Abstract
Background
Stroke rehabilitation consists of restorative and adaptive approaches. Multiple adaptive approaches exist.
Aims/Objectives
The objective of this study was to develop a framework for categorising adaptive stroke rehabilitation interventions, based on underlying theory.
Material and Methods
We searched multiple databases to April 2020 to identify studies of interventions designed to improve participation in valued activities. We extracted the name of the intervention, underlying explicit or implicit theory, intervention elements, and anticipated outcomes. Using this information, we proposed distinct groups of interventions based on theoretical drivers.
Results
Twenty-nine adaptive interventions were examined in at least one of 77 studies. Underlying theories included Cognitive Learning Theory, Self-determination Theory, Social Cognitive Theory, adult learning theories, and Psychological Stress and Coping Theory. Three overarching theoretical drivers were identified: learning, motivation, and coping.
Conclusions
At least 29 adaptive approaches exist, but each appear to be based on one of three underlying theoretical drivers. Consideration of effectiveness of these approaches by theoretical driver could help indicate underlying mechanisms and essential elements of effective adaptive approaches.
Significance
Our framework is an important advance in understanding and evaluating adaptive approaches to stroke rehabilitation.
Introduction
The majority of people living with stroke experience persistent challenges with participation in valued activities and social roles [Citation1]. Stroke rehabilitation uses two broad types of interventions to address these challenges, restorative and adaptive [Citation2]. Restorative interventions are designed to remediate stroke-related impairment through normalising body structures and function. Adaptive interventions aim to optimise abilities to carry out important activities through adapting the environment or the approach to the activity. In this way, adaptive approaches promote engagement in valued activities and life roles despite impairment [Citation3].
Current stroke rehabilitation best practice guidelines provide specific recommendations for restorative interventions. For example, to improve upper extremity function named interventions, such as constraint induced movement therapy, are recommended [Citation4]. However, to improve engagement in valued activities and life roles, guidelines provide only general advice [Citation5], such as using collaborative goal setting and providing “targeted, individualized interventions”, without referring to specific named interventions. Clinicians reading such guidelines may be unaware that named adaptative interventions exist.
Numerous adaptive interventions to improve participation following stroke have been developed and evaluated. Two broad approaches appear predominant: metacognitive approaches and self-management approaches [Citation6,Citation7]. For example, Cognitive Orientation to daily Occupational Performance (CO-OP) is a metacognitive approach aimed at promoting improvement in the performance of personally identified, meaningful activities. The Bridges to Self-Management Program is a stroke-specific program based on self-management principles. Each of these interventions has been evaluated in at least one randomised controlled trial [Citation8,Citation9].
While metacognitive and self-management approaches differ with regards to described components and mechanisms of action, they share similar components of goal setting and action planning. Interventions based on a metacognitive approach help patients develop problem-solving strategies to address current and future challenges through learning to think about and analyse the performance problem they are experiencing, propose ways to solve the problem, plan actions to test out their solutions, and reflect on the results of these experiments to further refine performance [Citation10]. Interventions based on a self-management approach assist patients to live well with chronic health issues through developing a better understanding of their condition and its management, and enhancing self-efficacy or confidence in their abilities to find and enact solutions to challenges that arise in living with this chronic health condition [Citation11]. The degree to which current adaptive interventions are informed by each of these approaches, or whether other approaches exist, is not well understood. As well, while the general approach is often identified in the description of an intervention, the theory underlying the development of the intervention may be unclear.
Adaptive interventions are complex in nature [Citation12]. Progress in the science of complex interventions cannot be made without elucidating theoretical principles, hypothesised methods of action, associated treatment elements, and anticipated outcomes [Citation13]. A method of cataloguing adaptive interventions, which allows for comparison of underlying explicit or implicit theory, intervention components, and anticipated outcomes, would be useful. The objective of this scoping review was to develop a framework for adaptive stroke rehabilitation, with an initial focus on interventions guided by a metacognitive or self-management approach, two frequently used approaches [Citation6,Citation7]. The research questions included which named, adaptive interventions have been described and evaluated, what theories are explicitly or implicitly evoked in describing these interventions, what intervention elements are included, what outcomes are anticipated, and how can these interventions be best theoretically grouped.
Material and methods
We carried out a scoping review, following the Joanna Briggs Institute methodology [Citation14]. Details of the review are described in the published protocol [Citation15]. A systematic search for relevant literature from data base inception to 14 April 2020 was carried out in the following: Medline and Medline In-Process (via OVID), Embase Classic and Embase (via OVID), PsycINFO (via OVID), CINAHL (via EBSCOHost), and AARP AgeLine (via EBSCOHost). A supplemental search of OTSeeker and Physiotherapy Evidence Database (PEDro) was also performed.
The search strategy was developed in consultation with a library scientist (LS) to identify rehabilitation interventions to improve participation based on metacognitive or self-management approaches among adults who had experienced stroke. The search strategy was initially developed in Medline (Supplementary Table 1) and then adapted to the other databases. The search included a combination of terms related to the population (e.g. stroke, cerebrovascular accident, adult), concepts (e.g. metacognition, self-management, problem-solving), and the names of known interventions (e.g. Cognitive Orientation to daily Occupational Performance (CO-OP), Bridges Self-Management Program (Bridges SMP).
Eligible studies included those that examined interventions to improve participation globally or specifically. The intervention had to contain at least one element of metacognitive strategy training or self-management, including goal setting, strategy teaching, strategy development, problem-solving, attempting the activity, reflecting on the experience of attempting the activity, emotional support, or education [Citation7,Citation16]. In addition, the study must have included measurement of participation through tools that included specific activities identified by the stroke survivor (specific aspect of participation) or a generic set of activities (broad participation). Measures of participation accepted included broad stroke evaluations that incorporated aspects of body functions and focused evaluations that included one element of participation such as measures of instrumental activities of daily living or leisure. This was done to help us cast a wide net for potential interventions. There was no restriction on research methodology or language. When an intervention was identified during the search, other research articles dealing with that intervention were sought.
