ABSTRACT
Background: A large number of patients undergoing major surgical procedures for the management of breast cancer complain of acute postoperative pain. The present study aimed to evaluate the effect of dexmedetomidine when added as an adjuvant to bupivacaine on the quality of this block after modified radical mastectomy (MRM) surgery.
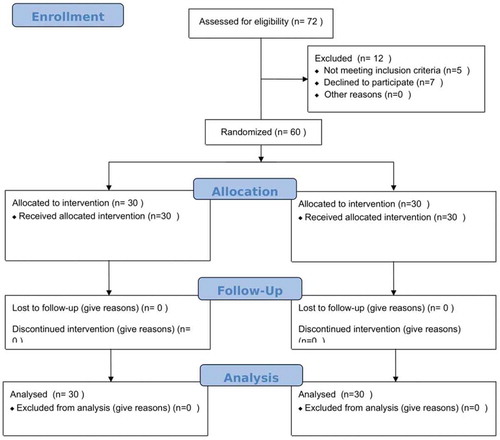
Patients and methods: Patients were randomly divided into two equal groups after induction of general anaesthesia. Bupivacaine group (I) (n = 30): received bupivacaine 0.25% in a dose of 0.5 ml/kg injected superficial to serratus anterior muscle. Bupivacaine–dexmedetomidine group (II) (n = 30): received bupivacaine of 0.25% as described above plus dexmedetomidine (0.5 µg/kg) injected superficial to serratus anterior muscle.
Results: Requesttime for first analgesic (duration of analgesia in group II (19 ± 3 h) when compared to the group I (14 ± 4 h) and decrease doses of morphine consumption postoperatively (group II (6 ± 2 mg/24 h) when compared to the group I (10 ± 2 mg/24 h)(p 0.01).
Conclusion: Dexmedetomidine used as an adjuvant to bupivacaine in ultrasound-guided serratus plane block during modified radical mastectomy surgery leads to an increase of analgesic effect and decrease doses of morphine consumption postoperatively.
1. Introduction
A large number of patients undergoing major surgical procedures for the management of breast cancer complain of acute postoperative pain and also postoperative nausea and vomiting [Citation1].
When postmastectomy pain managed by opioids alone may lead to many side effects such as nausea and vomiting, inadequate control of pain may lead to chronic pain syndrome (paraesthesias, intercostobrachial neuralgia, and phantom breast pain) in 25–40% of the patients [Citation2]. These complications lead to patient discomfort, extended post-anaesthesia care unit stays, prolonged admissions, and additional hospital costs. Therefore, regional analgesic techniques have been mandatory for effective pain management [Citation3].
Many regional analgesic techniques are trying to decrease the side effects associated with general anaesthesia and opioid consumption. These techniques involving local wound infiltration, thoracic epidural analgesia, intercostal nerve block, and thoracic paravertebral block [Citation4,Citation5].
Ultrasound-guided local anaesthetic injection in the fascial plane either superficial or deep to the serratus anterior muscle in the lateral chest wall anaesthetizes cutaneous branches of the intercostal nerves innervating the surgical site [Citation6].
Dexmedetomidine is a strong sedative, analgesic, and it has anaesthetic effects when used in general anaesthesia. If it is used as a perineural adjuvant will promote better anaesthesia and analgesia [Citation7]. A significant prolongation of the duration of analgesia was reported when dexmedetomidine was added to LA (by inhibiting the function of sodium channels and neuronal potassium) for epidural analgesia, subarachnoid block, caudal block, paravertebral block, ulnar nerve block, brachial plexus block, and greater palatine nerve block [Citation8].
This study aims to assess the dexmedetomidine effect as an adjuvant to bupivacaine on the quality of the ultra-sound guided serratus plane block after modified radical mastectomy surgery.
2. Patients and methods
This prospective, randomized, double-blind study conducted after approval by the Ethical Committee of Benha University Hospital on 60 American Society of Anesthesiologists (ASA) I and II women, aged 20 years or more, undergoing MRM under general anaesthesia at Anaesthesia Department, Benha University Hospitals from May 2019 to August 2020. The serratus plane block procedure and the visual analogue scale (VAS) identifying 0 as no pain and 10 as worst imaginable pain were explained to each patient before the surgery and informed written consent was obtained.
