ABSTRACT
Background
the use of ultrasound in performing epidural anesthesia is in the rise. Many techniques are recently described in order to enhance the use of ultrasound in the performance of epidural anesthesia. Some new ultrasound devices like the Accuro device has been developed but the comparison between all the different techniques determining the advantage of each is not yet fully investigated. In this study we aim to compare the Accuro device as an example of ultrasound-assisted epidural catheter placement technique on one hand with the real-time ultrasound aided by the acoustic puncture-assisted device (APAD) to perform the epidural anesthesia on the other hand.
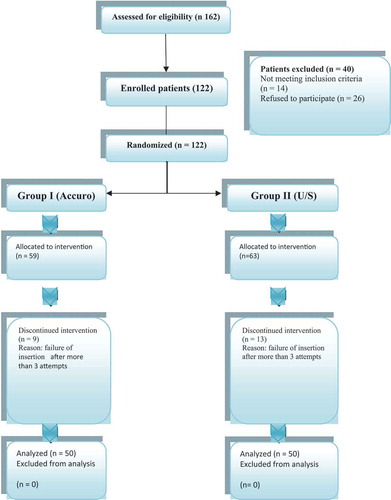
Methods
This study was performed on one hundred pregnant patients divided equally into two groups. Epidural anesthesia was performed in the first group using the Accuro device and in the second group using the (APAD) in combination with a real-time ultrasound.
Results
The first-time success rate was significantly higher in the second group 90% compared to 74%in the first group. The mean time to localize the epidural space and the total time of the procedure were significantly shorter in the second group.
Conclusion
the combination of real-time ultrasound with the APAD in performing epidural anesthesia resulted in easier and faster technique when compared with the new handheld pre-procedure Accuro ultrasound device.
1. Introduction
The ultrasound can be used in two ways to perform epidural anesthesia:
The ultrasound-assisted epidural anesthesia which involves performing a pre-procedural scan which helps to identify relevant landmarks and thus guides subsequent needle insertion.
The ultrasound guided epidural anesthesia Which is a real-time ultrasound-guided technique (where the needle is inserted under direct and continuous ultrasound visualization), on the other hand, remains an experimental and highly complex technique.
In order to improve the results of the real-time ultrasound guided technique and make it easier to be used while maintaining the advantage of the real-time imaging, we suggested a technique that uses two methods to perform the epidural anesthesia at the same time. This technique uses the ultrasound real time to guide the Tuohy needle through the anatomical track till it reaches the epidural space with combination of another technique the acoustic puncture-assisted device (APAD) to confirm the puncture of the ligamentum flavum.
Accuro is a new handheld ultrasound device used in ultrasound-assisted epidural anesthesia. It can detect the depth of the epidural space and give a three-dimensional image of the track of the epidural space.
The primary aim of this study is to compare two ultrasound techniques to perform epidural anesthesia. The first one is by using the handheld ultrasound device (Accuro). The other technique is using the real-time ultrasound to guide epidural catheter insertion combined with the acoustic puncture-assisted device to detect the loss of resistance when the Tuohy puncture the ligamentum flavum.
The secondary aim is to detect any difference in the incidence of complications associated with each technique.
2. Materials and methods
This study was performed on 100 pregnant patients in labor admitted to the obstetric department for normal vaginal delivery and requested epidural analgesia. .
One hundred patients was the calculated sample size to perform this study based on 98% success rate when using the conventional los of resistance technique; 80% power, the confidence interval (CI) of both techniques was 95% and the margin of error was assumed to be 30%.
The Ethics Committee of Alexandria Main University Hospitals reviewed the protocol then approved the study (no; 0304441). The study was registered prior to patient enrollment at ClinicalTrials.gov (Protocol ID: NCT04204070) the principal investigator: dr. Yasser Osman 12/18/2019.
All recruited patients in this study gave their written consent prior to admission to the examination room. In the examination room, all the patients were asked about their medical history and they were carefully examined. Routine laboratory investigations were ordered and reviewed.
A computer-generated program was used to randomize and divide the patients into two equal groups.
50 patients were assigned to the first group (Group I). The epidural catheter was inserted for those patients using the Accuro handheld ultrasound. (Accuro, Rivanna Medical, Charlottesville, VA) .
Figure 2. The wireless handheld ultrasound (Accuro, Rivanna medical, Charlottesville, VA) device investigated. The device has integrated software algorithm to depict bony landmarks and measure depth to spinous process and epidural space in real time. The image was downloaded from https://rivannamedical.com.

