health records, and a list of communities in both districts that was provided by the Government of Liberia Lofa County Health Team.
Standard survey data quality control and internal audit measures were used. Enumerators were not told which communities were ODF or EVD communities. Verbal informed consent was obtained from the respondents, and data security measures for confidentiality were implemented. Data were entered and cleaned using Predictive Analysis Statistical Software™. Simple frequencies and cross-tabs were run to detect inconsistencies. Any errors identified were corrected by comparing the data in the questionnaires with those in the Predictive Analysis Statistical Software™ data set.
Data were then analyzed using both univariate descriptive and inferential statistics. (a) Univariate descriptive analysis: Frequencies, proportions, percentages, and means of variables were computed. (b) Bivariate analysis: Pearson’s chi-square test was conducted to test the association between the dependent variable (the presence of an Ebola case in the community) and possible explanatory variables that were identified during the literature review. (c) Multivariate analysis: Logistic regression was performed to identify predictors of Ebola. Only variables that were found to be significantly associated with Ebola during the bivariate analysis stage were included in the regression model.Footnote3
Qualitative Methods
Ebola research, the CLTS and WASH literature, emergency response formative study reports, key project and government documents, and databases were reviewed. KIIs were held with government officials, project staff, and both formal and traditional community leaders. Male and female FGDs, using tools with questions based on the study research questions, were conducted in EVD and non-EVD communities in both health districts. FGDs within communities were gender disaggregated and consisted of 5–10 members per group. Qualitative findings were analyzed to identify common themes across groups. Findings were triangulated with other sources, including the household survey.
Findings
Of the 43 communities selected for the survey, 18 were beneficiaries of the IWASH CLTS project and 25 were not. Ten different clans were represented in the survey. One third of the households came from the Tahamba clan. The majority of survey respondents were from the Lorma and GbandiFootnote4 tribes, with MandingoFootnote5 and KissiFootnote6 also represented. There were 273 females and 278 males with a mean age of 40 years (Mdn = 38, SD = 14.78). Most respondents (80%) were married (10% widowed, 7% single, 3% separated/divorced). Christians constituted 63% of the respondents and Muslims 32%. The average household size was nine members (Mdn = 8, SD = 4.98). Half of the respondents had no formal education, and a total of 67% had not completed the lowest level of formal education. The main source of income was farming (86%; see ).
Table 1. Sociodemographic characteristics of study respondents
During the IWASH project and prior to the EVD epidemic, travel between Liberia and the other EVD countries was common. The borders between countries were open at the time; borders were not closed until after the outbreak in 2014 and after the IWASH CLTS activities had ended. Travel between communities within project districts and between project districts and other parts of Liberia, including the capital city of Monrovia, was also common. The study found that some EVD cases in the IWASH catchment population had originated in Monrovia.
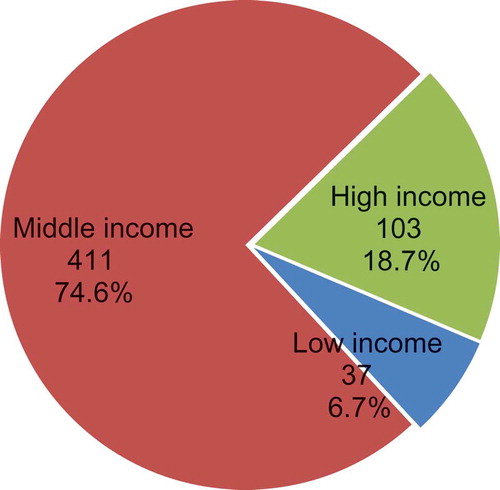
Data on household income were not available. The study included questions about the type of roof and floor in the house as proxies for income. This was similar to the process used in the 2013 Liberia Demographic and Health Survey (Liberia Institute of Statistics and Geo-Information Services, Ministry of Health and Social Welfare, National AIDS Control Program, & ICF International, Citation2014). Higher income groups in communities in the study corresponded to the middle quintile of the Liberian population surveyed in the Liberia Demographic and Health Survey (Liberia Institute of Statistics and Geo-Information Services, Ministry of Health and Social Welfare, National AIDS Control Program, & ICF International, Citation2014), middle income corresponded to the second lowest quintile, and lower income corresponded to the lowest income quintile (see ). The majority of households (75%) were in the middle income or next to lowest quintile of income.
