Abstract
Background
There is compelling evidence for an association between negative life events (NLE) and substance-related problems (SRP) during adolescence. The literature is, however, still limited with regards to protective factors for SRP among adolescents exposed to NLE.
Methods
A large population-based survey including 9,611 Norwegian adolescents aged 16 to 19 years, comprised the dataset of this study. The main explanatory variable was NLE. The main outcome variable was SRP, assessed by the CRAFFT scale. Potential protective factors were measured with five subscales from the Resilience Scale for Adolescents (READ) questionnaire. The potential protective factors and sex were explored as moderators for the associations between NLE and SRP.
Results
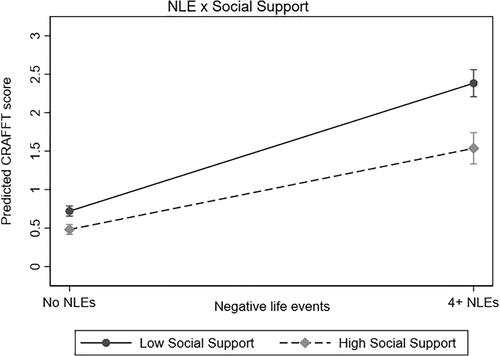
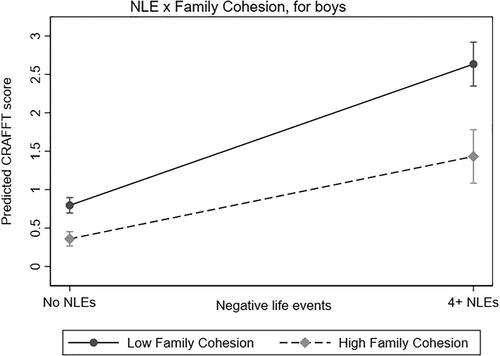
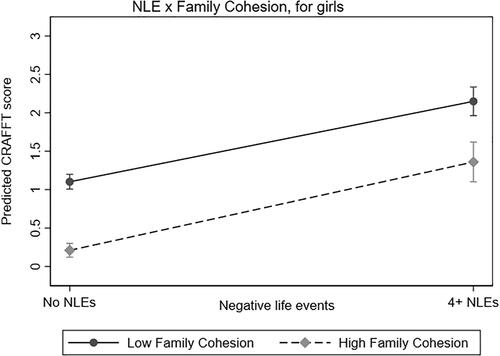
NLE were strongly associated with SRP. Four out of five potential protective factors (i.e., Goal Orientation, Self-confidence, Family Cohesion, and Social Support) showed evidence of a protective-stabilizing effect. Even if they had protective effect across all levels of exposure to NLE, these effects were even stronger for adolescents with high exposure. For Family Cohesion a protective-stabilizing effect was only evident for boys, while a direct protective effect was found for girls. Finally, Social Competence was the only factor that did not show any evidence of promoting resilience toward SRP.
Conclusions
NLE had a strong relation with SRP in this study. Protective factors buffered against SRP for all adolescents – but particularly so for adolescents who had high exposure to NLE. These findings highlight the need for preventive efforts to strengthen protective factors that may promote resilience among adolescents at risk for SRP.
Introduction
There is compelling evidence for an association between negative life events (NLE) and substance-related problems (SRP) during adolescence (Carliner et al., Citation2016; De la Peña-Arteaga et al., Citation2021; Dube et al., Citation2006; Giordano et al., Citation2014; Keyes et al., Citation2011). The scientific literature describes different types of NLE—and all these types appear to be associated with SRP—including adverse childhood experiences (ACE) such as childhood maltreatment and household dysfunction (Anda et al., Citation1999, Citation2006); lifetime exposure to interpersonal violence, e.g. physical assault, sexual assault, or witnessed violence (Keyes et al., Citation2011; Kilpatrick et al., Citation2003; Perkins & Jones, Citation2004); traumatic disasters or accidents, e.g. natural disasters, mass shootings or terrorism (Cerdá et al., Citation2011; DiMaggio et al., Citation2009); and interpersonal loss, e.g. death of parents, family members, friends, or romantic companions (Estaugh & Power, Citation1991; Kendler et al., Citation2002; Melhem et al., Citation2008). Individuals that experience multiple NLE have a substantially increased risk for SRP (Anda et al., Citation2006; Clements-Nolle et al., Citation2022; Enoch, Citation2011; Ford et al., Citation2010; Lloyd & Turner, Citation2008). However, not all adolescents who have been exposed to NLE develop SRP, indicating that moderating factors play an important role (Ma, Citation2006). Accordingly, a growing literature has focused on theoretical models and empirical studies of resilience, which is often defined as “a positive adaptation despite significant adversity” (Luthar et al., Citation2000; Masten et al., Citation1990; Rudzinski et al., Citation2017).
The resilience literature with regards to SRP is fairly new and therefore limited. A range of studies have used the resilience concept, but with large theoretical heterogeneity (Rudzinski et al., Citation2017). Specifically, different studies operationalize resilience as either a trait, an outcome, a process, or as a mix of these aspects (Rudzinski et al., Citation2017). This heterogeneity makes it rather difficult to summarize the existing knowledge and underscores the need for a high degree of specificity of how resilience is defined and operationalized in the context of a given study. Even though some have viewed it has a trait, resilience is probably better understood as the result of a dynamic and complex interplay between protective- and risk factors. This understanding of the concept is in line with the contributions from Fergus et al. (Fergus & Zimmerman, Citation2005) and Luthar et al. (Luthar et al., Citation2000). In their landmark contributions, Luthar and colleagues described resilience in terms of direct and interactive protective processes (Luthar et al., Citation1993, Citation2000). Direct protective processes imply that a protective factor is similarly associated with a favorable outcome across individuals with high and low exposure to adversity. That is, there is no moderation on the association between exposure to adversity and the outcome of interest. On the other hand, interactive processes imply that the presence of a protective factor differentially predicts the outcome based on exposure to adversity (i.e., a moderation is observed between exposure to adversity and the outcome of interest). Several subtypes of such interactive processes are described, including “protective-stabilizing,” “protective-enhancing,” and “protective but reactive” (Luthar et al., Citation2000). For example, if the presence of a protective factor is more strongly associated with a reduction in risk for SRP among adolescents with high exposure to NLE compared with their counterparts with low or no exposure to NLE, this indicates a protective-stabilizing process.