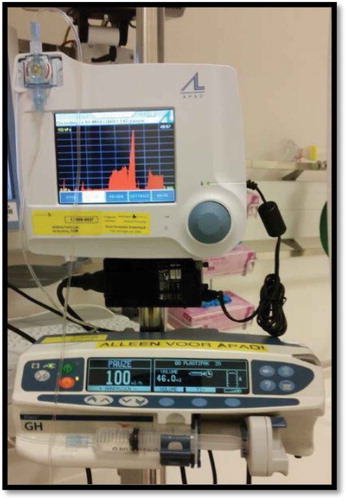
In the other group (Group II) consisting of another 50 patients the epidural catheter was inserted using the real-time ultrasound guided technique aided by the (APAD) .
Figure 3. The acoustic puncture-assisted device (APAD) (Medky equipment’s Schansestraat, the Netherlands).
Patients with precious baby or High-risk pregnancy were excluded from the study. Patients unwilling to participate in the study or having any contraindication for epidural analgesia were also excluded.
All study procedures were performed 30–45 min in advance of delivery in a room dedicated to the performance of regional block. All patients were connected to a monitor by three-lead electrocardiogram, non-invasive blood pressure, and pulse oximetry. Intravenous access was established, and the procedure was performed in both groups with the patient in the sitting position.
In group I the patient back was draped and sterilized then the Accuro device was placed in its sterile covering as instructed by the manufacturer (Rivanna Medical, Charlottesville, VA). The spine mode was selected and the Accuro was used in the transverse position to scan and detect the space, depth and direction of the epidural space. The Accuro locator needle guide was used to mark the skin. A Tuohy needle was inserted at the skin mark after giving local anesthesia, and loss of resistance technique using a glass syringe was used to identify the epidural space then an epidural catheter was inserted.
In group II a curved array probe (Sonosite Edge™ Bothell, WA, USA) 2–5 MHz was selected. After draping and positioning the patient, the probe was applied over the sacrum and scanning in a paramedian oblique sagittal plane was performed as described by Tran et al. The probe was then moved cephalad to count the intervertebral spaces till the chosen intervertebral level [Citation1,Citation2]. when an optimal view of the intevertebral space is reached the epidural anesthesia procedure using a real-time US Guided technique was performed. A 17 G Tuohy needle was carefully advanced to the interlaminar space, under real-time US guidance, until the tip pierces the ligamentum flavum. The Tuohy needle is connected to the APAD device through it’s transducer. The diaphragm of the transducer senses the pressure changes as the needle is advanced through the ligaments. A sensor in the device records change in pressure, this pressure changes is represented as audible acoustic signal and visual graphics displayed on the device monitor. This audible sound will help confirmation of the position of the Tuohy needle as it progresses under vision of the ultrasound and signals the loss of resistance when the tip of the needle pierces the ligamentum flavum.
The disposable kit of the APAD has two ends. One end is connected to a syringe filled with50 ml saline mounted on an infusion pump (delivers fluid at 50 ml/h.); the other end is the one connected to the epidural needle through the transducer. The proper function of the kit was tested before starting the procedure. First, the end of the tube that was connected to the needle was occluded by the thumb, and then the pressure is permitted to rise in the tubes. The rise in the pitch of acoustic signal was noted; the higher the pressure, the higher is the pitch tone. If the release of occlusion is followed by the sudden drop in the tone, then the device is cleared for the procedure.
The distance between the skin and the epidural space (EDS) was recorded by a research assistant. The assistant also recorded the number of attempts taken by the anesthetist to perform the epidural anesthesia, how many times did the anesthetist reposition the epidural needle either in the same space or in different space, the epidural space localization time (it is defined as time taken in seconds from skin puncture until the Tuohy needle pierce the ligamentum flavum and successfully reach the EDS).the total procedure time (time in seconds from the moment the patient is fully draped and in the proper sitting position till the end of insertion of the epidural catheter). Complications during the procedure were recorded. One attempt is defined as inserting the needle in the patients back till it is removed completely whether or not it has reached the epidural space.
In both groups, a 3 ml test dose of 2% lignocaine with epinephrine was administered to test the success of catheter placement.
3. Results
There was no statistical difference as regard the age of the patients in both groups ranging between 20 and 45 years with a mean of 26.8 in group I and between 19 and 45 years with a mean of 25.4 in group II. Also, there was no statistical difference as regard the patient’s body mass index and the depth of the epidural space from the skin as shown in .
Data were expressed by using mean ±SD.
p value for comparing between the two studied groups using t-test
*: statistical significant at p≤ 0.05
Table 1. Demographic data.