Knowledge About Ebola Transmission
Most respondents from households in communities without EVD believed that hand-washing practices (70%) and avoiding bodily contact (62%) were the key factors that prevented them from acquiring Ebola. Around one quarter (27%) believed that they were protected by avoiding visits by infected persons. In communities without EVD, irrespective of CLTS status, more households consistently reported that they felt that protection was due to hand washing, identifying the sick and avoiding contact with them, and having no cases in the community.
Respondents said they would call the Ebola Hotline (96%) if they suspected someone had Ebola and (97%) supported the statement that early treatment for Ebola was beneficial as it increases chances of survival (84%) and reduces risk of spreading the disease (71%). Early medical intervention for Ebola and avoiding contacts with suspected cases were also mentioned significantly more often by communities with EVD cases, but reporting a household member if he or she had Ebola was higher in communities without Ebola. Regardless of community EVD status, the majority (83%) reported they had changed their behaviors, specifically burial practices, washing hands with soap/disinfectant, avoiding bodily contact, and restricted movement, since the epidemic had begun. Decreased bodily contact with suspected cases was reported by a higher percentage of households in EVD communities.
CLTS ODF and Ebola
Involvement in the IWASH CLTS project was associated with a reduction in the odds of a community being affected with Ebola (odds ratio = 0.06, 95% confidence interval [0.04, 0.09], p < .001), supporting a negative association between CLTS and Ebola. To explore the relationship between EVD and the variables that had shown a significant association with community EVD status, we performed regression analysis to determine the direction and strength of these associations. The dependent variable in the model was the presence of a case of Ebola in the community according to the country database. Separate models were run for sociodemographic and CLTS-related activities. Sociodemographic factors that might have influenced the exposure of communities to Ebola—including locality/district, tribe, clan, religion, level of education, main source of income, overall income, household size, and the presence of WASH NGOs in the community before the epidemic—were included in the model. Demographic variables alone could explain only 78% and 86% of the variance in CLTS and non-CLTS households, respectively. Only locality, tribe, and income were statistically significant and only in non-CLTS communities.
By the time of the survey, intensive Ebola response activities, including border closures, had been in place for several months. Prevention knowledge and behaviors were relatively high in all of Lofa County. Differences in responses between EVD and non-EVD communities related to EVD knowledge were not significant. Ebola response activities implemented by NGOs started in mid-2014 and continued into 2015 (after IWASH CLTS activities had already ended). In KII, Lofa County Health Team officials said that communities that had participated in IWASH CLTS activities were more responsive to radio and government communications about identifying EVD and had changed their behaviors earlier than other communities. Eventually all communities responded to EVD communications and government EVD policies. At the time of the study, hygiene and sanitation measures (including burial practices) had improved significantly in all communities and the borders between the three countries had reopened. Survey data and community FGDs confirmed that both CLTS/ODF and EVD communities reported significant changes in WASH behaviors, specifically hand washing with soap and/or chlorine. Differences were found related to when these behaviors changed. CLTS/ODF FGDs confirmed that they were already practicing hand washing with soap at key times before the epidemic started. CLTS training includes person-to-person instruction by CLTS natural leaders (NLs) in several hygiene behaviors, including using soap for hand washing and constructing and using hand-washing stations and latrines using local materials. CLTS communities easily adapted to the addition of chlorine for hand washing after the EVD outbreak started.
General Knowledge About Ebola
WHO (Citation2015) found that a “lethal, tenacious and unforgiving virus plus fear and misunderstanding that fuelled high-risk behaviors” were the two factors that fueled the Ebola epidemic and called for more research into successful ways in which fear and misunderstandings were overcome. Survey participants were asked questions about general Ebola signs and symptoms, how the disease was transmitted, and how it could be prevented. Most respondents (98%) said that they would be interested in learning more about Ebola, especially prevention (84%).