Exclusion criteria include patients undergoing bilateral breast surgery or breast reconstruction; patient refusal, infection at the injection site, anticoagulant therapy, abnormal coagulation profile, hypersensitivity to LA; patients on chronic antiemetics or chronic pain medication; obese patients with a body mass index (BMI) >30 kg/m2 and pregnant patients.
Patients were randomly allocated through sealed envelopes to two equal groups (n = 30 in each group) using a computer-generated randomization schedule. Group I received bupivacaine 0.25% in a dose of 0.5 ml/kg injected superficial to serratus anterior muscle. Group II received bupivacaine 0.25% as described above, plus dexmedetomidine (0.5 mcg/kg) injected superficial to serratus anterior muscle.
Patients fasted for 6 h before the surgery. Routine monitoring, including ECG, pulse oximetry, non-invasive blood pressure, heart rate (HR), was done in the pre-anaesthesia room. Midazolam was intravenously administered (1–2 mg) as a premedication.
In all groups, GA was induced with sleep dose of propofol and fentanyl 1 μg/kg. Tracheal intubation was facilitated with vecuronium 0.1 mg/kg. Anaesthesia was maintained with oxygen, nitrous oxide, and isoflurane 1–2%. Fentanyl 0.5 μg/kg. Before recovery from general anaesthesia, and after the end of the surgery, the regional block technique was performed.
Neuromuscular blockade was reversed using neostigmine 0.05 mg/kg, and atropine 0.02 mg/kg and extubation were performed after complete neuromuscular reversal.
The ultrasound-guided Serratus Anterior Plane block was done after surgery ended, under sterile conditions with the patients in the lateral position with the diseased side up. A linear ultrasound transducer (10–12 MHz) was placed in a sagittal plane over the mid-clavicular region of the thoracic cage. The ribs were counted down till the fifth rib identified in the mid-axillary line. The latissimus dorsi (superficial and posterior), teres major (upper) and serratus muscles (deep and inferior) were identified overlying the fifth rib.
The primary outcome measure included pain rescue analgesic consumption in the first 24 h (time of first rescue analgesic and total rescue analgesic requirement). The degree of postoperative pain assessed at post-anaesthetic care unit (PACU), at 4, at 6, at 8, at 12, at 16, at 20, and 24 h using the VAS. When VAS was higher than 4, the patients were given morphine (5 mg IV). Secondary outcome measures included blood pressure and HR every hour for the first 6 h postoperatively. In addition, the occurrence of postoperative nausea and vomiting was recorded, which was managed by ondansetron 4 mg. Postoperative analgesia was maintained with IV paracetamol (1000 mg) every 8 h. Any complication related to the blocks and the duration of hospital stay was recorded.
3. Statistical analysis
Numerical data summarized as means and standard deviations or medians and ranges. Categorical data summarized as numbers and percentages. Comparisons between two groups done by using: independent t-test for normally distributed variables, test for non-normally distributed variables and Mann–Whitney U- test for non-normally distributed variables. Categorical variables compared between two groups by using χ2-test or Fisher’s exact test if appropriate. P values less than 0.05 considered significant, and less than 0.001 considered highly significant.
4. Sample size
Considering the alpha cut-off of 0.05 and power of 80% and (d = μ1-μ2 = 1.2), Zα/2 is dependent to the level of significance which for 5% this is 1.96, Zβ: is dependent on power and for 80% this is 0.84; so 30 patients in each group were calculated [Citation9].
5. Results
Sixty patients were recruited in this study; the patients allocated into two groups of 30 each. As regard to demographic data, there were insignificant statistical differences between the two groups ().
Table 1. Demographic data of both groups
As regards VAS during rest, there was a highly significant reduction (P < 0.001) in the median VAS in group II when compared to group I at the 12th h and a statistically significant reduction (P = 0.013) at the 16th h postoperatively. As regards VAS at PACU, 4, 8, 20, and 24 h postoperatively, there were no significant differences between both groups ().
