Abstract
Background
Patient-reported outcome measures (PROMs) provide clinicians a greater understanding of patients’ perceived ability in their physical performance. Existing PROMs on falls efficacy provide meaningful information about the perceived ability in older people to perform common activities of daily living without falling. However, the perceived ability to recover balance from a slip, a trip, or volitional movements has been inadequately assessed. Balance recovery confidence relates to the judgment of self-reactive ability. The scale of balance recovery confidence (BRC) is a new PROM that measures perceived balance recovery self-efficacy. The purpose of the study protocol is to describe the first psychometric evaluation of BRC’s measurement properties.
Objective
This study is a validation phase of a newly developed PROM conducted in Singapore.
Methods
Two hundred community-dwelling older adults, aged 65 years and older, will complete five self-reported instruments (BRC, Activities-specific Balance Confidence Scale, Falls Efficacy Scale-International, Late-Life Function and Disability Instrument-Function and Global Perceived Effect) and three performance measures (Hand strength dynamometer, 30-second Chair Stand, Mini BESTest). Classical test theory methods will assess acceptability, data completeness, targeting of the items, scaling assumptions, internal consistency reliability and construct validity. Factor analysis will establish unidimensionality. Rasch analysis will evaluate item fit, differential item functioning, response scale ordering, targeting of persons and items and the reliability.
Results
The findings from this study will be published in peer-reviewed journals and presented at national and international conferences in rehabilitation-specific context.
Conclusions
This is the first validation study of BRC. The study will give confidence among clinicians and researchers to use the BRC in fall management research and clinical practice.
Background
Patient-reported outcome measures (PROMs) have been widely used amongst physiotherapists to guide evidence-based treatment planning and delivery [Citation1]. These self-reported instruments elicit information about the status of a patient’s health condition directly from the patient without interpretation of the patient’s response by a clinician or anyone else [Citation2]. This approach of obtaining ‘patient-centred’ data has been actively encouraged for clinicians to demonstrate measurable improvements in these clinical outcomes of their patients as part of daily practice [Citation3,Citation4]. A well-designed PROM can accurately capture the patient’s own opinions on the impact of their condition, and its treatment, on their life [Citation1]. However, a poor designed PROM can constitute a waste of resources and is unethical [Citation5]. According to the international COSMIN (COnsensus-based Standards for the selection of health Measurement INstruments) initiative, a PROM developed with a coherent and transparent methodology provides confidence amongst clinicians and researchers about the validity of the PROM and meaningfulness of its data [Citation6].
Numerous PROMs have been developed to measure falls-related self-efficacy (falls efficacy) in older people. The conceptual frameworks of these PROMs have been underpinned by Bandura’s self-efficacy theory [Citation7], describing how older people are empowered to effect change in themselves and their situations through their efforts. Self-efficacy is defined as the ‘beliefs in one’s capability to organize and execute the courses of action required to produce given attainments’ [Citation8]. The first of such PROM developed for older people on falls is the Falls Efficacy Scale (FES) [Citation9]. FES was operationalized to measure fear of falling as this type of fear was identified to be ‘low perceived self-efficacy or confidence at avoiding falls’ [Citation9]. Over the last three decades, numerous PROMs have been further developed or modified from the original FES to measure various latent constructs including falls efficacy, balance confidence and fear of falling. Some of these PROMs were the modified Falls Efficacy Scale [Citation10], Activities-specific Balance Confidence Scale (ABC) [Citation11], Falls Efficacy Scale International (FES-I) [Citation12], Iconographical Falls Efficacy Scale (Icon-FES) [Citation13] and the CONFBal scale of balance confidence [Citation14].