The first-time success rate was significantly higher in the second group 90% compared to 74%in the first group with a p value of 0.037 when analyzed by the chi square test .
Table 2. The data collected.
There is a significant statistical difference between the two groups as regard the number of attempts needed to perform the epidural anesthesia being significantly lower in the first group.
The analysis of the incidence of repositioning of the epidural needle revealed that it was significantly lower in the second group with a p value of 0.047.
There was no statistical difference as regard the need to change the puncture site of the epidural needle with a p value of 0.052
The mean time to localize the epidural space was 79.3 sec in the group using the Accuro device and only 63.4 sec in the group using the real-time ultrasound technique with the acoustic end point, with a statistically significant difference between the two groups with a p value of 0.0012.
Moreover, the total time of the procedure was significantly shorter in the second group with a mean value of 159.64 sec compared to 216.84 sec in the first group and a p value of less than 0.0015.
As regard the incidence of complications, no complications were reported in any of the two groups.
3.1. Discussion
The significantly shorter time taken to insert an epidural catheter using a real-time ultrasound technique with the aid of the acoustic-assisted device to mark the end point of piercing the dura compared to the time taken when using the Accuro device suggest that it is easier to use such a technique. This conclusion was supported by the significantly shorter space localization time, the significantly less attempts needed in the second group to perform the epidural anesthesia, the significantly less need to redirect the needle or change the space chosen to perform the epidural anesthesia.
This relative ease of performing the epidural anesthesia may be explained by combining the benefits of real-time ultrasound and the APAD, making it possible to perform the real-time ultrasound by one operator. The operator is holding with one hand the ultrasound probe and with the other the Tuohy needle connected to the APAD that generates a pitch sound detecting the loss of resistance. So, by using the hearing sensation to detect the loss of resistance this technique makes it possible for the operator to focus all his vision on the ultrasound screen. Therefore, it was easy to guide the Tuohy needle step by step through the anatomy by direct real-time visual tracing using the ultrasound.
The use of the APAD to perform epidural anesthesia was discussed in many publications describing its benefits and concluding that it facilitates the process. Lechner TJ published some work on the use of the APAD; his work also included performing the epidural anesthesia for women in labor [Citation3,Citation4]
Although we did not find any publication comparing the real-time ultrasound epidural technique with the ultrasound-assisted epidural anesthesia, also there is no publication describing the use of ultrasound in combination with APAD but some efforts were found trying to determine the best way to use the ultrasound in performing the epidural anesthesia.
In 2011 Chin et al. published a paper comparing the use of ultrasound to identify the anatomical landmarks for spinal anesthesia in adult patients with difficult surface anatomic landmarks and the traditional method. After performing spinal anesthesia on 120 patients with difficult surface anatomic landmarks divided into two equal groups, he found that the first-attempt success rate was twice as high in when using the US to identify the landmarks (65% vs. 32%; P ˂ 0.001).
There was a twofold difference between both groups in needle insertion attempts (group US, 1 vs. group LM, 2; P ˂ 0.001) and a shorter spinal anesthesia performance time (group US, 5.0 ± 4.9 vs. group LM, 7.3 ± 7.6 min; P = 0.038).
He concluded that pre-procedural ultrasound imaging facilitates the performance of spinal anesthesia in patients with difficult anatomic landmarks [Citation5,Citation6].
In the pursuit of making the ultrasound easier to use a wireless handheld ultrasound (Accuro, Rivanna Medical, Charlottes ville, VA) device (AU), was developed. Pattern recognition software programmed to calculate the depth to epidural space and identify bony landmarks was also incorporated in that device. In 2018 Katherine M tested the efficiency of the Accuro ultrasound device when used in pregnant women and stated that the use of the Accuro device in identification of the insertion point resulted in successful epidural placement at first attempt in 78% of the patients, without redirects [Citation7].
A lot of researches as that done by Perlasin 2014, Shaikh in2013 and Chin indicate that the use of a preprocedural ultrasound scan to locate an appropriate interlaminar window for a midline needle approach to the epidural and intrathecal space reduces the number of needle passes required for success, especially in patients with predictors of technical difficulty (morbid obesity, previous spinal surgery, or spinal deformity). May also increase safety by decreasing the risk of traumatic procedures [Citation8–Citation10]
Chin KJ described the use of pre-procedural ultrasound to facilitate a paramedian (paraspinous) approach. The paramedian needle approach may be required in patients with narrow interspinous spaces or if a satisfactory Transverse interlaminar/interspinous view cannot be obtained [Citation11].