Potential studies were excluded if the intervention focused only on the provision of generic stroke education, reduction of a specific impairment such as cognition, or improved adherence to medical management. Studies with samples that included people experiencing non-stroke-related conditions and studies of children (<18 years) with stroke were also excluded.
The library scientist conducted the search in each database and uploaded the results into the web-based management software Covidence (Veritas Health Innovation, Melbourne, Australia) and duplicates were removed. Titles and abstracts were screened by two independent reviewers (AC, ME, DK) against the inclusion criteria. Potentially relevant papers were retrieved and assessed against the inclusion and exclusion criteria by two independent reviewers (ME and PD). Disagreements at each stage of the selection process were resolved by discussion between the reviewers and by a third reviewer (PM).
Data were extracted from included papers by two independent reviewers (NG-J and AC) using a data extraction table. A third reviewer (DK or ME) resolved discrepancies between the reviewers. The data extraction table was designed for the collection of data regarding the intervention name, theories identified or implied, and outcomes monitored. For each study, data were extracted from the introduction, intervention description, and discussion that identified or implied the theoretical basis of the intervention. This data included references to theories or theoretical concepts. Theories were considered implied if they were not named but references were made to key theorists. For example, self-efficacy theory was implied if Lorig, who developed a chronic disease self-management approach based on self-efficacy theory [Citation17], was referenced.
Based on the intervention description, information about elements of the intervention were extracted: goal setting preparation, goal setting, strategy development, experimentation, reflection on experimentation, emotional support, and education. Outcomes evaluated were also recorded.
Two authors (ME and DK) examined the interventions for commonalities related to theoretical orientation and mechanisms of action as suggested by the explicit or implied theories, components and outcomes measured. During this examination, they considered different logical groupings and selected the one they felt resulted in the most comprehensive yet succinct grouping. These findings were reviewed by the other authors.
Results
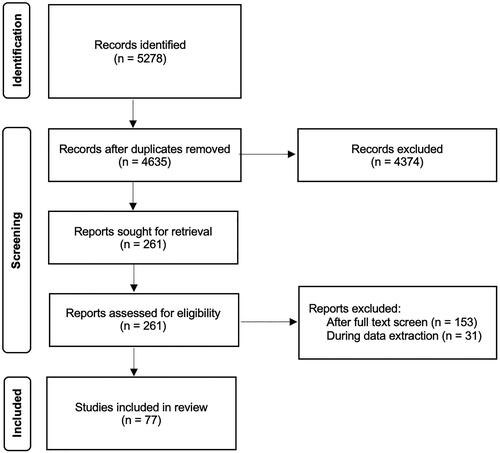
The search resulted in 5278 documents, of which 77 were included following the removal of duplicates and screening (). Twenty-nine different interventions were described in the included studies; eighteen of the interventions were evaluated in at least one randomised controlled trial (RCT) and eight were evaluated in at least two; theoretical foundations were explicitly named in 33 (42.9%) of the 77 studies ().
Table 1. Characteristics of the included studies according to theory groups.
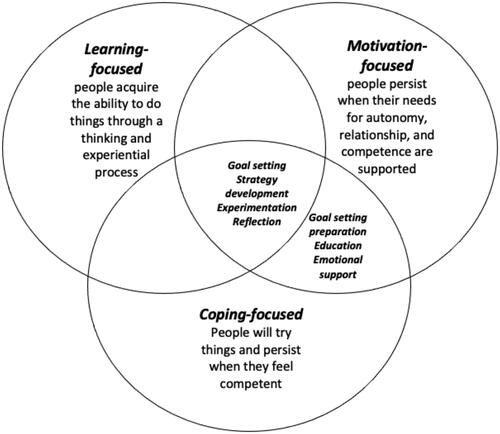
Theoretical orientation (explicit and implicit) and mechanisms of action, as suggested by these theories and the components and outcomes measured, were examined across interventions. Then, several possible logical groupings were proposed and considered. The grouping that best characterised succinct and meaningful relationships between the interventions related to how the intervention was seen to improve participation. This was termed the overarching theoretical driver – that is, the driver that primarily explained the relationship between the intervention and enhanced participation. Three overarching theoretical drivers were identified: learning, motivation, and coping (). The greatest number of named interventions were coping-driven (16 interventions, 44 studies), followed by motivation-driven (8 interventions, 13 studies), and learning-driven (5 interventions, 20 studies) ().
The theories guiding learning-driven interventions were Learning Theory and Cognitive Learning Theory. Intimately linked, these theories posit that people acquire the ability to do things through a thinking and experiential process (metacognition), that begins with setting a goal, and proceeds through steps of planning a strategy to achieve the goal, experimenting with this strategy, and then evaluating the results [Citation92]. Learning-driven interventions, therefore, would be expected to include elements that focus attention (goal-setting preparation, goal setting), promote thinking through the task such as mental imagery or use of a problem-solving framework, and application or testing of plans and reflection on the results. In study descriptions of learning-driven interventions, at least 75% of the intervention descriptions included goal setting, strategy development, experimentation, and reflection (). One intervention, Activating Physiotherapy, was included within the learning approaches because the authors stated it used metacognition. However, the intervention did not contain any metacognitive elements.
Table 2. Number of studies evaluating the self-management components.
Learning-driven interventions would not necessarily be expected to include education (except for education related to metacognition) or emotional support. Just over half (11 or 55.0%) of the learning approaches included education, while two (10.0%) of the interventions included emotional support ().
Specific participation was assessed in seven of 20 (35.0%) of the learning-driven intervention studies and broad participation was assessed in 8 (40.0%). Cognition and upper extremity function were also frequently tested outcomes (9 studies each, 45.0%). Mobility, depression, and quality of life were included less frequently as potential outcomes (Supplementary Table 2).