Two previous systematic reviews, which aimed to recommend a ‘gold standard’ falls efficacy instrument, reported inconsistencies within and across studies in providing evidence of the validity in the different instruments [Citation15,Citation16]. The interchangeable interpretations between the various fall-related psychological constructs of falls efficacy, balance confidence and fear of falling have led to clinicians and researchers using different PROMs to measure the different constructs, and this may be conceptually problematic [Citation17]. A recently conducted systematic review on 18 PROMs for falls-related self-efficacy revealed that different items in the PROMs were related to the judgment of one’s abilities to manage different fall-related circumstances [Citation18]. The PROMs measuring falls efficacy, such as the Perceived Ability to Manage the Risk of Falls, or Actual Falls [Citation19] and the Perceived Ability to Prevent and Manage Fall Risk scale [Citation20], had a list of items which were deemed expansive, concerning the perceived ability of individuals on performing activities without losing balance, preventing falls, falling safely or getting up or helped up from the floor. This suggested that falls efficacy may be better defined as the perceived ability to manage the threat of fall [Citation21]. The PROMs used for balance confidence, such as the Activities-specific Balance Confidence Scale [Citation11], the CONFBal scale of balance confidence [Citation14], and the modified Falls Efficacy Scale [Citation10], had items focusing on the perceived ability of individual to performing ADLs without losing balance or falling. This implied that balance confidence is a subset domain of falls efficacy. Fear of falling which relates to a lasting concern about falling that leads to an individual avoiding activities that he/she remains capable of performing [Citation22], differentiates itself from the self-efficacy construct [Citation7]. Some common PROMs used by clinicians for measuring fear of falling would include the Survey of Activities and Fear of Falling in the Elderly [Citation23], the Fear of Falling measure [Citation24], the Falls Efficacy Scale-International [Citation12] and the Iconographical Falls Efficacy Scale [Citation13].
Bandura [Citation25] viewed that a ‘one-measure fits all’ approach toward understanding falls efficacy would provide little or no relevance toward understanding the agency of older people to manage falls. This suggested that different measures reflecting a range of circumstances surrounding falls would be needed. An appropriately constructed PROM on specific domains of falls efficacy would facilitate a greater understanding amongst clinicians and researchers of the personal effectiveness in older people to deal with falls. Balance recovery is a crucial rehabilitation outcome given that most falls were related to different types of perturbations [Citation26]. Stevens and colleagues [Citation27] had reported that 68.5% of falls were caused by ‘lost balance, unsteady or wobbly’, ‘trip, caught foot, clumsy or tangled feet’ and ‘slip’. To successfully arrest a fall, the individual will need to effectively and efficiently execute various change-in-support maneuvers such as reach-to-grasp or compensatory stepping, to recover balance in response to a balance perturbation [Citation26,Citation28,Citation29]. Clinicians have been focusing on training the reactive ability in older people to avoid a fall by using perturbation-based training to simulate a slip, a trip or a loss of balance for the older adults to train this skill. [Citation30]. This mode of practice aims to intentionally cause the individual to lose balance during task or activity performance for the individual to catch oneself through a progressive, graded perturbation intensity [Citation31]. The goal of the rehabilitation intervention is to improve reactive balance recovery abilities using change-in-support maneuvers to restore equilibrium, which contrast itself from conventional balance training that concentrates predominantly on fixed support strategies in keeping balance.
Many PROMs on falls efficacy and balance confidence have been conventionally interpreted conceptually to measure the perceived ability to perform varying activities without losing balance [Citation32]. For example, the instructions from FES direct the respondent to answer, ‘How confident are you that you do the following activities without falling?’ [Citation9] or the question from the ABC, which asks the respondent ‘How confident are you that you will not lose your balance or become unsteady when you…’ [Citation11]. There has been an absence of a PROM that measures perceived ability to recover one’s balance from perturbations such as a slip, a trip, or a loss of balance caused by volitional movements [Citation18,Citation33]. These issues have led to the development of a newly developed PROM to measure balance confidence in community-dwelling older adults, known as the scale of Balance Recovery Confidence (BRC). Presently, the psychometric properties of the BRC are unknown. The psychometric properties of the BRC should be examined as well as to understand its relationship with other falls-related psychological concerns such as balance confidence, fear of falling and physical performance in community-dwelling older adults.