While a range of risk factors for SRP are described (e.g., Swadi, Citation1999,Hawkins et al., Citation1992), protective factors are generally less elaborated on. Protective factors include both internal strengths and external resources, and a distinction can be made between personal factors, factors in the family, and factors in the extended social network/community (Lensch et al., Citation2020; Vella & Pai, Citation2019). Examples of personal factors include self-efficacy, social competence, goals and aspirations, and problem solving; examples of family factors include parental supervision, family connectedness, and parental warmth; and examples of the factors in the extended social network include social support, prosocial peers, and school connectedness.
While a range of studies on substance use have incorporated some measures of resilience (Keyes et al., Citation2011; Rudzinski et al., Citation2017), few studies have investigated protective factors associated with resilience against SRP among adolescents exposed to NLE (Ashaba et al., Citation2022; Lensch et al., Citation2020; Perkins & Jones, Citation2004). Among the notable exceptions, a study by Perkins and colleagues (Perkins & Jones, Citation2004) reported that the personal factors of religiosity and view of future, as well as several factors from the extended social network (i.e., peer group characteristics, positive school climate, and social support) were associated with reduced risk for SRP among 12 to 17 year old adolescents subjected to physical abuse. A recent study by Chatterjee and colleagues (Chatterjee et al., Citation2018) reported that internal assets (i.e., a variety of individual qualities hypothesized to guide positive choices) moderated the associations between NLE and early initiation of marijuana and alcohol use for girls, but not for boys. Some new studies have reported that internal assets such as planning and decision making and commitment to learning (Belintxon et al., Citation2022), and external resources such as social participation (Ashaba et al., Citation2022), protected against SRP among youth who had experienced NLE. None of these studies, however, reported on whether these protective effects were protective-stabilizing, protective-enhancing, or protective but reactive. Some studies have pointed to associations between family factors and adolescent alcohol use (Protinsky & Shuts, Citation1990; Wetherill & Fromme, Citation2007), but these studies did not distinguish between individuals with NLE exposure and those without. In sum, there is emerging evidence that protective factors from both personal domains and the extended social network may be protective against SRP among adolescents exposed to NLE, while there is a lack of studies on how family factors may potentially be protective. Also of note, very little is known on potential sex differences in protective factors against SRP among adolescents exposed to NLE.
In the present study, we aimed to investigate how a range of NLE were associated with SRP during adolescence, considering the potential confounding effects from age and SES. We further explored the role of potential protective factors from the personal domain, the family, and the extended social network on the association between NLE and SRP. Based on previous research we expected to find protective effects of the included potential protective factors (possibly excluding family factors as no previous studies on this topic were found). However, the lack of previous comparable studies prevented more specific hypotheses on whether these protective processes would be best characterized by direct or interactive effects.
Methods
Study population
Data was employed from the youth@hordaland-survey. All adolescents born between 1993 and 1995 living in Hordaland County in Western Norway were invited to participate (n = 19,430), and of these, 10,257 adolescents chose to participate, giving a participation rate of 53%. After excluding participants who reported a high number of NLE in combination with unlikely scores on other variables (n = 12) and those with missing on all the NLE variables (n = 634), the final sample included 9,611 individuals.
Youth@hordaland is a cross-sectional population-based study carried out during early 2012, and data was collected from adolescents in upper secondary school. The adolescents received information per email and one school hour was used to complete the questionnaires at school. In addition, adolescents not going to school received the questionnaires by mail at their home address. Mental health services and other institutions were also contacted to facilitate participation in these settings. The questionnaires used in the youth@hordaland study were web-based, and electronic informed consent was obtained from all participants. The Regional Committee for Medical and Health Research Ethics in Western Norway approved the study.
Explanatory variable: Negative life events
Negative life events (NLE) included eight items: (1) “death of a parent”; (2) “death of a sibling”; (3) “death of a friend”; (4) “death of a boyfriend/girlfriend”; (5) “Having encountered an accident/disaster”; (6) “experienced violence from an adult”; (7) “having witnessing violence from an adult”; and (8) “unwanted sexual actions.” Items 1-4 were dichotomous (“Yes”/“No”); item 5 was ordinal with three response categories (“No, never,” “yes, once,” to “Yes, more than once”); and items 6-8 were ordinal with four response categories (“No, never,” “Yes, once,” “Yes, a few times,” to “Yes, many times”). All the ordinal variables were dichotomized to separate those answering “No, never” from those with positive responses. A variety scale was then constructed by summing the eight dichotomous NLE-variables. The total NLE-variable included the following levels: None; 1 NLE; 2 NLE; 3 NLE; and 4 or more NLE. See for more details on the distribution of NLE in our sample.
Table 1. Distribution of negative life experiences, protective factors and CRAFFT scores across sex (n = 9,611).