The theories guiding motivation-driven interventions included Self-determination Theory, Social Cognitive Theory, and adult learning theories. Self-determination Theory [Citation93] proposes that people will persist in their occupations in the face of challenges when their primary needs for autonomy, relationship, and competence are being met. Interventions leverage motivational forces through working towards valued goals while creating a relationship of trust, supporting autonomy, and encouraging the development of competence. Motivational forces support persistence in problem-solving and experimentation required to improve engagement in valued activities and social roles. Self-determination theory directs therapists to support autonomy (goal setting preparation, goal setting, strategy development, experimentation), competency (strategy development, experimentation, reflection, education) and relatedness (emotional support).
Social Cognitive Theory predicts that people will try to do activities they feel competent to perform. A sense of self-efficacy arises most powerfully from successful experimentation, but also from observation of peers, encouragement, and bodily sensations [Citation94]. Social Cognitive Theory was referred to explicitly or implicitly in both the motivation- and coping-driven interventions. In motivation-driven intervention application of Social Cognitive Theory, improved self-efficacy is a by-product of incremental success; improved self-efficacy supports further persistence in problem-solving through the expectation of success. Social Cognitive Theory directs therapists to include opportunities to experience mastery through practice under conditions that promote success (strategy development, experimentation), support self-evaluation of performance (reflection), allow learning from others’ experience (education), and promote monitoring of physiological states and provide verbal encouragement (emotional support).
Adult learning theories see patients as goal-directed learners interested in practical problems, who may change fundamental assumptions about their values during the learning process [Citation95]. In motivation-driven interventions, adult learning theories direct therapists to harness motivation by focusing on practical problems of high personal interest to the patient. Interventions are designed to ensure the relevance of what is to be learned (goal-setting preparation, goal setting), incorporate previous learning and experiences (strategy development), and promote reflection on experience and how it has led to changed assumptions (reflection).
Motivation-driven interventions would be expected to include elements to ensure activities targeted are of vital interest to the patient while promoting autonomy (goal-setting preparation), supporting competence (strategy development, experimentation, reflection) and developing a relationship of trust (emotional support). In the study descriptions of motivation-driven interventions, goal setting preparation, goal setting and strategy development were included in all intervention descriptions and experimentation was included in all but one. Emotional support was seen mainly in those motivation-focused interventions that named Self-determination Theory as part of their theoretical base. Education was included in all but one of the interventions ().
Specific participation was an outcome in 6 of the 13 motivation-driven intervention studies (46.2%), with broad participation assessed in 8 (61.5%). Cognition was assessed in 4 (30.8%). Upper extremity function was not assessed in any study. Mobility was included as an outcome in 2 studies (15.3%). Depression and quality of life were assessed in 4 studies (30.8%) (Supplementary Table 2).
The theories guiding coping-driven interventions were Social Cognitive Theory and Psychological Stress and Coping Theory. When applied to coping-driving interventions, Social Cognitive Theory proposes an improvement in self-efficacy as the dominant mechanism of action. That is, intervention helps patients strengthen their belief that they can cope with the effects of illness and carry out their valued activities and social roles. This strengthened belief supports persistence in problem-solving and experimentation required to improve engagement in valued activities and social roles [Citation94].
Psychological Stress and Coping theory posit that successful coping with difficult situations entails accurate assessment of threats and the use of active strategies, rather than passive strategies, to mobilise appropriate resources. Interventions informed by Psychological Stress and Coping theory see the mechanism of action as lessening gaps between threats and perceived resources, which leads to decreased stress and more effective coping with problems in day-to-day life [Citation96].
Coping-driven interventions would be expected to include elements that improve self-efficacy (goal setting, strategy-development, experimentation, reflection) and the ability to evaluate and respond to threats presented when trying to participate in valued activities despite impairment (education, emotional support). The majority (53-69%) of coping-driven intervention descriptions included goal setting, strategy development, experimentation, and reflection. Over half of the descriptions included education and approximately one-third included emotional support ().
In the studies of coping-driven interventions, specific participation was an outcome in 2 of the 44 intervention studies (4.5%) with broad participation assessed in 11 (25.0%). Cognition was assessed in 12 (27.2%). Upper extremity function was assessed in 3 studies (6.8%). Mobility was included as an outcome in 9 studies (20.5%). Depression was assessed in 17 (38.6%) studies and quality of life were assessed in 18 (40.9%) (Supplementary Table 2).
Discussion
Adaptive approaches to improving participation in valued activities and social roles following stroke represent pragmatic efforts to help people return to satisfying lives despite persisting impairment. The Canadian Stroke Best Practice Recommendations state that there is Level A evidence that ‘People with stroke who experience difficulty engaging in leisure and other social activities should receive targeted therapeutic interventions and individualised plans for participation based on collaborative goal setting with their health-care team’ [Citation5]. However, no additional recommendations are made; this may lead therapists to incorrectly assume that no specific interventions exist. This scoping work uncovered 29 named interventions for improving engagement in valued activities and social roles; their components and mechanisms can be understood through one of three primary mechanisms: learning, motivation, or coping.
Learning- and motivation-driven interventions frequently shared the features of goal setting, strategy development, experimentation, and reflection. This was not surprising given both included learning theories as part of their theoretical bases. What distinguished learning and motivation-driven interventions was the latter’s inclusion of emotional support. Therapists may provide emotional support as part of learning-driven interventions, seeing this as something any good clinician would do to develop a therapeutic relationship [Citation97]. However, these interventions are based on cognitive motor learning theories, which do not refer to emotional support. The hazard here is that without a way to reason about its importance, such support could be seen as optional.
In educational research, emotional support is seen as influencing student selection of socially important goals. Emotional support also allows students to select ‘approach’ goals (goals that require risk-taking to develop a skill), rather than ‘avoidance’ goals (in which the aim is to avoid risk, thus limiting development of skills) [Citation98]. Future work should make explicit the role of emotional support in learning-driven interventions. If there is debate about its importance, learning-driven interventions should be evaluated with and without explicit inclusion of emotional support to determine whether it is indeed a necessary element. Alternately, researchers could consider the possibility of constructing and testing a combined learning- and motivation-driven approach to ensure adequate consideration of relational aspects of intervention.