Table 2. Visual analogue scale at rest in both groups during 24 h postoperative
As regards VAS during movement, there was a significant decrease in the median VAS in group II when compared to group I at the 12th h (P < 0.044), a highly significant decrease at the 16th h postoperatively (P < 0.002). As regards VAS, at PACU, 4, 8, 20, and 24 h postoperatively, there were insignificant differences between both groups ().
Table 3. Visual analogue scale during movements in both groups during 24 h postoperative
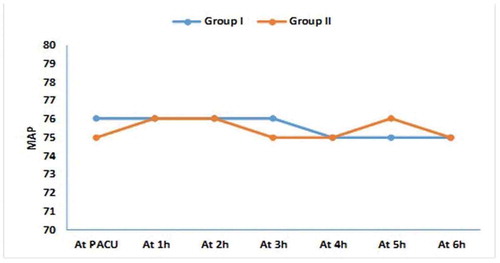
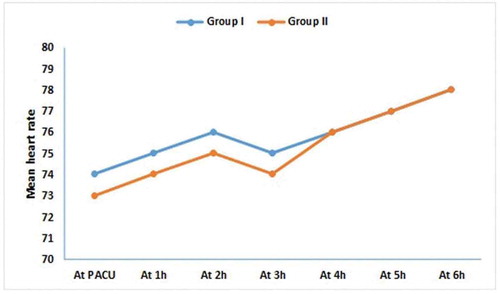
There were no statistical differences between both groups, as regards the MAP, and HR on arrival to the PACU and every hour for the first 6 h postoperatively with P-value more than 0.05 ().
As regards the time of first rescue analgesia, there was a significantly longer duration of analgesia in group II (19 ± 3 h) when compared to the group I (14 ± 4 h) with P-value of 0.007. As regards the total dose of morphine consumption during 24 h postoperatively, the total dose of morphine consumption was significantly lower in group II (6 ± 2 mg/24 h) when compared to the group I (9 ± 2 mg/24 h) with P-value of 0.01 ().
Table 4. Pain rescue-analgesia consumption in the first 24 h in both groups
6. Discussion
Dexmedetomidine has peripheral as well as central actions. Centrally it exerts analgesic action by inhibition of substance P release in the nociceptive pathway at the dorsal root neuron and by activation of alpha-2 receptors in locus coeruleus. The peripheral action of this alpha-2 agonist to produce analgesia is mediated by decreasing the release of norepinephrine [Citation10,Citation11].
The present study agrees with Bakr et al. [Citation12] who studied the efficacy of 1 µg/kg dexmedetomidine added to an ultrasound (US)-modified pectoral (Pecs) block on postoperative pain and stress response in patients undergoing MRM. Their study showed the addition of 1 µg/kg dexmedetomidine to a US-modified Pecs block has superior analgesia and more reduction to stress hormone levels without serious side effects when compared to a regular Pecs block in patients who undergo MRM.
In addition, this current study agrees with the study done by Manzoor et al. [Citation13] who studied the quality of postoperative analgesia and patient’s satisfaction with addition of dexmedetomidine to bupivacaine versus plain bupivacaine in pectoral nerve block type I and II in breast surgeries. Their study showed that the addition of dexmedetomidine increased the duration of postoperative analgesia in pecs I and II block without serious side effects.
Mohamed et al. [Citation14] observed that addition of dexmedetomidine 1 µg/kg to bupivacaine in the thoracic paravertebral block in patients undergoing modified radical mastectomy increased the duration of analgesia and decreased analgesic requirements with no serious hemodynamic adverse effects.
This current study goes with Haramritpal et al. [Citation15] who studied the effect of the addition of dexmedetomidine to LA agent on the total duration of analgesia and postoperative morphine consumption. Their study showed that the addition of 1 μg/kg dexmedetomidine to 0.25% ropivacaine for Pecs block prolongs the duration of analgesia and reduces postoperative morphine consumption.
Keplinger et al. [Citation16] observed that dexmedetomidine with ropivacaine produces a dose-dependent increase in the duration of the sensory block. Higher doses of dexmedetomidine may be associated with a higher incidence of sedation. A dose of 100 μg may represent a balance between efficacy and sedation.
Abdallah and Brull [Citation17] reported that dexmedetomidine in doses of 1 μg/kg seems to provide an optimal balance between adequate postoperative analgesia and adverse effects in peripheral nerves blocks.