A third (33%) of the study respondents said that they knew how Ebola entered Liberia, and most (97%) knew that it was through an infected person from a neighboring country. Touching an infected person, human waste, “playing with dead bodies,”Footnote7 and contact with bodily fluids were the most cited modes of Ebola transmission (68%, 62%, 54%, and 41%, respectively).
The majority (96%) knew that Ebola can be prevented by avoiding bodily contact with an infected person (92%) and washing hands (81%). Agreement with the statement that Ebola was preventable was high but higher in CLTS communities (98% of CLTS communities vs. 94% for non-CLTS communities). Nausea and vomiting, diarrhea, red eyes, and fever were the most frequent signs and symptoms cited.
Sources of Ebola Information
Questions about initial and most trusted sources of Ebola information were included in both the survey and community FGDs. The majority of respondents, regardless of CLTS or EVD status, named radio as their initial source of EVD information, followed by health workers, NGOs, and family and friends. CLTS communities had more access to radios for information than EVD-affected communities. EVD community FGDs mentioned family and friends, including those living overseas, as major sources of initial information about the disease and what to do. But when asked which sources of sources they trusted for information and advice, participants listed health workers significantly more often than other sources, followed by radio and NGOs (see ).
Fig. 3. Most trusted sources of Ebola information by number of households. ODF = Open Defecation Free; CLTS = community-led total sanitation; EHT = Environmental Health Technician; NGO = nongovernmental organization.
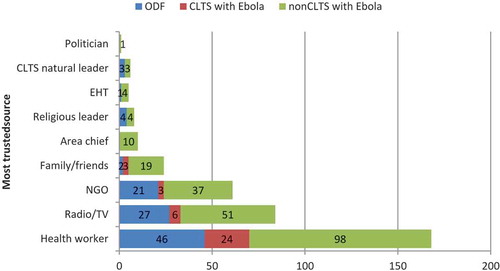
Willingness to follow advice that they heard early in the epidemic was much higher in CLTS communities, who said their increased adherence to hand washing was because “they were already doing it [meaning hand washing]” was very important. They also mentioned that they listened to the advice of the CLTS NL, whom they had come to trust when they took the actions as a community to become ODF.
EVD communities confirmed their initial strong resistance to following instructions from the radio (one district ambulance was attacked). They said this was due to their “denial” or “ignorance” and they “didn’t believe Ebola was real.” They said they “took advice from family and friends until it was too late” and the epidemic got out of control.
Access to trusted sources (health workers) varied in the study districts. Lofa County had a dearth of health workers, even before the EVD outbreak. Shortages were exacerbated by health worker deaths from Ebola and health facility closures. It is estimated that 83 health workers died during the epidemic (Evans, Goldstein, & Popova, Citation2015). Many health workers in Lofa do not come from the area, do not speak local languages, and were not the initial source of information for many survey respondents. Access to radios was found to be limited before the epidemic. The 2013 Liberia Demographic and Health Survey found that only 48% of men and 20% of women in Lofa County listened to the radio at least once a week (Liberia Institute of Statistics and Geo-Information Services, Ministry of Health and Social Welfare, National AIDS Control Program, & ICF International, Citation2014). Study survey data found that 45% of households said they had access to a radio in their community, but 82% of those said they had received their radios in 2014 (after the epidemic started).
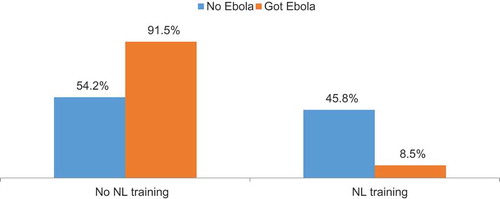
More than a quarter (28%) of the households had received training from a CLTS NL (56% vs. 7% for CLTS and non-CLTS communities). By definition, training from an NL was connected only to IWASH CLTS. CLTS methodology requires NLs to be selected based on their behavior during initial community CLTS triggeringFootnote8 events. Their behavior identifies whether they are already trusted members of the community. Most of those who had received training from an NL said that trainings covered overall hygiene and (later) Ebola topics, including hand washing with soap at critical times, constructing hand-washing stations and latrines with locally available materials, safe disposal of human and animal feces, covering water containers, and using clotheslines and dish racks.