Notably, there was significant overlap in terms of elements of all interventions regardless of theoretical driver. What differed were underlying ideas about mechanisms of action and related to these, anticipated outcomes. Goal setting, strategy development and experimentation were included in most coping-driven interventions, which seems reasonable given their focus on competency-building. However, coping-driven interventions focus on building competency to deal with stressors, whereas learning- and motivation-driven interventions focus on building competencies for participating in valued activities and social roles. It is not surprising then that studies of coping-driven interventions were less likely to include measures of specific participation. Further examination of coping-driven intervention protocols suggests that goal setting, strategy development, and experimentation regarding valued activities and social roles were minor components of the interventions. This is not surprising as the focus of these interventions was on decreasing stress and improving health management. Given this focus, coping-driven interventions may be less effective for promoting participation without additional sessions focused on patients’ specific valued activity goals [Citation99]. Oh and colleagues provide preliminary evidence of this assertion in their meta-analysis of self-management interventions with action components [Citation99].
Given its attention to the theory underlying intervention, this framework has both clinical and research relevance. While helping clinicians identify specific tested approaches to stroke rehabilitation, it can also help them consider the underlying theoretical approaches and what needs to be included in an intervention to ensure the appropriate use of theory. For example, the underlying theory of all interventions directs therapists to include goal setting, experimentation, and reflection. Finally, this framework can help ensure that team members providing the interventions have the necessary skills in the underlying components. For example, all of the interventions require expertise in helping people develop goals, a skill that is challenging for many rehabilitation providers [Citation100].
Substantial progress in the development of adaptive approaches will best occur when techniques are consistent with the underlying theory and reflect relevant changes as these theories advance. Researchers could use this framework to refine existing interventions, through modifications that create better theoretical consistency and incorporate new developments in the underlying theories. Notably, this framework could be used to better group interventions in systematic reviews and meta-analyses. Meta-analyses that group interventions by theoretical drivers may be helpful in identifying which specific types of interventions (learning-, motivation-, or coping-driven) best address participation outcomes. It appears that current reviews contain all three types of interventions. For example, when we examined three systematic reviews on self-management interventions [Citation99,Citation101,Citation102], we found the inclusion of interventions that could be better classified as learning- [Citation29] or motivation- [Citation41,Citation42,Citation44] driven rather than coping-driven.
There are three main limitations of this review. First, we may have missed participation-focused interventions during our literature search given our initial search focus on meta-cognitive and self-management approaches. There may be other named interventions with different theoretical drivers. Second, we note that the theoretical bases for interventions were explicitly stated less than half of the time. While we were careful in our identification of implicit theory, we may have made incorrect assumptions during this process. Finally, our results are based on the literature to mid-April 2020. While this is a limitation, we note that we were not attempting to calculate the current best estimates of the effects of these interventions. Rather, we were attempting to describe the theoretical orientations of these interventions. A recent search for randomised controlled trials of participation-focused interventions for people who have experienced stroke produced four additional studies. The interventions tested included self-management programs (coping-driven) [Citation103,Citation104] and CO-OP (learning-driven) [Citation105,Citation106], suggesting that our framework is applicable to more recent studies as well.
Despite these limitations, this study makes an important contribution to the literature. An excellent understanding of underlying mechanisms of action is critical in developing, evaluating, and refining complex interventions. Adaptive interventions are frequently delivered by inter-professional teams, increasing the need to be explicit and clear regarding theoretical underpinnings. Increasingly, investigators are mapping out the elements and theoretical connections of participation-directed interventions [Citation107]. By focusing on the underlying theoretical bases, the framework developed in this study provides an important starting point for a broad discussion of elements and mechanisms of action of interventions to improve participation in valued activities and social roles.
Supplemental Material
Download MS Word (117.3 KB)Disclosure statement
No potential competing interest was reported by the author(s).
Additional information
Funding
References
- Wolf T, Brey J, Baum C, et al. Activity participation differences between younger and older individuals with stroke. Brain Impair. 2012;13(1):16–23. doi: 10.1017/BrImp.2012.1.
- Reinkensmeyer D, Burdet E, Casadio M, et al. Computational neurorehabilitation: modeling plasticity and learning to predict recovery. J Neuroeng Rehab. 2016;13(1):42. doi: 10.1186/s12984-016-0148-3.
- Cheeran B, Cohen L, Dobkin B, et al. The future of restorative neurosciences in stroke: driving the translational research pipeline from basic science to rehabilitation of people after stroke. Neurorehabil Neural Repair. 2009;23(2):97–107. doi: 10.1177/1545968308326636.
- Teasell R, Salbach NM, Foley N, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part one: rehabilitation and recovery following stroke; 6th edition update 2019. Int J Stroke. 2020;15(7):763–788. doi: 10.1177/1747493019897843.
- Mountain A, Patrice Lindsay M, Teasell R, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part two: transitions and community participation following stroke. Int J Stroke. 2020;15(7):789–806. doi: 10.1177/1747493019897847.
- Kersey J, Hammel J, Baum C, et al. Effect of interventions on activity and participation outcomes for adults with brain injury: a scoping review. Brain Inj. 2022;36(1):21–31. doi: 10.1080/02699052.2022.2034043.
- Warner G, Packer T, Villeneuve M, et al. A systematic review of the effectiveness of stroke self-management programs for improving function and participation outcomes : self-management programs for stroke survivors. Disabil Rehabil. 2015;37(23):2141–2163. doi: 10.3109/09638288.2014.996674.
