ABSTRACT
Background
Awake tracheal intubation (ATI) is becoming a gold standard in managing the difficult airway. Airway anesthesia is the cornerstone for the preparation of awake fiberoptic intubation (AFOI). Many topical and regional techniques have been developed to attenuate airway reflexes and facilitate AFOI. Glossopharyngeal superior laryngeal and recurrent laryngeal nerves must be blocked to attain adequate reflex abolishment.
Aim
This randomized controlled prospective study was performed to evaluate the effectiveness of adding airway nerve blocks to lignocaine nebulization for nasal AFOI.
Methodology
This was a comparative study conducted in 50 patients randomly allocated into two groups of 25 each: Group A and Group B; both received nebulization of 2% lignocaine 10 mL. Group B was then given airway blocks as bilateral superior laryngeal (2% lignocaine 1.5 mL each) and transtracheal (2% lignocaine 2 mL) block. Group A received the same airway nerve block by the same volume with normal saline 0.9%. Two puffs of 10% lignocaine to the nose and postnasal space on each side were given to both groups. Awake nasal fiberoptic intubation was performed. Vital parameters, such as intubation time, intubation condition, patient comfort scale, satisfaction score, and side effects, were recorded. Statistical analysis for both groups was done.
Results
Statistically, no significant differences were found in demographics and hemodynamics. Regarding intubation time and intubation condition scale, there was a significant improvement in Group B than in Group A. Also, overall patient comfort and satisfaction scores were significantly better in Group B than in Group A.
Conclusion
Upper airway lignocaine nebulization may provide adequate anesthesia for AFOI, but when supplemented by airway nerve blocks, it improves the quality of anesthesia and patient satisfaction.
1. Introduction
The presence of unanticipated difficult airway can threaten the patient life. ‘Cannot intubate, cannot oxygenate’ (CICO) scenario occurs when many attempts for oxygenation by different devices as supraglottic airway device (SAD), facemask or trachea lintubation have failed, and the patient becomes at risk of irreversible hypoxic brain injury and even death. Fronneckt-of- airway (FONA) method may rapidly become the lifesaving method for immediate oxygenation [Citation1], usually by performing a cricothyrotomy. CICO situations are rare and may be associated with significant morbidity and mortality, especially with any hesitation to take the decision of cricothyrotomy [Citation1–Citation3]. This emergency situation pushes Rehak and Watterson to investigate the institutional preparedness of a group of hospitals in New Zealand and Australia for CICO scenarios [Citation4]. Using a flexible fiberoptic bronchoscope for awake intubation is considered a relatively safe and simple way for intubation under direct vision in most situations [Citation5,Citation6]. The incidence of difficult airway intubation cases shows a range of 1–18% of all intubations with different degrees [Citation7]. Before AFOI, appropriate anesthesia of the nose, pharynx, larynx, and trachea, to suppress reflex coughing and gaging during bronchoscopy and intubation. Airway anesthesia can be done by application of local anesthetic over airway mucous membranes (viscous solutions, soaked cotton pledges, spray and nebulization) or by airway nerve block techniques [Citation8]. Nebulization of local anesthetic can achieve effective anesthesia in the most upper respiratory system for AFOI. This technique is simple and there is no fear of needle pain; also, little working knowledge about the anatomy of the airway is sufficient for its successful use [Citation9]. Topical anesthesia alone may be inadequate for AFOI in some patients because the submucosal stretch receptors at the base of tongue may cause gag reflex; these receptors may not be completely blocked by topical nebulization, so they have to be augmented by specific airway blocks [Citation10]. Airway nerve blocks are in the form of glossopharyngeal, superior laryngeal (SLN) and trans tracheal block to abolish gag reflex, closure of the glottis and reflex coughing [Citation9,Citation10]. These nerve blocks may be inadequate in some patients because of bad technique, lack of experience and anatomical variations which can disturb the patient cooperation and can abort AFOI [Citation11–Citation14]. Local anesthesia nebulization can cover a large area in the airway, but with low intense block [Citation9]. Supplementation of this technique with selective airway nerve blocks can be an alternative way to achieve effective anesthesia for AFOI [Citation9,Citation15]. A lot of studies have been done to compare lignocaine nebulization or spray technique with airway nerve block technique, but there is a paucity of the literatures that studied the combined effects of both techniques. So, we hypothesize that by combining the two techniques, we can achieve more suitable condition for AFOI and also better patient cooperation and satisfaction during the procedure. This randomized prospective study was conducted to evaluate the effectiveness of using airway blocks in addition to lignocaine nebulization for topical anesthesia for AFOI in a patient with suspected difficult airway. Also, we used midazolam for sedation, which results in a stable hemodynamic profile and does not compromise respiratory function of the patient. Our primary objective was to compare the intubation time of the two groups, and the secondary objectives were to assess the intubation condition, cough severity and patient satisfaction.