Radio messages were most frequently broadcast in Liberian English (52%), but 77% said they would have preferred the messages in a different language.Footnote9 Most households (63%) reported having a WASH NGO in the community before the Ebola outbreak but not specifically IWASH or CLTS. The presence of NGOs implementing WASH activities was reported more often in CLTS/ODF communities than others (73% vs. 56%, respectively).
FGD respondents in ODF communities confirmed survey findings that they were already practicing protective hygiene practices before EVD arrived. They believed that this was the reason they were not infected. They also said that they increased their hygiene behaviors after they heard about EVD. They were also accustomed to their NL, whom they already trusted, bringing them accurate new information about EVD.
CLTS ODF and the Incidence of Ebola
Quantitative analysis of the household survey found that out of 551 households sampled, 272 (49%) were in communities that had at least one case of EVD. Of the 272 households that were in EVD communities, only 36 (13%) were located in a CLTS community but dropped out and did not reach ODF status. The remaining 236 households (87%) that reported EVD were in communities that had not participated in the CLTS project.
Data confirmed that there were no cases of EVD in communities that reached ODF status. In addition, communities that had been triggered for CLTS were 17 times less likely to get Ebola than communities that were not triggered for CLTS even if ODF status was not attained (see ).
Regression analysis found a strong inverse correlation (R = –.6) between Ebola and CLTS. With an overall predication percentage of 82.4%, the binary logistic regression model was strong and showed that the independent variables together explained a very large proportion of the variance in the incidence of Ebola. In particular, when we held all other factors constant, households with higher income,Footnote10 those without hygiene training from an NL,Footnote11 those without a community radio, and those with low levels of knowledge of the signs and symptoms of Ebola were more vulnerable to Ebola. It is noteworthy that these predictors are necessary for Ebola transmission but not sufficient causes in our understanding of causality.
Qualitative investigation of the one EVD community that was triggered for CLTS but did not reach ODF status found that internal conflict had destroyed the community cohesion that would have enabled the community to successfully progress to ODF status (personal communication, KII with Lofa County CLTS staff; Kar & Chambers, Citation2008).
Differences in common water and sanitation-related infectious diseases between CLTS and non-CLTS communities were reported, but the overall prevalence of the diseases in all communities was low. The evidence base to confirm the effectiveness of specific community WASH behaviors directly on decreased prevalence of some common diseases remains to be established.
The Specific Influence of CLTS on EVD Cases
Statistically significant differences in health status were also found between communities that reported training by an NL. By definition, NL training is a result of CLTS, and households that had not had NL training either were not in CLTS communities, did not participate, or might have been in a small number. More than a quarter (28%) of households surveyed overall had received training from a CLTS NL (56% vs. 7% for CLTS and non-CLTS communities, respectively). The study did not investigate specific NL behaviors (see ).
Fig. 4. Ebola virus disease results by ODF CLTS status: 100% of sampled ODF households remain Ebola free, 73% of households in non-ODF project communities remain Ebola free, and only 24% of nonbeneficiary households remain Ebola free. CLTS = community-led total sanitation.
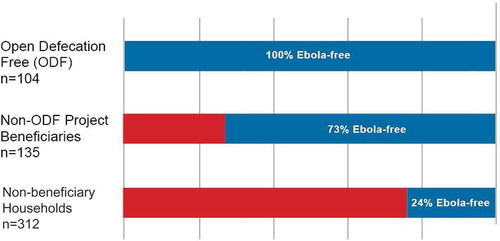
Fig. 5. Ebola virus disease status by community-led total sanitation NL training. NL = natural leader.