Outcome variable: Substance-related problems
SRP was the main outcome variable in this study and was measured using the six-item CRAFFT scale. This scale has been designed to identify potential SRP among adolescents, has been demonstrated to have acceptable sensitivity and specificity at a cutoff of ≥2 (Dhalla et al., Citation2011), and has shown to be effective as a screening tool for SRP (Pediatric Emergency Care Applied Research Network., 2019). This scale has previously been investigated in relation to psychometric properties and convergent validity in the present sample (Skogen et al., Citation2013), showing a linear relationship between the continuous CRAFFT score and excessive alcohol consumption, binge drinking, and illicit drug use. In the present study, we used the continuous total score on CRAFFT (ranging from 0 to 6; mean = 0.82) as an outcome variable for SRP.
Potential protective factors
The Resilience Scale For Adolescents (READ) was originally developed as an adaptation of the Resilience Scale for Adults (RSA) to adolescents (Friborg et al., Citation2003; Hjemdal et al., Citation2001). READ includes 28 items, which were originally grouped into five scales. Several studies have found a poor fit for the original factor solution and have modified the scale by removing problematic items (Moksnes & Haugan, Citation2018; von Soest et al., Citation2010) or identifying a new factor structure (Ruvalcaba-Romero et al., Citation2014). A recent Norwegian study based on the youth@hordaland-population (which also forms the basis for the present study) concluded that changes to the original factor structure were necessary and that the items assess the following five factors: (1) Goal Orientation; (2) Self-confidence; (3) Social Competence; (4) Family Cohesion; and (5) Social Support (Askeland et al., Citation2020). In the present study, we used this operationalization of the factors. We defined the first three as personal protective factors, the fourth as a family factor, and the last as a factor from the extended social network. See for the distribution of READ scores in our sample. Prior to use in the regression analyses, the scores on each READ scale were converted to z-scores (a common standardization of the data: i.e., a z-score of 0 equals the mean; a z-score of 1 equal one standard deviation over the mean).
Included co-variates
Demographic information was included and used as control variables in the main regression analyses. Age and sex were retrieved from the Norwegian Population Registry and were available for all participants in the youth@hordaland-sample. Self-reported information about family economic well-being were collected as either (1) “poorer than others,” (2) ‘equal to others,” or (3) “better than others.” Self-reported information on maternal and paternal educational attainment was divided into primary school, high school, or university or higher education. The variables of self-reported family financial circumstances, paternal educational attainment, and maternal educational attainment were all used as indicators of socioeconomic status (SES) (Skogen et al., Citation2014).
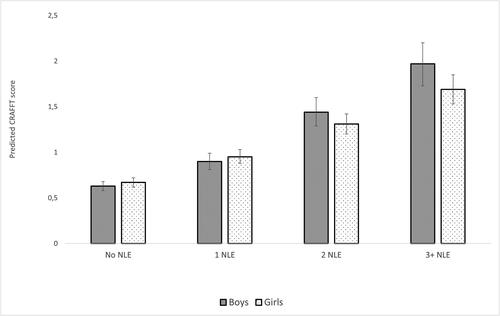
Statistical analysis
We conducted the following statistical analyses: First, the sample was described according to age, sex, and SES. We used t-tests for independent samples and Pearson chi-square tests to indicate sex differences in the participants’ rates of NLE and mean level of protective factors. In addition, Cohen’s d effect size of mean differences across sex were reported where applicable (). Second, we conducted linear regression analyses for associations between ordinal levels of NLE and total CRAFFT scores. These analyses were adjusted by age, SES, and the interaction term of “NLE x gender.” Due to a significant interaction of “NLE x gender” (p < 0.01), we stratified all these analyses by sex. To explore whether this association was graded, we visualized predicted CRAFFT scores across ordinal levels of NLE for each sex, with 95% confidence intervals. Due to small cells in the “4+ NLE” category, we reduced the NLE variable to the following levels (“No NLE,” “1 NLE,” “2 NLE,” and “3+ NLE”) for this analysis (see and ). Third, we conducted linear regression analyses for associations between ordinal levels of NLE and total CRAFFT scores, including the variables of sex, age, and SES in all analyses. Individual analyses were done for each of the five protective factors from READ, repeated through three models (totaling 15 analyses; see ). In model 1 we included the specific protective factor of interest. Model 2 added to model 1 the adjustment for the two-way interaction term of “NLE x protective factor.” Model 3 added to model 1 the three-way interaction of “NLE x protective factor x sex.” Finally, we constructed margin plots that displayed SRP (i.e., predicted CRAFFT scores) across the interactions between levels of NLE and z-scores of each protective factor. Specifically, −2 standard deviations indicated “low scores” on a protective factor while +2 standard deviations indicated “high scores.” These margin plots were stratified by sex if model 3 (see ) indicated a three-way interaction; otherwise, they showed analyses from both sexes combined. Missing was handled with listwise deletion. A sensitivity analysis was conducted by repeating all analyses with a dichotomous CRAFFT score. (All analyses were performed using STATA V.16.0 (StataCorp, Citation2019).
Table 2. Results from interaction models predicting CRAFFT score from negative life events and protective factors (n = 9,611).
Results
The distribution of NLE was positively skewed for both genders (mean= 0.63; median = 0; interquartile range: 0-1; skewness = 1.74; kurtosis = 6.56). Girls had a higher mean number of NLE compared with boys (Cohens d = 0.25, p < 0.001). Specifically, girls reported more frequently to having encountered an accident/disaster, experienced violence from an adult, witnessed violence from an adult, and having encountered sexual unwanted actions (all ps < 0.001). Also, the distribution of CRAFFT scores was positively skewed for both genders (mean = 0.82; median = 0; interquartile range: 0-1; skewness = 1.78; kurtosis = 6.13). Girls reported slightly higher CRAFFT scores (Cohens d = 0.09; p < 0.001). See for details. In relation to protective factors, boys had higher mean scores on the protective factors of Goal Orientation, Family cohesion, Social Competence, and Self-confidence, while girls had higher mean score on Social Support (all ps < 0.001).