- Polatajko HJ, McEwen SE, Ryan JD, et al. Pilot randomized controlled trial investigating cognitive strategy use to improve goal performance after stroke. Am J Occup Ther. 2012;66(1):104–109. doi: 10.5014/ajot.2012.001784.
- Mckenna S, Jones F, Glenfield P, et al. Bridges self-management program for people with stroke in the community: a feasibility randomized controlled trial. Int J Stroke. 2015;10(5):697–704. doi: 10.1111/ijs.12195.
- Missiuna C, Mandich A, Polatajko H, et al. Cognitive orientation to daily occupational performance (CO-OP). Part. Phys. & Occup Ther Pediatr. 2001;20(2):69–81. doi: 10.1300/J006v20n02_05.
- Barlow J, Sturt J, Hearnshaw H. Self-management interventions for people with chronic conditions in primary care: examples from arthritis, asthma and diabetes. Health Educ J. 2002;61(4):365–378. doi: 10.1177/001789690206100408.
- Bernhardt J, Borschmann K, Boyd L, et al. Moving rehabilitation research forward: developing consensus statements for rehabilitation and recovery research. Int J Stroke. 2016;11(4):454–458. doi: 10.1177/1747493016643851.
- Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: medical research council guidance. BMJ. 2015;350(mar19 6):h1258–h1258. doi: 10.1136/bmj.h1258.
- Peters MDJ, Godfrey C, McInerney P, et al. Scoping Reviews. Joanna Briggs Inst Rev Man [Internet]. The Joanna Briggs Institute; 2017. Available from: https://reviewersmanual.joannabriggs.org/.
- Egan M, Kessler D, Duong P, et al. Participation-focused interventions for stroke rehabilitation: a scoping review protocol. JBI Evid Synth. 2020;18(12):2666–2672. doi: 10.11124/JBISRIR-D-19-00387.
- Skidmore ER, Holm MB, Whyte EM, et al. The feasibility of meta-cognitive strategy training in acute inpatient stroke rehabilitation: case report. Neuropsychol Rehabil. 2011;21(2):208–223. doi: 10.1080/09602011.2011.552559.
- Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01.
- Allen KAM, Dittmann KR, Hutter JA, et al. Implementing a shared decision-making and cognitive strategy-based intervention: knowledge user perspectives and recommendations. J Eval Clin Pract. 2020;26(2):575–581. doi: 10.1111/jep.13329.
- Song CS, Lee ON, Woo HS. Cognitive strategy on upper extremity function for stroke: a randomized controlled trials. Restor Neurol Neurosci. 2019;37(1):61–70. doi: 10.3233/RNN-180853.
- Boone AE, Wolf TJ, Engsberg JR. Combining virtual reality motor rehabilitation with cognitive strategy use in chronic stroke. Am Journ. 2019;73:1–9.
- Boone AE, Morgan KA, Engsberg JR. A new combined motor and cognitive strategy training intervention for stroke: stakeholder perceptions. Br J Occup Ther. 2017;80(12):726–734. doi: 10.1177/0308022617714748.
- Ahn S, Yoo E, Jung M, et al. Comparison of cognitive orientation to daily occupational performance and conventional occupational therapy on occupational performance in individuals with stroke: a randomized controlled trial. NeuroRehabilitation. 2017;40(3):285–292. doi: 10.3233/NRE-161416.
- Henshaw E, Polatajko H, McEwen S, et al. Cognitive approach to improving participation after stroke: two case studies. Am J Occup Ther. 2011;65(1):55–63. doi: 10.5014/ajot.2011.09010.
- McEwen SE, Polatajko HJ, Huijbregts MPJ, et al. Exploring a cognitive-based treatment approach to improve motor-based skill performance in chronic stroke results of three single case experiments. Brain Inj. 2009;23(13-14):1041–1053. doi: 10.3109/02699050903421107.
- McEwen SE, Polatajko HJ, Davis JA, et al. ‘There’s a real plan here, and I am responsible for that plan’: participant experiences with a novel cognitive-based treatment approach for adults living with chronic stroke. Disabil Rehabil. 2010;32:540–550.
- McEwen SE, Polatajko HJ, Huijbregts MPJ, et al. Inter-task transfer of meaningful, functional skills following a cognitive-based treatment: results of three multiple baseline design experiments in adults with chronic stroke. Neuropsychol Rehabil. 2010;20(4):541–561. doi: 10.1080/09602011003638194.
- McEwen SE, Polatajko H, Baum C, et al. Combined cognitive-strategy and task-specific training improves transfer to untrained activities in Sub-acute stroke: an exploratory randomized controlled trial. Neurorehabil Neural Repair. 2015;29(6):526–536. doi: 10.1177/1545968314558602.
- Poulin V, Korner-Bitensky N, Bherer L, et al. Comparison of two cognitive interventions for adults experiencing executive dysfunction post-stroke: a pilot study. Disabil Rehabil. 2017;39(1):1–13. doi: 10.3109/09638288.2015.1123303.
- Wolf TJ, Polatajko H, Baum C, et al. Combined cognitive-strategy and task-specific trainning affects cognition and upper-extremity function in subacute stroke: an exploratory randomized controlled trial. Am J Occup Ther. 2016;70:1–10.
- Richardson J, DePaul V, Officer A, et al. Development and evaluation of self-management and task-oriented approach to rehabilitation training (START) in the home: case report. Phys Ther. 2015;95(6):934–943. doi: 10.2522/ptj.20130617.
- Pyoria O, Talvitie U, Nyrkkö H, et al. The effect of two physiotherapy approaches on physical and cognitive functions and independent coping at home in stroke rehabilitation. A preliminary follow-up study. Disabil Rehabil. 2007;29(6):503–511. doi: 10.1080/09638280600902497.
- Levine B, Schweizer TA, O’Connor C, et al. Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Front Hum. 2011;5:1–9.