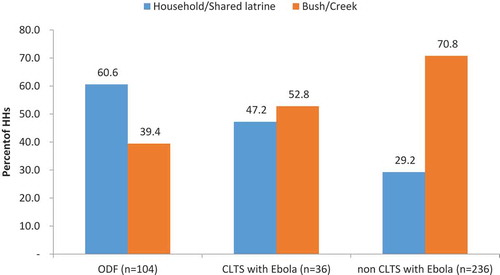
In spite of there being no known connection between latrine use and EVD, a correlation was found between improved latrine and feces disposal practices, a major focus of CLTS, and the absence of EVD in a community. Some studies have shown the presence of the Ebola virus in urine and feces (Centers for Disease Control and Prevention, Citation2015). This highlights the possibility that proper disposal of fecal matter and urine as promoted in CLTS may reduce Ebola transmission (see ).
Discussion
Study findings support a correlation between successful implementation of CLTS (through ODF verification) and significantly reduced risk of EVD, but whether CLTS was the only difference between communities requires additional investigation. Training by an NL (by definition an intervention of CLTS) was also significantly correlated with decreased risk of EVD. Findings from qualitative methods supported survey findings that positive behaviors in hand washing, latrine use, water treatment, and safe disposal of feces that started prior to the EVD outbreak were significantly higher in CLTS/ODF communities than in non-CLTS communities and may have provided protection against EVD transmission in those communities. Additional research will be needed to understand whether the CLTS-specific interventions were the cause of the differences.
ODF status validation, conducted by trained government officials, included direct observation that physical structures (such as hand-washing stations and latrines) were in place and provided objective verification of community, project, and Lofa County Health Team reports. These were all indications that triangulated communities’ claims and verified that they had taken the actions they had committed to take to improve their environmental health practices well before the outbreak started.
Survey data, FGDs and KIIs, and project and government reports provided evidence to support the fact that differences in hygiene behaviors promoted by CLTS were related to avoiding EVD in ODF communities. More research in well-designed controlled studies would need to be done before a cause-and-effect relationship can be confirmed between ODF and human diseases. Ethical considerations and the nature of EVD would make case–control studies of a rapidly spreading and highly lethal disease impractical. Other less deadly hygiene-related diseases such as seasonal diarrhea, dysentery, and cholera might serve as proxies for studying any links between ODF and reductions in disease prevalence. Studies elsewhere have shown the impact of ODF on reduction of the incidence of diseases related to poor sanitation and management of public health risks posed by failure to safely confine excreta at the community level (Aiello & Larson, Citation2002; Spears, Ghosh, & Cumming, Citation2013; UNICEF, Citation2016). However, more rigorous studies would need to be done before a cause-and-effect relationship can be confirmed between ODF and Ebola.
Although this study can establish that there was a correlation between adoption of CLTS behaviors prior to the Ebola outbreak and avoidance of EVD cases in communities, it does not prove that CLTS was the only explanation. Identifying correlations, however, is usually the first step pointing researchers in the right direction to help identify causes and methods for addressing them. Even if CLTS were confirmed to be the determining factor in preventing EVD transmission, this would not explain why many communities without CLTS also had no cases. There may be common elements in what the CLTS communities were doing that protected them and what other non-CLTS, non-EVD communities were also doing. It is possible that positive deviant households or individuals were practicing protective behaviors even when other members of the household or community were not. Of course, contact with someone infected with EVD was necessary for a community to be at risk for having a case. There may be other factors related to movement within the population that were not captured in the study. According to WHO (Citation2015), “Community resistance must be tackled by all outbreak responders with the greatest urgency. During 2014, (we) learned that community leaders, including religious leaders as well as tribal chiefs, can play an especially persuasive role in reducing high-risk behaviors.” IWASH/CLTS engaged community leaders, including tribal chiefs. A very important element is the identification of NLs within each community to implement the interventions. Support from formal and informal (tribal) leaders validated and acknowledged communities’ capacity to take actions with their own resources. Although the study was intended to measure differences only between ODF and EVD communities, the data showed that those communities that had been triggered for CLTS but could not complete all of the steps to become ODF also had a much lower risk of having EVD in their community. Only 1 out of 17 non-ODF CLTS communities got Ebola, and a breakdown of community relationships in that community would have prevented the effectiveness of the CLTS approach. Higher percentages of households in CLTS communities, even those that did not reach ODF status, were using latrines at the time of the survey compared to EVD communities. It is possible that participation in CLTS itself may have offered some protective effect. Additional research is needed to understand these findings.