2. Methodology
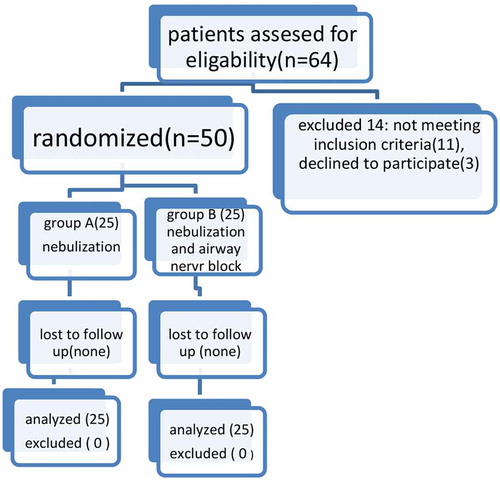
After institutional ethical committee approval, this randomized prospective double-blinded study was conducted in 50 patients in 6-month duration. Patients were allocated into two groups of 25 each of either sex, age 18–60 years, and American Society of Anesthesiologists (ASA) Classes I and underwent surgery under general anesthesia with suspected difficult intubation by using modified Mallampatti grading, thyromental distance and upper lip bite test. We excluded patients who did not provide consent, had an allergy to study drugs or were complaining of bronchial asthma, epilepsy, coagulation disorders or hemodynamically unstable. ENT (ear, nose, and throat) specialist examined patient tonsils to roll out sepsis before glossopharyngeal nerve block. Also, patients with nasal diseases or fracture skull base were excluded. The patients were explained about AFOI for more cooperation, laboratory investigation and medical reports; fasting times were checked and informed consent was obtained. The patients were randomly allocated to two equal groups using computer-generated tables of random numbers. For the purpose of investigator blinding, the baseline parameters, such as heart rate, noninvasive blood pressure, oxygen saturation and electrocardiographic data were recorded in the preparation room with insertion of an intravenous (i.v.) line, ranitidine 50 mg injection (i.v). Glycopyrolate (0.05 mg/kg) was given intravenously (IV) and two drops of xylometazoline 0.1% were instilled in each nasal opening. Fentanyl (1 ug/kg, IV) was injected i.v. 15 min before the procedure. Then, Group A and Group B patients were connected to a nebulizer with oxygen flow rate of 7–10 L/min used to deliver up to 10 mL of 2% lidocaine (lidocaine HCl, injection, USP), 20 mg/mL 50 mL multiple-dose vial (200 mg of which 25% is typically absorbed) [Citation16] into the naso-oro-pharynx, and the patients were encouraged to breathe deeply to facilitate entrainment of nebulized lidocaine into their airway over 10–15 min. Airway nebulization by lignocaine was supplemented by airway nerve block with placebo (normal saline 0.9%) in Group A or lidocaine in Group B with the same volume in both groups. Airway nerve blocks including glossopharyngeal nerve were performed using 1.5 ml of lidocaine 2% in a syringe connected to spinal needle 25 gauge. The tongue was retracted medially, and then the needle was inserted at 0.5 cm lateral to the base of the tongue on the posterior tonsillar pillar; then, the other side was injected [Citation17]. The superior laryngeal nerves were blocked bilaterally by infiltrating 1.5 ml of lignocaine 2% on each side at the lateral and inferior aspect of the hyoid bone. Then, 1% lignocaine 2 mL (20 mg) was injected into the trachea through the cricothyroid membrane. Finally, two puffs of 10% lignocaine to the nose and postnasal space on each side (10 mg) were given in both groups. The amount of local anesthetic was usually within the safe range of the doses allowed; we intended to not exceed 5 mg/kg 400 mg totally (25% only absorbed from topically used lidocaine) [Citation16]. To ensure investigator blinding, all airway blocks (nerve blocks or