Study aim and objectives
This protocol aims to outline the intended approach to the first evaluation of BRC’s psychometric properties. There are several measurement properties such as unidimensionality, validity (to what extent does the instrument measure the construct it purports to measure) and reliability (the degree to which measurement is free from error) of the PROM that is needed to be studied [Citation34]. This psychometric validation aims to provide the evidence that the PROM can be purposefully used in practice, given that rigorous methods have been applied for the development and validation of the BRC. For the study, balance recovery confidence is defined as the perceived ability to recover one’s balance from perturbations, such as a slip, a trip, or a loss of balance that can occur in common, everyday activities. This focus will leave little ambiguity about precisely what is being measured. The resulting questionnaire is intended to be approximately 20 questions and should not take longer than 10 min to complete. The instrument is not intended to be used as a diagnostic tool of impaired specific balance recovery mechanisms. The BRC allows clinicians and researchers to quantifiably determine the balance recovery confidence in older adults and use the scale as a conduit for understanding older people’s perspectives when encountering different perturbations during their daily activities.
The objectives are to:
To evaluate the measurement properties of the BRC, i.e. unidimensionality, acceptability, targeting, scaling assumptions and reliability using Classical Test Theory (CTT) and Rasch measurement theory (RMT) in the Singapore community-dwelling older adults.
To assess the construct validity of the refined BRC against commonly used PROMs and performance measures in the Singapore community-dwelling older adults.
To refine the items, response categories, and scale structure of the BRC using Rasch measurement theory in an English-speaking sample of community-dwelling older adults in Singapore.
Methods and analysis
This study protocol is a prospective validation study conducted to assess the psychometric properties of a newly-developed PROM. The study is proposed under Bandura’s guide to developing self-efficacy scales [Citation25] and uses the procedures recommended by De Vet and colleagues [Citation34] to develop a PROM. This approach provides evidence for developing a PROM that measures the construct that is intended to be measured and provide evidence of its use as an outcome measure in clinical practice and research trials.
Development of the BRC
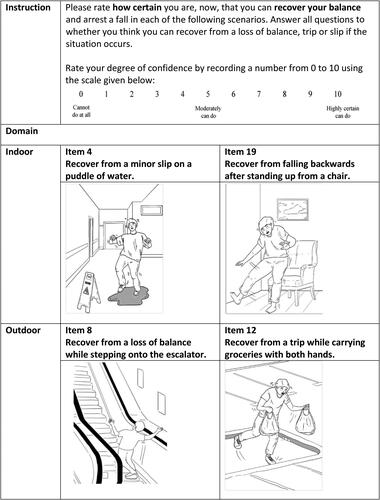
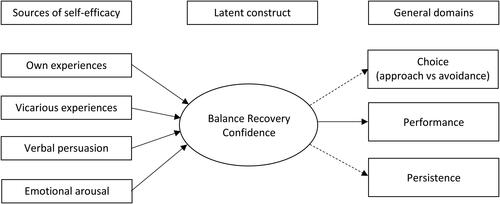
The BRC was developed iteratively with the following stages: concept identification, concept elicitation, pilot testing for instrument refinement and instrument validation [Citation35,Citation36]. The balance recovery concept had been previously identified through literature review, a systematic review conducted on falls efficacy related instruments for community-dwelling older adults [Citation18] and a feasibility study was done to establish that the balance recovery concept was relatable with the target population [Citation35]. Construction of BRC’s items was completed with twelve community-dwelling older adults, aligning to the reflective conceptual model of the instrument (). The preliminary BRC was pilot tested using Delphi with a new group of community-dwelling older adults and an international panel of medical and healthcare professionals. The content was refined accordingly to the feedback given by both panels of experts to meet an acceptable level of content validity. Exemplar items are presented in .
Figure 1. The conceptual framework of the PROM that measures balance recovery confidence (BRC). The BRFES's conceptual framework has been developed and refined based on the literature from Bandura's self-efficacy concept, Maki's change-in-support paradigm, the definition of a near fall and the systematic review conducted (Bandura, 1977; Maidan et al., 2014; Maki & McIlroy, 1997; Soh, Lane, Xu, Gleeson, et al., 2020).