- Tornas S, Løvstad M, Solbakk AK, et al. Goal management training combined with external cuing as a means to improve emotional regulation, psychological functioning, and quality of life in patients with acquired brain injury: a randomized controlled trial. Arch Phys Med Rehabil. 2016;97(11):1841–1852.e3. doi: 10.1016/j.apmr.2016.06.014.
- Schweizer TA, Levine B, Rewilak D, et al. Rehabilitation of executive functioning after focal damage to the cerebellum. Neurorehabil Neural Repair. 2008;22(1):72–77. doi: 10.1177/1545968307305303.
- Ownsworth T. A metacognitive contextual approach for facilitating return to work following acquired brain injury: three descriptive case studies. Work. 2010;36(4):381–388. doi: 10.3233/WOR-2010-1041.
- Belliveau D, Belliveau I. Use of occupational performance coaching for stroke survivors (OPC-Stroke) in late rehabilitation: a descriptive case study. Open J Occup Ther. 2016;4: article 7.
- Kessler D, Ineza I, Patel H, et al. Occupational performance coaching adapted for stroke survivors (OPC-Stroke): a feasibility evaluation. Phys Occup Ther Geriatr. 2014;32(1):42–57. doi: 10.3109/02703181.2013.873845.
- Nott M, Wiseman L, Seymour T, et al. Stroke self-management and the role of self-efficacy. Disabil Rehabil. 2019;27:1–10.
- Kessler D, Egan M, Dubouloz CJ, et al. Occupational performance coaching for stroke survivors: a pilot randomized controlled trial. Am J Occup Ther. 2017;71:7103190020.
- Kessler D, Egan MY, Dubouloz CJ, et al. Occupational performance coaching for stroke survivors (OPC-Stroke): understanding of mechanisms of actions. Br J Occup Ther. 2018;81(6):326–337. doi: 10.1177/0308022618756001.
- Fu V, Weatherall M, Mcpherson K, et al. Taking charge after stroke: a randomized controlled trial of a person-centered, self-directed rehabilitation intervention. Int J Stroke. 2020;0:1–11.
- Harwood M, Weatherall M, Talemaitoga A, et al. Taking charge after stroke: promoting self-directed rehabilitation to improve quality of life – a randomized controlled trial. Clin Rehabil. 2012;26(6):493–501. doi: 10.1177/0269215511426017.
- Carlstedt E, Iwarsson S, Ståhl A, et al. BUS TRIPS—a self-management program for people with cognitive impairments after stroke. Int J Environ Res Public Health. 2017;14(11):1353. doi: 10.3390/ijerph14111353.
- Guidetti S, Ytterberg C. A randomised controlled trial of a client-centred self-care intervention after stroke: a longitudinal pilot study. Disabil Rehabil. 2011;33(6):494–503. doi: 10.3109/09638288.2010.498553.
- Northcott S, Burns K, Simpson A, et al. “Living with aphasia the best way I can”: a feasibility study exploring solution-focused brief therapy for people with aphasia. Folia Phoniatr Logop. 2015;67(3):156–167. doi: 10.1159/000439217.
- Escher AA, Amlani AM, Viani AM, et al. Occupational therapy in an intensive comprehensive aphasia program: performance and satisfaction outcomes. Am J Occup Ther. 2018;72:1–7.
- Sorensen SL, Pedersen SKS, Pallesen H. Social psychological mechanisms and processes in a novel, health professional-led, self-management intervention for older stroke individuals: a synthesis and phenomenological study. BMC Health Serv Res. 2019;19(1):320. doi: 10.1186/s12913-019-4150-x.
- Folden SL. Effect of a supportive-educative nursing intervention on older adults perceptions of self-care after a stroke. Rehabil Nurs. 1993;18(3):162–167. doi: 10.1002/j.2048-7940.1993.tb00745.x.
- Jones F, Gage H, Drummond A, et al. Feasibility study of an integrated stroke self-management programme: cluster-randomised controlled trial. BMJ Open. 2016;6(1):e008900. doi: 10.1136/bmjopen-2015-008900.
- Jones F, Pöstges H, Brimicombe L. Building bridges between healthcare professionals, patients and families: a coproduced and integrated approach to self-management support in stroke. NeuroRehabilitation. 2016;39(4):471–480. doi: 10.3233/NRE-161379.
- Jones F, Mckevitt C, Riazi A, et al. How is rehabilitation with and without an integrated self-management approach perceived by UK community-dwelling stroke survivors ? A qualitative process evaluation to explore implementation and contextual variations. BMJ Open. 2017;7(4):e014109. doi: 10.1136/bmjopen-2016-014109.
- Kulnik ST, Pöstges H, Brimicombe L, et al. Implementing an interprofessional model of self-management support across a community workforce a mixed-methods evaluation study. J Interprof Care. 2017;31(1):75–84. doi: 10.1080/13561820.2016.1246432.
- Singer B, Jones F, Lennon S. Adapting the bridges stroke. Int J Ther Rehabil. 2018;25(8):414–423. doi: 10.12968/ijtr.2018.25.8.414.
- Jones F, Livingstone E, Hawkes L. ‘Getting the balance between encouragement and taking over’—reflections on using a new stroke self-management programme. Physiother Res Int. 2013;18(2):91–99. doi: 10.1002/pri.1531.
- Cadilhac DA, Kilkenny MF, Srikanth V, et al. Do cognitive, language, or physical impairments affect participation in a trial of self-management programs for stroke? Int J Stroke. 2016;11(1):77–84. doi: 10.1177/1747493015607522.
- Cadilhac DA, Hoffmann S, Kilkenny M, et al. A phase II multicentered, single-blind, randomized, controlled trial of the stroke self-management program. Stroke. 2011;42(6):1673–1679. doi: 10.1161/STROKEAHA.110.601997.
- Lo SHS, Chang AM, Chau JPC. Stroke self-management support improves survivors’ self-efficacy and outcome expectation of self-management behaviors. Stroke. 2018;49(3):758–760. doi: 10.1161/STROKEAHA.117.019437.