nebulization) were performed in the separate preparation room which was well equipped by monitors and anesthesia machine and performed by an independent anesthesiologist, who was expert in airway block. The time taken for airway blocks and patient’s preparation was 15–20 min; then, the patient was transferred to the main operative room to undergo AFOI by expert well-trained anesthesia consultant who was blinded to study groups. A flexible 5.0-mm fiberoptic bronchoscope (Karl Storz GmbH & Co. KG, Germany) with a flexible endotracheal tube with internal diameter of 7.0 or 7.5 mm (for females and males, respectively) was used. Intubating conditions and vocal cord position () were recorded by the intubating anesthesiologist, while patient comfort (), post-intubation patient satisfaction (), intubation time and vital signs were recorded by another independent observer who was blinded to the study group. Vital signs were recorded immediately and at 1, 3, 5 and 10 min after intubation. Intubation time is the time from passing the fiberoptic bronchoscope tip into the patient nose to the first capnography reading obtained after endotracheal intubation. Intubating conditionscores indicate the ease of intubation, and reflect the degree of suppression of pharyngeal and laryngeal reflexes, and movement of vocal cord. After confirmation of endotracheal intubation by bronchoscopy and capnography, general anesthesia was started with propofol (2 mg/kg, IV) and atracurium bromide (0.5 mg/kg, IV). Post-operative assessment to assess any adverse effects such as hoarseness, sore throat or any hematoma formation was done by assistant of ENT specialist.
Table 1. Intubation condition, vocal cord position, postoperative patient satisfaction.
Table 2. Patient comfort indices (cough severity, intubation comfort, postintubation assessment).
2.1. Sample size
Based on a previous study by Mathur et al. [Citation18] who reported 30% difference in the intubation time, a total sample size of 50 patients (25 patients in each group) enables us to reject the null hypothesis that the failure rates for study and control subjects are equal with probability (power) of 0.80, when type I error probability associated with this test is 0.05, after adding 20% for possible dropout of patients.
2.2. Statistical analysis
Statistical analyses were performed using SPSS software, version 22.0 (IBM Corp., USA). Quantitative variables are expressed as mean ± SD or median (interquartile range), and categorical variables as number and percent. Shapiro–Wilk test was used to assess normality of quantitative data. To compare variables between two groups, Student’s t test was used for quantitative parametric data, the Mann-Whitney U test for quantitative nonparametric data and Chi-square or Fisher’s test for categorical data. P values <0.05 were considered to be statistically significant.
3. Results
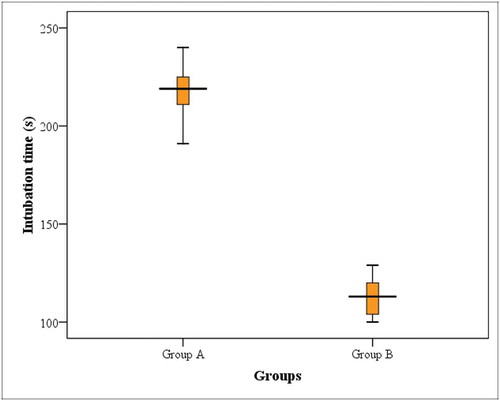
There were non-significant statistical differences in demographic data and airway assessment between both groups (). As shown in and , Group B (nebulizer and airway nerve block) showed significantly shorter intubation time in comparison to Group A (nebulizer group) (112.32 ± 9 s versus 217.08 ± 13.52 s, P < 0.001).