Psychometric evaluation of the BRC
Assessing unidimensionality
The unidimensionality of the BRC to measure balance recovery confidence needs to be determined for the scoring of items (i.e. the certainty to recover the balance across different situations is because of their balance recovery confidence). The structural validity is defined as ‘the degree to which the scores of a measurement instrument are an adequate reflection of the dimensionality of the construct to be measured’ [Citation37]. The understanding of the structural validity will give evidence that the BRC adequately reflects the dimensionality of the balance recovery confidence construct in community-dwelling older adults.
Assessing acceptability, targeting, scaling assumptions and reliability
Acceptability refers to the questions of whether or not respondents would be willing to complete the PROM [Citation34]. Acceptability will be informed through data completeness (i.e. missing or incomplete data for items and sample). Data completeness will establish the extent to which scale items are scored, and total scores can be computed. Targeting may be defined as ‘the extent to which the range of the variable measured by the scale matches the range of the latent variable in the study sample [Citation38]. Targeting will be assessed on the ability of the BRC to span the entire scale range, skewness, and the floor and ceiling effects [Citation34]. The examination of scaling assumptions assesses the legitimacy to group items into a scale to produce a scale score [Citation39]. Reliability is defined as ‘the degree to which the measurement is free from measurement error’ [Citation34]. The reliability of the BRC will be assessed for internal consistency reliability and test-retest reliability. The internal consistency reliability establishes the inter-relatedness among items and is an assessment of the unidimensionality of a scale or subscale. The test-retest reliability evaluates the scores remaining the same for repeated measurements over time for patients who have not changed [Citation34].
Assessing the construct validity
Construct validity may be defined as the extent to which the scores of an instrument are a valid measure of the latent construct [Citation34]. The construct validity of the BRC will be assessed by applying criteria specified by the COSMIN initiative. The COSMIN specifies that construct validity may be assessed by testing a priori hypotheses based on the literature and the experience of the study team [Citation40]. The construct validity of the BRC will be assessed by the degree to which the sum score of the BRC is consistent with predefined hypotheses regarding the relationship between the BRC and the other measures. Six hypotheses have been formulated listed in .
Table 1. Hypotheses for construct validity.
Assessing the items, response categories and scale structure
The item fit refers to the degree of mismatch between the pattern of the actual observed responses, and the Rasch modeled expectations [Citation34]. Specifically, whether the pattern for each item across persons investigated fits to the Rasch measurement model. The response categories of the BRC (i.e. the number of categories and their definitions) will be evaluated whether the options are sufficient or should be adjusted to provide better coverage of the latent construct of balance recovery confidence. The scale structure will be explored whether the relative distribution of items matching the range of the respondents’ latent trait.
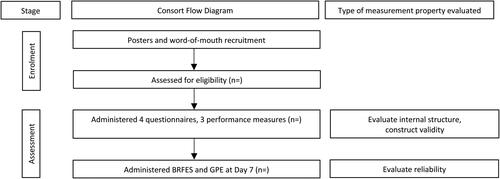
Recruitment and data collection
The participants' eligibility criteria are presented in . Recruitment will be done through posters dissemination and word-of-mouth recommendations through Singapore Institute of Technology (SIT) Health and community partners. Interested participants will be briefed about the research by a team member. Consent will be obtained when the older adult meets the eligibility criteria and has decided to participate in the study. All participants will complete a self-reported demographic questionnaire, four questionnaires which are the BRC [Citation41], ABC [Citation11], FES-I [Citation12], Late-Life Function and Disability Instrument-Function (LLFDI-F) [Citation42] and three performance measures: Jamar hand strength dynamometer [Citation43], 30-second chair stand test [Citation44] and Mini BESTest [Citation45] (). After seven days, participants will be asked to complete the BRC, and the Global Perceived Effect (GPE) scale [Citation46] () which will be used to ensure participants’ perception of their abilities remained unchanged during the seven days. The time interval of 7-day had been reported to be sufficient to minimize recall bias [Citation47]. Participants will be asked if they have had experienced a fall, near-fall, or encountered any incident that might affect their balance recovery ability over the past seven days. The procedure is reflected in the CONSORT flow diagram (). All participants will be coded with a unique identifier generated by an online code generator, and no personal identifiable information will be retained by the study team.