Because communities also make a commitment to taking specific and measurable actions to become ODF, one would expect WASH indicators to be higher in CLTS/ODF communities than in non-CLTS communities. Well-designed studies looking at individual components of CLTS leading to ODF as well as behavioral indicators will be needed to understand the key factors that made the difference.
Ebola was a new disease to the study area and to all of Liberia, hence EVD prevalence at the debut of IWASH was known to be zero. Almost no information about Ebola prevention other than strict isolation of hospitalized patients has been documented. Previous Ebola health research was largely undertaken at health facilities in remote locations in other countries and focused on clinical care; very little is known about community and household factors. The Ebola ODF study was retrospective and not a case–control experimental study (with clearly defined outcomes to compare between intervention and nonintervention communities). The global health community still has much to learn about interrupting disease transmission at the community level, and any correlations identified in the study could help to point the way toward where to look.
Diarrhea and respiratory diseases continue to kill thousands of children in Liberia and other developing countries every year. Although supported in disease transmission theory, and despite anecdotal reports of reduced diseases related to water and hygiene behaviors associated with WASH and CLTS, direct associations as to cause and effect between CLTS implementation and reduced disease prevalence have not yet been confirmed in rigorous public health research studies (Pickering, Djebbari, Lopez, Coulibaly, & Alzua, Citation2015). Most WASH programs, including those implementing CLTS, do not collect information on disease prevalence, and health system data do not effectively measure disease trends at the community level. Two major scientific disciplines that would need to be involved to eventually produce evidence of direct impact of CLTS on human health, public health and WASH, have been working together to develop common implementation language and measurement indicators, but this remains a work in progress.
Methods to measure the direct connection between WASH interventions and improvements in general health status, even those caused by contaminated water and poor sanitation, are still under development. There is a dearth of independently verifiable evidence to support the claim that CLTS has a direct impact on reducing disease prevalence, and more research exploring a set of common indicators used by both the WASH and health sectors is needed (“Measuring Health Impacts of WASH Programs” webinar with Johns Hopkins University School of Public Health and the CORE group, personal communication, January 2015).
Numerous studies linking increased coverage of hand washing with soap and/or point-of-use water treatment and decreased diarrhea and respiratory illness (primarily in children) have been done (Aiello, Coulborn, Perez, & Larson, Citation2008; Luby et al., Citation2005). There are, however, no published studies directly linking water and hygiene behaviors to preventing Ebola transmission. Observational studies and anecdotal reports have noted that improved hygiene practices, especially hand washing and safe disposal of bodily fluids (including from dead bodies), appear to reduce the incidence of new cases of EVD, and those findings are consistent with those found in this study. More research on these practices as well as greater understanding of the overall epidemiology of EVD is needed.
Acknowledgments
We wish to thank the Government of Liberia, including the Lofa County Health Team, for its valuable assistance in conducting the field research.
Funding
The research reported in this article was conducted by Global Communities as part of the Improving Water, Sanitation, and Hygiene (IWASH) project in Liberia funded by USAID.
Additional information
Funding
Notes
1 EVD and Ebola are used interchangeably in this study.
2 The percentage of households exposed to EVD was unknown, and therefore assumptions had to be built in to the model. Experience with field surveys had shown that some households selected for the survey may have declined to participate or there may have been errors in data collection.
3 The full household survey report is available on request.
4 The Lorma and Gbandi ethnic groups live along both sides of the Liberia–Guinea border. Travel between both countries is common (Wikipedia, Citationn.d.a; Citationn.d.b).
5 Mandingos originate in Sierra Leone, but a sizable population in Liberia (Wikipedia, Citationn.d.c) live in the IWASH project districts. Travel between these communities and Sierra Leone is common.
6 Kissi is an ethnic group found in all three EVD countries. Although primarily Christian, Kissi are strongly influenced by animistic and traditional beliefs, especially related to burial practices that were relevant to EVD transmission (Wikipedia, Citationn.d.d). Travel among Kissi populations in all three countries is common.
7 This is a local term referring to intimate contact that includes washing and dressing bodies in preparation for burial and the practice of all funeral attendees touching the body.