- Damush TM, Ofner S, Yu Z, et al. Implementation of a stroke self-management program. Transl Behav Med. 2011;1(4):561–572. doi: 10.1007/s13142-011-0070-y.
- Kidd L, Lawrence M, Booth J, et al. Development and evaluation of a nurse-led tailored stroke self-management intervention. BMC Health Serv Res. 2015;15(1):359–370. doi: 10.1186/s12913-015-1021-y.
- Wolf TJ, Baum CM, Lee D, et al. The development of the improving participation after stroke self-management program (IPASS): an exploratory randomized clinical study. Top Stroke Rehabil. 2016;23(4):284–292. doi: 10.1080/10749357.2016.1155278.
- Lee D, Fischer H, Zera S, et al. Examining a participation-focused stroke self-management intervention in a day rehabilitation setting: a quasi-experimental pilot study. Top Stroke Rehabil. 2017;24(8):601–607. doi: 10.1080/10749357.2017.1375222.
- Lee D, Fischer H, Hammel J, et al. Improving participation after stroke: examining a stroke Self-Management intervention in day rehabilitation setting. Arch Phys Med Rehabil. 2016;97(12):e33. doi: 10.1016/j.apmr.2016.09.090.
- Lee D, Kravitt R, Hammel J, et al. Improving participation with self-management skills: qualitative evaluation of a stroke self- management program. Arch Phys Med Rehabil. 2017;98(10):e132. doi: 10.1016/j.apmr.2017.08.431.
- Tielemans NS, Visser-Meily JMA, Schepers VPM, et al. Effectiveness of the restore4stroke self-management intervention “plan ahead!”: a randomized controlled trial in stroke patients and partners. J Rehabil Med. 2015;47(10):901–909. doi: 10.2340/16501977-2020.
- van Mastrigt GAPG, van Eeden M, van Heugten CM, et al. A trial-based economic evaluation of the Restore4Stroke self-management intervention compared to an education-based intervention for stroke patients and their partners. BMC Health Serv Res. 2020;20(1):294. doi: 10.1186/s12913-020-05103-x.
- Tielemans NS, Schepers VPM, Visser-Meily JMA, et al. Process evaluation of the restore4stroke self-management intervention ‘plan ahead!’: a stroke-specific self-management intervention. Clin Rehabil. 2016;30(12):1175–1185. doi: 10.1177/0269215515620255.
- van Mierlo ML, van Heugten CM, Post MWM, et al. A longitudinal cohort study on quality of life in stroke patients and their partners: restore4Stroke cohort. Int J Stroke. 2014;9(1):148–154. doi: 10.1111/j.1747-4949.2012.00882.x.
- Hadidi NN, Lindquist R, Buckwalter K, et al. Feasibility of a pilot study of problem-solving therapy for stroke survivors. Rehabil Nurs. 2015;40(5):327–337. doi: 10.1002/rnj.148.
- Mikami K, Jorge RE, Moser DJ, et al. Prevention of poststroke apathy using escitalopram or problem-solving therapy. Am J Geriatr Psychiatry. 2013;21(9):855–862. doi: 10.1016/j.jagp.2012.07.003.
- Visser MM, Heijenbrok-Kal MH, Van’t Spijker A, et al. Problem-solving therapy during outpatient stroke rehabilitation improves coping and health-related quality of life: randomized controlled trial. Stroke. 2016;47(1):135–142. doi: 10.1161/STROKEAHA.115.010961.
- Chalmers C, Leathem J, Bennett S, et al. The efficacy of problem solving therapy to reduce post stroke emotional distress in younger (18–65) stroke survivors. Disabil Rehabil. 2019;41(7):753–762. doi: 10.1080/09638288.2017.1408707.
- Robinson RG, Jorge RE, Moser DJ, et al. Escitalopram and problem-solving therapy for prevention of poststroke depression: a randomized controlled trial. J Am Med Assoc. 2008;299(20):2391–2400. doi: 10.1001/jama.299.20.2391.
- Catalano T, Dickson P, Kendall E, et al. The perceived benefits of the chronic disease self-management program among participants with stroke: a qualitative study. Aust. J. Prim. Health. 2003;9(3):80–89. doi: 10.1071/PY03028.
- Hirsche RC, Williams B, Jones A, et al. Chronic disease self-management for individuals with stroke, multiple sclerosis and spinal cord injury. Disabil Rehabil. 2011;33(13-14):1136–1146. doi: 10.3109/09638288.2010.523103.
- Wolf TJ, Spiers MJ, Doherty M, et al. The effect of self-management education following mild stroke: an exploratory randomized controlled trial. Top Stroke Rehabil. 2017;24(5):345–352. doi: 10.1080/10749357.2017.1289687.
- Kendall E, Catalano T, Kuipers P, et al. Recovery following stroke: the role of self-management education. Soc Sci Med. 2007;64(3):735–746. doi: 10.1016/j.socscimed.2006.09.012.
- Huijbregts MPJ, Myers AM, Streiner D, et al. Implementation, process, and preliminary outcome evaluation of two community programs for persons with stroke and their care partners. Top Stroke Rehabil. 2008;15(5):503–520. doi: 10.1310/tsr1505-503.
- Huijbregts MPJ, McEwen S, Taylor D. Exploring the feasibility and efficacy of a telehealth stroke self-management programme: a pilot study. Physiother Can. 2009;61(4):210–220. doi: 10.3138/physio.61.4.210.
- Taylor DM, Cameron JI, Walsh L, et al. Exploring the feasibility of videoconference delivery of a self-management program to rurarl participants with stroke. Telemed J E Health. 2009;15(7):646–654. doi: 10.1089/tmj.2008.0165.
- Taylor DM, Stone SD, Huijbregts MP. Remote participants’ experiences with a group-based stroke self-management program using videoconference technology. Rural Remote Health. 2012;12:1–15.