Table 3. Demographic data, airway assessment and intubation time in the studied groups.
Comparison of intubating conditions between both groups () revealed that Group B had significant statistical differences in the frequencies of optimal intubating condition (P = 0.027), relaxed vocal cord position/glottis opening (P = 0.001), cough severity (P < 0.001), intubation comfort (P = 0.001), cooperation after intubation (P = 0.001) and excellent/good patient satisfaction postoperatively (P = 0.001).
Table 4. Comparison of intubating conditions between both groups.
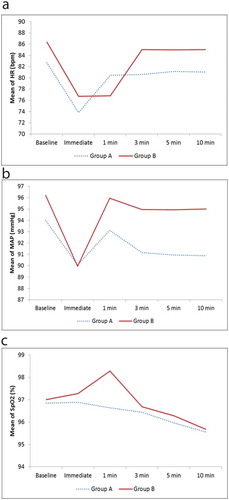
Hemodynamic changes in both groups are presented in . Intragroup comparison of baseline HR (heart rate) and MAB (mean arterial pressure), obtained just after nebulization in GroupA or nebulization and nerve block in Group B and 1 minute after awake fiberoptic intubation, revealed a significant reduction in heart rate and blood pressure in both groups, which returned to near baseline levels at 3, 5 and 10 min post intubation. Heart rate and mean arterial pressure were comparable between the groups 10 minutes after fiberoptic intubation. There were no significant differences regarding oxygen saturation among the study group.
4. Discussion
Awake tracheal intubation (ATI) means insertion of tracheal tube in an awake patient to maintain his spontaneous breathing, most commonly with either flexible bronchoscopy (ATI:FB) or video-assisted laryngoscopy (ATI:VL). This allows securing the patient airway before starting the general anesthesia, avoiding the morbidity and even mortality of management of unanticipated difficult airway [Citation19,Citation20].
Since the invention of the flexible fiberoptic bronchoscope by Dr. Shigeto Ikeda in 1966 [Citation21] and its subsequent application for tracheal intubation in 1967 by Dr. Peter Murphy [Citation22], regional anesthesia of the airway made awake fiberoptic intubation acceptable and not distressing for patients and also allow better control over different intubation conditions. Many authors have compared different airway anesthesia techniques. Webb et al. [Citation23] compared tow techniques of trans-cricoid lidocaine injection and spray-as-you-go for awake fiberoptic intubation in 70 adult patients. Graham et al. [Citation24] compared three different techniques of providing airway anesthesia during fiberoptic bronchoscopy intubation in 53 patients. Kundra et al. [Citation25] studied the effect of nebulized lignocaine 4% combined with airway nerve block for awake fiberoptic intubation in 48 adult patients. Airway nebulization by local anesthetics is an important technique that deposits small droplets of local anesthetic over the mucosa directly, thus producing surface anesthesia without the need for multiple painful injections of local anesthesia. Also, this simple technique may require less detailed knowledge about anatomy, less experience and skills; it can also be used in cases of neck swelling which makes some difficulties with airway nerve block. However, it has some disadvantages including a higher chance of failure, requirement for higher doses of local anesthetic (due to drug wastage during administration) and relatively delayed onset of action. Airway nerve blocks for fibereoptic intubation include: blocks of glossopharyngeal nerve (which anesthetize the oropharynx and abolish the gag reflex), superior laryngeal nerve block (which anesthetize larynx above the vocal cords level and abolishes glottic closure reflex) and trans-tracheal nerve blocks (which anesthetize larynx below the vocal cords the trachea and abolish cough reflex). Airway nerve blocks provide deep and rapid anesthesia by small doses of local anesthetic, but this technique requires thorough knowledge of upper respiratory system anatomy, operator skill and experience; it also has a risk of intravascular injection and sometimes neural injury can not be excluded. In cases of disturbed airway anatomy such as neck swelling, traumatic injury to the face or the neck and local infection, the airway nerve block may become difficult [Citation26,Citation27].