Table 2. Study eligibility criteria for recruitment of participants.
Table 3. List of outcome measures used in the study.
Sample size
The sample size is determined at 200 based on the recommendations made by Cappelleri and colleagues [Citation48] and De Vet and colleagues [Citation34]. The determination of sample sizes in studies of PROM validation is, in part, dependent on the properties of the scale itself. The minimum sample size is calculated at four to ten participants per item of the scale, but 100 participants is an absolute minimum for field testing [Citation34]. BRC contains 19-item, which implied that the minimum number of participants is ranged between 76 to 190. For classical test theory (CTT) measurement, an appropriate sample size provides rigorous quantitative analyses of standard errors. For the one-parameter Rasch model polytomous items analysis (RA), the item difficulty (and person measure) calibration can be evaluated to be within one logit of a stable value with 95% confidence [Citation49] The sample size of 200 accommodates a dropout rate of up to 50%, would allow the psychometric properties of the newly developed scale to be adequately assessed with two measurement theories.
Statistical analysis
Quantitative data will be analyzed and interpreted through two measurement test theories using IBM SPSS Statistic V.26.0 (for CTT) and Winsteps V.4.5.0 (for RMT). CTT is a traditional quantitative approach to test the validity and reliability of a scale based on its items [Citation48]. This approach is based on the assumption that every observed score is a function of an individual’s true score and random error [Citation50]. To supplement evaluating the measurement instrument using CTT, RA is employed to understand the probability of a person's level on an item is a function of the person's ability and of the difficulty of the item. RA evaluates a scale against a mathematical measurement model and analyses the scale at the level of each item, and each person [Citation51]. CTT focuses on the total score of a measure, whereas RA targets more specifically on the characteristics of individual items. RA will allow developers to establish whether an item’s response scale is functioning as expected and, if not, suggest improvements.
Various psychometric properties are assessed using the CTT and the RMT. Factor analysis will be undertaken to assess the structural validity of the BRC and establish its unidimensionality. The acceptability of the BRC will be established by the percentage of missing data for each item and the percentage of people for whom a PROM score can be computed. The amount of missing item-level data less than 5% missing will be considered acceptable. Targeting is assessed by the score distribution, including skew of scale scores and presence of floor and ceiling effects through item-level response descriptive statistics. A low floor and ceiling effects will be defined as <15% of the sample [Citation34]. The Rasch model will empirically demonstrate how respondents use the BRC’s rating scale informing future iterations of the BRC to ensure it yields high-quality data [Citation51]. Tests of scaling assumptions examine item-total correlations, mean scores and SD. When checking homogeneity of the LEQ-CI’s scales, the heuristic that items should correlate with the total score above 0.20 will be applied. Item-total correlations will be calculated using the Pearson product-moment correlation. The internal consistency reliability of the BRC will be assessed by calculating inter-item and item-total correlations and Cronbach’s alpha. The person separation index (PSI) will estimate the spread or separation of the person on the measured variable [Citation51]. A PSI > 0.7 will be considered an adequate measure of reliability. Test-retest reliability of the total score will be assessed using the intraclass correlation coefficient (ICC). As this is the first psychometric study of BRC, weighted Cohen's κ values will be calculated to assess test-retest reliability at the item level. The scores are expected to remain stable with a high intraclass correlation of 0.80 hypothesized. The construct validity of the BRC will be evaluated with the different outcome measures using Pearson’s correlation coefficient. The item fit of actual observed response to Rasch model will be assessed by examining item infit and outfit statistics [Citation51]. Mean square standardized residual (MNSQ) within the 0.5-1.5 range considered acceptable for productive measurement. Mean square values less than 0.5 indicate overfit (i.e. the items are too predictable relative to the Rasch model), while mean square values greater than 1.5 are indicative of too much noise (randomness) relative to the Rasch model [Citation51]. The response category order will be assessed using the Rasch probability curves, examining the data for category disordering and threshold disordering [Citation49]. The examination will indicate whether the response options selected are adequate or should be adjusted to provide better coverage of the latent trait, justifying whether the scale structure should be adjusted or sufficiently constructed.