Linear regression analyses demonstrated a strong positive association between NLE and SRP for both sexes (all ps < 0.001), but with somewhat stronger magnitude for boys (adjusted mean difference = 0.38, 95%CI: [0.32, 0.43]) compared with girls (adjusted mean difference = 0.30, 95%CI: [0.26, 0.34]). shows that the association between ordinal levels of NLE and SRP was characterized by a graded effect (for details, see ).
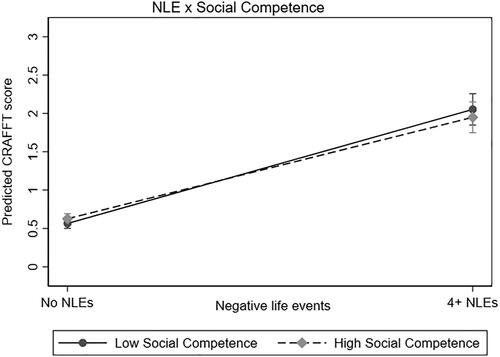
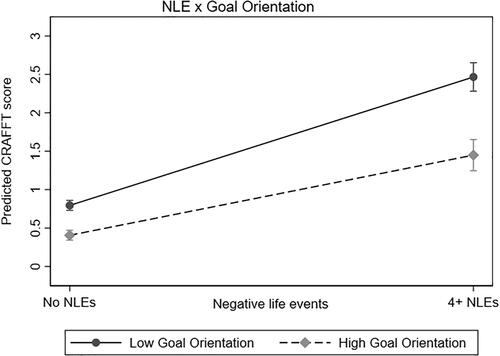
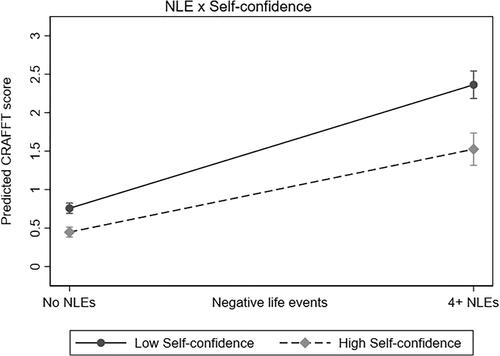
outlines the analyses including the protective factors as moderators of the association between NLE and SRP. In model 1, four out of five protective factors (i.e., Goal Orientation, Social Support, Family Cohesion, and Self-confidence) significantly reduced the magnitude of the association between NLE and SRP (mean differences [mean diff] ranging from −0.09 to −0.18, all ps < 0.001). Social Competence did not show any significant protective effects (). In model 2 there were additional two-way interactions between NLE and Goal Orientation, NLE and Social Support, and NLE and Self-confidence (mean diff ranging from −0.03 to −0.04, all ps <0.01), indicating interactive protective effects. More specifically, these interaction effects were protective-stabilizing (Luthar et al., Citation2000) (see ). For model 3, one significant three-way interaction in the prediction of SRP was identified between NLE, Family Cohesion and sex (mean diff = −0.05, p < 0.05), indicating sex differences for this interactive protective effect. Hence, there was a protective-stabilizing effect from Family Cohesion for boys (), but only a direct protective effect of Family Cohesion for girls ().
A sensitivity analysis using dichotomous CRAFFT scores for the most part confirmed these results, with the exception that the two-way interaction between Goal Orientation and NLE (p = 0.06) and the three-way interaction between Family Cohesion, NLE, and Sex (p = 0.11) were no longer statistically significant.
Discussion
The present study revealed a strong relation between NLE and SRP. These findings support the large literature that has shown clear links between NLE and substance-related outcomes. Whereas some of the most influential studies in this research field have reported adverse childhood experiences as potent risk factors for SRP (Anda et al., Citation1999, Citation2006), we used relatively common lifetime-aggregated NLE as our explanatory variables. These findings are consistent with a range of studies that has documented that NLE from different domains (e.g., interpersonal loss/death, interpersonal violence, and traumatic disasters/accidents) increase the risk of adolescent SRP (Estaugh & Power, Citation1991; Keyes et al., Citation2011; Kilpatrick et al., Citation2003). The present study showed a graded relationship between these common lifetime-aggregated NLE and adolescent SRP. Thus, our study adds to the scientific literature that points to a particularly high risk of SRP among individuals with a high exposure to NLE (Anda et al., Citation2006; Clements-Nolle et al., Citation2022; Enoch, Citation2011; Ford et al., Citation2010). The main contribution from the present investigation is, however, related to our analyses of resilience. We found protective-stabilizing effects for four out of five potential protective factors on the association between NLE and SRP. Specifically, these protective-stabilizing effects were detected from personal factors (i.e., Goal Orientation and Self-confidence), a family factor (i.e., Family Cohesion, boys only), and a factor from the extended social network (i.e., Social Support).