After conducting a learning curve study on 18 anesthesiologists, Margarido concluded that it is difficult to achieve competence in different aspects of ultrasound assessment of the lumbar spine [Citation12].
Some researches were conducted on the real-time ultrasound used to perform epidural anesthesia as that performed by Karmakar how tested the feasibility of performing real-time US-guided paramedian epidural access with the epidural needle inserted in the plane of the US beam in 15 adults patients surgery under an epidural or combined spinal–epidural anesthesia and concluded the possibility of performing epidural using this technique. [Citation13]
Another study by Menace C was published in 2014 aiming to improve the real-time ultrasound usage in epidural anesthesia. Menace C compared three types of Tuohy needles the traditional strata Tuohy needle with the new echogenic Tuohy needles (a strata one and a curved one) and concluded that echogenic Tuohy needles can significantly improve ultrasound-guided neuraxial block performance for needle tip visibility, image quality, and physician comfort [Citation14].
Some studies aimed at finding ways to improve the real-time ultrasound guided epidural anesthesia by improving the technique itself and making it possible to be performed by one operator only. One example of these trials is published by Denis Tran, and concluded that a real-time aim-and-insert ultrasound- guided epidural needle insertion can be performed by a single operator .but described Several limitations, mostly related to the needle guide geometry and the ease of detecting the end point (the epidural space) [Citation15].
The number of qualified doctors who can perform the epidural anesthesia using ultrasound was limited and this was considered as a limitation in this study.
4. Conclusion
combining the use of real-time ultrasound with the APAD in performing epidural anesthesia resulted in easier and faster technique when compared with the new handheld preprocedure Accuro ultrasound device.
Disclosure statement
No potential conflict of interest was reported by the author.
References
- Saravanakumar K, Rao SG, Cooper GM. Obesity and obstetric anaesthesia. Anaesthesia. 2006;61:36–48.
- Grau T, Leipold RW, Conradi R, et al. Ultrasound control for presumed difficult epidural puncture. Acta Anesthesiol Scand. 2001;45:766–771.
- Lechner TJ, van Wijk MG, Maas AJ, et al. Clinical results with the acoustic puncture assist device, a new acoustic device to identify the epidural space. Anesth Analg. 2003;96:1183–7.
- Lechner TJ, van Wijk MG, Jongenelis AA, et al. The use of a sound‑enabled device to measure pressure during insertion of an epidural catheter in women in labour. Anaesthesia. 2011;66:568–73.
- Chin KJ, Perlas A, Chan V, et al. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomical landmarks. Anesthesiology. 2011;115:94–101.
- Chin KJ, Karmakar MK, Peng P. Ultrasonography of the adult thoracic and lumbar spine for central neuraxial blockade. Anesthesiology. 2011;114:1459–1485.
- Seligman KM, Weiniger CF, Carvalho B. Te accuracy of a handheld ultrasound device for neuraxial depth and landmark assessment: a prospective cohort trial. Anesth Analg. 2018;126:1995–1998.
- Perlas A, Chaparro LE, Chin KJ. Lumbar neuraxial ultrasound for spinal and epidural anesthesia: a systematic review and meta-analysis. Reg Anesth Pain Med. 2016;41(2):251–260.
- Shaikh F, Brzezinski J, Alexander S, et al. Ultrasound imaging for lumbar punctures and epidural catheterisations: systematic review and meta analysis. BMJ. 2013;346:f1720.
- Chin KJ, Perlas A, Chan V, et al. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomic landmarks. Anesthesiology. 2011;115:94–101.
- Chin KJ, Perlas A, Chan V. The ultrasound-assisted paraspinous approach to lumbar neuraxial blockade: a simplified technique in patients with difficult anatomy. Acta Anaesthesiol Scand. 2015;59:668–673.
- Margarido CB, Arzola C, Balki M, et al. Anesthesiologists’ learning Margarido curves for ultrasound assessment of the lumbar spine. Can J Anaesth. 2010;57:120–126.
- Karmakar MK, Li X, Ho M-H, et al. Real-time ultrasound guided paramedian epidural access of a novel in-plane technique. Br J Anaesth. 2009;102:845–854.
- Menace C, Choquet O, Abbal B, et al. Real-time ultrasound-guided epidural anaesthesia technique can be improved by new echogenic Tuohy needles: a pilot study in cadavers. Br J Anaesth. 2014;113(2):299–301.
- Tran D, Kamani AA, Al-Attas E, et al. Single-operator real-time ultrasound-guidance to aim and insert a lumbar epidural needle. Can J Anaesth. 2010;57:313–321.