In our study, we used 10 ml of 2% lignocaine (200 mg) for nebulization, in addition to lidocaine 10% puffs in both nostril (20 mg), and even after supplementation of nebulization group by airway nerve block (Group B), the total dose did not exceed the maximum allowed dose of lignocaine. Sutherland et al. [Citation28] used a nebulization median dose of 512 mg which caused toxicity in two patients at a plasma concentration above 5 μg/ml, but that a dose of 370 mg did not cause toxicity. Gjonaj et al. [Citation29] used two doses, 8 mg/kg and 4 mg/kg lignocaine, for airway nebulization and found no toxicity observed; also, Parkes et al. [Citation8] who used a dose of 6 mg/kg lignocaine, noticed plasma lignocaine level did not exceed 0.45 mg/L in any of their patients. Because in our study there was no way to measure concentrations of plasma lignocaine, we limited the maximum lignocaine dose to 400 mg. Techanivate et al. [Citation30] found effective upper airway anesthesia for fiberoptic bronchoscopy intubation using 2% lignocaine in the form of nebulization and topical application of cocaine in the nose.
Many studies compared the different techniques of awake FOB intubation, but this randomized controlled study was performed to study the effectiveness of using airway nerve blocks in addition to lignocaine nebulization and local anesthesia nebulization before needle injection decreases the discomfort of airway instrumentation [Citation31]. Airway nerve blocks provide good anesthesia to facilitate the awake FOB intubation [Citation6].
In our study, there was no failed intubation in either group. The mean intubation time was significantly shorter in Group B (mixed block) than in Group A (nebulization block). Also, intubation condition, relaxed vocal cords, patient comfort during AFOI and post-intubation satisfaction all were significantly improved in Group B than in Group A.
Manish Khandelwal et al. [Citation32] reported that patient comfort and patient satisfaction score were better in the group of mixed block of nebulization and airway nerve block than the other group of airway nerve block alone, despite no significant difference regarding the intubation time and intubation grading scale which may be due to low dose of lidocaine used in nebulization (4 ml 2% lidocaine) than in our study. Augmenting our idea of supplementation of the nebulization by air way neve block, the study by Reasoner et al. [Citation27] found no significant difference in the intubation time between the topical anesthesia and nerve block group. The topical anesthesia group received 20 mL of 4% lignocaine through nebulization with a trans-tracheal injection of 3 mL lidocaine. The airway nerve block group received glossopharyngeal, SLN blocks and trans-tracheal injection of lidocaine. No difference in the result may be regarded to trans-tracheal injection in topical anesthesia group of nebulization, which further improved the quality of anesthesia. This explains the significant improvement in our combined group than the nebulization group that we did not inject trans-tracheal lidocaine in topical nebulized group plus needle intraoral injection of glossopharyngeal nerve in our mixed group. Blocking the glossopharyngeal nerve is a part of effective block [Citation23]. It should be noted that in all previous studies no standardized scale for measuring intubating conditions was used, and so it was difficult to compare their intubating conditions with those in our study. The patient comfort compared between our two study groups was indicated by cough severity and intubation comfort scores during and after AFOI; it was higher in the mixed block Group B. This can be regarded to direct injection of lignocaine in the vicinity of the airway nerves. However, during nebulization, the lignocaine is deposited over the airway mucosa, so a big amount of local anesthetic is needed. In addition, it can lead to patchy, less effective anesthesia. Gupta et al. [Citation6] also observed significant coughing in the group of nebulization compared with airway nerve block group.