Discussion
There is no existing PROM that measures balance recovery confidence in community-dwelling older adults. BRC aims to be meaningfully used in falls rehabilitation, especially in work focusing on improving the balance control of older adults. This protocol describes the rationale, design and methodology of developing BRC based on well-established international guidelines for its purposeful use [Citation34].
The results of this study will provide evidence of a systematic approach toward the validation of a PROM. If the instrument is found to show good psychometric properties, BRC will be a useful outcome measure of balance recovery confidence in community-dwelling older adults. The study may illuminate the necessary refinement of the BRC, which can further strengthen the justification of its purpose. This inaugural study aims to provide necessary evidence of a PROM to be accepted by different stakeholders, including healthcare professionals and community-dwelling older adults in the work of falls rehabilitation.
Disclaimer statements
All authors have made substantial contributions to the article. SS, JL and CW conceived the study. SS wrote the protocol and this manuscript. JL, CW and NG provided critical review of the protocol and this manuscript. TX, FR, TY, BS provided support of the project conducted in Singapore. All authors read and approved the final manuscript.
Ethics approval
Ethical consent for the study has been granted by Queen Margaret University [#REP 0220] and Singapore Institute of Technology [#2020098].
Acknowledgments
The authors would like to thank the older people and healthcare professionals who participated in the different stages of developing the BRC. They would also like to acknowledge the assistance of community partners supporting this project. We would like to express our appreciation to Ms Nina Neo from Singapore Institute of Technology with the illustrations.
Disclosure statement
All authors declare that they have no conflict of interest.
Additional information
Notes on contributors
Shawn Leng-Hsien Soh
Shawn Leng-Hsien Soh is a senior lecturer in health and social sciences cluster at Singapore Institute of Technology. Shawn is a PhD candidate at Queen Margaret University. Shawn has a BSc in physiotherapy and MPT in manipulative physiotherapy. Research interests are falls efficacy, patient-reported outcome measures and balance-related rehabilitation.
Judith Lane
Judith Lane is a senior lecturer in dietetics, nutrition and biological sciences, physiotherapy, podiatry and radiography division at Queen Margaret University. Dr Lane has a MSc in Bioengineering, MSc in Professional and Higher Education and Ph.D. Research interests include orthopedic research, rehabilitation, patient satisfaction.
Nigel Gleeson
Nigel Gleeson is a professor of rehabilitation sciences at Queen Margaret University. Prof Gleeson has a M.Phil. (Biomedical Science) and a Ph.D. in exercise physiology. Research interest include exercise physiology, neuromechanics and clinical rehabilitation.
Tianma Xu
Tianma Xu is an assistant professor in health and social sciences cluster at Singapore Institute of Technology. Dr Xu has a BSc (Occupational Therapy), MS in occupational therapy and Ph.D. in health sciences (Occupational Therapy). Research interests are falls prevention and management, telerehabilitation and stroke rehabilitation.
Fahria Bte Abdul Rahman
Fahria Bte Abdul Rahman is a principal physiotherapist in St Luke’s Hospital. Fahria has a Dip in physiotherapy and MS in physiotherapy. Research focuses on neurological rehabilitation, clinical and community rehabilitation.
Ting-Ting Yeh
Ting-Ting Yeh is an assistant profession in health and social sciences cluster at Singapore Institute of Technology. Dr Yeh has a BSc. (Physical Therapy) and Ph.D. in kinesiology. Research interest includes balance control, physical activity in older adults and stroke rehabilitation.
Benjamin Soon
Benjamin Soon is an associate profession in health and social sciences cluster at Singapore Institute of Technology. Dr Soon has a BSc. (Physiotherapy), M.Manip. Therapy and Ph.D. in physiotherapy. Research focus is on musculoskeletal rehabilitation, pain and manual therapy
Chee-Wee Tan
Chee-Wee Tan is a lecturer in the department of physiotherapy and paramedicine at Glasgow Caledonian University. Dr Tan has a BSc (Hons) in physiotherapy and Ph.D. in physiotherapy. Research interest includes symptom management, long-term conditions and health technologies in physiotherapy.