Our findings highlight that two out of three protective factors from the personal domain (i.e., Goal Orientation and Self-confidence) mitigated the risk for adolescent SRP, while no such protective effect was found for Social Competence. These findings add knowledge to the existing literature base in several respects. Other studies have highlighted goals and aspirations, and view of the future, as internal protective factors in relation to adolescent SRP (Hodder et al., Citation2016; Perkins & Jones, Citation2004). As the READ scale of Goal Orientation in part focus on goals and a positive evaluation of one’s efficacy in reaching those goals in the future, our study may be interpreted to support those previous findings. The Self-confidence scale focus on self-confidence and self-efficacy skills relating to solving difficult life situations. Hypothetically, self-confidence may contribute to the choice of other means of coping than “self-medication” with substances in the face of emotional and social problems following life difficulties, or to a lower vulnerability when it comes to adopting deviant behaviors and substance use following peer pressure. Supporting this notion, self-medication with substances is closely linked with deficits in self-regulation skills, in part arising from difficulties with regulating affects, self-esteem, relationships, and self-care (Khantzian, Citation1997). Furthermore, self-esteem—which bear similarities with the READ scale of Self-confidence—is associated with developmentally healthy outcomes, including reduced alcohol use and susceptibility to peer pressure (Zimmerman et al., Citation1997). In short, our study points to the need for interventions that aim to strengthen the personal domains of goal orientation and self-confidence among adolescents with high exposure to NLE.
In the present study, Family Cohesion was a protective factor in the association between NLE and SRP. Our findings support previous studies that have pointed to associations between family factors, such as family cohesion and parental warmth, and adolescent alcohol use (Protinsky & Shuts, Citation1990; Wetherill & Fromme, Citation2007). A study by Marshal and Chassin (Marshal & Chassin, Citation2000) reported that parental social support and discipline buffered adolescent girls from the influence of substance-use promoting peers in relation to alcohol use, while both variables (parental social support and discipline) exacerbated peer effects on boys’ alcohol use. The present study adds to these previous results by also highlighting family cohesion as a robust protective factor following NLE exposure. Our results are also novel in highlighting that family cohesion had a somewhat stronger protective effect among boys with higher levels of NLE compared with boys with lower levels of NLE. It is difficult to provide firm conclusions on why this risk moderation effect was not seen among girls. Potentially, this has to do with differences in the distribution of NLE across the sexes (for example, girls had higher rates of experiences with unwanted sexual events compared with boys). This is a mere speculation, however, and future studies are needed to replicate whether there are true sex differences in the protective factor of family cohesion on risk for SRP and how these sex differences could be explained. It should also be noted in this respect that both girls and boys had a direct protective effect from family cohesion on the risk or SRP. Therefore, our study underscores the need for interventions that aim to strengthen a supportive family environment as a means of reducing risk for SRP among adolescents with high NLE exposure.
We also found protective effects of the Social Support scale on the association between NLE and SRP. This scale focuses on caring relationships with family and friends, as well as access to support, without distinguishing between peer and adult social support. Some previous studies have pointed to associations between social support and adolescent SRP. Previous studies have for example suggested that external factors such as positive peer group characteristics and social support protect adolescents from substance use-involvement (Hodder et al., Citation2016; Perkins & Jones, Citation2004). A study by Wills and Vaughan (Wills & Vaughan, Citation1989) reported that adult social support was associated with reduced adolescent alcohol use, while peer social support was associated with more alcohol use for subjects with low levels of adult support. Hence, the blending of peer and family social support in the READ Social Support-variable confounds the interpretation of our findings. Nevertheless, our findings suggest that social support—as a composite of peer and family social support—contributed to lower risk for SRP, particularly among individuals exposed to NLE. This finding lend some support to a previous study that highlighted social support among the factors that protected adults exposed to potentially traumatic events from psychopathology, including substance use (Bonanno et al., Citation2007). Thus, social support appears as another potential target of intervention for SRP prevention efforts among at-risk adolescents.
Finally, we found that Social Competence was the only protective factor from the READ questionnaire that did not have any statistically significant protection effect on adolescent SRP. This finding lends support to a study by Belintxon and colleagues who reported that social competence did not facilitate resilience toward SRP among adolescents exposed to NLE, unlike for example planning and decision making (Belintxon et al., Citation2022). A study by Scheier and coworkers reported that a general measure of social competence had no long-term effects on alcohol use among adolescents, while poor refusal skills (i.e., a specific sub-type of social competence) were associated with higher alcohol use (Scheier et al., Citation1999). The items comprising the READ Social Competence scale resolves around general social skills such as competence in making friends and the ability to have positive conversations. Hence, these social competence skills may not be as relevant in relation to reducing risk of adolescent SRP as for example refusal skills. A study by Chen and coworkers found that two sub-factors of social competence (i.e., prosociality and sociability) were associated with SRP in opposite directions (Chen et al., Citation2019). Thus, different aspects of social competence appear to increase and decrease probability of SRP, respectively. Furthermore, substance use during adolescence appears to have a predominantly social nature (Colder et al., Citation2013), and high social competence per se may therefore not protect against substance involvement during this period in life.
Implications
Previous literature is limited in regards to factors that may promote resilience in adolescents exposed to high risk for SRP (Keyes et al., Citation2011). Better knowledge of factors that contribute to reducing the risk for SRP among adolescents that has experienced NLE, may be pivotal in informing more targeted prevention initiatives. For instance, asset-building programs may potentially mitigate the consequences of high-risk backgrounds in adolescence and even into adulthood (Chatterjee et al., Citation2018). It has been suggested that interventions aiming at reducing risk for adolescent SRP need to focus on specific protective factors (Hodder et al., Citation2016). The present study highlights the potential benefits of promoting protective factors from the personal domain, family, and the extended social network in adolescents at high-risk for SRP. Specifically, Goal Orientation and Self-confidence are personal protective factors that may be leveraged to alleviate risk for problematic substance use involvement. In addition, Social Support and Family Cohesion are external protective factors that should also be promoted in high-risk adolescents. Family cohesion could potentially be increased through various family-strengthening programs. Interestingly, Social Competence was not associated with any protective effects against SRP in the present study. This does not necessarily imply that strengthening of social competence is ineffective as part of prevention programs toward SRP. However, this finding actualizes the need to critically evaluate which social skills that should be targeted in such programs and why. For example, life skills-program that include focus on refusal skills/drug resistance skills show promising results for adolescents (Botvin & Griffin, Citation2014). To enhance our understanding of the potential protective effects of social competence on substance use outcomes, future research should therefore take aim at measuring specific domains of social competence, and follow-up results from adolescence into adulthood. Future studies are needed to expand our understanding of the mechanisms involved in the protective effects that derive from selected variables across the personal domain, the family, and the extended social network.