Kundra et al. [Citation25] compared two techniques of airway anesthesia for AFOI. One group was blocked by 4 mL of 4% lignocaine through nebulization and the other group received airway nerve blocks; intubation time was nearly similar in both groups; grimace scores and hemodynamic parameters were significantly higher in nebulization group during. In our study, both groups were given nebulization and one group was supplemented with airway nerve block, and hence, cough reflex in the form of bronchoscopy time, intubation grading and vocal cord movement was significantly better in combined group than in nebulized one. Hemodynamic parameters in our patients remained stable; this can be regarded to fentanyl injection before the procedures. Although we noted some reduction in mean blood pressure and heart rate from baseline just after AFOI in both groups, without the need for any pharmacological intervention, they normalized within 3–5 minutes after intubation. In contrast to our study, Kundra et al. [Citation25] reported increase in patient hemodynamics in their groups, although the increase was significantly greater in the nebulization group than in combined block group. We found that oxygen saturation parameter was comparable between Group A and Group B. The patients received supplemental oxygen through the bronchoscope channel and no desaturation was recorded during the AFOI.
The local anesthetic (lignocaine) concentrations used in our study were below the acceptable toxic limits. But we lookout for any signs and symptoms of lignocaine toxicity.
4.1. Limitation
Limitation of our study was not having the facility for measuring serum lignocaine level especially in combined methods of airway blocks. Secondly, our results cannot be directly interpreted to the cases with difficult airways as the study included all grades of airway; so, further studies may be required.
5. Conclusion
Our study revealed that anesthesia of the airway using lignocaine nebulization supplemented by airway nerve blocks is superior to lignocaine nebulization alone for awake fiberoptic bronchoscopy intubation. Regarding the ease of intubation, patient comfort and satisfaction, lignocaine airway nebulization may be used as an alternative technique for airway anesthesia when airway nerve block is not accessible as we observed no case of failed AFOI and no complications recorded during nebulization.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the fourth national audit project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011;106:617–631.
- Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth. 2012;109:i68–85.
- Groom P, Schofield L, Hettiarachchi N, et al. Performance of emergency surgical front of neck airway by head and neck surgeons, general surgeons, and anaesthetists: an in-situ simulation study. Br J Anaesth. 2019;123:696–703.
- Rehak A, Watterson LM. Institutional preparedness to prevent and manage anaesthesia-related ‘can’t intubate, can’t oxygenate’ events in Australian and New Zealand teaching hospitals. Anaesthesia. 2020;75:767–774.
- Panchabhai TS, Mehta AC. Historical perspectives of bronchoscopy. Connecting the dots. Ann Am Thorac Soc. 2015;12:631–641.
- Gupta B, Kohli S, Farooque K, et al. Topical airway anesthesia for awake fiberoptic intubation: comparison between airway nerve blocks and nebulized lignocaine by ultrasonic nebulizer. Saudi J Anaesth. 2014;8:S15–9.
- Langenstein H, Cunitz G. Difficult intubation in adults. Anaesthesist. 1996;45:372–383.
- Parkes SB, Butler CS, Muller R. Plasma lignocaine concentration following nebulization for awake intubation. Anaesth Intensive Care. 1997;25:369–371.
- Pani N, Kumar Rath S. Regional and topical anaesthesia of upper airways. Indian J Anaesth. 2009;53:641–648. [PMC free articlePubMedGoogle Scholar].
- Hagberg CA, Artime CA, Aziz MF. Hagberg and Benumof’s airway management. 4th ed. Texas (USA): Elsevier publication; 2017.
- Faccenda KA, Finucane BT. Complications of regional anaesthesia incidence and prevention. Drug Saf. 2001;24:413–442. [PubMed] [Google Scholar].
- Auroy Y, Narchi P, Messiah A, et al. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology. 1997;87:479–486. [PubMed] [Google Scholar].