References
- Kyte DG, Calvert M, Van der Wees PJ, et al. An introduction to patient-reported outcome measures (PROMs) in physiotherapy. Physiotherapy. 2015;101(2):119–125.
- FDA. Guidance for industry patient-reported outcome measures: use in medical product development to support labeling claims. In: U.S. Department of Health and Human Services, editor. Rockville, MD: Office of Communication, Education, and Radiation Programs; 2009. [cited 2021 Apr 10]. Available from: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm
- CSP. Outcome and experience measures. UK: The Chartered Society of Physiotherapy; 2014. [cited 2021 Apr 10]. Available from: https://www.csp.org.uk/professional-clinical/research-evaluation/outcome-experience-measures
- Johnston BC, Patrick DL, Devji T, et al. Chapter 18: patient-reported outcomes. In: Cochrane handbook for systematic reviews of interventions version 60 (updated July 2019). London: Cochrane; 2019. [cited 2020 Nov 10]. Available from: http://www.training.cochrane.org/handbook
- Ioannidis JP, Greenland S, Hlatky MA, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383(9912):166–175.
- Mokkink LB, Prinsen CAC, Patrick DL, et al. COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1171–1179.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
- Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997.
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45(6):P239–43.
- Hill KD, Schwarz JA, Kalogeropoulos AJ, et al. Fear of falling revisited. Arch Phys Med Rehabil. 1996;77(10):1025–1029.
- Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–M34.
- Yardley L, Beyer N, Hauer K, et al. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34(6):614–619.
- Delbaere K, Smith ST, Lord SR. Development and initial validation of the Iconographical Falls Efficacy Scale. J Gerontol A Biol Sci Med Sci. 2011;66(6):674–680.
- Simpson JM, Worsfold C, Fisher KD, et al. The CONFbal scale: a measure of balance confidence-a key outcome of rehabilitation. Physiotherapy. 2009;95(2):103–109.
- Jørstad EC, Hauer K, Becker C, et al. Measuring the psychological outcomes of falling: a systematic review. J Am Geriatr Soc. 2005;53(3):501–510.
- Moore DS, Ellis R. Measurement of fall-related psychological constructs among independent-living older adults: a review of the research literature. Aging Ment Health. 2008;12(6):684–699.
- Hughes CC, Kneebone II, Jones F, et al. A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling older people. Int Psychogeriatr. 2015;27(7):1071–1087.
- Soh SLH, Lane J, Xu T, et al. Falls efficacy instruments for community-dwelling older adults: a COSMIN-based systematic review. BMC Geriatr. 2021;21(1):21.
- Tennstedt S, Howland J, Lachman M, et al. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B-Psychol. 1998;53B(6):P384–P392.
- Yoshikawa A, Smith ML. Mediating role of fall-related efficacy in a fall prevention program. Am J Health Behav. 2019;43(2):393–405.
- Payette MC, Bélanger C, Léveillé V, et al. Fall-related psychological concerns and anxiety among community-dwelling older adults: systematic review and meta-analysis. PLoS One. 2016;11(4):e0152848.
- Tinetti ME, Powell L. Fear of falling and low self-efficacy: a cause of dependence in elderly persons. J Gerontol. 1993;48(Special_Issue):35–38.
- Lachman ME, Howland J, Tennstedt S, et al. Fear of falling and activity restriction: the survey of activities and fear of falling in the Elderly (SAFFE). J Gerontol B-Psychol. 1998;53B(1):P43–P50.
- Velozo CA, Peterson EW. Developing meaningful fear of falling measures for community dwelling elderly. Am J Phys Med Rehabil. 2001;80(9):662–673.
- Bandura A. Guide for constructing self-efficacy scales. In: Pajares F, Urdan TC, editors. Self-efficacy beliefs of adolescents. Connecticut: Information Age Publishing; 2006.
- Tokur D, Grimmer M, Seyfarth A. Review of balance recovery in response to external perturbations during daily activities. Hum Mov Sci. 2020;69(102546):1–18.
- Stevens JA, Mahoney JE, Ehrenreich H. Circumstances and outcomes of falls among high risk community-dwelling older adults. Inj Epidemiol. 2014;1(5).