- Johnston M, Bonetti D, Joice S, et al. Recovery from disability after stroke as a target for a behavioural intervention: results of a randomized controlled trial. Disabil Rehabil. 2007;29(14):1117–1127. doi: 10.1080/03323310600950411.
- Jones F, Mandy A, Partridge C. Changing self-efficacy in individuals following a first time stroke: preliminary study of a novel self-management intervention. Clin Rehabil. 2009;23(6):522–533. doi: 10.1177/0269215508101749.
- Joice S, Johnston M, Bonetti D, et al. Stroke survivors’ evaluations of a stroke workbook-based intervention designed to increase perceived control over recovery. Health Educ J. 2012;71(1):17–29. doi: 10.1177/0017896910383555.
- Alexopoulos GS, Wilkins VM, Marino P, et al. Ecosystem focused therapy in poststroke depression: a preliminary study. Int J Geriatr Psychiatry. 2012;27(10):1053–1060. doi: 10.1002/gps.2822.
- Claiborne N. Effectiveness of a care coordination model for stroke survivors: a randomized study. Health Soc Work. 2006;31(2):87–96. doi: 10.1093/hsw/31.2.87.
- Damush TM, Myers L, Anderson JA, et al. The effect of a locally adapted, secondary stroke risk factor self-management program on medication adherence among veterans with stroke/TIA. Transl Behav Med. 2016;6(3):457–468. doi: 10.1007/s13142-015-0348-6.
- Ertel K, Glymour M, Glass T, et al. Frailty modifies effectiveness of psychosocial intervention in recovery from stroke. Clin Rehabil. 2007;21(6):511–522. doi: 10.1177/0269215507078312.
- Hoffmann T, Ownsworth T, Eames S, et al. Evaluation of brief interventions for managing depression and anxiety symptoms during early discharge period after stroke: a pilot randomized controlled trial. Top Stroke Rehabil. 2015;22(2):116–126. doi: 10.1179/1074935714Z.0000000030.
- Marsden D, Quinn R, Pond N, et al. A multidisciplinary group programme in rural settings for community-dwelling chronic stroke survivors and their carers: a pilot randomized controlled trial. Clin Rehabil. 2010;24(4):328–341. doi: 10.1177/0269215509344268.
- Mawson S, Nasr N, Parker J, et al. Developing a personalised self-management system for post stroke rehabilitation; utilising a user-centred design methodology. Disabil Rehabil Assist Technol. 2014;9(6):521–528. doi: 10.3109/17483107.2013.840863.
- Sit JWH, Chair SY, Choi KC, et al. Do empowered stroke patients perform better at self-management and functional recovery after a stroke? A randomized controlled trial. Clin Interv Aging. 2016;11:1441–1450. doi: 10.2147/CIA.S109560.
- Mcewen SE, Huijbregts MPJ, Ryan JD, et al. Cognitive strategy use to enhance motor skill acquisition post-stroke: a critical review. Brain Inj. 2009;23(4):263–277. doi: 10.1080/02699050902788493.
- Ryan RM, Ryan WS, Di Domenico SI, et al. The nature and the conditions of human autonomy and flourishing: self-determination theory and basic psychological needs. In Ryan RM, editor. Oxford handb hum motiv. Oxford: Oxford University Press; 2019. p. 89–110.
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Heal. 1998;13(4):623–649. doi: 10.1080/08870449808407422.
- Collins J. Education techniques for lifelong learning: principles of adult learning. Radiographics. 2004;24(5):1483–1489. doi: 10.1148/rg.245045020.
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
- Bishop M, Kayes N, McPherson K. Understanding the therapeutic alliance in stroke rehabilitation. Disabil Rehabil. 2021;43(8):1074–1083. doi: 10.1080/09638288.2019.1651909.
- Martin A, Dowson M. Interpersonal relationships, motivation, engagement, and achievement: yields for theory, current issues, and educational practice. Rev Educ Res. 2009;79(1):327–365. doi: 10.3102/0034654308325583.
- Oh H, De Silva D, Toh Z, et al. The effectiveness of self-management interventions with action-taking components in improving health-related outcomes for adult stroke survivors: a systematic review and meta-analysis. Disabil Rehabil. 2021;10:1–16.
- Rosewilliam S, Roskell CA, Pandyan AD. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin Rehabil. 2011;25(6):501–514. doi: 10.1177/0269215510394467.
- Lau S, Judycki S, Mix M, et al. Theory-based self-management interventions for community-dwelling stroke survivors: a systematic review and meta-analysis. Am J Occup Ther. 2022;76(4):7603393030.
- Pedersen SKS, Sorensen SL, Stabel HH, et al. Effect of self-management support for elderly people post-stroke: a systematic review. Geriatrics. 2020;5:38.
- Forster A, Ozer S, Brindle R, et al. An intervention to support stroke survivors and their carers in the longer term: results of a cluster randomised controlled feasibility trial (LoTS2Care). Pilot Feasibility Stud. 2023;9(1):40. doi: 10.1186/s40814-023-01258-6.
- Te Ao B, Harwood M, Fu V, et al. Economic analysis of the “take charge” intervention for people following stroke: results from a randomised trial. Clin Rehabil. 2022;36(2):240–250. doi: 10.1177/02692155211040727.
- Dawson D, Anderson N, Binns M, et al. Strategy-training post-stroke via tele-rehabilitation: a pilot randomized controlled trial. Disabil Rehabil. 2022;14:1–10. doi: 10.1080/09638288.2022.2154397.
- Beit Yosef A, Jacobs J, Shames J, et al. A performance-based teleintervention for adults in the chronic stage after acquired brain injury: an exploratory pilot randomized controlled crossover study. Brain Sci. 2022;12(2):213. doi: 10.3390/brainsci12020213.
- Fraser T, Karon L, Lund A, et al. Examining components of community psychosocial stroke interventions using concept mapping. Scand J Occup Ther. 2022;29:325–336. doi: 10.1080/11038128.2021.1933172.