Conclusion
The addition of dexmedetomidine as an adjuvant to bupivacaine in ultrasound-guided serratus plane block during MRM surgery increases the analgesic effect and decrease doses of morphine consumption postoperatively.
Financial support and sponsorship
Nil.
Disclosure statement
There are no conflicts of interest.
References
- Poleshuck EL, Katz J, Andrus CH, et al. Risk factors for chronic pain following breast cancer surgery: a prospective study. J Pain. 2006;7:626–634.
- Andersen KG, Kehlet H. Persistent pain after breast cancer treatment: a critical review of risk factors and strategies for prevention. J Pain. 2011;12:725–746.
- Gartner R, Jensen MB, Nielsen J, et al. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302:1985–1992.
- Boughey JC, Goravanchi F, Parris RN, et al. Prospective randomized trial of paravertebral block for patients undergoing breast cancer surgery. Am J Surg. 2009;198:720–725.
- Moller JF, Nikolajsen L, Rodt SA, et al. Thoracic paravertebral block for breast cancer surgery. A randomized, double-blind study. Anesth Analg. 2007;105:1848–1851.
- Chakraborty A, Khemka R, Datta T. Ultrasound-guided truncal blocks: A new frontier in regional anaesthesia. Indian J Anaesth. 2016;60:703–711.
- Das B, Lakshmegowda M, Sharma M, et al. Supraclavicular brachial plexus block using ropivacaine alone or combined with dexmedetomidine for upper limb surgery: a prospective, randomized, double-blinded, comparative study. Rev Esp Anestesiol Reanim. 2016;63:135–140.
- Gu XY, Liu BL, Zang KK, et al. Dexmedetomidine inhibits tetrodo- toxin-resistant Nav1.8 sodium channel activity through Gi/Co-dependent pathways in rat dorsal root ganglion neurons. Mol Brain. 2015;8:15.
- Gupta K, Srikanth K, Girdhar KK, et al. Analgesic efficacy of ultrasound-guided paravertebral block versus serratus plane block for modified radical mastectomy: a randomized, controlled trial. Indian J Anaesth. 2017;16:381–386.
- Biswas S, Das RK, Mukherjee G, et al. Dexmedetomidine as an adjuvant to levobupivacaine in supraclavicular brachial plexus block: a randomized, double-blind prospective study. Ethiop J Health Sci. 2014;24:203–208.
- Köksal E, Karakaya D, Can B, et al. Intracerebroventricular application of dexmedetomidine produces antinociception and does not cause neurotoxicity in rats. Balkan Med J. 2013;30:355–361.
- Bakr MA, Mohamed SA, Mohamad MF, et al. Effect of dexmedetomidine added to modified pectoral block on postoperative pain and stress response in patient undergoing modified radical mastectomy. Pain Physician. 2018;21(2):E87–E96.
- Manzoor S, Taneja R, Sood N, et al. Comparative study to assess the quality of analgesia of bupivacaine and bupivacaine with dexmedetomidine in ultrasound-guided pectoral nerve block type I and II in breast surgeries. J Anaesthesiol Clin Pharmacol. 2018;34(2):227–231.
- Mohamed SA, Fares KM, Mohamed AA, et al. Dexmedetomidine as an adjunctive analgesic with bupivacaine in paravertebral analgesia for breast cancer surgery. Pain Physician. 2014;17:589–598.
- Haramritpal K, Poonam A, Gurpreet S, et al. Dexmedetomidine as an adjunctive analgesic to ropivacaine in pectoral nerve block in oncological breast surgery: A randomized, double-blind prospective study. J Anaesthesiol Clin Pharmacol. 2017;33(4):457–461.
- Keplinger M, Marhofer P, Kettner SC, et al. pharmacodynamic evaluation of Dexmedetomidine as an additive drug to ropivacaine for peripheral nerve blockade: A randomized, triple-blind controlled study in volunteers. Eur J Anaesthesiol. 2015;32:790–796.
- Abdallah FW, Brull R. Facilitatory effects of perineural dexmedetomidine on neuraxial and peripheral nerve block: A systematic review and meta-analysis. Br J Anaesth. 2013;110:915–925.