- Naguib M, Magboul MM, Samarkandi AH, et al. Adverse effects and drug interactions associated with local and regional anaesthesia. Drug Saf. 1998;18:221–250.
- Cotter JT, Nielsen KC, Guller U, et al. Increased body mass index and ASA physical status IV are risk factors for block failure in ambulatory surgery-an analysis of 9,342 blocks. Can J Anaesth. 2004;51:810–816.
- Ovassapian A. Fiberoptic tracheal intubation in adults. Fiberoptic endoscopy and the difficult airway. 2nd ed. New York: Lippincott Raven. [Google Scholar].
- Kritzinger S, Greunen VM. Awake fiberoptic intubation: the basics anaesthesia tutorial of the week 201. Wakefield (UK): World Federation of Societies of Anaesthesiologists; 2010.
- Simmons ST, Schleich AR. Airway regional anesthesia for awake fiberoptic intubation. Reg Anesth Pain Med. 2002;27:180–192.
- Mathur PR, Jain N, Kumar A, et al. Comparison between lignocaine nebulization and airway nerve block for awake fiberoptic bronchoscopy-guided naso tracheal intubation: a single-blind randomized prospective study. Korean J Anesthesiol. 2018;71(2):120–126.
- Cook TM. Strategies for the prevention of airway complications – a narrative review. Anaesthesia. 2018;73:93–111.
- Alhomary M, Ramadan E, Curran E, et al. Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia. 2018;73:1151–1161.
- Ikeda S, Yanai N, Ishikawa S. Flexible bronchofiberscope. Keio J Med. 1968;17:1–16.
- Murphy P. A fibre-optic endoscope used for nasal intubation. Anaesthesia. 1967;22:489–491.
- Webb AR, Fernando SS, Dalton HR, et al. Local anaesthesia for fibreoptic bronchoscopy: transcricoid injection or the “spray as you go” technique? Thorax. 1990;45:474–477.
- Graham DR, Hay JG, Clague J, et al. Comparison of three different methods used to achieve local anesthesia for fiberoptic bronchoscopy. Chest. 1992;102:704–707.
- Kundra P, Kutralam S, Ravishankar M. Local anaesthesia for awake fibreoptic nasotracheal intubation. Acta Anaesthesiol Scand. 2000;44:511–516.
- Cohn AI, Zornow MH. Awake endotracheal intubation in patients with cervical spine disease: a comparison of the bullard laryngoscope and the fiberoptic bronchoscope. Anesth Analg. 1995;81:1283–1286. [PubMed] [Google Scholar].
- Reasoner DK, Warner DS, Todd MM, et al. A comparison of anesthetic techniques for awake intubation in neurosurgical patients. J Neurosurg Anesthesiol. 1995;7:94–99.
- Sutherland AD, Santamaria JD, Nana A. Patient comfort and plasma lignocaine concentrations during fibreoptic bronchoscopy. Anaesth Intensive Care. 1985;13:370–374.
- Gjonaj ST, Lowenthal DB, Dozor AJ. Nebulized lidocaine administered to infants and children undergoing flexible bronchoscopy. Chest. 1997;112:1665–1669.
- Techanivate A, Leelanukrom R, Prapongsena P, et al. Effectiveness of mouthpiece nebulization and nasal swab stick packing for topical anesthesia in awake fiberoptic nasotracheal intubation. J Med Assoc Thai. 2007;90:2063–2071.
- Cullen L, Taylor D, Taylor S, et al. Nebulized lidocaine decreases the discomfort of nasogastric tube insertion: a randomized, double-blind trial. Ann Emerg Med. 2004;44:131–137.
- Khandelwal M, Saini VK, Kothari S, et al. Role of lignocaine nebulization as an adjunct to airway blocks for awake fiber-optic intubation: a comparative study. Anesth Essays Res. 2018 July–Sep;12(3):735–741.