Strengths and limitations
The present study has several strengths. We used a large population-based sample of adolescents; a validated questionnaire for the measurement of potential protective factors (Askeland et al., Citation2020), and SRP (Skogen et al., Citation2013); and a set of relatively common stressful or negative life events to construct a composite measure of cumulative load of NLE. We adhered to a pronounced call in the scientific literature for more studies that investigate protective effects, including risk moderation effects, in the associations between NLE and SRP. A previous population-based study found that the geographical area from where the adolescents came, Hordaland county, to be regarded as relatively representative of the general Norwegian population (Folkehelseinstituttet, Citation2010). The study also has some limitations. The cross-sectional design of the study limits our ability to draw conclusions on causality or directionality of the analyzed associations and moderation effects. All the included measures were based on self-report, and the application of either registry data or clinical interview would have added strength to our data. We also acknowledge the possibility of dependent error given that the exposures (NLE and protective factors) and outcome (substance use) were self-reported on the same survey questionnaire (Ranker et al., Citation2019).
Conclusions
NLE are strong and robust correlates of SRP among adolescents, and we found a graded relationship between common lifetime-aggregated NLE and adolescent SRP. Protective factors from the personal domain, the family, and the extended social network moderated the associations between NLE and SRP. These findings highlight the need for prevention efforts to strengthen selected protective factors in individuals at risk for developing SRP during adolescence.
| Abbreviations | ||
| SRP | = | substance-related problems |
| NLE | = | negative life events |
| READ | = | Resilience Scale for Adolescents |
Acknowledgements
We thank the Bergen Child Study at the Regional Centre for Child and Youth Mental Health and Child Welfare at NORCE Norwegian Research Centre for collecting the data, and for making it available for this study.
Declaration of interest
The authors declare that they have no conflict of interest. The authors alone are responsible for the content and writing of the article.
Data availability statement
The Norwegian Health research legislation and the Norwegian Ethics committees require explicit consent from the participants to transfer health research data outside of Norway. For the Bergen Child study, which constitutes the data for the current analyses, ethics approval was also contingent on storing the research data on secure storage facilities located in our research institution, which prevents us from providing the data as supplementary information or to transfer it to data repositories. Individual requests for data access should be sent to [email protected].
Additional information
Funding
References
- Anda, R. F., Croft, J. B., Felitti, V. J., Nordenberg, D., Giles, W. H., Williamson, D. F., & Giovino, G. A. (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA, 282(17), 1652–1658. https://doi.org/10.1001/jama.282.17.1652
- Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186. https://doi.org/10.1007/s00406-005-0624-4
- Ashaba, S., Kakuhikire, B., Baguma, C., Satinsky, E. N., Perkins, J. M., Rasmussen, J. D., Cooper-Vince, C. E., Ahereza, P., Gumisiriza, P., Kananura, J., & Bangsberg, D. R. (2022). Adverse childhood experiences, alcohol consumption, and the modifying role of social participation: Population-based study of adults in southwestern Uganda. SSM-Mental Health, 2, 100062. https://doi.org/10.1016/j.ssmmh.2022.100062
- Askeland, K. G., Hysing, M., Sivertsen, B., & Breivik, K. (2020). Factor structure and psychometric properties of the Resilience Scale for Adolescents (READ). Assessment, 27(7), 1575–1587.
- Belintxon, M., Calatrava, M., Osorio, A., Balaguer, Á., & Vidaurreta, M. (2022). Internal developmental assets and substance use among Hispanic adolescents. A cross‐sectional study. Journal of Advanced Nursing, 78(7), 1990–2003.
- Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5), 671–682. https://doi.org/10.1037/0022-006X.75.5.671
- Botvin, G. J., & Griffin, K. W. (2014). Life skills training: Preventing substance misuse by enhancing individual and social competence. New directions for Youth Development, 2014(141), 57–65, 11. https://doi.org/10.1002/yd.20086
- Carliner, H., Keyes, K. M., McLaughlin, K. A., Meyers, J. L., Dunn, E. C., & Martins, S. S. (2016). Childhood trauma and illicit drug use in adolescence: A population-based national comorbidity survey replication–adolescent supplement study. Journal of the American Academy of Child and Adolescent Psychiatry, 55(8), 701–708. https://doi.org/10.1016/j.jaac.2016.05.010
- Cerdá, M., Tracy, M., & Galea, S. (2011). A prospective population based study of changes in alcohol use and binge drinking after a mass traumatic event. Drug and Alcohol Dependence, 115(1–2), 1–8. https://doi.org/10.1016/j.drugalcdep.2010.09.011
- Chatterjee, D., McMorris, B., Gower, A. L., Forster, M., Borowsky, I. W., & Eisenberg, M. E. (2018). Adverse childhood experiences and early initiation of marijuana and alcohol use: The potential moderating effects of internal assets. Substance use & Misuse, 53(10), 1624–1632.