- Maki BE, McIlroy WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age Ageing. 2006;35 Suppl 2:ii12–ii18.
- Rinaldi NM, Lim J, Hamill J, et al. Walking combined with reach-to-grasp while crossing obstacles at different distances. Gait Posture. 2018;65:1–7.
- Shumway-Cook A, Woollacott MH. Motor control: translating research into clinical practice. 5th ed. Philadelphia, PA: Wolters Kluwer; 2017.
- Okubo Y, Sturnieks DL, Brodie MA, et al. Effect of reactive balance training involving repeated slips and trips on balance recovery among older adults: a blinded randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2019;74(9):1489–1496.
- Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health. 2011;23(1):3–23.
- Maki BE, Cheng KC, Mansfield A, et al. Preventing falls in older adults: new interventions to promote more effective change-in-support balance reactions. J Electromyogr Kinesiol. 2008;18(2):243–254.
- De Vet HCW, Terwee CB, Mokkink LB, et al. Measurement in medicine: a practical guide. Cambridge: Cambridge University Press; 2011.
- Soh SLH, Tan CW, Lane J, et al. Near-falls in Singapore community-dwelling older adults: a feasibility study . Pilot Feasibility Stud. 2021;7(1):25.
- Soh SLH, Lane J, Tan CW. Researcher as instrument: a critical reflection using nominal group technique for content development of a new patient-reported outcome measure. IPDJ. 2020;10(2):1–9.
- Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–745.
- Gorecki C, Brown JM, Cano S, et al. Development and validation of a new patient-reported outcome measure for patients with pressure ulcers: the PU-QOL instrument. Health Qual Life Outcomes. 2013;11(1):95.
- Streiner DL, Norman GR. Health measurement scales. A practical guide to their development and use. New York: Oxford University Press; 2008.
- Prinsen CAC, Mokkink LB, Bouter LM, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–1157.
- Soh SLH, Lane J, Xu TT, et al. Development of the balance recovery falls-efficacy scale for the community-dwelling older adults. 2019. [cited 2021 Apr 10]. Available from: https://clinicaltrials.gov/ct2/show/NCT04087551
- Haley SM, Jette AM, Coster WJ, et al. Late life function and disability instrument: II. Development and evaluation of the function component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M217–M222.
- Durkin K. Procedure for measuring hand grip strength using the jamar dynamometer. BRC Standard Operating Procedure. Southampton: NIHR Southampton Biomedical Research Centre; 2014. [cited 2021 Apr 10]. Available from: https://www.uhs.nhs.uk/Media/Southampton-Clinical-Research/Procedures/BRCProcedures/Procedure-for-measuring-gripstrength-using-the-JAMAR-dynamometer.pdf
- Centers for Disease Control and Prevention. 30-second chair stand assessment. Washington: U.S. Department of Health & Human Services; 2017. [cited 2021 Apr 10]. Available from: https://www.cdc.gov/steadi/pdf/STEADI-Assessment-30Sec-508.pdf
- Franchignoni F, Horak F, Godi M, et al. Using psychometric techniques to improve the Balance Evaluation Systems Test: the mini-BESTest. J Rehabil Med. 2010;42(4):323–331.
- Kamper SJ, Ostelo RW, Knol DJ, et al. Global perceived effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. J Clin Epidemiol. 2010;63(7):760–766.
- Devon HA, Block ME, Moyle-Wright P, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–164.
- Cappelleri JC, Jason Lundy J, Hays RD. Overview of classical test theory and item response theory for the quantitative assessment of items in developing patient-reported outcomes measures. Clin Ther. 2014;36(5):648–662.
- Linacre M. Sample size and item calibration [or person measure] stability. Rasch Meas Trans. 1994;7(4):328.
- Tractenberg RE. Classical and modern measurement theories, patient reports, and clinical outcomes. Contemp Clin Trials. 2010;31(1):1–3.
- Bond TG, Fox CM. Applying the rasch model: fundamental measurement in the human sciences. 3rd ed. New York: Routledge; 2015.