8 Triggering is a community event with activities intended to evoke disgust of open defecation in the environment and spur communities to commit to a specific set of actions to change behaviors that lead to ODF status.
9 Additional data from the survey report are available on request.
10 This is an unexpected finding; reasons require further investigation.
11 NLs are only found in CLTS communities.
References
- Aiello, A., Coulborn, R. M., Perez, V., & Larson, E. L. (2008). Effect of hand hygiene on infectious disease risk in the community setting: A meta-analysis. American Journal of Public Health, 98, 1372–1381. doi:10.2105/AJPH.2007.124610
- Aiello, A. E., & Larson, E. L. (2002). What is the evidence for a causal link between hygiene and infections? The Lancet Infectious Diseases, 2, 103–110. doi:10.1016/S1473-3099(02)00184-6
- Centers for Disease Control and Prevention. (2015, October 1). Review of human-to-human transmission of Ebola virus. Retrieved from http://www.cdc.gov/vhf/ebola/transmission/human-transmission.html
- Cochran, W. G. (1963). Sampling techniques (2nd ed.). New York, NY: Wiley.
- D’Harcourt, E. (2014, November). Responding to the Ebola epidemic in Liberia and Sierra Leone: Myth and reality. Presentation at the annual meeting of the American Public Health Association, New Orleans, LA.
- Evans, D. K., Goldstein, M., & Popova, A. (2015). Health-care worker mortality and the legacy of the Ebola epidemic. Lancet Global Health, 3(8), e439–e440. doi:10.1016/S2214-109X(15)00065-0
- Government of Liberia. (2014). Overview of Lofa County. Retrieved from http://tiny.cc/qfsbux
- Government of Liberia, National Technical Coordinating Unit. (2012, December). Guidelines for community-led total sanitation implemented in Liberia. Retrieved from http://wash-liberia.org/wp-content/blogs.dir/6/files/sites/6/2013/06/Final_CLTS_guidlines2.pdf
- Kar, K., & Chambers, R. (2008). Handbook on community led total sanitation. London, UK: Plan UK.
- Liberia Institute of Statistics and Geo-Information Services, Ministry of Health and Social Welfare, National AIDS Control Program, & ICF International. (2014). Liberia Demographic and Health Survey 2013. Retrieved from https://dhsprogram.com/pubs/pdf/FR291/FR291.pdf
- Luby, S. P., Agboatwalla, M., Felkin, D. R., Painter, J., Billhimer, W., Altaf, A., & Hoekstra, R. M. (2005). Effect of handwashing on child health: A randomised controlled trial. The Lancet, 366, 225–233. doi:10.1016/S0140-6736(05)66912-7
- Pickering, A. J., Djebbari, H., Lopez, C., Coulibaly, M., & Alzua, M. L. (2015). Effect of a community-led sanitation intervention on child diarrhoea and child growth in Rural Mali: A cluster-randomised controlled trial. The Lancet Global Health, 3(11), e701–e711. doi:10.1016/S2214-109X(15)00144-8
- Spears, D., Ghosh, A., & Cumming, O. (2013). Open defecation and childhood stunting in India: An ecological analysis of new data from 112 districts. PLoS ONE, 8(9), e73784. doi:10.1371/journal.pone.0073784
- UNICEF. (2016). The state of the world’s children, 2016: A fair chance for every child. New York, NY: United Nations.
- Wikipedia. (n.d.a). Voinjama. Retrieved from https://en.wikipedia.org/wiki/Voinjama
- Wikipedia. (n.d.b). Gbandi people. Retrieved from https://en.wikipedia.org/wiki/Gbandi_people
- Wikipedia. (n.d.c). Mandingo people of Sierra Leone. Retrieved from https://en.wikipedia.org/wiki/Mandingo_people_of_Sierra_Leone
- Wikipedia. (n.d.d). Kissi people. Retrieved from https://en.wikipedia.org/wiki/Kissi_people
- World Health Organization, Global Action and Response. (2015, January). What needs to happen in 2015. Retrieved from http://www.who.int/csr/disease/ebola/one-year-report/response-in-2015/en/