- Chen, L., Chen, X., Zhao, S., French, D. C., Jin, S., & Li, L. (2019). Predicting substance use and deviant behavior from prosociality and sociability in adolescents. Journal of Youth and Adolescence, 48(4), 744–752. https://doi.org/10.1007/s10964-018-0940-4
- Clements-Nolle, K. D., Lensch, T., Drake, C. S., & Pearson, J. L. (2022). Adverse childhood experiences and past 30-day cannabis use among middle and high school students: The protective influence of families and schools. Addictive Behaviors, 130, 107280. https://doi.org/10.1016/j.addbeh.2022.107280
- Colder, C. R., Scalco, M., Trucco, E. M., Read, J. P., Lengua, L. J., Wieczorek, W. F., & Hawk, L. W. (2013). Prospective associations of internalizing and externalizing problems and their co-occurrence with early adolescent substance use. Journal of Abnormal Child Psychology, 41(4), 667–677. https://doi.org/10.1007/s10802-012-9701-0
- De la Peña-Arteaga, V., Nogueira, S. O., Lynskey, M., & Hines, L. A. (2021). The relationship between childhood physical and sexual abuse and adolescent cannabis use: A systematic review. Frontiers in Psychiatry, 12, 631245. https://doi.org/10.3389/fpsyt.2021.631245
- Dhalla, S., Zumbo, B., & Poole, G. (2011). A review of the psychometric properties of the CRAFFT instrument: 1999-2010. Current Drug Abuse Reviews, 4(1), 57–64. https://doi.org/10.2174/1874473711104010057
- DiMaggio, C., Galea, S., & Li, G. (2009). Substance use and misuse in the aftermath of terrorism. A Bayesian meta‐analysis. Addiction (Abingdon, England), 104(6), 894–904. https://doi.org/10.1111/j.1360-0443.2009.02526.x
- Dube, S. R., Miller, J. W., Brown, D. W., Giles, W. H., Felitti, V. J., Dong, M., & Anda, R. F. (2006). Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health, 38(4), 444-e1–444-e10. https://doi.org/10.1016/j.jadohealth.2005.06.006
- Enoch, M.-A. (2011). The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology, 214(1), 17–31. https://doi.org/10.1007/s00213-010-1916-6
- Estaugh, V., & Power, C. (1991). Family disruption in early life and drinking in young adulthood. Alcohol and Alcoholism (Oxford, Oxfordshire), 26(5–6), 639–644. https://doi.org/10.1093/oxfordjournals.alcalc.a045168
- Fergus, S., & Zimmerman, M. A. (2005). Adolescent resilience: A framework for. Annual Review of Public Health, 26, 399–419. https://doi.org/10.1146/annurev.publhealth.26.021304.144357
- Folkehelseinstituttet. (2010). The Hordaland Health Study 1997–1999.
- Ford, J. D., Elhai, J. D., Connor, D. F., & Frueh, B. C. (2010). Poly-victimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 46(6), 545–552. https://doi.org/10.1016/j.jadohealth.2009.11.212
- Friborg, O., Hjemdal, O., Rosenvinge, J. H., & Martinussen, M. (2003). A new rating scale for adult resilience: What are the central protective resources behind healthy adjustment? International journal of Methods in Psychiatric Research, 12(2), 65–76. https://doi.org/10.1002/mpr.143
- Giordano, G. N., Ohlsson, H., Kendler, K. S., Sundquist, K., & Sundquist, J. (2014). Unexpected adverse childhood experiences and subsequent drug use disorder: A Swedish population study (1995–2011). Addiction (Abingdon, England), 109(7), 1119–1127. https://doi.org/10.1111/add.12537
- Hawkins, J. D., Catalano, R. F., & Miller, J. Y. (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin, 112(1), 64–105. https://doi.org/10.1037/0033-2909.112.1.64
- Hjemdal, O., Friborg, O., Martinussen, M., & Rosenvinge, J. H. (2001). Mestring og psykologisk motstandsdyktighet hos voksne: Utvikling og foreløpig validering av et nytt instrument. Tidsskrift for Norsk Psykologforening.
- Hodder, R. K., Freund, M., Bowman, J., Wolfenden, L., Gillham, K., Dray, J., & Wiggers, J. (2016). Association between adolescent tobacco, alcohol and illicit drug use and individual and environmental resilience protective factors. BMJ Open, 6(11), e012688. https://doi.org/10.1136/bmjopen-2016-012688
- Kendler, K. S., Sheth, K., Gardner, C. O., & Prescott, C. A. (2002). Childhood parental loss and risk for first-onset of major depression and alcohol dependence: The time-decay of risk and sex differences. Psychological Medicine, 32(7), 1187–1194. https://doi.org/10.1017/s0033291702006219
- Keyes, K. M., Hatzenbuehler, M. L., & Hasin, D. S. (2011). Stressful life experiences, alcohol consumption, and alcohol use disorders: The epidemiologic evidence for four main types of stressors. Psychopharmacology, 218(1), 1–17. https://doi.org/10.1007/s00213-011-2236-1
- Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. https://doi.org/10.3109/10673229709030550
- Kilpatrick, D. G., Ruggiero, K. J., Acierno, R., Saunders, B. E., Resnick, H. S., & Best, C. L. (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology, 71(4), 692–700. https://doi.org/10.1037/0022-006x.71.4.692
- Lensch, T., Clements-Nolle, K., Oman, R. F., Lu, M., & Evans, W. P. (2020). Prospective relationships between youth assets, negative life events, and binge drinking in a longitudinal cohort of the youth. Annals of Epidemiology, 46, 24–30. https://doi.org/10.1016/j.annepidem.2020.04.005
- Lloyd, D. A., & Turner, R. J. (2008). Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug and Alcohol Dependence, 93(3), 217–226. https://doi.org/10.1016/j.drugalcdep.2007.09.012
- Luthar, S. S., Cicchetti, D., & Becker, B. (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71(3), 543–562. https://doi.org/10.1111/1467-8624.00164
- Luthar, S. S., Doernberger, C. H., & Zigler, E. (1993). Resilience is not a unidimensional construct: Insights from a prospective study of inner-city adolescents. Development and Psychopathology, 5(4), 703–717. https://doi.org/10.1017/S0954579400006246
- Ma, E. (2006). Genetic and environmental influences on the development of alcoholism: Resilience vs. risk. Annals of the New York Academy of Sciences, 1094(1), 193–201.
- Marshal, M. P., & Chassin, L. (2000). Peer influence on adolescent alcohol use: The moderating role of parental support and discipline. Applied Developmental Science, 4(2), 80–88. https://doi.org/10.1207/S1532480XADS0402_3
- Masten, A. S., Best, K. M., & Garmezy, N. (1990). Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology, 2(4), 425–444. https://doi.org/10.1017/S0954579400005812
- Melhem, N. M., Walker, M., Moritz, G., & Brent, D. A. (2008). Antecedents and sequelae of sudden parental death in offspring and surviving caregivers. Archives of Pediatrics & Adolescent Medicine, 162(5), 403–410. https://doi.org/10.1001/archpedi.162.5.403
- Moksnes, U. K., & Haugan, G. (2018). Validation of the Resilience Scale for Adolescents in Norwegian adolescents 13–18 years. Scandinavian Journal of Caring Sciences, 32(1), 430–440. https://doi.org/10.1111/scs.12444
- Perkins, D. F., & Jones, K. R. (2004). Risk behaviors and resiliency within physically abused adolescents. Child abuse & Neglect, 28(5), 547–563. https://doi.org/10.1016/j.chiabu.2003.12.001
- Protinsky, H., & Shuts, L. (1990). Adolescent substance use and family cohesion. Family Therapy: The Journal of the California Graduate School of Family Psychology, 17(2), 173–175.
- Ranker, L. R., Petersen, J. M., & Fox, M. P. (2019). Awareness of and potential for dependent error in the observational epidemiologic literature: A review. Annals of Epidemiology, 36, 15–19. https://doi.org/10.1016/j.annepidem.2019.06.001
- Rudzinski, K., McDonough, P., Gartner, R., & Strike, C. (2017). Is there room for resilience? A scoping review and critique of substance use literature and its utilization of the concept of resilience. Substance abuse Treatment, Prevention, and Policy, 12(1), 41. https://doi.org/10.1186/s13011-017-0125-2
- Ruvalcaba-Romero, N. A., Gallegos-Guajardo, J., & Villegas-Guinea, D. (2014). Validation of the resilience scale for adolescents (READ) in Mexico. Journal of Behavior, Health & Social Issues (México, 6(2), 21–34. ). https://doi.org/10.22201/fesi.20070780.2014.6.2.48555
- Scheier, L. M., Botvin, G. J., Diaz, T., & Griffin, K. W. (1999). Social skills, competence, and drug refusal efficacy as predictors of adolescent alcohol use. Journal of Drug Education, 29(3), 251–278. https://doi.org/10.2190/M3CT-WWJM-5JAQ-WP15
- Shenoi, R. P., Linakis, J. G., Bromberg, J. R., Casper, T. C., Richards, R., Mello, M. J., Chun, T. H., Spirito, A., & Pediatric Emergency Care Applied Research Network. (2019). Predictive validity of the CRAFFT for substance use disorder. Pediatrics, 144(2), e20183415. https://doi.org/10.1542/peds.2018-3415
- Skogen, J. C., Bøe, T., Knudsen, A. K., & Hysing, M. (2013). Psychometric properties and concurrent validity of the CRAFFT among Norwegian adolescents. Ung@ hordaland, a population-based study. Addictive Behaviors, 38(10), 2500–2505. https://doi.org/10.1016/j.addbeh.2013.05.002
- Skogen, J. C., Sivertsen, B., Lundervold, A. J., Stormark, K. M., Jakobsen, R., & Hysing, M. (2014). Alcohol and drug use among adolescents: And the co-occurrence of mental health problems. Ung@ hordaland, a population-based study. BMJ Open, 4(9), e005357. https://doi.org/10.1136/bmjopen-2014-005357
- StataCorp. (2019). Stata Statistical Software: Release 16. StataCorp LLC.
- Swadi, H. (1999). Individual risk factors for adolescent substance use. Drug and Alcohol Dependence, 55(3), 209–224. https://doi.org/10.1016/s0376-8716(99)00017-4
- Vella, S.-L. C., & Pai, N. B. (2019). A theoretical review of psychological resilience: Defining resilience and resilience research over the decades. Archives of Medicine and Health Sciences, 7(2), 233. https://doi.org/10.4103/amhs.amhs_119_19
- von Soest, T., Mossige, S., Stefansen, K., & Hjemdal, O. (2010). A validation study of the Resilience Scale for Adolescents (READ). Journal of Psychopathology and Behavioral Assessment, 32(2), 215–225. https://doi.org/10.1007/s10862-009-9149-x
- Wetherill, R. R., & Fromme, K. (2007). Perceived awareness and caring influences alcohol use by high school and college students. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors, 21(2), 147–154. https://doi.org/10.1037/0893-164X.21.2.147
- Wills, T. A., & Vaughan, R. (1989). Social support and substance use in early adolescence. Journal of Behavioral Medicine, 12(4), 321–339. https://doi.org/10.1007/BF00844927
- Zimmerman, M. A., Copeland, L. A., Shope, J. T., & Dielman, T. E. (1997). A longitudinal study of self-esteem: Implications for adolescent development. Journal of Youth and Adolescence, 26(2), 117–141. https://doi.org/10.1023/A:1024596313925